Abstract
Clinic blood pressure (BP) is recognized as the gold standard for the screening, diagnosis, and management of hypertension. However, optimal diagnosis and successful management of hypertension cannot be achieved exclusively by a handful of conventionally acquired BP readings. It is critical to estimate the magnitude of BP variability by estimating and quantifying each individual patient’s specific BP variations. Short-term BP variability or exaggerated circadian BP variations that occur within a day are associated with increased cardiovascular events, mortality and target-organ damage. Popular concepts of BP variability, including “white-coat hypertension” and “masked hypertension”, are well recognized in clinical practice. However, nocturnal hypertension, morning surge, and morning hypertension are also important phenotypes of short-term BP variability that warrant attention, especially in the primary-care setting. In this review, we try to theorize and explain these phenotypes to ensure they are better understood and recognized in day-to-day clinical practice.
Background
Hypertension, one of the most important preventable causes of death globally, accounts for more than 12.8% of all deaths annually.Citation1,Citation2 Elevated blood pressure (BP) is one of the major modifiable contributing factors to cardiovascular risk; however, there is often uncertainty as to the “true underlying BP”, as patients often present with discrepant BP readings.Citation3 This is because BP is a continuous variable that fluctuates constantly in response to various changes in physical and mental activities, sleep, and autonomic, humoral, mechanical, myogenic and environmental stimuli.Citation4 It is characterized by marked spontaneous oscillations over short- and long-term periods.Citation5 As such, clinic BP or home BP (HBP) in an individual at one time can be considerably different from his/her average day and nighttime BP.Citation4 This presents a challenge in diagnosing and prescribing treatments for patients correctly.
Physiology of relationship between sleep and BP regulation
Sleep usually involves calmness and detachment from the external environment, and hence generally causes a reduction in BP at night.Citation6 This decrease does not occur under conditions of total sleep deprivation. Sleep disturbances, including sleep restriction, sleep apnea, insomnia, and shift work, have also been found to induce stress on the cardiovascular system and play a role in the development of cardiovascular disorders.Citation7 The sleep-dependent changes in BP are specific to each sleep state, and result from the integration between cardiovascular reflexes (which modulate heart rate in response to changes in BP) and central autonomic commands to heart and resistance vessels.Citation6,Citation8 The pathophysiological mechanisms behind these clinical associations probably alter the integration of these cardiovascular reflexes and central autonomic commands.Citation6 A positive beneficial association has been found between “close relationships” and BP dipping, while posttraumatic stress disorder and obstructive sleep apnea have been associated with diminished nocturnal BP fall.Citation9–Citation11
Blood-pressure variability
Even though average clinic BP values remain the gold standard for the diagnosis and treatment of hypertension, recent studies in hypertensive subjects have demonstrated that the assessment and quantification of BP variability (BPV) in addition to normal BP values, is of both physiopathological and prognostic importance.Citation2,Citation12 For instance, there is strong evidence to show that increased BPV is independently associated with higher risk of target-organ damage, cardiovascular events, and mortality.Citation2,Citation5,Citation13 It follows that controlling BPV in addition to reducing absolute BP levels may contribute to optimal cardiovascular protection in hypertensive patients.Citation14
Continuous intra-arterial BP recordings are used to assess very short-term beat-to-beat changes in BPV, whereas continuous monitoring systems, such as ambulatory BP monitoring (ABPM), are used for assessing short-term BP fluctuations within a day (24 hours). On the other hand, home BP monitoring (HBPM) or office BP monitoring (OBPM) over lengthy time periods are used to detect long-term changes in BP stretching over days or visits.Citation2,Citation15
Some studies have observed that the extent of BPV is directly proportional to mean BP values, and hence BPV is generally higher in hypertensive subjects compared to normotensive subjects.Citation16 It is also noted that a reduction in mean BP values leads to a proportional reduction in BPV, and thus it has been suggested that employment of longer-acting BP-lowering drugs might be particularly beneficial in controlling BPV in addition to BP control.Citation16 However, setting the optimal therapeutic target for BPV control with antihypertensive therapy remains a challenge.Citation14
Different types of BPV
Popular concepts of BPV, such as “white-coat hypertension” and “masked hypertension”, are well recognized in clinical practice, and have been studied extensively for their prognostic relevance.Citation13 White-coat hypertension or isolated office hypertension is characterized by elevated office BP (OBP) with normal ambulatory BP (ABP) or HBP, and might be caused by anxiety or in response to an unusual clinical setting.Citation17,Citation18 Masked hypertension, on the other hand, is characterized by normal OBP, even though ABP or HBP levels are elevated.Citation19 However, it is important to recognize that BPV is a complex phenomenon that expands beyond such popular concepts, and is influenced by fluctuations in both the short term, ranging from seconds to hours, and the long term, ranging from days to months.Citation2,Citation5,Citation14 In general, BPV can be divided into three different types, based on the time frame it occurs: very short-term BPV, short-term BPV and long-term BPV.Citation2,Citation15 Depending on the method and time interval considered for its assessment, the clinical significance and prognostic implications of a given measure of BPV differ.Citation2,Citation14
Very short-term BPV
Very short-term BPV refers to beat-to-beat fluctuations in BP due to the interplay of different cardiovascular control systems, such as the baroreceptor reflex, the renin–angiotensin system, the vascular myogenic response, and the release of nitric oxide from the endothelium, as well as changes in behavioral and emotional mechanisms.Citation2,Citation5,Citation20 It is usually assessed in a laboratory via intra-arterial recording or under ambulatory conditions by noninvasive finger cuffs that continuously track finger-BP levels through infrared photoplethysmography.Citation2,Citation15 Standard deviations of BP values or fluctuations in BP obtained from spectral analyses at various frequency bands are often used as the main indices for assessing very short-term BPV.Citation2
