Abstract
Objective
The aim of this study was to determine the in-hospital survival of patients referred to the 2 stroke centers in North-West of Iran during a full seasonal year from April 2015.
Methods
All the consecutive patients with stroke admitted to the 2 main stroke centers at Tabriz (Imam Reza University Hospital and Razi University Hospital) were recruited in this study. Stroke patients from both ischemic and hemorrhagic subtypes were selected based on the registry data and International Classification of Diseases, 10th edition. At admission, details of examination including vital signs, neurologic and systemic examination, Modified Rankin Scale, and Glasgow Coma Scale were recorded. Baseline hematological and biochemical parameter assessments as well as computerized tomographic scanning were conducted. Cox regression was used to investigate and detect potential predictors of in-hospital survival.
Results
A total of 1,990 patients with stroke were studied. Males comprised 52.1% (1,036) of the subjects. The mean age of the patients was 65.8 years. Three hundred and fifty-seven (17.9%) patients had hemorrhagic stroke vs 1,633 (82.1%) with ischemic stroke. In-hospital case-fatality proportion was 12.5% (95% CI: 11.1–14). Based on modified Rankin Scale score at admission, 1,377 of 1,990 patients (69.2%) had a poor outcome (modified Rankin Scale score ≥3) at the admission time. The regression analysis showed that at least 7 variables could independently predict hospital survival of patients with stroke including age ≥65 years, higher admission modified Rankin Scale score, lower admission Glasgow Coma Scale score, hemorrhagic stroke nature, diabetes, having valvular heart disease, and having aspiration pneumonia.
Conclusion
The case-fatality of stroke in the present study setting is high and needs to be appropriately addressed through prevention or management of some of these factors such as diabetes, pneumonia, and valvular heart diseases.
Introduction
Stroke is a serious neurologic disease leading to disability and death worldwide. Stroke is the fifth most common cause of mortality and a prominent cause of disability in the United States.Citation1 Hemorrhagic stroke ranks the highest with respect to in-hospital fatality among stroke subtypes, with a range of about 24%–28% reported based on various studies.Citation1–Citation3 It is also considered a major public health problem with high morbidity and mortality in low- and middle-income countries, including Iran, with rates exceeding that in high-income countries.Citation4–Citation8
Although, hospitalization, especially in stroke-designated centers, has been shown to improve the prognosis of stroke, it is quite vital to improve stroke outcomes and survival through depicting the role of stroke predictors especially those that can be manipulated for this purpose.Citation9–Citation11 Stroke mortality, especially in-hospital mortality, is an outstanding indicator in stroke care and control. In-hospital mortality of stroke reflects the efficiency of medical care for this disease. Stroke promotion programs worldwide focus on the reduction of morbidity and mortality of this disease, particularly the in-hospital mortality. In order to achieve this goal, it is recommended that the time of delivery of stroke care be shortened as much as possible. Moreover, the quality of care of stroke, including thrombolysis and thrombectomy, as the most updated approved treatment needs to be improved.Citation2,Citation12–Citation16 In line with the everyday developing programs of stroke care promotion, identifying in-hospital mortality predictors and their integration could advance stroke medical care further.
The studies investigating epidemiology, risk factors, and outcomes of stroke which are conducted based on quality registries from low- and middle-income countries including Iran are scarce.Citation6,Citation17–Citation20 This is crucial because hospital fatality or its predictors or at least the magnitudes of effect sizes of potential predictors could vary in different populations. Although some studies have been conducted comparing stroke mortality over some potential predictors, due to lack of comprehensive assessments of potential predictors such as the situation in stroke registries, there is a need for prognostic studies using appropriate data while capturing natural variations in stroke distributions over time, location, and a comprehensive set clinical and paraclinical investigations including stroke severity surrogates. The implementation of the Tabriz pilot national stroke registry in Iran has provided such an opportunity. The aim of this study, as the first analytical report from Tabriz Stroke Registry (TSR), was to determine the in-hospital survival of patients referred to the 2 stroke centers in North-West of Iran during a full seasonal year from April 2015.
