Abstract
Background
Red cell distribution width (RDW) is a quantitative measurement and shows heterogeneity of red blood cell size in peripheral blood. RDW has recently been associated with cardiovascular events and cardiovascular diseases, and it is a novel predictor of mortality. In this study, we aimed to evaluate the clinical usefulness of measuring RDW in patients with coronary stent thrombosis.
Patients and methods
We retrospectively reviewed 3,925 consecutive patients who presented with acute coronary syndrome and who underwent coronary angiography at the Siyami Ersek Hospital between May 2011 and December 2013. Of the 3,925 patients, 73 patients (55 males, mean age 59±11 years, 55 with ST elevated myocardial infarction) with stent thrombosis formed group 1. Another 54 consecutive patients who presented with acute coronary syndrome (without coronary stent thrombosis, 22 patients with ST elevated myocardial infarction, 44 males, mean age 54±2 years) and underwent percutaneous coronary intervention in May 2011 formed group 2. Data were collected from all groups for 2 years. The RDW values were calculated from patients 1 month later at follow-up. Syntax scores were calculated for all the patients. The patients were also divided as low syntax score group and moderate–high syntax score group.
Results
The patients in group 1 with stent thrombosis had significantly higher RDW level (13.85) than the patients in group 2 without stent thrombosis (12) (P<0.001). In addition, in all study patients, the moderate–high syntax score group had significantly higher RDW level (13.6) than the low syntax score group (12.9) (P=0.009). A positive correlation was determined between RDW and syntax scores (r=0.204).
Conclusion
RDW is a new marker of poor prognosis in coronary artery disease. Increased RDW level is correlated with angiographic severity of coronary artery disease, and RDW may be an important clinical marker of coronary stent thrombosis in patients undergoing coronary intervention.
Introduction
The red cell distribution width (RDW) is a measurement of size variation and an index of the heterogeneity of erythrocytes, which is calculated by dividing the standard deviation of red blood cell volume by the mean corpuscular volume and multiplying by 100 to express the result as a percentage. The normal reference range of RDW spans between 11% and 14%.Citation1 In recent studies, the predictive and prognostic value of RDW levels has been shown in several cardiovascular diseases. High RDW values were also shown to be associated with increased mortality with coronary artery disease (CAD).Citation2 A few studies demonstrated that higher RDW, even within the normal reference range, was strongly associated with increased risk of death and cardiovascular events in middle-aged and older adults.Citation3 Stent thrombosis is a rare but mortal condition, due to which predictors of stent thrombosis were investigated in many studies.Citation4 Several studies have reported an association between inflammation and stent thrombogenicity. However, there are limited trials that studied the relationship between RDW and the risk of stent thrombosis in patients with CAD. Therefore, in this study, we examined the clinical usefulness of RDW value in patients with coronary stent thrombosis.
Patients and methods
Study population
We retrospectively reviewed 3,925 consecutive patients who presented with acute coronary syndrome and who underwent coronary angiography at the Siyami Ersek Hospital between May 2011 and December 2013. Of the 3,925 patients, 73 patients (55 males, mean age 59±11 years, 55 with ST elevated myocardial infarction [STEMI]) with stent thrombosis formed group 1. Another 54 consecutive patients who presented with acute coronary syndrome (without coronary stent thrombosis, 22 patients with STEMI, 44 males, mean age 54±2 years) and underwent percutaneous coronary intervention (PCI) on May 2011 formed group 2. Data were collected from both groups for 2 years. Only one patient in group 2 had stent thrombosis during the 2 years. This patient was excluded from the study. Patients who had blood transfusion within 4 months, malignancy, connective tissue disease, and hematological disease were excluded from the study. The study was approved by Siyami Ersek Hospital review board. This retrospective study was deemed exempt written informed consent by the Siyami Ersek Hospital review board because it used only retrospective, de-identified patient data.
Methods
Coronary angiography and angioplasty
Group 1 and group 2 patients underwent angiography using the Judkins technique. Severity of CAD was determined with syntax score. Low syntax score was defined as <23, and moderate–high syntax score was defined as ≥23. PCI of patients in the groups was done according to the European Society of Cardiology guidelines.Citation5–Citation7
Laboratory measurements
The RDW and other laboratory values were obtained from the collected data 1 month after the intervention.
Statistical analysis
Predictive Analytics SoftWare (PASW), Statistics 18 (SPSS Inc, Chicago, USA) for Windows program was used for data input and statistical analysis. Mean, median, standard deviation, and minimum and maximum values were used to describe the results. Kolmogorov–Smirnov test was used to test data normality. Independent-samples t-test was used to compare two groups showing normal distribution, and Mann–Whitney U test was used to compare two groups with abnormal distribution. Chi-square analysis was used for categorical data comparison. Pearson’s and Spearman correlation analysis tests were used to determine the correlation between variables. Values of P<0.05 were considered to be statistically significant.