Even though its usefulness and reliability in practical usage is questionable, very short-term BPV has been used as a tool in diagnosing and treating patients with cardiovascular disease, as well as to study the mechanism of action of anti-hypertensive drugs.Citation2,Citation20–Citation22 Detecting changes in beat-to-beat BPV can also help in rationally selecting antihypertensive drugs.Citation5 For instance, hypertensive patients with elevated low-frequency BPV may present with enhanced sympathetic modulation of vascular tone, and hence may respond well to sympatholytic antihypertensive drugs.Citation20
Short-term BPV
Short-term BPV refers to the BP changes that occur within a day (24 hours), and is characterized by normal circadian variations, such as nocturnal BP dipping and morning BP surge.Citation2,Citation14,Citation15,Citation23 It is mainly influenced by central neural factors, reflex autonomic modulation, and changes in the elastic properties of arteries and humoral systems and rheological and mechanical factors.Citation15,Citation24–Citation29 However, all these factors are often inextricably intertwined with each other.Citation14 Various studies have demonstrated that higher 24-hour BPV independently of mean BP values is clinically important, as this can increase cardiovascular (CV) events, mortality, and target-organ damage.Citation30–Citation37
Short-term BPV can be measured in two ways: using either ABPM to measure BP every 15–30 minutes over a 24-hour period or special HBPM devices that can measure BP while sleeping.Citation2,Citation14,Citation38,Citation39 Some common indices of measurement for short-term BPV include standard standard deviation (SD) of BP values measured over the whole 24-hour period, waking hours, or sleeping hours.Citation2 Other indices include coefficient of variation (CoV), 24-hour weighted SD, and average real variability (ARV).Citation2,Citation40–Citation42 These indices are covered in detail in “Understanding indices of short-term BPV” section. The main advantages of short-term BPV monitoring are that it can provide extensive information on BP changes over a day and detect important circadian BP changes, such as morning BP surge and nocturnal dipping, that may have important prognostic implications.Citation43–Citation47
Long-term BPV
Long-term BPV refers to day-to-day, visit-to-visit, and season-to-season BP changes.Citation2,Citation15 Factors contributing to long-term BPV remain relatively unclear.Citation2 Long-term BPV could be a consequence of poor BP control in treated patients, such as inadequate treatment by the physician, poor patient adherence, or improper BP-measurement methods.Citation2,Citation15 It may also be influenced by behavioral changes in an individual, as well as environmental factors, such as outdoor temperature and daylight-hour differences between different seasons.Citation2,Citation4,Citation15 For instance, BPV was found to be greater during winter than in summer, possibly due to increased sodium retention and vascular resistance caused by augmented sympathetic activity.Citation4 Some studies have also suggested that increased arterial stiffness contributes to the pathogenesis of long-term BPV.Citation5,Citation48
Day-to-day BPV can be assessed by ABPM over 48 hours or HBPM data collected over several days, weeks, or months, while visit-to-visit BPV is usually assessed by ABPM or OBPM that is usually spaced by visits over weeks, months, and years.Citation2,Citation15 However, the reliability of using OBPM to assess long-term BPV has been questioned, as it does not take into account the patient’s normal activities and requires frequent visits to the physician for BP measurements.Citation2,Citation15 A recent single-center cross-sectional study showed significant differences between single OBPM and means of consecutive BP measurements.Citation49 In-office measurements are also sometimes inaccurate, mainly because of the white-coat effect, inadequate or uncalibrated devices, and suboptimal measurement techniques (eg, incorrect cuff size, no rest before measurement).Citation50,Citation51 Although a large number of recommendations on correct OBPM techniques have been published (), these guidelines are generally not translated into primary-care practice.Citation51,Citation52
Table 1 Recommendations for OBP monitoring from key guidelines on hypertension
There is strong evidence to suggest that increased long-term BPV is associated with higher risk of stroke, cardiovascular events, and mortality, including all-cause mortality.Citation53–Citation57 Therefore, measuring long-term BPV might be clinically important, as it can provide useful insights into the long-term control of the patient’s BP and effectiveness of the patient’s current antihypertensive therapy.Citation2
Understanding short-term BP variability
Nocturnal dipping and nocturnal hypertension
BP generally dips about 10%–20% during sleep in normotensive patients, due to a phenomenon known as nocturnal dipping.Citation14,Citation15 However, in hypertensive patients, the extent of BP dipping can differ significantly, and individuals can be categorized into four groups based on the extent of fall in nighttime BP. These include extreme dippers, dippers, non-dippers, and reverse dippers.Citation15 In general, individuals whose BP falls in the range of 10%–20% are known as dippers.Citation58 Those who dip >20% are known as extreme dippers, while those exhibit <10% dip in BP are called nondippers. On the other hand, those who have an increase in nocturnal BP, instead of a fall, are known as “risers” or “reverse dippers”.Citation58 Various causes for the absence of dipping have been proposed including sleep disturbance, depression, obesity, obstructive sleep apnea, orthostatic hypotension, autonomic dysfunction, chronic kidney disease, diabetic neuropathy, and old age.Citation23,Citation59–Citation61
There is strong evidence indicating that such circadian variations have prognostic significance in both hypertensive and normotensive patients. For instance, blunted or reverse nocturnal BP dipping and exaggerated morning BP surge are independently associated with increased cardiovascular events, stroke, and target-organ damage.Citation4,Citation37,Citation43,Citation62–Citation77 These circadian variations within 24 hours can also give rise to other phenotypes of short-term BP variations, such as nocturnal hypertension and morning hypertension.Citation78,Citation79
Nocturnal hypertension is defined as having an average of nocturnal BP values of ≥ 120/70 mmHg and is generally caused by a failure in nocturnal dipping and hence usually observed in nondippers or reverse dippers.Citation59 It is especially important to control nocturnal BP, as it is more likely to represent the patient’s actual BP more closely, as it is often not influenced by the pressor effects of physical, emotional, and other environmental factors that occur during the day.Citation14 Moreover, patients with nocturnal hypertension have been found to be at significantly higher risk of organ damage and cardiovascular events, independently of OBP or morning BP values.Citation59,Citation64,Citation80–Citation82 Nocturnal BP has also been found to be a superior predictor of cardiovascular disease than daytime BP.Citation45,Citation83 Previously, nocturnal hypertension was able to be detected only by ABPM. However, development of novel semiautomatic HBPM devices that can intermittently measure BP during sleep have allowed HBPM to monitor nocturnal BP accurately.Citation59,Citation84–Citation87 Nocturnal HBP values obtained by such devices are comparable to nocturnal BP values obtained by traditional ABPM.Citation59,Citation85
