Abstract
Mild head trauma had been defined in patients with direct impact or deceleration effect admitted with a Glasgow Coma Scale score of 13–15. It is one of the most frequent causes of morbidity in emergency medicine. Although common, several controversies persist about its clinical management. In this paper, we describe the Brazilian guidelines for mild head trauma, based on a critical review of the relevant literature.
Introduction
Mild head trauma scoring 13–15 on the Glasgow Coma Scale (GCS)Citation1 cannot be neglected. This is a very common situation that may lead to severe morbidity or even mortality, depending on the history of the trauma, the patient’s previous health status, and physical and neurological examination during hospital attendance.
Mild head trauma is caused by direct head impact or by an encephalic deceleration effect that produces a period of temporal and spatial disorientation, post-traumatic amnesia, or unconsciousness for up to 20 minutes.Citation1–Citation3 Patients are admitted to the emergency room with a GCS score of 13–15, usually without focal neurological lesions.Citation1,Citation2,Citation4–Citation6
Dacey et alCitation7 estimate that 300,000–325,000 patients in the US need medical treatment due to mild head trauma each year, which represents 80% of all head trauma patients admitted to American hospitals. Between 52% and 72% of these patients need to stay in hospital for observation or specific treatment.Citation8,Citation9 However, these figures are underestimated, because a large number of patients with mild head trauma do not seek medical attention, given the apparent trivial nature of the symptoms.
In 1981, Rimel et alCitation10 found a 35% increase in blood alcohol levels in patients admitted with mild head trauma (scoring 13–15 on the GCS). High levels of alcohol in the blood make it harder to diagnose head trauma, because of alterations in consciousness caused by alcohol that are independent of the severity of head trauma. Almost all patients show a significant decrease in GCS score when the concentration of alcohol in the blood is higher than 200 mL/dL.Citation10,Citation11 Therefore, the initial assessment of such patients is difficult, and their first GCS scores need to be reconsidered by doctors. In this study, the authors review the classification and management of patients with mild head injury, and present the guidelines adopted by the Brazilian Neurosurgery Society and Brazilian Medical Association.
Trauma classification and management
A significant number of patients initially classified as having mild head trauma may have memory or neuropsychological disorders, or even severe headaches, which can lead to social dysfunction and loss of productivity, especially related to work.Citation12 They may also need neurosurgical intervention, and failure to make the correct diagnosis might have fatal consequences.
When dealing with patients suffering from mild head trauma, an ideal classification scale should establish which patients, even when neurological examinations are normal, may have an increased risk of intracranial hematomas or a negative progression such as “talk and deteriorate” or “talk and die”.Citation4,Citation12–Citation16
Based on evidence in the literature and regional characteristics in our country, we classified mild head trauma using the GCS, as well as signs and symptoms during admission, into low-risk, medium-risk, and high-risk.
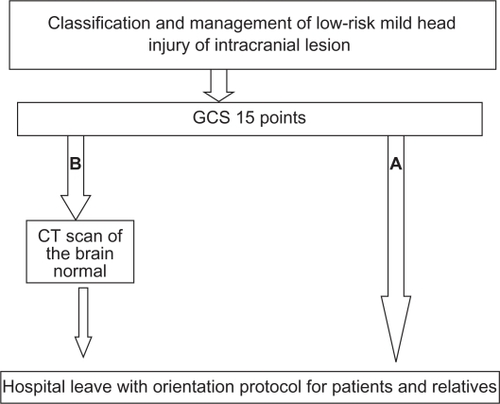
shows the flow chart for management of low-risk mild head trauma (GCS 15), which is divided into three groups. Group 1 consists of patients with low intensity head trauma, who are totally asymptomatic, with a normal physical and neurological examination, and who could be assisted by a general practitioner and sent for a simple skull X-ray according to medical criteria. If this is normal, the patient then receives medical orientation and is subsequently discharged. Group 2 consists of patients with mild head trauma and symptoms, including nonprogressive headache, dizziness, or temporary amnesia. These patients might be submitted for a simple skull X-ray. If this is normal and the patient becomes asymptomatic, they receive specific orientation and are then discharged. In case of a normal examination with persistence of symptoms, the patient may stay under medical observation and undergo an encephalic computed tomography (CT) scan. Group 3 includes patients who show signs of fracture on X-ray. These patients need to undergo a CT scan. If this is normal, they can be discharged after 12 hours of observation. Patients with a CT scan showing intracranial air, traumatic subarachnoid hemorrhage, or intracranial hematoma need to stay in hospital and receive specific treatment for moderate head trauma.Citation1,Citation2
Figure 1 Management of patients with low-risk mild head trauma. A) Asymptomatic patients. B) Patients with minor clinical symptoms.