Methods
This study enrolled patients with stroke registered between April 2015 and April 2016 in the stroke registry of East Azerbaijan Province of Iran named TSR.
Prospective ascertainment of cases was carried out by a combined hot and cold pursuit of admitted patients hospitalized with diagnosis of stroke to any of the wards in the involved hospitals. Case definition in TSR is based on the current World Health Organization definition of stroke as “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours (unless interrupted by surgery or leading to death), with no apparent cause other than that of vascular origin.”Citation21 Stroke patients from both ischemic and hemorrhagic subtypes were selected based on the registry data and International Classification of Diseases, 10th edition nomenclature.
Diagnosis was recorded based on International Classification of Diseases, 10th edition categorization, as one of 3 types including ischemic stroke, hemorrhagic stroke, or other diagnosis. Subtypes were also recorded including thrombotic stroke (and the involved vessel) or embolic stroke (and the source of emboli) as subtypes of ischemic stroke, intracerebral hemorrhage or intraventricular hemorrhage or subarachnoid hemorrhage as subtypes of hemorrhagic stroke, or stroke of uncertain type as subtypes of the other diagnosis.
This explanation was added to the main text and highlighted.
The registry data collection was started from 2015 regularly, consecutively, and in the paper-based manner, and has been continued since then. The paper-based manner was later transferred to a software platform specifically designed for this registry. The full registry collects data on over 150 elements, including demographic information, clinical findings, primary imaging and lab findings, history of risk factors, drug history, discharge, follow-up, stroke severity indicators, complications, and delivered treatments. Data collection occurs at 3 phases: admission, discharge, and follow-up. Details of Tabriz stoke registry are given elsewhere [Design and Implementation of Tabriz Stroke Registry, unpublished data, 2017]. Parts of the registry elements approved to be included in present research form part of a PhD degree thesis project at Tabriz Neuroscience Research Center for the time period up to discharge or death at the hospital.
All the consecutive patients with stroke admitted to the 2 main stroke centers at Tabriz (Imam Reza University Hospital and Razi University Hospital) were registered and consequently recruited in this study.
Trained abstractors, who were educated physicians, reviewed the primary data for each case recorded in the hospital, then they visited the patients and data collection was continued afterwards. Data were further completed on discharge, and then after 3-month follow-up.
A detailed medical history of the condition presentation including headache, vomiting, seizures, loss of consciousness, and focal neurological deficits was obtained and a history of risk factors was taken. At admission, details of examination including vital signs, systemic examination, Modified Rankin Scale (mRS), and Glasgow Coma Scale (GCS) were recorded. Baseline hematological and biochemical parameter assessments as well as computerized tomographic scanning were conducted. The primary outcome of interest in present study was either death or survival within the hospital.
Statistical analysis
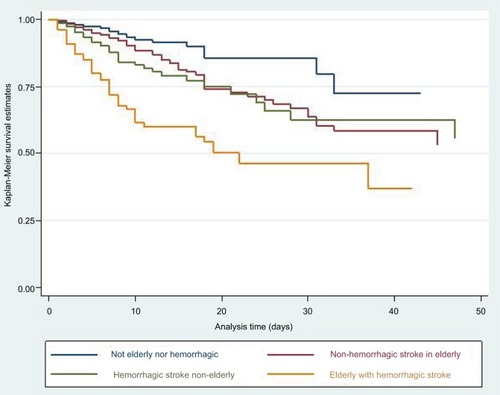
Data analysis was conducted using STATA version 14 statistical software package (StataCorp LLC, College Station, TX, USA). Both descriptive and analytical methods were applied. Kaplan–Meier survival graphs were produced to compare survival rates between various conditions. Multiple semi-parametric Cox regression model was used to investigate and detect potential predictors of in-hospital survival, and hazard ratios along with their 95% CIs were reported. The proportional hazard assumption was checked and confirmed to hold. A P-value below 0.05 was considered statistically significant.
Ethical considerations
The study was approved as part of a PhD thesis project by the research committee and regional ethics committee at Tabriz University of Medical Sciences.