Morning surge and morning hypertension
BP tends to surge higher in the morning, and this is considered a normal physiological process, but exaggerated morning BP surge has been observed in some hypertensive patients.Citation23 Early-morning BP is also viewed as a missed therapeutic target, since the timing of the trough plasma-drug level and the lowest pharmacological effect may coincide with early-morning rise in BP, especially for antihypertensives taken once daily in the morning.Citation88
Morning hypertension is diagnosed if morning BP values are ≥135/85 mmHg using out-of-office BP monitoring or ≥140/90 mmHg using OBPM in the morning.Citation89 It can also be defined as having a morning–evening BP difference of >15 mmHg or a morning–nocturnal BP difference of >35–55 mmHg.Citation59,Citation90 It is recommended to take two to three BP readings every morning for 5–7 days, and the average of these BP readings should be used for evaluation.Citation89 There are two types of morning hypertension that can be detected by HBPM: one is caused by extreme morning BP surge, whereas the other is caused by prolonged nocturnal hypertension that extends into the morning.Citation59,Citation66,Citation79,Citation91 In the latter case, persistent nocturnal hypertension overlaps partially with morning hypertension, and it is often observed in patients with nondipping or reverse nocturnal dipping patterns.Citation78,Citation91
The morning surge observed by ABPM has been found to be unreproducible.Citation90 Also, a threshold above which the morning surge in BP becomes pathological remains elusive, and there is still no consensus on a clear definition and assessment of this parameter.Citation14,Citation23 Morning BP, however, may be regarded as a therapeutic target for preventing target-organ damage and subsequent cardiovascular events in hypertension. Morning hypertension is best monitored through HBPM under fixed conditions at the same time in the morning and evening (or during sleep if possible) over a long period.Citation78 Japanese Society of Hypertension guidelines recommend morning HBP be measured within 1 hour of waking and after urination, but before medications or meals, while evening HBP should be measured just before going to bed ().Citation92,Citation93
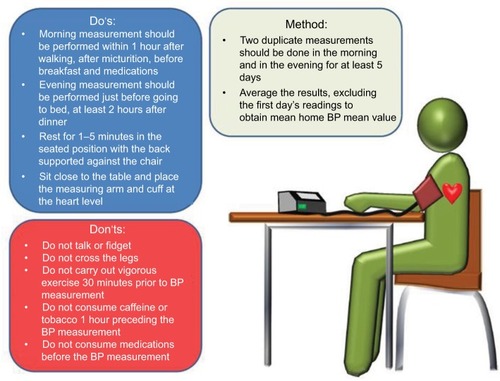
Figure 1 Measurement of home blood pressure (BP).
Abbreviations: JSH, Japanese Society of Hypertension; NICE, National Institute for Health and Care Excellence.
Measurement of short-term BPV
There is increasing evidence to show that conventional OBPM to diagnose and monitor a patient’s response to antihypertensive treatment may not be effective.Citation14,Citation23,Citation49 OBP measurements have some serious limitations, such as their inability to assess the dynamic characteristics of BP and collect data in the patient’s usual daily setting.Citation14 They also rely heavily on the technique of the operator, and thus may give rise to observer bias.Citation14 Lastly, white-coat hypertension and masked hypertension are also commonly associated with BP readings taken in a clinical setting, which may lead to an inaccurate diagnosis of hypertension.Citation2,Citation14,Citation18 HBPM and ABPM, on the other hand, are recommended in clinical practice to diagnose white-coat hypertension and masked hypertension and can estimate increased BPV, since they are able to detect various changes in BP associated with such conditions.Citation23,Citation94
A major advantage of out-of-office BP monitoring is that it can provide a large number of BP measurements away from the medical environment. Evidence is growing that such out-of-office measurements can also have better prognostic values for cardiovascular events, and these are now widely considered as significantly superior to OBPM readings.Citation14,Citation23,Citation73,Citation95–Citation100 As such, out-of-office measurements, such as ABPM and HBPM, are increasingly recommended by major guidelines to complement conventional OBP measurements in clinical practice ().Citation101–Citation104
Table 2 Recommendations on out-of-office BP measurements from key international guidelines on hypertension
HBPM is defined as regular measurement of BP at home by the patient outside any clinical setting.Citation3 Despite the widespread use of HBPM, there is no standardized protocol for its measurement, and this might result in an inaccurate assessment of BP. Therefore, it is vital to adopt a standardized protocol that has been validated.Citation3 HBPM is recommended to be measured as such:
BP measurement should be taken in a quiet room in a seated position using a validated automatic BP device with correct arm-cuff sizeCitation3,Citation103,Citation105
the patient should be seated with their back supported and feet flat on the floor with legs uncrossed, while the measuring arm should be relaxed and supported at heart levelCitation3,Citation105
the patient should be in a comfortable and calm state while the measurement is made, and should have at least 1–5 minutes of seated rest before the measurementCitation39,Citation105,Citation106
measurement should be taken before medication, food, or vigorous exercise and after micturitionCitation3,Citation105,Citation107–Citation110
stimulants containing such products as coffee and cigarettes should not be consumed for 30 minutes before BP measurement.Citation3,Citation105
Two measurements should be conducted, 1 minute apart, in the morning, as well as in the evening, for a total of 7 days (at least 5 days).Citation94,Citation105,Citation111–Citation113 Measurements should be taken at around the same time while maintaining similar conditions throughout the measuring period to minimize the BPV around the true mean BP value.Citation114 HBP is then calculated by averaging systolic and diastolic BP recorded over the period after excluding the first day’s readings.Citation3 In general, HBP higher than 135/85 mmHg is accepted as the criterion for diagnosis of hypertension by various guidelines ().Citation3,Citation92,Citation93,Citation101,Citation103,Citation104,Citation115 However, it has been found that many physicians may not follow this BP-cutoff point for diagnosis of hypertension, but instead use a higher BP cutoff (>140/90 mmHg) to diagnose hypertension based on HBPM recordings.Citation116–Citation118
Table 3 Recommendations from key international guidelines on diagnosis of hypertension using OBP and out-of-office BP monitoring