The literature shows an incidence of skull fractures in patients with low-risk mild head trauma of only 0.4%, and none of them developed intracranial hematomas.Citation17
Patients who show any of the following findings can be classified as medium-risk mild head trauma:
Medical history of complex trauma with moderate kinetic energy, child battery, involvement in a severe accident, alcohol or drug intoxication, progressive headache, vomiting, convulsions, or transient loss of consciousness
General physical examination findings of periocular or postauricular ecchymosis (Battle’s sign), major scalp lesions, multiple body trauma, penetrating head trauma, severe facial lesions, or anosmia
Neurological/neuropsychological findings of temporal and spatial disorientation, amnesia, memory disorder, and behavioral/attention or concentration disorders.Citation15
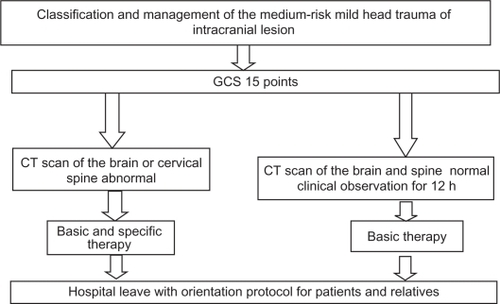
Patients with medium-risk mild head trauma show a 4.2% incidence of skull fractures and a 4% incidence of intracranial lesions.Citation18 Therefore, these patients need to undergo a CT scan of their head and an X-ray of the cervical spine. If all examinations are normal, the patient receives specific orientation and is discharged after 12 hours of medical observation, provided he or she has become asymptomatic. If the examinations are not normal, the patient stays in hospital and is given care according to what is established by the protocol for management of medium-risk mild head trauma ().Citation1,Citation2,Citation18
Figure 2 Management of medium-risk mild head trauma. All patients must undergo a computed tomography scan of the brain.
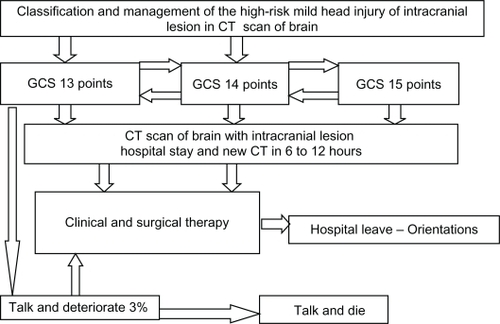
Patients scoring 13 or 14 on GCS, or those who score 15 and also show a severe trauma mechanism, despite normal general and neurological examination, with loss of consciousness for up to 20 minutes and no intracranial lesions on the CT scan, are classified as patients with high-risk mild head trauma.Citation19 Other patients classified as high-risk include battered children with a head trauma, hemophiliacs, patients with pre-existing mental disabilities, pregnant women, those with coagulation disorders, and those with visual deficit or signs of cerebrospinal fluid leak. All of these patients need a CT head scan and a cervical spinal X-ray, or even a spinal CT scan. Even if these examinations are normal, the patient should stay under medical observation for 48 hours. Even though the patient’s condition may progress to “talk and deteriorate” or “talk and die”, they usually show gradual improvement when they receive specific orientation, and are discharged after 48 hours of observation ( and ). According to Masters et al, these patients show skull fractures in 21.5% of cases, in addition to a 29% incidence of intracranial lesions.Citation17 In our service, we applied this protocol when attending 112 patients with mild traumatic brain injury, and found a patient with a head injury and a score of 15 on GCS as well as a case of epidural hematoma, in whom a CT scan would always be performed using this protocol.
Figure 3 Patients with high-risk mild head trauma and normal first computed tomography scan of the brain.
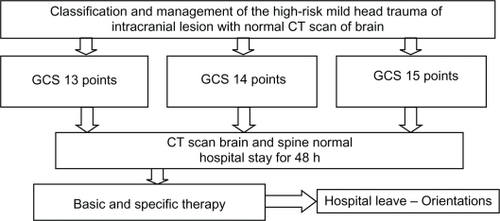
Figure 4 Patients with high-risk mild head injury and intracranial lesion in the first computed tomography scan of the brain.
