Abstract
Introduction:
Statin therapy is a well established treatment for hyperlipidemia. However, little is known about prescribing of statins for primary prevention in the real world, and even less about what happens to patients requiring primary prevention who are seen in a secondary care setting. The purpose of this research was to investigate the appropriateness of statin prescriptions by using the Joint British Society cardiovascular disease (JBS CVD) risk score for primary prevention in a large secondary care center.
Methods:
We retrospectively analyzed 500 consecutive patients in whom a statin prescription was initiated over a four-month period. We excluded patients who met secondary prevention criteria. We used the JBS CVD risk prediction chart to calculate 10-year composite risk. We also studied which statins were prescribed and their starting doses.
Results:
Of 500 patients consecutively started on statins in secondary care, 51 patients (10.2%) were treated for primary prevention. Of these, seven (14%) patients had a 10-year composite cardiovascular event risk of more than 20% (high-risk category), and were hence receiving appropriate therapy. Three main statins were prescribed for primary prevention, ie, atorvastatin (22 patients, 43%), simvastatin (25 patients, 49%), and pravastatin (four patients, 8%). The statins prescribed were initiated mainly at the 40 mg dose.
Conclusions:
Statin prescribing in secondary care for primary prevention is limited to about 10% of initiations. There is some overprescribing, because 86% of these patients did not require statins when risk-stratified appropriately. The majority of the prescriptions were for simvastatin 40 mg and atorvastatin 40 mg.
Introduction
Statin therapy is a well established treatment for hyperlipidemia. In the UK, the Joint British Society (JBS) has developed national guidelines on prevention of cardiovascular disease (CVD) in clinical practice. In these guidelines, the JBS has taken account of scientific evidence from both epidemiologic and randomized controlled studies, and preference has been given to evidence that is based on systematic reviews or meta-analyses rather than single observational studies or trials. The guidelines help to risk-stratify patients who will benefit most from drug therapy.Citation1
Total CVD risk for an asymptomatic individual is estimated from several risk factors, ie, age, gender, smoking habit, systolic blood pressure, and ratio of total cholesterol (TC) to high-density lipoprotein (HDL) cholesterol. This is expressed as a probability (percentage chance) of developing CVD over a defined period of time, which in the JBS guideline is calculated over 10 years. The logic for estimating total CVD risk based on major risk factors is that CVD is multifactorial in origin, risk factors tend to cluster, and coexistent risk factors tend to have a multiplicative effect on CVD risk.Citation2
According to the JBS, statin therapy in the CVD risk range of 10%–20% is appropriate on the basis of scientific evidence, although absolute benefits will be small. When the CVD risk is <10% over the next 10 years, the benefit of treatment is not established and may be too small in absolute terms to justify drug treatment. However, recommendations for a healthy lifestyle are still important.
Various primary prevention trials have used mainly pravastatin 20–40 mg (West Of Scotland Coronary Prevention Study, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial [ALLHAT]), lovastatin 20–40 mg (Air Force/Texas Coronary Atherosclerosis Prevention Study), and Atorvastatin10 mg (Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm [ASCOT-LLA]).Citation3–Citation6 These statins at the doses mentioned earlier have similar clinical efficacy.Citation7 Of note, the number needed to treat was 250 with ALLHAT and 91 with ASCOT. The Heart Protection Study used simvastatin 40 mg and included patients needing both secondary and primary prevention.Citation8 The proportional reduction in event rate was similar (and significant) in both groups. Recently, the Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese trial of primary prevention showed reduction of primary events by 33% in Japanese patients treated with low-dose pravastatin 10–20 mg.Citation9
Little is known about real-world prescribing in primary prevention, and even less about what happens to patients requiring primary prevention in a secondary care setting. The aim of this study was to investigate statin prescriptions for primary prevention in a large secondary care center.
Methods
We retrospectively analyzed 500 consecutive patients who were prescribed statins over a four-month period. We excluded patients who met secondary prevention criteria. This group included anyone who had an acute coronary syndrome, a cerebrovascular event, or transient ischemic attack, and patients with diabetes and ischemic heart disease. From electronic records and case notes, we collected data for gender, age, TC, HDL, blood pressure, and history of smoking. We used the JBS CVD risk prediction chart to calculate the 10-year composite risk for each patient.
