Abstract
Introduction
Serratia marcescens is a Gram-negative bacillus which belongs to the family Enterobacteriaceae. It is a facultative anaerobe and produces red pigment at room temperature. It naturally occurs in soil and water as well as the intestines, and it is responsible for nosocomial infections. There have been few reports about community acquired pneumonia of Serratia.
Case presentation
This report presents a 37-year-old man with hemoptysis, fever, and shortness of breath. The clinical and laboratory examinations revealed that the patient had pseudohemoptysis due to S. marcescens pneumonia, on an immunocompromised pattern, because of the coexistence of sarcoidosis (stage 1).
Conclusion
Appropriate antibiotic therapy for Serratia was administered, and the patient’s symptoms regressed. The patient is healthy and asymptomatic after 1-year follow-up. To the best of the authors’ knowledge, this is the first reported case of a pseudohemoptysis in a patient with pulmonary sarcoidosis.
Introduction
Serratia, is an opportunistic pathogen, mainly responsible for infecting the urinary system, respiratory tract, central nervous system, and bloodstream.Citation1 Infections of colonized individuals are associated with invasive devices, surgery, and immunocompromised states. Serratia ubiquitously thrives in moist environments and frequently contaminates liquids and equipment. In the outpatient setting, it has been associated with community-acquired pneumonias, but only limited case reports exist, and usually are associated with some degree of immunocompromise. This paper reports a case where the poor living environment and coexistence of sarcoidosis were likely the predisposing factors that developed pneumonia from Serratia.
Case report
A 37-year-old man presented in the emergency department complaining of productive cough with blood-tinged sputum, intermittent fever, and shortness of breath for the last 20 days. He was a lifelong nonsmoker, currently unemployed, and occasionally homeless. His past medical history was remarkable only for arterial hypertension treated with atenolol.
On examination, he was ill-appearing but in no acute distress. His axillary temperature was 37.8°C, blood pressure was 140/80 mm Hg with a normal heart rate of 90 bpm, and oxygen saturation SpO2: 94%. Lung auscultation revealed crackles over the lower right lung.
On laboratory testing, the patient had a mildly elevated white blood cell count of 10,900 cells/μL, with normal differential. The hemoglobin level was 10.6 g/dL, with a hematocrit of 32.5%; the platelet count was 455,000/L. The erythrocyte sedimentation rate was 55 mm after the first hour. A basic metabolic panel was notable for an elevated serum creatinine of 2.52 mg/dL, with urea of 57 mg/dL, and normal electrolytes. Serum angiotensin converting enzyme was slightly elevated at 57 IU/mL (normal range 8–52 IU/mL). The acute renal failure was attributed to the Serratia infection, since the patient did not previously have this disorder and Serratia is known to induce renal failure.Citation1
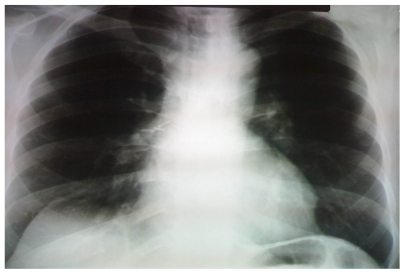
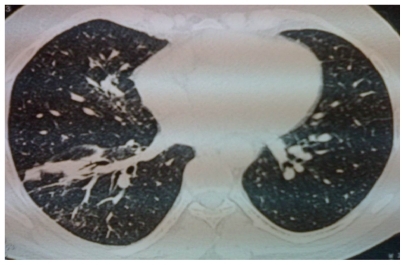
There was no lymphadenopathy observed in general examination, but chest x-radiography demonstrated bilateral hilar prominence, lower-right lung lobe opacification, and right hemidiaphragm elevation (). Chest high-resolution computed tomography scan was performed according to the department’s protocol for investigating the thorax. The scan revealed consolidation of the anterior segment of the right lower lobe, and bilateral paratracheal, subcarinal, and hilar lymphadenopathy (). In addition, transbronchial needle biopsy aspiration was conducted as a diagnostic approach.