The consensus target HBP for antihypertensive treatment remains controversial. The recent American Heart Association guidelines now recommend HBP of 135/85 mmHg as target for treatment in hypertensive patients and 130/80 mmHg in high-risk patients.Citation115 Japanese Society of Hypertension guidelines, on the other hand, recommend HBP of 125/80 mmHg as target for treatment in young and middle-aged persons and 135/85 mmHg in the elderly.Citation93,Citation119
ABPM is defined as the method of measuring BP readings noninvasively at short intervals over a 24-hour period with the aid of an automated BP device while the patient is going about their daily routine.Citation39,Citation105,Citation120 An ABPM device automatically takes BP readings every 15 minutes during the day and 30 minutes at night over a 24-hour period.Citation23 Daytime for ABPM is defined as 9:00–21:00 while the patient is normally awake. On the other hand, nighttime is defined as 1:00–6:00 while the patient is asleep. A total of at least 20 valid readings when awake and seven valid readings while asleep (about 70% of total readings) are needed to confirm the results at the end of the 24-hour ABPM. The ABPM device automatically provides the user with unique data, such as 24-hour average BP, daytime (awake hours) BP, nighttime (sleeping) BP, dipping status, early-morning BP surge, BP load, trough:peak ratio, and smoothness index. The actual diagnosis of hypertension depends on the time frame of ABPM used.Citation23,Citation94 In general, patients with greater-than-average BP of 130/80 mmHg measured over a 24-hour period are considered hypertensive.Citation94 In addition, a daytime average >135/85 mmHg or a nighttime average >120/70 mmHg are also considered hypertensive.Citation94
Understanding indices of short-term BPV
There are a few different methods to represent short-term BPV.Citation15 SD of 24-hour average ABP values is one of the most commonly used parameters in measuring short-term BPV, but it is sometimes expressed as the weighted mean of daytime and nighttime BP levels to take into account the fall in BP during sleep.Citation15,Citation41,Citation121 However, the validity of SD has been questioned as an appropriate index of short-term BPV, considering that it reflects only the dispersion of values around the mean, does not account for the order in which BP measurements are obtained, and is sensitive to the low sampling frequency of ABPM.Citation122
Therefore, other indices, eg, 24-hour weighted SD, CoV, and ARV, are also used to overcome the limitations of traditional SD values and provide more accurate assessment better to predict target-organ damage and cardiovascular risk:Citation2,Citation40–Citation42
24-hour SD can also be divided by the corresponding mean BP and multiplied by 100 to be expressed as a CoV;Citation2 CoV has been observed to have greater prognostic ability than SD, as it can pinpoint individuals whose BPV falls outside its anticipated rangeCitation4
24-hour weighted SD is the average of daytime and nighttime BP that has been adjusted for the duration of the day and night period to account for day–night BP changes.Citation41
ARV is another index that is the average of the absolute differences between consecutive BP measurements, and some studies have shown it to be more reliable prognostic indicator compared to SD, as it is more sensitive to the individual BP-measurement sequence and less sensitive to low sampling frequency.Citation4,Citation2,Citation40,Citation123
ABPM vs HBPM for assessment of short-term BPV
ABPM monitors changes in BP at many time points throughout the day in an unrestricted manner, whereas HBPM detects BP fluctuations under standardized conditions over a longer period.Citation78 Multiple readings of ABPM obtained within 24 hours allow for more detailed analyses of both night- and daytime readings, making ABPM more suitable than HBPM for monitoring of intraday BP fluctuations.Citation14,Citation23 As such, ABPM may provide several advantages over HBPM in providing more extensive information on BP changes throughout the day.Citation23
Even though ABPM can provide extensive information, such as average day and night readings, BPV, morning BP surge, and BP load, ABPM still faces many issues regarding practicality, reproducibility, and long-term usage.Citation2,Citation3,Citation23,Citation78,Citation124 Previously, only ABPM had the ability to record nocturnal BP values, which are superior to daytime values in predicting mortality.Citation43,Citation77,Citation83,Citation124–Citation126 With recent developments and newer HBPM devices with the ability to record accurate nocturnal recordings, HBPM might offer a reliable alternative to ABPM for monitoring short-term BPV within a day.Citation95
HBPM is also highly practical and more affordable and accessible to patients compared with ABPM.Citation127 HBPM can also be easily repeated over prolonged periods (days to months) in the patient’s own environment, making it more suitable for the monitoring of longer-term BPV in day-to-day or visit-to-visit parameters.Citation2,Citation23,Citation95,Citation104,Citation128,Citation129 As such, HBPM was found to be the more common tool used by physicians to diagnose hypertension, even though ABPM was ranked the more valuable tool for assessing hypertension.Citation78,Citation116 Moreover, mean BP values from HBPM are stable and highly reproducible, since they are obtained under fixed conditions and not easily influenced by changes in daily activities.Citation78 In addition, HBPM is easily available to the general public, and can thus be used in both normotensive and hypertensive individuals.Citation78,Citation130
HBPM can also provide instant feedback directly to the health-care professional regarding the diagnosis and treatment of hypertension, while there is usually a delay in ABPM in relaying the information.Citation78,Citation131–Citation134 However, HBPM is prone to patient-recording errors and improper BP-recording techniques, which may compromise the accuracy and reliability of the data.Citation78,Citation135,Citation136 Therefore, it is useful to use a device with integrated memory, and patients should be properly trained on the method for its use.Citation2,Citation23,Citation78,Citation105,Citation137–Citation139 On balance, HBPM has been suggested as the method of choice to monitor BPV over the long term in clinical practice by many guidelines, even though it may not provide insights as extensive as ABPM.Citation2,Citation58,Citation92,Citation93,Citation103,Citation104,Citation140,Citation141
Conclusion
Short-term BPV within 24-hours is heavily influenced by circadian variations, resulting in many important phenotypes, such as morning BP surge, morning hypertension, nocturnal dipping, and nocturnal hypertension. Such variations in short-term BPV are only captured and reflected through out-of-office BP measurements like 24-hour ABPM or HBPM. As such, it is important to have a good understanding of proper use of these out-of-office measurements in a clinically validated manner. Both physicians and patients should be strongly encouraged to use ABPM and/or HBPM for monitoring BP, as a reduction in nocturnal hypertension and exaggerated morning BP surge are vital for the effective management of hypertension, rather than simply controlling average BP levels.
