Abstract
Purpose
To report a rare case of extreme leukocytosis and leukemoid reaction associated with lung sarcomatoid carcinoma (LSC) and increase people’s awareness of the disease.
Patients and methods
A 58-year-old male patient was diagnosed with LSC; however, after the end of the second course of chemotherapy, his white blood cells increased gradually without fever or use of medications such as granulocyte colony-stimulating factor and steroids. A bone marrow biopsy then confirmed it to be a leukemoid reaction.
Results
The patient died of multiple organ failure 2 months after being diagnosed with leukocytosis.
Conclusion
LSC associated with leukemoid reaction is very rare and the prognosis is poor. When a patient’s white blood cells are extremely elevated, we should think of the possible causes of the tumor itself and identify it with other diseases. However, more data and evidence are still needed to find an effective adjuvant therapy for these patients.
Introduction
Lung sarcomatoid carcinomas (LSCs) are very rare, mostly reported in the form of case reports, and leukemoid reactions has rarely been described in patients with LSC, to the best of our knowledge. Meanwhile, the mechanism of leukocytosis is not very clear. Here, we discuss an unusual case of extreme leukocytosis and a leukemoid reaction associated with the LSC. We summarize the relevant reports, hoping to provide some help for other clinicians when they encounter similar disease or symptoms.
Case presentation
A 58-year-old male patient had symptoms of intermittent cough and hemoptysis with no incentives in June 2014, and accompanying chest tightness and shortness of breath. He was first admitted to a local hospital, where computed tomography of the chest showed a left lung mass, suggesting a probability of tuberculosis. Therefore, he was treated for tuberculosis, but had no significant relief of symptoms. He then visited our hospital, where he underwent computed tomography-guided biopsy; the pathology results showed poorly differentiated adenocarcinoma (left lung). He then underwent surgery for resection of the mass; pathological examination showed poorly differentiated peripheral pulmonary carcinoma with the tumor being composed of mononuclear and multinucleated tumor giant cells with significant atypia. Immunohistochemistry showed: creatine kinase (CK) (−), P63 (−), thyroid transcription factor (TTF)-1 (−), CK18 (+), Napsin A (−), CK (+), vimentin (+), smooth muscle actin (SMA) (−), desmin (−), epidermal growth factor receptor (EGFR) (++), Ki-67 (+60%), epithelial membrane antigen (EMA) (+); the consideration is sarcomatoid carcinoma (giant cell carcinoma). The patient received two courses of chemotherapy in our hospital after surgery, gemcitabine 1.4 D1and 8 + cisplatin 30 mg D1–4 and tolerated it well.
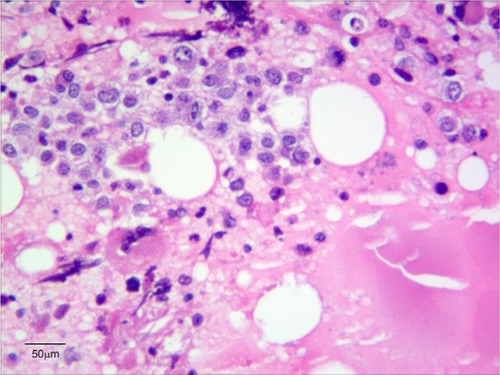
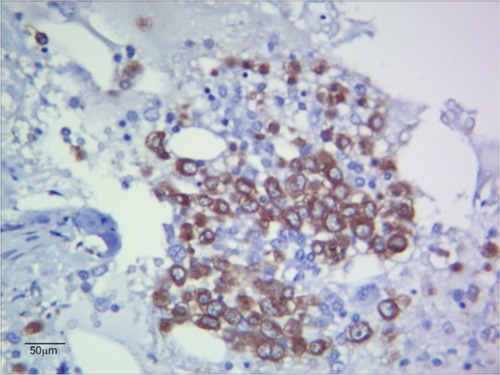
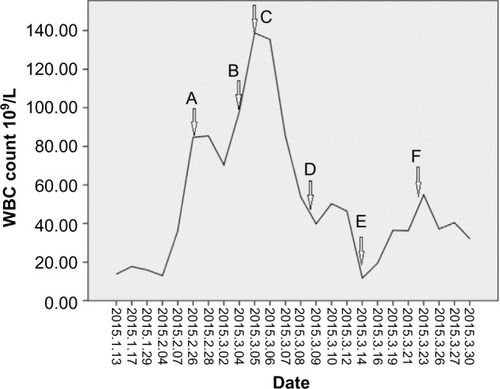
However, the patient’s white blood cells (WBCs) increased gradually without fever or use of medications, such as granulocyte colony-stimulating factor (G-CSF) and steroids, after the end of the second course (), and neutrophils accounted for ~93%. While his hemoglobin and platelets were within the normal range. We initially used antibiotics empirically, which was ineffective. Next, a bone marrow biopsy was performed; the results showed myeloid and erythroid focal hyperplasia and significant partial immature myeloid cell proliferation (). Immunohistochemistry showed individual lymphocytes CD3 (+), individual lymphocytes CD20 (+), erythroid CD235a (+), megakaryocytes CD61 (+), CD34 (−), individual monocytes CD14 (+), individual plasma cells CD138 (+), a large number of myeloid myeloperoxidase (MPO) (+) (). Finally, the patient was diagnosed with leukocytosis, then he and his family refused further chemotherapy, so we put the patient on “hydroxyurea” to control the leukocytosis. The patient died of multiple organ failure 2 months after being diagnosed with leukocytosis. This study was approved by the Ethics Committee of The Affiliated Cancer Hospital of Zhengzhou University.