Figure 1 Chest radiograph, demonstrating prominent hilar shadows bilaterally, opacity at the lower lobe of the right lung, and elevation of the ipsilateral hemiseptum.
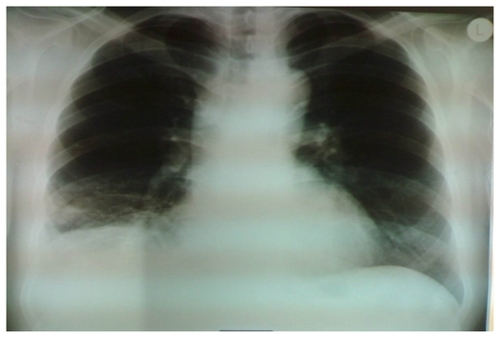
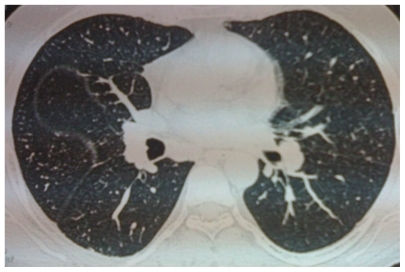
Figure 2 Computed tomography scan of the chest, revealing a right lung consolidation, with bronchogram, of the anterior segment of the lower lobe.
Pulmonary function testing after remission of the productive cough (2 days) showed a restrictive pattern with a forced vital capacity (FVC) of 49% predicted, a forced expiratory volume in one second (FEV1) of 47% predicted, and an FEV1/FVC ratio of 71%. The total lung capacity was 66% of predicted, and the residual volume was 79% of predicted. There was reduction of the diffusion lung capacity for carbon monoxide to 68% of predicted.
Serologic studies for human immunodef iciency, hepatitis B virus, and a tuberculin skin test were negative. Urine antigen for Streptococcus pneumoniae and Legionella were given upon admission, but they were also negative.
Fiberoptic bronchoscopy revealed a partial extraluminal compression of the trachea without other endobronchial lesions. No evidence of inflammation, granulomas, malignancy, vasculitis, or alveolar wall necrosis were found on biopsy. The cytological results from the bronchoalveolar lavage fluid (BALF) showed no malignancy. The cell count on the BALF was 10.5 × 1010 cell/L, with 78% alveolar macrophages, 12% lymphocytes, and 10% neutrophils. No red blood cells or hemosiderin-laden macrophages were seen. BALF flow cytometry showed that 69% of the lymphocytes were T-lymphocytes, 7% were B-lymphocytes, and the T4/T8 ratio was 1.9, while the blood T4/T8 ratio was 1.4. Microbiology cultures of the BALF grew Serratia marcescens, which was sensitive to ciprofloxacin, tobramycin, and amikacin. The smear for acid-fast bacilli was negative, and cultures for mycobacteria remained negative after 6 weeks.
The patient was treated with ciprofloxacin 500 mg twice daily for 3 weeks. After the third day of treatment, the cough improved, and the reddish appearance of the sputum completely resolved. On follow-up after 1 month, chest x-radiography presented complete remission on right lower lobe infiltrate, while the perihilar lymphadenopathy persisted. A surgical mediastinal biopsy showed nonnecrotizing granulomas, consistent with sarcoidosis. The final diagnosis was pneumonia due to S. marcescens and stage I pulmonary sarcoidosis.
After 1-year follow-up, the patient remains asymptomatic, and on chest x-radiography the infiltrate has completely resolved, while enlargement of the perihilar lymph nodes persists ( and ).
Discussion
This is a case of pseudohemoptysis due to pulmonary infection with S. marcescens and concomitant sarcoidosis unexpectedly found. S. marcescens is a Gram-negative, rod-shaped bacterium in the Enterobacteriaceae family, found in soil, water, plants, and human gut flora. At room temperature, it produces the red pigment prodigiosin. Pseudohemoptysis, which is the appearance of bright reddish or pinkish colored sputum without the evidence of any red blood cells, has been well described in colonization or infection with Serratia and is attributed to this pigment. In this patient, similarly to previously published cases, no red blood corpuscles were seen on direct microscopic examination of his sputum.Citation2
Lymph node hyperplasia occurs in Serratia infections and may persist after treatment. This is due to the marked follicular, primary and secondary germinal center and medullar hyperplasia.Citation3 In this case, the lymph node biopsy did not show any of these features but only nonnecrotizing granulomas without evidence of infection.