The JBS recommends intervention with lipid-lowering drug therapy in asymptomatic patients with known atherosclerotic disease, CVD risk ≥20% over 10 years, diabetes, and/or particularly elevated single risk factors.
Statin therapy is recommended for diabetic patients over 40 years of age, those aged 18–39 years with retinopathy, nephropathy, poor glycemic control (ie, glycosylated hemoglobin >9%), elevated blood pressure requiring antihypertensive therapy, raised TC (≥6.0 mmol/L), features of metabolic syndrome (central obesity and fasting triglycerides >1.7 mmol/L [non-fasting >2.0 mmol/L], and/or HDL cholesterol <1.0 mmol/L in men or <1.2 mmol/L in women), and/or a family history of premature CVD in a first-degree relative.
Patients with particularly elevated single risk factors also require CVD prevention. This is because they too are at high cardiovascular risk, regardless of the presence of other risk factors. This includes patients with an elevated TC/HDL cholesterol ratio of ≥6.0 and those with familial dyslipidemia, such as familial hypercholesterolemia or familial combined hyperlipidemia.
It was assessed whether statin therapy was initiated according to JBS guidelines, in addition to the type of statins used and their starting doses.
Statistical analysis
We obtained quantitative results for initial analysis of data. We analyzed the data using one-way analysis of variance (ANOVA) statistics to calculate P values and confidence intervals (CI).
Results
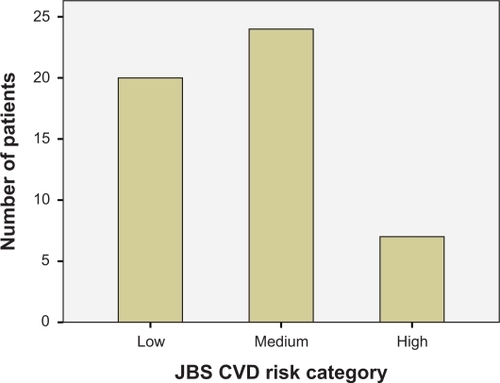
Five hundred consecutive patients were started on statins in secondary care and 51 (10.2%) of these patients were treated for primary prevention (). Of these, seven patients (14%) had a 10-year composite cardiovascular event risk of more than 20% (high-risk category) and hence were receiving appropriate therapy. No patients had significant hyperlipidemia requiring treatment without consulting the JBS charts. The basic demographic characteristics of patients are presented in the .
Table 1 Baseline characteristics of patientsTable Footnote*
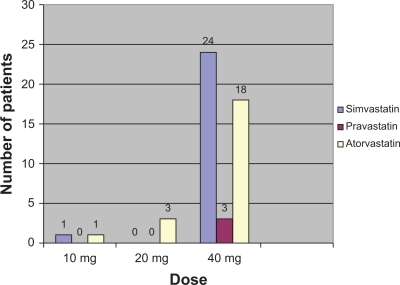
Three main statins were prescribed, ie, atorvastatin (22 patients, 43%), simvastatin (25 patients, 49%), and pravastatin (four patients, 8%). Twenty of 22 of those on atorvastatin were at low or medium JBS risk. Twenty of the 25 patients who were on simvastatin were at equally low or medium JBS risk. Only seven patients were in the high-risk category, and none of these patients were on pravastatin. The CI for mean JBS risk score was overlapping for the three statins used (atorvastatin 95% CI: 7.3–12.4, simvastatin 96% CI: 10.0–21.1, pravastatin 95% CI: 1–24). ANOVA analysis also did not show any significant relationship between JBS risk category and statin used (P = 0.252). The preferred starting dose of all statins was 40 mg (n = 45), 20 mg (n = 4), and 10 mg (n = 2) (). Atorvastatin 40 mg was the most potent and highest starting dose used for primary prevention.
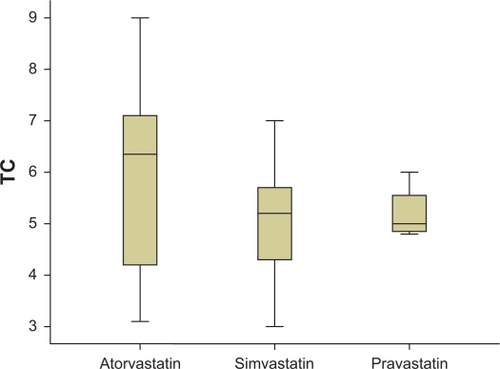
Mean TC levels among patients prescribed all three drugs were similar (atorvastatin 5.9 ± 1.6, simvastatin 5.1 ± 1.2, pravastatin 5.2 ± 0.55, P > 0.05, ). TC levels were also similar for the different dosages of statins (P > 0.05). On further analysis of the data, we noticed that patients whose TC levels were ≤6 mmol (n = 34) received simvastatin (n = 21, 61%), atorvastatin (n = 9, 26%), and pravastatin (n = 4, 11%). Patients whose TC levels were >6 mmol (n = 17) received atorvastatin (n = 13, 76%) and simvastatin (n = 4, 24%).