In contrast, Mendelow et alCitation18 report that patients with a skull fracture and alteration of consciousness have a 25% chance of developing intracranial hematoma, and the incidence of such lesions in patients without a skull fracture is one in every 6000 persons.
Mild head trauma and CT scan
Smits et alCitation20 described a CT scan protocol for head trauma based on an evaluation of 3181 patients. Pre-existing protocols based on signs and symptoms were used, and a high sensitivity and specificity for surgical and nonsurgical intracranial lesions were subsequently found. Therefore, the use of patients’ signs and symptoms as predictors of such lesions showed a high sensitivity and specificity.Citation20
Patients who scored 15 on GCS, and were either sent for immediate CT scan or only stayed under medical observation, progress similarly. However, the early CT scan is the best cost-benefit strategy, because when this is normal during the patient’s admission, it suggests a good prognosis without neurological complications.Citation21
According to Advanced Trauma Life Support®, patients with mild head trauma are awake, but show amnesia for events that happened right before or after the trauma. Almost all patients with mild head trauma make good progress, with occasional, slight neurological alterations. However, about 3% of them may have a sudden deterioration.Citation22 The ideal practice is to perform a CT scan in all patients who show more than mere temporary unconsciousness, amnesia, or severe headache.Citation20 If a CT scan is not available and the patient is completely awake and asymptomatic, the patient should stay under medical observation for 12 to 24 hours at the hospital. A study with 658 patients with a history of post-trauma unconsciousness or amnesia revealed an 18% incidence of altered findings on CT scan and a 5% incidence of surgical lesions.Citation23 Among patients who scored 13 on the GCS, 40% of altered CT scans and 10% of surgical lesionsCitation24 were described, more likely to be moderate head traumas. None of the 542 patients with a normal CT scan on admission showed deterioration or a need for surgery.
Complications
Although mild head trauma has traditionally received less attention than severe head trauma, it represents a significant problem for the neurosurgeon and for emergency room doctors for a number of reasons. First of all, according to Dacey et al,Citation7 a small yet considerable number of patients with mild head trauma may have fatal complications that require urgent neurosurgical intervention. Also, the great majority of hospitalized head trauma patients have had a mild head trauma, which constitutes one of the most common reasons for hospitalization of post-trauma patients. Moreover, because of its high incidence and the risk of complications in a small proportion of patients, evaluation of those with mild head trauma requires considerable time and expenditure. Finally, some patients show persistent symptoms or neurological deficits that lead to high morbidity.Citation25 Rimel et alCitation2 described that 79% of these patients had headaches, 59% of them remained with memory disorders, and 34% were incapable to return to work.
In 1996, while studying the individual relationship between patients admitted with GCS scores of 13, 14, and 15 points and trauma severity, Culotta et alCitation26 demonstrated that the degree of brain injury and the need for neurosurgical intervention increase significantly with a decrease in the GCS from 15 to 13. Patients with mild head trauma which deteriorates (including death, a persistent vegetative state, and/or severe complications) are related in about 0.2%–3.4% of cases.Citation27
With regard to postconcussion syndrome, if it persists, psychological features will entirely account for the symptoms in some individuals, and organic or quasi-organic features will entirely account for symptoms in others. Because the vast majority of patients with uncomplicated mild head injury will not receive extensive investigations, it may be prematurely inferred that organic processes are not present, and therefore psychological processes must be the only, or predominant, cause of the syndrome.Citation28 CoetzerCitation29 describes that future research on management could potentially enhance the prevention of chronic symptomatology developing into postconcussion syndrome. This might also explain our understanding of patients in whom postconcussion symptoms persist beyond one year following injury.
Conclusion
Mild head injury is a very common condition seen in neurosurgery, and represents 80% of all head trauma patients admitted to hospital. Mortality is extremely rare and can be almost completely avoided by early diagnosis and treatment. Identification of risk factors for an intracranial lesion is important to determine which patients can be assessed and discharged, and which patients should be admitted and investigated. Because patients with mild head trauma are not usually evaluated by neurosurgeons, it is vital that general practitioners and emergency doctors know what factors are reference points to perform adequately with when dealing with mild head trauma.
Disclosure
The authors report no conflicts of interest in this work.