The coexistence of sarcoidosis and opportunistic infection in the absence of any immunosuppressive therapy has previously been documented.Citation4 An infection can be the presenting problem subsequently leading to the diagnosis of sarcoidosis, as in this case.
In sarcoidosis immunopathogenesis, the immune system undergoes a reactivity change. Primary features are a reduction in circulating CD4+ lymphocytes (T-helper cells), while their numbers in tissue increase, which is associated with a marked increase in tissue cytokine production, particularly interferon-γ, granulocyte-macrophage colony-stimulating factor, and interleukin-2.Citation5,Citation6 This T-helper 1 (Th-1) cytokine profile recruits macrophages, eventually forming a granulomatous reaction.Citation7
In contrast to these highly active tissue-based responses, the immunity related to the circulatory cells expression is depressed by cutaneous anergy and poor responses to antigen recall testing. In addition, the production of inhibitory cytokines by macrophages appears to interfere with the normal immune response. Girard et al reported five cases and reviewed 65 additional cases of opportunistic infections associated with sarcoidosis.Citation8 While the majority of these occurred in patients receiving corticosteroids and were accompanied by CD4 lymphocytopenia, they described opportunistic infections in four untreated individuals. Observations have suggested a pathogenetic role of Gram-negative infections in sarcoidosis by driving an interleukin-18 response as another feature of the Th-1 pathway.Citation9 This has been postulated for infections with Hemophilus influenzae and Moraxella catarrhalis.Citation10
Conclusion
In summary, this report describes a rare case of an opportunistic infection in an outpatient setting. In this case, the sarcoidosis was the underlying condition that induced an infection by Gram-negative bacilli.
Consent
Written informed consent was obtained from the patient upon discharge for publication of this case report and all accompanying images.
Acknowledgments
All authors contributed equally to the preparation of the manuscript.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
- HaddyRIMannBLNadkarniDDNosocomial infection in the community hospital: severe infection due to Serratia speciesJ Fam Pract1996422732778636679
- Hurtado AyusoJEOtero CandeleraRLopez CasanovaCPseudohemoptysis due to Serratia marcescens, an etiology to rememberArch Bronconeumol19993519419510330545
- PedersenNCDeanGABernalesJSukuraAHigginsJListeria monocytogenes and Serratia marcescens infections as models for Th1/ Th2 immunity in laboratory catsVet Immunol Immunopathol199863831039656444
- SadikotRTDorePArnoldAGSarcoidosis and opportunistic infectionsSouth Med J200194757711213950
- KatariaYPHolterJFImmunology of sarcoidosisClin Chest Med1997187197399413655
- MollersMAriesSPDromannPMascherBBraunJDalhoffKIntracellular cytokine repertoire in different T cell subsets from patients with sarcoidosisThorax20015648749311359967
- AgostiniCFaccoMChilosiMSemenzatoGAlveolar macrophage-T cell interactions during Th1-type sarcoid inflammationMicrosc Res Tech20015327828711340673
- GirardNCottinVHotAEtienne-MastroianniBChidiacCCordierJFOpportunistic infections and sarcoidosisRev Mal Respir2004211083109015767952
- AntoniouKMTzouvelekisAAlexandrakisMUpregulation of Th1 cytokine profile (IL-12, IL-18) in bronchoalveolar lavage fluid in patients with pulmonary sarcoidosisJ Interferon Cytokine Res20062640040516734560
- KellyDMGreeneCMMeacheryGEndotoxin up-regulates interleukin-18: potential role for gram-negative colonization in sarcoidosisAm J Respir Crit Care Med20051721299130716100009