Results
Demographic and clinical characteristics of the study groups are presented in . Group 1 and group 2 were similar in terms of sex distribution. Mean age was higher in group 1 (59.87±11.02 years) than in group 2 (54.37±1.79 years) (P=0.01). Both groups had similar diabetes rates, but hypertension was more frequent in stent thrombosis group (group 1 n: 58, group 2 n: 29, P=0.003). Hemoglobin levels were lower in patients with stent thrombosis (group 1 Hb: 13 mg/dL, group 2 Hb: 14 mg/dL, P=0.001). Mean platelet volume and white blood cell levels of the groups were similar. Creatinine, triglyceride, and high-density lipoprotein levels were similar. Group 2 had higher levels of low-density lipoprotein (P=0.04). C-reactive protein (CRP) levels were higher in patients with stent thrombosis (group 1 CRP: 0.7, group 2 CRP: 0.3, P=0.001). There were eleven patients with aspirin resistance in group 1, while group 2 had none (P=0.001). Both groups had similar clopidogrel resistance rates. Mean ejection fraction was 50% (20–60) in group 1 and 55% (35–65) in group 2 (P=0.01).
Table 1 Demographic and clinical characteristics of the study groups
Comparison of syntax scores showed that group 2 had lower syntax scores (group 1 mean syntax score was 12.90 [2.00–42.00], and mean syntax score of group 2 was 10.00 [1.00–36.00], P=0.009). Drug-eluting stent (DES) was higher in group 1 (DES group 1, n=33; DES group 2, n=11; P=0.001).
RDW value was 13.85 (11.40–18.70) in group 1 and 12.00 (10.70–14.00) in group 2 (P<0.001). demonstrates the comparison of RDW values between group 1 and group 2. There was no relation between RDW and the timing of occurrence of stent thrombosis (stent thrombosis in the first 24 hours after implantation [n=16] RDW 14.05±0.65, 24 hours–1 month [n=31] RDW 14.42±1.94, 1 month–1 year [n=20] RDW 13.96±1.35, after 1 year [n=7] RDW 14±2.01, P=0.8). Group 1 with low syntax score (n=51) had a mean RDW value of 13.75 (11.40–18.70), and group 2 with low syntax score (n=46) had a mean RDW value of 12.00 (10.70–14.00) (P<0.01). Group 1 with moderate–high syntax score (n=22) had a mean RDW value of 14.15 (12.10–18.70), and group 2 with moderate–high syntax score (n=7) had a mean RDW value of 12.40 (11.80–12.90) (P<0.01). In group 1, there was no significant difference between patients with low syntax score and moderate–high syntax score (P>0.05). These results are presented in . When the patient groups with and without stent thrombosis were combined, mean RDW levels were 12.9 (10.70–18.70) in patients with a low syntax score and 13.6 (11.80–18.70) in patients with moderate–high syntax score (P=0.09). A positive correlation was determined between RDW level and syntax score when the groups were combined (r=0.204). This is further highlighted in . Group 1 with aspirin resistance had a mean RDW value of 13.6±1.8, and group 1 without aspirin resistance had a mean RDW value of 14.2±1.6. There was no significant difference between patients with and without aspirin resistance (P=0.33). The higher CRP and lower ejection fraction values had no influence on the RDW level in group 1 and group 2 (P<0.05). The RDW values were not significantly different according to DES usage in group 1 and group 2. The decrease in hemoglobin level was correlated with an increase in RDW (P=0.01).
Figure 1 Comparison of values of RDW% between cases (group 1) and controls (group 2).
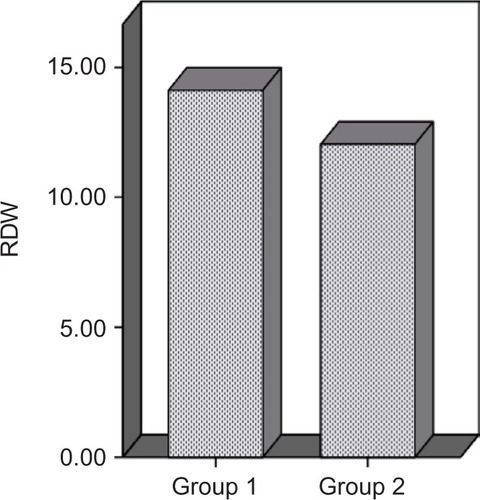
Figure 2 Statistical correlation between RDW% and syntax score.