Figure 1 WBC gradually increased postoperatively.
Abbreviations: bid, twice daily; po, per os; tid, three times a day; WBC, white blood cell.
Discussion
Sarcomatoid carcinoma is a poorly differentiated malignant cancer, which is composed of both carcinomatous and sarcomatous elements. It can occur in many parts of the body, but most commonly affects the respiratory tract, lungs, breasts, and kidneys. Clinically, sarcomatoid carcinoma originating in the lung (LSC) is very rare, accounting for 0.3%–4.7% of all lung malignancies.Citation1 LSC is a non-small-cell lung carcinoma, which has a high degree of malignancy, and is more aggressive than the average lung cancers. The effects of radiotherapy and chemotherapy are not very good; therefore, the prognosis of LSC is poor.Citation2–Citation4
Leukemoid reaction is defined as a WBC count >50×109/L without evidence of leukemia or infection.Citation5 Leukemoid reaction is a potential cause for leukocytosis, especially in the presence of predominately mature granulocytic leukocytosis. A leukemoid reaction is caused by an exaggerated myeloid; it has been associated with infections, allergies, burns, intoxications, acute hemorrhage, malignant neoplasms, and several other stimuli.Citation6–Citation9
LSC associated with leukemoid reaction is very rare. The mechanism of leukemoid reaction is not very clear. Cancer-related symptoms, may be caused by G-CSF secreted by the tumor cells.Citation10–Citation12 Chen et alCitation13 indicated that, in cases of leukemoid reaction, leukocytosis is frequently mediated by tumor-related cytokines and CSF including G-CSF, granulocyte-macrophage CSF, interleukin 6 or 1α.
Jardin et alCitation14 have reported a case with lung sarcoma and leukemoid reaction. The patient’s G-CSF concentration increase was observed after the first cycle of chemotherapy (>20,000 pg/mL). Dramatically, the highest G-CSF concentration level was observed when the WBC count was lowest, suggesting that a massive cytokine release appeared after tumor lysis related to chemotherapy.Citation14 We also observed a similar phenomenon in our report; after chemotherapy, the patient’s WBC experienced dramatic increases. For various reasons, we have not measured G-CSF concentration level, but we can speculate that perhaps the reason was the same.
Leukemoid reaction always indicates a high degree of malignancy, high probability of metastasis, and recurrence and wretched prognosis. In our report, the patient died of multiple organ failure 2 months after being diagnosed with leukocytosis. This is consistent with other reports correlating leukemoid reactions with advanced and aggressive tumor cell growth and poor outcome.Citation6,Citation15
In conclusion, LSC associated with leukemoid reaction is very rare and the prognosis is poor. When a patient’s WBC is extremely elevated, we should think of possible causes of the tumor itself and identify it with other diseases. However, more data and evidence are still needed to find an effective adjuvant therapy for these patients.
Acknowledgments
Written informed consent was obtained from this patient for publication of this case report and any accompanying images.
Disclosure
The authors report no conflicts of interest in this work.
References
- PelosiGSonzogniADe PasTPulmonary sarcomatoid carcinomas: a practical overviewInt J Surg Patho12010182103120
- MartinLWCorreaAMOrdonezNGSarcomatoid carcinoma of the lung: a predictor of poor prognosisAnn Thorac Surg200784397398017720411
- VenissacNPopDLassalleSBerthierFHofmanPMourouxJSarcomatoid lung cancel(spindle/giant cells): an aggressive disease?J Thorac Cardiovasc Surg2007134361962317723808
- YukiTSakumaTOhbayashiCPleomorphic carcinoma of the lung: a surgical outcomeJ Thorac Cardiovasc Surg2007134239940417662779
- McKeeLExcess leukocytosis (leukemoid reactions) associated with malignant diseasesSouth Med J19857812147514823877987
- StavKLeiboviciDSiegelYILindnerALeukemoid reaction associated with transitional cell carcinomaIsr Med Assoc J20024322322411908271
- MarinellaMAExtreme leukemoid reaction associated with retroperitoneal hemorrhageArch Intern Med199815833003019472215
- Pina-CeballosVMMontemayor-GarzaRGonzalez-OritzJLeukemoid reaction secondary to prenatal use of betamethasone in a premature neonateRev Mex Pediatr199764197200
- AbramsonNMeltonBLeukocytosis: basics of clinical assessmentAm Fam Physician20006292053206011087187
- NimieriHSMakoniSNMadziwaFHNemiaryDSLeukemoid reaction response to chemotherapy and radiotherapy in a patient with cervical carcinomaAnn Hematol200382531631712739065
- TuralicHDeamantFDReeseJHParaneoplastic production of granulocyte colony-stimulating factor in a bladder carcinomaScand J Urol Nephrol200640542943217060092
- LeeMYKaushanskyKJudkinsSALottsfeldtJLWaheedAShad-duckRKMechanism of tumor-induced neutroneutrophilia: constitutive production of colony-stimulating factors and their synergistic actionsBlood1989741151222473793
- ChenYMWhang-PengJLiuJMLeukemoid reaction resulting from multiple cytokine production in metastatic mucoepidermoid carcinoma with central necrosisJpn J Clin Oncol19952541681727545252
- JardinFVasseMDebledMParaneoplastic neutrophilic leukemoid reaction related to a G-CSF-secreting lung sarcomaAm J Hematol200580324324516247754
- KasugaIMakinoSKiyokawaHKatohHEbiharaYOhyashikiKTumor-related leukocytosis is linked with poor prognosis in patients with lung carcinomaCancer20019292399240511745296