Author contributions
All authors were involved in the conception, design, and analysis and interpretation of data. All authors were also involved in preparation of the manuscript, revising it for scientific content and final approval before its submission for publication.
Acknowledgments
The authors would like to thank Ms. Tanaya Bharatan, Pfizer, for her editorial support with this manuscript.
Disclosure
KS and SS are employees of Pfizer. MTY underwent indirect patient-care pharmacy training for 3 months at Pfizer, Singapore. The other authors report no conflicts of interest in this work.
References
- World Health OrganizationA Global Brief on Hypertension: Silent Killer, Global Public Health CrisisGenevaWHO2013
- ParatiGOchoaJELombardiCBiloGAssessment and management of blood-pressure variabilityNat Rev Cardiol201310314315523399972
- SharmanJEHowesFSHeadGAHome blood pressure monitoring: Australian expert consensus statementJ Hypertens20153391721172826136205
- FlorasJSBlood pressure variability: a novel and important risk factorCan J Cardiol201329555756323618505
- HöchtCBlood pressure variability: prognostic value and therapeutic implicationsISRN Hypertens20132013398485
- SilvaniAPhysiological sleep-dependent changes in arterial blood pressure: central autonomic commands and baroreflex controlClin Exp Pharmacol Physiol200835998799418565197
- KooDLNamHThomasRJYunCHSleep disturbances as a risk factor for strokeJ Stroke2018201123229402071
- SilvaniAMagossoEBastianiniSLenziPUrsinoMMathematical modeling of cardiovascular coupling: central autonomic commands and baroreflex controlAuton Neurosci20111621667121550860
- Holt-LunstadJJonesBQBirminghamWThe influence of close relationships on nocturnal blood pressure dippingInt J Psychophysiol200971321121718930771
- MellmanTABrownDDJeniferESHipolitoMMRandallOSPosttraumatic stress disorder and nocturnal blood pressure dipping in young adult African AmericansPsychosom Med200971662763019483123
- KarioKObstructive sleep apnea syndrome and hypertension: ambulatory blood pressureHypertens Res200932642843219494815
- ManciaGGrassiGRedonJManual of Hypertension of the European Society of HypertensionAbingdonTaylor and Francis2008
- ParatiGOchoaJEBiloGBlood pressure variability, cardiovascular risk, and risk for renal disease progressionCurr Hypertens Rep201214542143122903810
- ParatiGOchoaJESalviPLombardiCBiloGPrognostic value of blood pressure variability and average blood pressure levels in patients with hypertension and diabetesDiabetes Care201336Suppl 2S312S32423882065
- ChenniappanMBlood pressure variability: assessment, prognostic significance and managementJ Assoc Physicians India20156354753
- ManciaGFerrariAGregoriniLBlood pressure and heart rate variabilities in normotensive and hypertensive human beingsCirc Res1983531961046861300
- ParatiGUlianLSantucciuCOmboniSManciaGDifference between clinic and daytime blood pressure is not a measure of the white coat effectHypertension1998315118511899576133
- FagardRHCornelissenVAIncidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysisJ Hypertens200725112193219817921809
- PickeringTGDavidsonKGerinWSchwartzJEMasked hypertensionHypertension200240679579612468559
- StaussHMIdentification of blood pressure control mechanisms by power spectral analysisClin Exp Pharmacol Physiol200734436236817324151
- LangagerAMHammerbergBERotellaDLStaussHMVery low-frequency blood pressure variability depends on voltage-gated L-type Ca2+ channels in conscious ratsAm J Physiol Heart Circ Physiol20072923H1321H132717056668
- SouzaHCMartins-PingeMCda SilvaVJHeart rate and arterial pressure variability in the experimental renovascular hypertension model in ratsAuton Neurosci20081391384518276197
- PriestnerLKhuranaRHome blood pressure monitoring, blood pressure variability and morning blood pressure surgeSingapore Fam Physician20164226469
- ManciaGParatiGPomidossiGCasadeiRDi RienzoMZanchettiAArterial baroreflexes and blood pressure and heart rate variabilities in humansHypertension1986821471533080371
- ParatiGSaulJPDi RienzoMManciaGSpectral analysis of blood pressure and heart rate variability in evaluating cardiovascular regulation: a critical appraisalHypertension1995256127612867768574
- ConwayJBoonNDaviesCJonesJVSleightPNeural and humoral mechanisms involved in blood pressure variabilityJ Hypertens1984222032086398335
- ParatiGCastiglioniPDi RienzoMOmboniSPedottiAManciaGSequential spectral analysis of 24-hour blood pressure and pulse interval in humansHypertension19901644144212210809
- SchillaciGBiloGPucciGRelationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databasesHypertension201260236937722753222
- BertinieriGParatiGUlianLHemodilution reduces clinic and ambulatory blood pressure in polycythemic patientsHypertension19983138488539495271
- ParatiGPomidossiGAlbiniFMalaspinaDManciaGRelationship of 24-hour blood pressure mean and variability to severity of target-organ damage in hypertensionJ Hypertens19875193983584967
- ManciaGParatiGHennigMRelation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA)J Hypertens200119111981198911677363
- ManciaGParatiGThe role of blood pressure variability in end-organ damageJ Hypertens Suppl2003216S17S2314513947
- SegaRCorraoGBombelliMBlood pressure variability and organ damage in a general population: results from the PAMELA study (Pressioni Arteriose Monitorate e Loro Associazioni)Hypertension2002392 Pt 271071411882636
- TatascioreARendaGZimarinoMAwake systolic blood pressure variability correlates with target-organ damage in hypertensive subjectsHypertension200750232533217562971