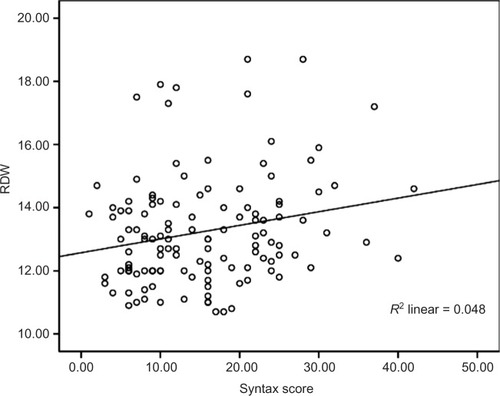
Table 2 The relationship between of syntax scores and RDW values.
Discussion
Stent thrombosis occurs in 0.5%–1% of patients within 1 year. It has been associated with 30-day mortality rate of 10%–25%. Approximately 20% of patients with a first stent thrombosis experience a recurrent stent thrombosis episode within 2 years. The mechanism underlying stent thrombosis is multifactorial.Citation8–Citation11
RDW is a parameter that is routinely reported as part of the complete blood count. In recent years, the predictive and prognostic value of RDW has been shown in several cardiovascular diseases and events.Citation1–Citation3 Although the exact physiological mechanisms between increased RDW and atherosclerosis are unknown, oxidative stress, inflammation, and increase in cholesterol levels in erythrocyte membrane are responsible for erythrocyte malformation; thus, they increase RDW levels. Inflammation or oxidative stress might contribute to an increased RDW by impairing iron metabolism, inhibiting the production of or response to erythropoietin, and shortening red blood cell survival.Citation12,Citation13 Lippi et alCitation14 stated that there is an increase in RDW levels during acute coronary syndrome. They showed the clinical usefulness of RDW for the risk stratification of these patients over a 1-year period. When the cutoff value of RDW was 14%, the sensitivity and specificity of RDW were 79% and 50%, respectively.
In our study, the RDW levels of the group that has stent thrombosis are higher than those of the other group without stent thrombosis. There was no relation between RDW and timing of occurrence of stent thrombosis. Similar to the previous studies, high RDW levels are associated with risk factors (age, hypertension, hyperlipidemia, high CRP levels).Citation3,Citation4,Citation15,Citation16 Increased RDW has been shown to be correlated with severity of coronary atherosclerosis.Citation17 In this study, RDW levels increased as the syntax scores increased. These findings support the study by Fatemi et al, which showed high RDW levels in patients with two or more vessel disease.Citation17 In another study, it was reported that RDW levels increased even in patients with early phase of atherosclerosis.Citation2 Vaya et alCitation18 studied 119 patients with acute myocardial infarction and concluded that RDW levels >14 are associated with a sixfold increase in cardiovascular events even after adjusting for anemia. During the follow-up period, 30 patients developed a recurrent cardiovascular event in their study. However, they did not find an association between high-sensitivity CRP and the risk of developing future cardiovascular events.
Osadnik et alCitation19 studied the effects of RDW levels on long-term prognosis over 2 years in 2,550 stable angina pectoris patients who underwent PCI, and they showed that mortality is four times higher in patients with a high RDW level. They could not demonstrate a relationship between RDW and stent thrombosis rate. The association of RDW and long-term mortality in patients undergoing PCI was observed by Fatemi et alCitation17 and Poludasu et al.Citation20 Poludasu et alCitation20 also reported that RDW was a predictor of mortality in patients who had hemoglobin values exceeding 10.4 g/dL. That study excluded patients who had STEMI.Citation20 In our study, the mean hemoglobin levels in group 1 and group 2 were 13 g/dL and 14 g/dL, respectively. This difference was statistically significant, and lower hemoglobin values were associated with increasing RDW values. Fatemi et alCitation17 investigated the prognostic value of RDW in 1,689 patients treated with stent implantation for 1 year. That study included 55 patients with hemoglobin <10.4 g/dL and 150 patients who had STEMI. The authors analyzed whether there was a significant difference between RDW quartiles and death, myocardial infarction (MI), and combined events, but not of unplanned revascularization.Citation17 Additionally, stent type did not change the results for RDW in that study. Yao et alCitation21 demonstrated that high RDW was associated with an increased risk of all cause death, cardiac death, and with stent thrombosis in nonanemic patients with CAD treated with DES. They did not measure high-sensitivity CRP in most of the patients. In our study, CRP levels are high in patients with high RDW level and stent thrombosis as well. But high CRP values were not associated with increasing RDW values (P>0.05). The other studies showed that patients who are resistant to aspirin are at greater risk of adverse cardiovascular events regardless of the assay used to measure aspirin resistance.Citation22,Citation23 In our study, aspirin resistance was more frequent in the stent thrombosis group. There was no relation between RDW and aspirin resistance. There is also no known association between aspirin and clopidogrel resistance and RDW levels.Citation19 Based on these studies, we can conclude that high RDW level may be the reason for high stent thrombosis rates.
Even though patients with anemia were excluded, lower hemoglobin values in the stent thrombosis group may contribute to the increase of RDW levels. It can be considered as a limitation of this study. Another limitation is that iron, vitamin B12, and folate levels were not measured.