During admission, patients gave their written informed consent to transfer their data into academic databases including registries. Throughout data collection, no further interventions or tests were defined other than the routine clinical procedures of the hospital, and thus additional consent taking was not required. Moreover, the administrative processes in the TSR included identity protection, and therefore access to the identity information of the patients in the registry is highly restricted. All the data included in this manuscript are deidentified.
Results
A total of 1,990 patients with stroke were studied. Males comprised 52.1% (1,036) of the subjects. The mean age was 65.8 years with SD of 14.8. The mean age for male patients was 66.3 years (SD =14.4) and for female patients was 65.3 years (SD =15.3) with no significant difference (P=0.1). The other demographic data of patients are presented in .
Table 1 Demographic data of recruited cases and P-value for mortality prediction
With respect to the type of stroke, 357 (17.9%) were hemorrhagic vs 1,633 (82.1%) with ischemic stroke. In 93.5% of the subjects, the symptoms were identified at home.
The baseline admission values of some blood bioassays are given in , compared for males and females.
Table 2 Blood bioassay results of patients with stroke between males and females
Median GCS scores of the patients at admission were 13.8 and 15, respectively (interquartile range =1). A GCS below 13 was observed in 18%, and a GCS below 10 was observed in 9.3% of the participants. Mean mRS scores of the patients at admission were 3.3 (SD =1.4).
It was shown that those with diabetes mellitus were 1.8 times more likely to have ischemic stroke rather than hemorrhagic stroke (odds ratio =1.81, 95 CI: 1.4–2.4).
In-hospital case-fatality proportion was 12.5% (95% CI: 11.1–14). The case-fatality was 25.1% and 1.7% for Imam Reza and Razi University hospitals, respectively (). Based on mRS at admission, 1,377 of 1,990 patients (69.2%) had a poor outcome (mRS ≥3) at the admission time.
Table 3 In-hospital mortality statistics according to the stroke type, age group, and center
The multiple Cox regression analysis showed that at least 7 variables could independently predict hospital survival of patients with stroke. The elderly (≥65 years) were 1.6 times more likely to die during hospitalization. Higher admission mRS scores, lower admission GCS score, hemorrhagic stroke nature, diabetes, having valvular heart disease, and having aspiration pneumonia increased the risk of hospital mortality (). Diagnosis of aspiration pneumonia was based on positive sputum culture, which was requested when the medical team suspected pneumonia based upon the clinical presentations.
Table 4 Results from TSR of multiple regression analysis to determine independent predictors of in-hospital stroke mortality
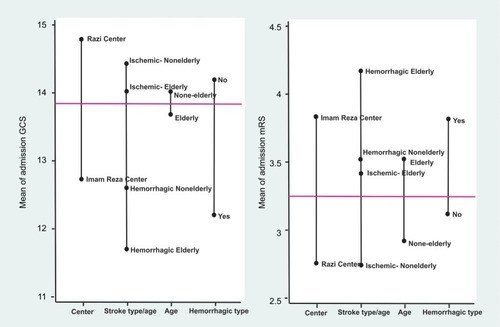
Mean scores of mRS and GCS at admission time, as the surrogates of stroke severity, were compared for different variables, and the results are shown in . compares the survival graphs for age group and stroke type. The elderly (≥65 years) patients with hemorrhagic stroke had a hazard ratio of hospital mortality equal to 2.4 (95% CI: 1.5–3.6) when compared to those with ischemic stroke and age under 65 years, after controlling for other factors included in the model.
Discussion
In line with the findings of the previous studies, we found that, in-hospital case-fatality in patients admitted with stroke was associated with higher age, stroke severity, stroke nature (type), and some medical conditions and comorbidities.