- ManiosETsagalisGTsivgoulisGTime rate of blood pressure variation is associated with impaired renal function in hypertensive patientsJ Hypertens200927112244224819644388
- FrattolaAParatiGCuspidiCAlbiniFManciaGPrognostic value of 24-hour blood pressure variabilityJ Hypertens19931110113311378258679
- SanderDKuklaCKlingelhöferJWinbeckKConradBRelationship between circadian blood pressure patterns and progression of early carotid atherosclerosis: a 3-year follow-up studyCirculation2000102131536154111004145
- StergiouGSParatiGAsmarRO’BrienERequirements for professional office blood pressure monitorsJ Hypertens201230353754222241143
- ShimamotoKAndoKFujitaTThe Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014)Hypertens Res201437425339024705419
- MenaLPintosSQueipoNVAizpuruaJAMaestreGSulbaranTA reliable index for the prognostic significance of blood pressure variabilityJ Hypertens200523350551115716690
- BiloGGiglioAStyczkiewiczKA new method for assessing 24-h blood pressure variability after excluding the contribution of nocturnal blood pressure fallJ Hypertens200725102058206617885548
- Stolarz-SkrzypekKThijsLRichartTBlood pressure variability in relation to outcome in the international database of ambulatory blood pressure in relation to cardiovascular outcomeHypertens Res201033875776620613762
- HansenTWLiYBoggiaJThijsLRichartTStaessenJAPredictive role of the nighttime blood pressureHypertension201157131021079049
- VerdecchiaPSchillaciGGatteschiCBlunted nocturnal fall in blood pressure in hypertensive women with future cardiovascular morbid eventsCirculation19938839869928353926
- BoggiaJLiYThijsLPrognostic accuracy of day versus night ambulatory blood pressure: a cohort studyLancet200737095941219122917920917
- LurbeERedonJKesaniAIncrease in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetesN Engl J Med20023471179780512226150
- VerdecchiaPAngeliFMazzottaGDay-night dip and early-morning surge in blood pressure in hypertension: prognostic implicationsHypertension2012601344222585951
- ShimboDSheaSMcClellandRLAssociations of aortic distensibility and arterial elasticity with long-term visit-to-visit blood pressure variability: the Multi-Ethnic Study of Atherosclerosis (MESA)Am J Hypertens201326789690223537891
- BurkardTMayrMWinterhalderCLeonardiLEcksteinJVischerASReliability of single office blood pressure measurementsHeart Epub2018312
- SheppardJPMartinUGillPStevensRMcManusRJProspective Register of Patients Undergoing Repeated Office and Ambulatory Blood Pressure Monitoring (PROOF-ABPM): protocol for an observational cohort studyBMJ Open2016610e012607
- SeboPPechere-BertschiAHerrmannFRHallerDMBovierPBlood pressure measurements are unreliable to diagnose hypertension in primary careJ Hypertens201432350951724299914
- LevyJGerberLMWuXMannSJNonadherence to recommended guidelines for blood pressure measurementJ Clin Hypertens2016181111571161
- KikuyaMOhkuboTMetokiHDay-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama studyHypertension20085261045105018981332
- RothwellPMHowardSCDolanEPrognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertensionLancet2010375971889590520226988
- JohanssonJKNiiranenTJPuukkaPJJulaAMPrognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home StudyHypertension201259221221822215704
- ShimboDNewmanJDAragakiAKAssociation between annual visit-to-visit blood pressure variability and stroke in postmenopausal women: data from the Women’s Health InitiativeHypertension201260362563022753206
- MuntnerPShimboDTonelliMReynoldsKArnettDKOparilSThe relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: findings from NHANES III, 1988 to 1994Hypertension201157216016621200000
- PickeringTGHallJEAppelLJRecommendations for blood pressure measurement in humans and experimental animals – part 1: blood pressure measurement in humans – a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure ResearchCirculation2005111569771615699287
- KarioKTomitaniNMatsumotoYResearch and development of information and communication technology-based home blood pressure monitoring from morning to nocturnal hypertensionAnn Glob Health201682225427327372530
- KarioKSchwartzJEDavidsonKWPickeringTGGender differences in associations of diurnal blood pressure variation, awake physical activity, and sleep quality with negative affect: the work site blood pressure studyHypertension2001385997100211711488
- KarioKEssential Manual of 24-Hour Blood Pressure Management from Morning to Nocturnal HypertensionLondonWiley-Blackwell2015
- LurbeERedonJKesaniAIncrease in Nocturnal blood pressure and progression to microalbuminuria in type 1 diabetesN Engl J Med20023471179780512226150
- MetokiHOhkuboTKikuyaMPrognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama studyHypertension200647214915416380533
- OhkuboTHozawaAYamaguchiJPrognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama studyJ Hypertens200220112183218912409956
- VerdecchiaPPrognostic value of ambulatory blood pressure: current evidence and clinical implicationsHypertension200035384485110720605
- KarioKPickeringTGUmedaYMorning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective studyCirculation2003107101401140612642361
- KarioKIshikawaJPickeringTGMorning hypertension: the strongest independent risk factor for stroke in elderly hypertensive patientsHypertens Res20062958117137213
- AmiciACicconettiPSagrafoliCExaggerated morning blood pressure surge and cardiovascular events. a 5-year longitudinal study in normotensive and well-controlled hypertensive elderlyArch Gerontol Geriatr2009492e105e10919070375