Conclusion
In this study, high RDW level was associated with increased risk of stent thrombosis, but it was not related to the timing of occurrence of stent thrombosis. Increased RDW was also correlated with angiographic severity of CAD. More studies with large patient population are needed to support its prognostic significance in patients undergoing PCI who are at risk of stent thrombosis. RDW may be an important clinical marker to estimate the coronary stent thrombosis in PCI.
Author contributions
AE, BT, and USC conceived and designed the study. A Erdem, KO, A Emre, and EZ performed the experiments. A Esen, SY, ST, and BT analyzed and interpreted the data. A Erdem and KY wrote the manuscript and revised the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or nonprofit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
- MontagnanaMCervellinGMeschiTLippiGThe role of red cell distribution width in cardiovascular and thrombotic disordersClin Chem Lab Med201250463564122505527
- WenYHigh red cell distrubition width is closely associated with risk of carotid artery atherosclerosis in patients with hypertensionExp Clin Cardiol2010153374020959889
- PatelKSembaRFerrucciLRed cell distribution width and mortality in older adults: a meta analysisJ Gerontol A Biol Sci Med Sci201065325826519880817
- MalandrinoNWuWTaveiraHWhitlatchHSmithJAssociation between red cell distribution width and macrovascular and microvascular complications in diabetesDiabetologia201255122623522002006
- KirtaneAStoneGHow to minimize stent thrombosisCirculation2011124111283128721911796
- KappeteinAFeldmanTMackMComparison of coronary bypass surgery with drug eluting stenting fort the treatment of left main and/or three-vessel disease: 3- year follow-up of the SYNTAX trialEur Heart J201132172125213421697170
- ShiomiHMarimotoTHayanoMCREDO-Kyoto PCI/CABG Registry Cohort-2 InvestigatorsComparison of long-term outcome after percutaneous coronary intervention versus coronary bypass grafting in patients with unprotected left main coronary artery disease (from the CREDO-Kyoto PCI/CABG registry cohort-2)Am J Cardiol2012110792493222721575
- KolhPDanchinNAlfonsoFGuidelines on myocardial revascularizationEur Heart J201031202501255520802248
- WindeckerSMeierBLate coronary stent thrombosisCirculation2007116171952196517965406
- ZangQLiYWangXIncidence and predictors of definite stent thrombosis after coronary stent implantationChin Med J201212591547155122800819
- BuchananGBasavarajaiahSChieffoAStent thrombosis: incidence, predictors and new technologyThrombosis2012201295696222577541
- KalayNAytekinMKayaMThe relationship between inflammation and slow coronary flow:increased red cell distribution width and serum uric acid levelsArch Turk Soc Cardiol2011396463468
- TziakasDChalikiasGGrapsaAGiokaTTentesIKonstantinidesSRed blood cell distribution width-a strong prognostic marker in cardiovascular disease-is associated with cholesterol content of erythrocyte membraneClin Hemorheol Microcirc201251424325422277951
- LippiGFilippozziLMontagnanaMClinical usefulness of measuring red blood cell distribution width on admission in patients with acute coronary syndromesClin Chem Lab Med200947335335719676148
- AzabBTorbeyEHatoumHUsefulness of red cell distribution width in predicting all- cause long-term mortality after non ST elevation myocardial infarctionCardiology20111192728021849785
- Al- NajjarYGoodeKMZhangJClelandJGClarkALRed cell distribution width: an inexpensive and powerful prognostic marker in heart failureEur J Heart Fail200911121155116219926599
- FatemiOParanilamJRainowARed cell distribution width is a predictor of mortality in patients undergoing percutaneous coronary interventionJ Thromb Thrombolysis2013351576422752404
- VayaAHernandezJZorioEBautistaDAssociation between red blood cell distribution width and the risk of future cardiovascular eventsClin Hemorheol Microcirc201250322122522240356
- OsadnikTStrzelczykJHawranekMRed cell distribution width is associated with long term prognosis in patients with stable coronary artery diseaseBMC Cardiovasc Disord20131311324320974
- PoludasuSMarmurJDWeedonJKhanWCavusogluERed cell distribution width (RDW) as a predictor of long-term mortality in patients undergoing percutaneous coronary interventionThromb Haemost2009102358158719718480
- YaoHSunTZhangXRed blood cell distribution width and long-term outcome in patients undergoing percutaneous coronary intervention in the drug-eluting stenting era: a two year cohort studyPLoS One201494e9488724722190
- KrasopoulosGBristerSBeattieSBuchananMAspirin resistance and risk of cardiovascular morbidity: systematic review and meta analysisBMJ2008336763719519818202034
- BiondiGLotrionteMAspirin resistance in cardiovascular diseaseBMJ200833616516718218999