Cox multiple regression analyses showed that increasing age, higher admission mRS scores, lower admission GCS score, hemorrhagic stroke nature, diabetes, having valvular heart disease, and having aspiration pneumonia increased the risk of hospital mortality, each being independent predictors of survival. Gender and smoking, although considered as survival predictors in some studies, were not found to affect the survival of patients admitted with stroke while controlling for their potential effect in multivariate model. These did not also show they could confound the effect of other potential predictors of in-hospital survival. However, it should be taken into account that our study only aimed at short-term survival. A stroke cohort assessing 10-year survival of stroke patients found that adjusting for age, stroke severity, stroke type, and risk factors, females had a higher probability of survival at 1-, 5-, and 10-year follow-ups but no such a difference could be explored 9 months post-stroke concluding that short-term survival of stroke is not affected by gender.Citation22 The time dependency of gender effect on stroke has also been reported by Olsen et alCitation23 through a very recent Danish study; nevertheless, they believed that female/male stroke mortality rate favors females from the first month of stroke while reversing over the second month in favor of males, then back to female survival advantage afterwards.
Similarly, the effect of smoking on long-term survival is reported in some studiesCitation24–Citation28 mostly assessing long-term survival, such as the one by Kim et alCitation28 from Canada who found that patients with stroke who smoked at the time of their stroke or prior to that had higher risk of mortality when compared with patients who were never smokers. However, this should be interpreted with caution due to the fact that at least part of such mortality may be due to higher risk of recurrence of stroke among smokers over the long period of assessment for long-term survival. Although smoking is used by the iScore, well-conducted studies based on American stroke registry on stroke patients with thrombolytic therapy did not find smoking to be associated with in-hospital mortality.Citation29 Another argument to be considered in the discussion regarding the association of smoking with stroke fatality is that the effect of smoking on survival may be confounded by stroke severity. In the present study, mRS and GCS at admission time were included as indicators of stroke severity in a multivariate model finding no independent role for smoking on short-term survival. Similarly, a large study with above 16,000 stroke patients in Denmark which had included the National Institute of Health Stroke Scale in multivariate analysis has not reported the smoking as an independent stroke survival predictor.Citation30
It has been commonly stated by many studies that increasing age is an independent risk factor for in-hospital death, however, some studies have assumed the effect of age to be more especially for the elderly (≥65 years), but it could not be independently associated with poor outcome (mRS ≥3) assessed through mRS score at discharge.Citation29,Citation31 Although age may possess an effect through increased severity of stroke assessed by GCS and mRS scores as early outcomes, our study showed that even after controlling for baseline GCS, mRS scores, as well as comorbid conditions, age ≥65 years increased the risk of hospital mortality by 55%. A study from Cameroon with a similar design and analysis methodology to ours and including both ischemic and hemorrhagic stroke found that only the GCS, hyperglycemia, and the hemorrhagic nature of the stroke were found to be independent predictors of in-hospital survival and that age was not found to be an independent predictor of survival.Citation32 The mentioned study has the statistical power limitation due to low sample size. However, the current investigation incorporated a sample size approximately six times higher, and this could provide more statistical power for detection of predictors.
Our study showed that admission GCS and mRS scores are potent predictors of in-hospital survival. In case of hemorrhagic stroke, it has been shown that even assessing easily measurable levels of consciousness can have much higher predictive power than imaging predictors such as estimating the hemorrhage volume through computerized tomography or transcranial Doppler sonography examination in stroke patients.Citation33,Citation34
Acute stroke case-fatality rates can be used as a quality indicator for acute stroke treatment, but after taking into account the potential confounders.Citation35 One such a confounding factor could be severity indicators such as mRS and GCS at admission.
Imam Reza center is the referral designated stroke center in the northwest of Iran. It has been shown that regardless of the individual predictors of in-hospital mortality, being admitted to a designated stroke center could improve survival after intracerebral hemorrhage.Citation3 The overall case-fatality proportion was 12.5% in current study. It reached up to 25.1% in Imam Reza University Hospital vs only 1.7% in Razi University Hospital. This is expected due to the severity confounding effect. Imam Reza University Hospital is a referral center that admits severe stroke cases, and those who come with a less severe condition are usually referred to Razi University Hospital. This means that severity status is associated with hospital selection, and thus considering the known association between severity and fatality, a confounding effect exists; therefore, the lower case-fatality proportions at Razi cannot be attributed to its higher quality of care. The case-fatality in Imam Reza University Hospital was nearly 5 times that of the study in Denmark; however, about 90% of the patients referred to it had a moderate-to-severe status vs about 50% in the Danish study.Citation30 Other major factors to be taken into account in interpreting and comparing case-fatality rates could be age distribution and comorbidities.