References
- LevinHSOutcomes from mild head injuryNarayanRKWilbergerJEPovlishockJTNeurotraumaNew York, NYMcGraw-Hill1996
- RimelRWGiordaniBBarthJTModerate head injury: Completing the clinical spectrum of brain traumaNeurosurgery1982113443517133350
- AndradeAFCiquiniOFigueiredoEGBrockRSMarinoJRJrDiretrizes do atendimento ao paciente com traumatismo craniencefálicoArq Bras Neurocir199918131176 Spanish.
- AndradeAFMarinoRJrCiquiniOJrGuidelines for neurosurgical trauma in BrazilWorld J Surg2001251186120111571957
- LangfittTWGennarelliTAObristWDProspects for the future in the diagnosis and management of head injury: Pathophysiology, brain imaging in population based studiesGalbraithJGClinical NeurosurgeryBaltimore, MDWilliams & Wilkins1982
- KellyDFDobersteinCBeckerDPGeneral principles of head injury managementNarajanRKWilbergerJEPovlishokJTNeurotraumaNew York, NYMcGraw-Hill1996
- DaceyRGJrAlvesWMRimelRWNeurosurgical complications after apparently minor head injuryJ Neurosurg1986652032103723178
- KrausJFEpidemiology of head injuryCooperPRHead Injury3rd edBaltimore, MDWillians & Wilkins1993
- RoseJValtonenSJennettBAvoidable factors contributing to death after head injuryBr Med J19772615661409450
- RimelRWGiordaniBBarthJTDisability caused by minor head injuryNeurosurgery198192212287301062
- GalbraithSMurrayWRPatelARThe relationship between alcohol and head injury and its effect on the conscious levelBr J Surg1976631281301252711
- WilliamsDHLevinHSEisenbergHMMild head injury classificationNeurosurgery1990274224282234336
- FrenchBNDublinABThe value of computerized tomography in the management of 1000 consecutive head injuriesSurg Neurol19777171183847631
- AndradeAFCiquiniOJrFigueiredoEGDiretrizes do atendimento ao paciente com TCEFreireETrauma: A Doença do SéculoSão PauloAtheneu2001
- AndradeAFMarinoRJrMiuraFKProjeto Diretrizes da Associação Médica Brasileira e Conselho Federal de Medicina. Diagnóstico e Conduta no Paciente com Traumatísmo Craniencefálico LeveSão PauloAMB/CFM2001
- LeeJHMartinNAAlsinaGMcArthurDLZauchaKHovdaDAHemodynamically significant cerebral vasospasm and outcome after head injury: A prospective studyJ Neurosurg1997872212239254085
- MastersSJMcCleanPMArcareseJSSkull x-ray examinations after head trauma. Recommendations by a multidisciplinary panel and validation studyN Engl J Med198731684913785359
- MendelowADTeasdaleGJennetBRisk of intracranial hematoma in head injuried adultsBr Med J1983287117311766414615
- HsiangJNKYeungTAshleyLMPoonWSHigh-risk mild head injuryJ Neurosurg1997872342389254086
- SmitsMDippelDWSteyerbergEWPredicting intracranial traumatic findings on computed tomography in patients with minor head injury: The CHIP prediction ruleAnn Intern Med200714639740517371884
- af GeijerstamJLOredssonSBrittonMOCTOPUS Study InvestigatorsMedical outcome after immediate computed tomography or admission for observation in patients with mild head injury: Randomized controlled trialBr Med J200633346516895944
- Comitê de Trauma do Colégio Americano de CirurgiõesSuporte Avançado de Vida no Trauma (SAVT-ATLS®6th edChicago, ILAmerican College of Surgeons1997
- SteinSCSpettellCYoungGRossSELimitations of neurological assessment in mild head injuryBrain Inj199374254308401484
- SteinSCRossSEModerate head injury: A guide to initial managementJ Neurosurg1992775625641527615
- de AndradeAFde AlmeidaANBor-Seng-ShuELourençoLMandelMMarinoRJrThe value of cranial computed tomography in high-risk, mildly head-injured patientsSurg Neurol200665Suppl 11011
- CullottaVPSementilliMEGeroldKClinicopathological heteronegenity classification of mild head injuryNeurosurgery1996382452508869050
- ServadeiFCiucciGLoroniLCusciniMPiolaCAristaADiagnosis and management of minor head injury: A regional multicenter approach in ItalyJ Trauma1995396967017473958
- KingNSPost-concussion syndrome: Clarity amid the controversy?Br J Psychiatry200318327627814519601
- CoetzerBRManagement of post-concussion syndromeBr J Psychiatry2004184868714702238