- FlorasJSJonesJVHassanMOOsikowskaBSeverPSSleightPCuff and ambulatory blood pressure in subjects with essential hypertensionLancet1981282381071096113479
- VerdecchiaPAngeliFBorgioniCPrognostic value of circadian blood pressure changes in relation to differing measures of day and nightJ Am Soc Hypertens200822889620409890
- OhkuboTImaiYTsujiIRelation between nocturnal decline in blood pressure and mortality: the Ohasama studyAm J Hypertens19971011120112079397237
- FagardRHDipping pattern of nocturnal blood pressure in patients with hypertensionExpert Rev Cardiovasc Ther20097659960519505275
- DolanEStantonAThijsLSuperiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome studyHypertension200546115616115939805
- MeadMAJGriffithKEKassaianosGKhanELewisPVoraJControlling blood pressure over 24 hours: a review of the evidenceBr J Cardiol20081513134
- IrigoyenMCde AngelisKdos SantosFDartoraDRRodriguesBConsolim-ColomboFMHypertension, blood pressure variability, and target organ lesionCurr Hypertens Rep20161843127002717
- XieJCYanHZhaoYXLiuXYPrognostic value of morning blood pressure surge in clinical events: a meta-analysis of longitudinal studiesJ Stroke Cerebrovasc Dis201524236236925511618
- StaessenJAThijsLFagardRPredicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertensionJAMA1999282653954610450715
- ImaiYObaraTAsamayaKOhkuboTThe reason why home blood pressure measurements are preferred over clinic or ambulatory blood pressure in JapanHypertens Res201336866167223595050
- KarioKSaitoIKushiroTHome blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational studyHypertension201464598999625156169
- HoshideSKarioKHoshideYAssociations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensivesAm J Hypertens200316643443812799090
- HoshideSIshikawaJEguchiKOjimaTShimadaKKarioKMasked nocturnal hypertension and target organ damage in hypertensives with well-controlled self-measured home blood pressureHypertens Res200730214314917460384
- LiYStaessenJALuLLiLHWangGLWangJGIs isolated nocturnal hypertension a novel clinical entity? Findings from a Chinese population studyHypertension200750233333917576859
- SegaRFacchettiRBombelliMPrognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) studyCirculation2005111141777178315809377
- KarioKProposal of a new strategy for ambulatory blood pressure profile-based management of resistant hypertension in the era of renal denervationHypertens Res201336647848423514717
- IshikawaJHoshideSEguchiKIshikawaSShimadaKKarioKNighttime home blood pressure and the risk of hypertensive target organ damageHypertension201260492192822892810
- ChonanKKikuyaMArakiTDevice for the self-measurement of blood pressure that can monitor blood pressure during sleepBlood Press Monit20016420320511805470
- HosohataKKikuyaMOhkuboTReproducibility of nocturnal blood pressure assessed by self-measurement of blood pressure at homeHypertens Res200730870771217917318
- ShimadaKKarioKUmedaYHoshideSHoshideYEguchiKEarly morning surge in blood pressureBlood Press Monit20016634935312055414
- WangJGKarioKChenCHManagement of morning hypertension: a consensus statement of an Asian expert panelJ Clin Hypertens20182013944
- WiznerBDecheringDGThijsLShort-term and long-term repeatability of the morning blood pressure in older patients with isolated systolic hypertensionJ Hypertens20082671328133518551007
- KarioKTime for focus on morning hypertension: pitfall of current antihypertensive medicationAm J Hypertens2005182 Pt 114915115752939
- ImaiYOtsukaKKawanoYJapanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at homeHypertens Res2003261077178214621179
- ImaiYKarioKShimadaKThe Japanese Society of Hypertension guidelines for self-monitoring of blood pressure at home (second edition)Hypertens Res201235877779522863910
- ManciaGFagardRNarkiewiczK2013 ESH/ESC guidelines for the management of arterial hypertensionJ Hypertens20133171281135723817082
- StergiouGSBliziotisIAHome blood pressure monitoring in the diagnosis and treatment of hypertension: a systematic reviewAm J Hypertens201124212313420940712
- FuchsSCMelloRGFuchsFCHome blood pressure monitoring is better predictor of cardiovascular disease and target organ damage than office blood pressure: a systematic review and meta-analysisCurr Cardiol Rep2013151141324057836
- WardAMTakahashiOStevensRHeneghanCHome measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studiesJ Hypertens201230344945622241136
- BliziotisIADestounisAStergiouGSHome versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysisJ Hypertens20123071289129922499289
- OhkuboTImaiYTsujiIPrediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in OhasamaJ Hypertens19971543573649211170
- [No authors listed]Hypertension in Diabetes Study (HDS) – II: increased risk of cardiovascular complications in hypertensive type 2 diabetic patientsJ Hypertens19931133193258387090
- ChobanianAVBakrisGLBlackHRThe seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 reportJAMA2003289192560257212748199
- ParatiGPickeringTGHome blood-pressure monitoring: US and European consensusLancet2009373966787687819286071
- ManciaGde BackerGDominiczakA2007 Guidelines for the management of arterial hypertensionJ Hypertens20072561105118717563527
- ParatiGStergiouGSAsmarREuropean Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure MonitoringJ Hypertens20082681505152618622223
- WheltonPKCareyRMAronowWS2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adultsHypertension Epub20171113
- BoivinJMBoutteEFayRRossignolPZannadFHome blood pressure monitoring: a few minutes of rest before measurement may not be appropriateAm J Hypertens201427793293824561656