Although the current study has assessed the predictors of in-hospital survival which are considered for short-term prognosis, it has been demonstrated that short-term and long-term stroke case-fatality share many common predictors.Citation36
We found several medical conditions affecting the likelihood of stroke survival. Although some predictors of stroke are difficult to be prevented, medical conditions such as pneumonia can be dealt with high priority in stroke centers. Actually, it has been stated that the majority of improvement in stroke prognosis could be attributed to better prevention or management plans for complications in recent decades.Citation37
Conclusion
The case-fatality of stroke in present study setting is high and needs to be appropriately addressed through prevention or management of some of these factors such as diabetes, pneumonia, and valvar heart diseases.
Acknowledgments
We thank the hospital staff of the academic and nonacademic hospitals in Tabriz for their cooperation in data collection for the Tabriz Stroke Registry. We also thank Dr M Zamanlu for her kind cooperation in the Tabriz Stroke Registry project.
Disclosure
The authors report no conflicts of interest in this work.
References
- MozaffarianDBenjaminEJGoASHeart disease and stroke statistics – 2015 update: a report from the American Heart AssociationCirculation20151314e29e32225520374
- SmithEEShobhaNDaiDA risk score for in-hospital death in patients admitted with ischemic or hemorrhagic strokeJ Am Heart Assoc201321e00520723525444
- GatollariHJColelloAEisenbergBDesignated stroke center status and hospital characteristics as predictors of in-hospital mortality among hemorrhagic stroke patients in New York, 2008–2012Cerebro-vasc Dis2017431–24353
- AbegundeDOMathersCDAdamTOrtegonMStrongKThe burden and costs of chronic diseases in low-income and middle-income countriesLancet200737096031929193818063029
- Dehghani FiroozabadiMKazemiTSharifzadehGDadbehSDehghanPStroke in Birjand, Iran: a hospital-based study of acute strokeIran Red Crescent Med J201315326426823984011
- DaneshfardBIzadiSShariatAToudajiMABeyzaviZNiknamLEpidemiology of stroke in Shiraz, IranIran J Neurol201514315816326622981
- ThriftAGArabshahiSIs stroke incidence in low- to middle-income countries driven by economics?Int J Stroke20127430730822583522
- FowkesFGRudanDRudanIComparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysisLancet201338299011329134023915883
- BhallaADundasRRuddAGWolfeCDDoes admission to hospital improve the outcome for stroke patients?Age Ageing200130319720311443020
- JacobsBSBakerPLRoychoudhuryCMehtaRHLevineSRImproved quality of stroke care for hospitalized Medicare beneficiaries in MichiganStroke20053661227123115879336
- TammASiddiquiMShuaibAImpact of stroke care unit on patient outcomes in a community hospitalStroke201445121121624253547
- PatelMDRoseKMO’BrienECRosamondWDPrehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina stroke care collaborativeStroke20114282263226821659638
- KidwellCSStarkmanSEcksteinMWeemsKSaverJLIdentifying stroke in the field: prospective validation of the Los Angeles Prehospital Stroke Screen (LAPSS)Stroke2000311717610625718
- NogueiraRGLiebeskindDSSungGDuckwilerGSmithWSMERCIMulti MERCI Writing CommitteePredictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and multi MERCI trialsStroke200940123777378319875740
- LahrMMHOrganizational Models for Thrombolysis in Acute Ischemic Stroke: A Simulation Exemplar [thesis]Groningen, NetherlandsUniversity of Groningen Library2013133
- PikijaSCvetkoDMalojčićBA population-based prospective 24-month study of stroke: incidence and 30-day case-fatality rates of first-ever strokes in CroatiaNeuroepidemiology201238316417122473420