Discussion
This study shows that statin prescriptions for primary prevention in secondary care vary with dose and choice of statin. A preference for atorvastatin and simvastatin in patients whose TC levels were >6 mmol was identified. This prescription tendency may be influenced by local guidelines for secondary prevention (Cheshire and Merseyside Cardiac Network), which actually suggest a starting dose of simvastatin at 40 mg (baseline cholesterol ≤6 mmol) and of atorvastatin at 40 mg (baseline cholesterol ≥6 mmol). These variations in prescribing may occur because there is no set guidance for starting or maintenance doses of statins for primary prevention.
The JBS CVD risk prediction charts or similar risk scoring tools should be used before initiating statins for primary prevention. This approach would not only identify the group of patients who would benefit most from statins but also limit side effects due to inappropriate use, and also have huge financial implications within the National Health Service. Future clinical trials to compare various statins and their optimum doses (also in various ethnic groups) for primary prevention are needed to improve the effectiveness of statin prescriptions for primary prevention.
Recommendations
Statin therapy for primary prevention should be offered to patients who are at increased risk of cardiovascular disease
The JBS CVD risk scoring system helps to risk-stratify asymptomatic patients who would benefit the most from treatment
Clinicians are keen to treat cholesterol to target levels; however, patients are not risk-stratified appropriately and may receive unnecessary treatment
Regional guidelines for secondary prevention appear to influence statin prescriptions for primary prevention
Clinicians appear to favor a higher starting dose of statin for primary prevention.
Conclusion
Only 14% of patients received statin therapy appropriately for primary prevention, and the rest of the prescriptions were issued to patients with a low to medium cardiovascular composite risk score. We noticed that the choice of statin and dosage were not related to TC levels or JBS CVS risk score. However, we identified a preference for atorvastatin and simvastatin in patients whose TC levels were >6 mmol. Clinicians in hospital medicine preferred a higher dose of statins for primary prevention. We noticed an influence of secondary prevention guidelines in primary prevention prescriptions, which could potentially lead to more side effects and noncompliance with statins, especially in a group of patients who are otherwise healthy.Citation10
Disclosure
The authors report no conflicts of interest in this work.
References
- British Cardiac Society, British Hypertension Society, Diabetes UK, HEART UK, Primary Care Cardiovascular Society, The Stroke Association JBS 2Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practiceHeart20059115215604317
- AndersonKMOdellPMWilsonPWFCardiovascular disease risk profilesAm Heart J19901212932981985385
- ShepherdJCobbeSMFordIPrevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study GroupN Engl J Med1995333130113077566020
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research GroupThe antihypertensive and lipid-lowering treatment to prevent heart attack trial. Major outcomes in moderately hypercholesterolemic, hypertensive people randomized to pravastatin vs usual care: The antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT-LLT)JAMA20022882998300712479764
- DownsJRClearfieldMWeisSPrimary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: Results of AFCAPS/TexCAPS. Air Force/Texas coronary atherosclerosis prevention studyJAMA1998279161516229613910
- SeverPSDahlofBPoulterNRPrevention of coronary and stroke events with atorvastatin in hypertensive people who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian cardiac outcomes trial – lipid-lowering arm (ASCOT-LLA): A multicentre randomised controlled trialLancet20033611149115812686036
- Third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final reportCirculation20021063143342112485966
- Heart Protection Study Collaborative GroupMRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: A randomised placebo-controlled trialLancet200236072212114036
- NakamuraHArakawaKItakuraHPrimary prevention of cardiovascular disease with pravastatin in Japan (MEGA study): A prospective randomized controlled trialLancet20063681155116317011942
- EscobarCEcharriRBarrioVRelative safety profiles of high dose statin regimensVasc Health Risk Manag2008452553318827903