- AsayamaKOhkuboTKikuyaMPrediction of stroke by home “morning” versus “evening” blood pressure values: the Ohasama studyHypertension200648473774316952977
- EguchiKPickeringTGHoshideSAmbulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetesAm J Hypertens200821444345018292756
- HoshideSKarioKYanoYAssociation of morning and evening blood pressure at home with asymptomatic organ damage in the J-HOP studyAm J Hypertens201427793994724473255
- KamoiKUsefulness of morning home blood pressure measurements in patients with type 2 diabetes mellitus: results of a 10-year, prospective, longitudinal studyClin Exp Hyperten20143030
- VerberkWJKroonAAKesselsAGThe optimal scheme of self blood pressure measurement as determined from ambulatory blood pressure recordingsJ Hypertens20062481541154816877956
- NiiranenTJJohanssonJKReunanenAJulaAMOptimal schedule for home blood pressure measurement based on prognostic data: the Finn-Home studyHypertension20115761081108621482956
- NiiranenTJAsayamaKThijsLOptimal number of days for home blood pressure measurementAm J Hypertens201528559560325399016
- LindenAAssessing regression to the mean effects in health care initiativesBMC Med Res Methodol20131311924073634
- PickeringTGMillerNHOgedegbeGKrakoffLRArtinianNTGoffDCall to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses AssociationHypertension20085211918497371
- SetiaSSubramaniamKTayJCTeoBWHypertension and blood pressure variability management practices among physicians in SingaporeVasc Health Risk Manag20171327528528761353
- SetiaSSubramaniamKTeoBWTayJCAmbulatory and home blood pressure monitoring: gaps between clinical guidelines and clinical practice in SingaporeInt J Gen Med20171018919728721085
- RedonJErdineSBöhmMPhysician attitudes to blood pressure control: findings from the Supporting Hypertension Awareness and Research Europe-wide surveyJ Hypertens20112981633164021720274
- OgiharaTKikuchiKMatsuokaHThe Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2009)Hypertens Res2009321310719300436
- GrossmanEAmbulatory blood pressure monitoring in the diagnosis and management of hypertensionDiabetes Care201336Suppl 2S307S31123882064
- BiloGGiglioAStyczkiewiczKHow to improve the assessment of 24-h blood pressure variabilityBlood Press Monit200510632132316496448
- PierdomenicoSDDi NicolaMEspositoALPrognostic value of different indices of blood pressure variability in hypertensive patientsAm J Hypertens200922884284719498342
- JullienVAzoulayESchwebelCPopulation pharmacokinetics of micafungin in ICU patients with sepsis and mechanical ventilationJ Antimicrob Chemother201772118118927609051
- ManciaGDi RienzoMParatiGAmbulatory blood pressure monitoring use in hypertension research and clinical practiceHypertension19932145105248458650
- KikuyaMOhkuboTAsayamaKAmbulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama studyHypertension200545224024515596571
- FagardRHvan den BroekeCde CortPPrognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practiceJ Hum Hypertens2005191080180715959536
- ParkSBuranakitjaroenPChenCHExpert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia NetworkJ Hum Hypertens201832424925829386668
- O’BrienEAsmarRBeilinLEuropean Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurementJ Hypertens200321582184812714851
- MasdingMGJonesJRBartleyESandemanDDAssessment of blood pressure in patients with type 2 diabetes: comparison between home blood pressure monitoring, clinic blood pressure measurement and 24-h ambulatory blood pressure monitoringDiabet Med200118643143711472460
- ObaraTOhkuboTTanakaKPharmacists’ awareness and attitude toward blood pressure measurement at home and in the pharmacy in JapanClin Exp Hypertens201234644745522502629
- BosworthHBOlsenMKGrubberJMTwo self-management interventions to improve hypertension control: a randomized trialAnn Intern Med20091511068769519920269
- StahlSMKelleyCRNeillPJGrimCEMamlinJEffects of home blood pressure measurement on long-term BP controlAm J Public Health19847477047096742256
- BaguetJPMallionJMSelf-monitoring of blood pressure should be used in clinical trialsBlood Press Monit200271555912040245
- Lambert-KerznerAHavranekEPPlomondonMEPatients’ perspectives of a multifaceted intervention with a focus on technology: a qualitative analysisCirc Cardiovasc Qual Outcomes20103666867420923992
- MengdenTSchwartzkopffBStrauerBEWhat is the value of home (self) blood pressure monitoring in patients with hypertensive heart disease?Am J Hypertens19981178138199683042
- MyersMSelf-measurement of blood pressure at home: the potential for reporting biasBlood Press Monit19983Suppl 1S19S22
- JohnsonKAPartschDJRippoleLLMcVeyDMReliability of self-reported blood pressure measurementsArch Intern Med1999159222689269310597759
- MengdenTMedinaRMBeltranBAlvarezEKraftKVetterHReliability of reporting self-measured blood pressure values by hypertensive patientsAm J Hypertens19981112141314179880121
- MatsumotoSFukuiMHamaguchiMIs home blood pressure reporting in patients with type 2 diabetes reliable?Hypertens Res201437874174524718300
- McManusRJMantJRoalfeATargets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysisBMJ2005331751549316115830
- WhitworthJA2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertensionJ Hypertens200321111983199214597836
- National Institute for Health and Care ExcellenceHypertension in Adults: Diagnosis and ManagementLondonNICE2011
- HouleSKPadwalRPoirierLTsuyukiRTThe 2015 Canadian Hypertension Education Program (CHEP) guidelines for pharmacists: an updateCan Pharm J (Ott)2015148418018626448770