- FarhoudiMMehrvarKSadeghi-BazarganiHStroke subtypes, risk factors and mortality rate in northwest of IranIran J Neurol201716311211729114365
- Borhani-HaghighiASafariRHeydariSTHospital mortality associated with stroke in southern IranIran J Med Sci201338431432024293785
- AlmekhlafiMATrends in one-year mortality for stroke in a tertiary academic center in Saudi Arabia: a 5-year retrospective analysisAnn Saudi Med201636319720227236391
- BhattacharyaSSahaSPBasuADasSKA 5 years prospective study of incidence, morbidity and mortality profile of stroke in a rural community of eastern IndiaJ Indian Med Assoc20051031265565916821657
- World Health OrganizationCerebrovascular diseases: prevention, treatment, and rehabilitation: Monaco WHO meeting reportGenevaWorld Health Organization1971
- AndersenMNAndersenKKKammersgaardLPOlsenTSSex differences in stroke survival: 10-year follow-up of the Copenhagen stroke study cohortJ Stroke Cerebrovasc Dis20051452152017904029
- OlsenTSDehlendorffCAndersenKKSex-related time-dependent variations in post-stroke survival – evidence of a female stroke survival advantageNeuroepidemiology2007293–421822518075278
- OksalaNKHeikkinenMMikkelssonJSmoking and the platelet fibrinogen receptor glycoprotein IIb/IIIA PlA1/A2 polymorphism interact in the risk of lacunar stroke and midterm survivalStroke2007381505517138951
- KammersgaardLPSurvival after stroke. Risk factors and determinants in the Copenhagen Stroke StudyDan Med Bull20105710B418921040687
- ErikssonMNorrvingBTeréntAStegmayrBFunctional outcome 3 months after stroke predicts long-term survivalCerebrovasc Dis200825542342918349536
- CorreiaMMagalhãesRSilvaMRMatosISilvaMCStroke types in rural and urban northern Portugal: incidence and 7-year survival in a community-based studyCerebrovasc Dis Extra2013311374924348498
- KimJGallSLDeweyHMMacdonellRASturmJWThriftAGBaseline smoking status and the long-term risk of death or nonfatal vascular event in people with stroke: a 10-year survival analysisStroke201243123173317823103491
- TongXGeorgeMGYangQGillespieCPredictors of in-hospital death and symptomatic intracranial hemorrhage in patients with acute ischemic stroke treated with thrombolytic therapy: Paul Coverdell Acute Stroke Registry 2008–2012Int J Stroke20149672873424024962
- KoenneckeHCBelzWBerfeldeDFactors influencing in-hospital mortality and morbidity in patients treated on a stroke unitNeurology2011771096597221865573
- SaposnikGKapralMKLiuYIScore: a risk score to predict death early after hospitalization for an acute ischemic strokeCirculation2011123773974921300951
- MapoureNYTchaleu NguenkamCBMbatchou NgahaneHBPredictors of in-hospital mortality for stroke in Douala, CameroonStroke Res Treat2014201468120924724038
- Savadi-OskoueiDSadeghi-BazarganiHHashemilarMDeAngelisTSymptomatologic versus neuroimaging predictors of in-hospital survival after intracerebral haemorrhagePak J Biol Sci201013944344720973398
- VajargahKFSadeghi-BazarganiHMehdizadeh-EsfanjaniRSavadi-OskoueiDFarhoudiMOPLS statistical model versus linear regression to assess sonographic predictors of stroke prognosisNeuropsychiatr Dis Treat2012838739222973104
- HeuschmannPUBieglerMKBusseODevelopment and implementation of evidence-based indicators for measuring quality of acute stroke care: the Quality Indicator Board of the German Stroke Registers Study Group (ADSR)Stroke200637102573257816960092
- SaposnikGHillMDO’DonnellMVariables associated with 7-day, 30-day, and 1-year fatality after ischemic strokeStroke20083982318232418566303
- EvansAPerezIHarrafFCan differences in management processes explain different outcomes between stroke unit and stroke-team care?Lancet200135892931586159211716885