Abstract
In recent years, there has been a major advance in the treatment of pulmonary hypertension. New medications are continually added to the therapeutic arsenal. The prostanoids are among the first agents used to treat pulmonary hypertension and are currently considered the most effective. This case study describes a 63-year-old man who was diagnosed with chronic thromboembolic pulmonary hypertension and successfully treated with subcutaneously administered treprostenil for 6 months before a successful pulmonary thromboendarterectomy. Treatment of chronic thromboembolic pulmonary hypertension often requires a multidisciplinary approach before surgery. Further evaluation of prostanoids is needed to define their role and time of initiation of medical therapy in these patients.
Introduction
Chronic thromboembolic pulmonary hypertension (CTEPH) has emerged as one of the leading causes of severe pulmonary hypertension.Citation1–Citation3 The disease is notoriously underdiagnosed, and its true prevalence is still unclear. However, with the development of improved therapeutic modalities, cardiologists and thoracic surgeons have shown increasing interest in the diagnostic work-up of this entity. The diagnosis and management of CTEPH requires a multidisciplinary approach involving the specialties of pulmonary medicine, cardiology, radiology, anesthesiology, and thoracic surgery. CTEPH is characterized by intraluminal thrombus organization and fibrous stenosis or complete obliteration of pulmonary arteries.
Due to clinically evident acute pulmonary embolism episodes being absent in >50% of patients, the diagnosis of CTEPH can be difficult. Computed tomography pulmonary angiogram is the gold standard test for diagnosing CTEPH and will show features of chronic pulmonary embolism. Another method used is the lung scintiscan showing segmental mismatched perfusion defects. Pulmonary angiography confirms the diagnosis and determines the feasibility of endarterectomy according to the location of the disease (proximal versus distal). The technique of angiography must be perfect with the whole arterial tree captured on the same picture for each lung. The lesions must start at the level of the pulmonary artery trunk or at the level of the lobar arteries, in order to find a plan for the endarterectomy. When the hemodynamic gravity corresponds to the degree of obliteration, pulmonary thromboendarterectomy can be performed.Citation4
CTEPH induces hypoxemia and pulmonary hypertension, eventually leading to respiratory failure and right heart failure. Treatment of CTEPH often requires a multidisciplinary approach and may involve surgery, medical treatment, or both.Citation5,Citation6 Vascular disobliteration by pulmonary endarterectomy (PTE) is the preferred treatment for patients with CTEPH,Citation7,Citation8 but not all patients are eligible for surgery.Citation9 When surgical indications are carefully selected, pulmonary thromboendarterectomy using intermittent circulatory arrest under profound hypothermia is quite effective for treating CTEPH.
Case report
A 63-year-old man presented in the emergency department complaining of progressive dyspnea on exertion and signs of right heart dysfunction including fatigue and palpitations. The patient was an ex-smoker (25 pack-years), had a history of percutaneous transluminal coronary angioplasty 5 years previously, was on anticoagulant treatment (warfarin), and had an international normalized ratio level of 2.3 at the time of admission. He had decreased daily movement and was obligated to stop for rest every 100 meters of walking. He was in his usual state of health until 15 days before presentation, when he noted the onset of bilateral lower extremity edema. His symptoms of fatigue, orthopnea, paroxysmal nocturnal dyspnea, and a productive cough of clear sputum had progressed. His exercise tolerance had decreased from several kilometers to 10–20 meters at a walking pace of less than 100 meters.
Physical findings included a left parasternal heave, a prominent pulmonary component of S2, left block, and a systolic murmur of tricuspid regurgitation. He was hypoxic, hyperventilating (respiratory rate 30/minute), had low oxygen saturation (SpO2), and had signs of right heart failure (extended neck veins, legs swelling, and acrocyanosis). At the time of admission, arterial blood gases on air were pH 7.46, partial pressure carbon dioxide 31 mmHg, partial pressure of oxygen 53 mmHg, and SpO2 89%. Blood gas analysis revealed a wide alveolar and arterial oxygen tension difference, which is typical for patients with CTEPH. His blood pressure was 100/90 mmHg. Chest x-ray revealed hyperlucency, diminished vasculature, and cardiomegaly with prominent central pulmonary arteries ().
Figure 1 Cardiomegaly and dilatation of right and left lung hilum. Increased vascular shadowing in both sides. Costophrenic regions free of pleural effusion.

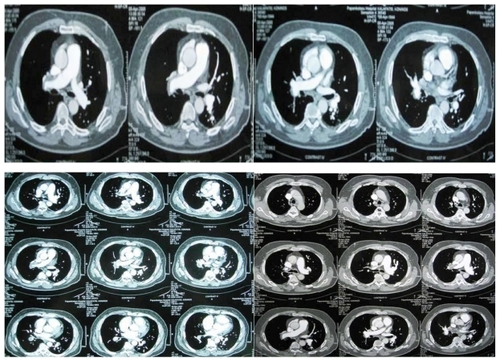
Transthoracic echocardiography was the initial diagnostic tool that demonstrated enlarged right heart cavities with normal sized left ventricle, paradoxical movement of interventricular septum, and severe pulmonary hypertension (right ventricle systolic pressure [RVSP] 73 mmHg). The ventilation-perfusion scanning demonstrated multiple perfusion deficits in both lungs compatible with chronic thromboembolic disease (). Diagnosis was supported by computed tomography angiography, which revealed eccentric thrombotic material within the main branch of the right pulmonary artery, the branches of the right lower lobe, and the descending branch of the left lung; subpleural densities; and a characteristic mosaic attenuation of the pulmonary parenchyma (). Because a previous computed tomography angiogram was not available, it was presumed based upon the clinical findings that new emboli were formulated on established chronic thromboembolic disease. Although additional radiographic imaging with high-resolution computed tomography can assist in establishing venoocclusive disease, this method was not performed.Citation10,Citation11 The patient did not have severe hemodynamic instability and thrombolysis was not performed. Although acute pulmonary embolism may be clinically silent,Citation12 there is accumulating evidence that CTEPH may also develop in the absence of previous pulmonary embolism.Citation13 In these cases, the disease is probably initiated by thrombotic or inflammatory lesions in the pulmonary vasculature. Once vessel obliteration is sufficient to cause increases in the pulmonary arterial pressure, a process of pulmonary vascular remodelling is started, which self-perpetuates the progression of pulmonary hypertension, even in the absence of further thromboembolic events.Citation14
Figure 2 High probability for pulmonary embolism ventilation/perfusion scan demonstrating normal ventilation and multiple mismatched segmental and larger defects more in the right lung. The rate of perfusion for the right and the left lung is 27.4% and 72.4%, respectively.
Figure 3 Computed tomographic angiogram demonstrating findings of chronic pulmonary embolism and showing occlusive thrombus in the right pulmonary artery and its branches for the right lower lobe. Embolus within the left main pulmonary artery extending into the lobar branches. Small pericardial effusion, enlarged right ventricle, and congestion of inferior vena cava and hepatic veins.
Additional procoagulant work-up included activated partial thromboplastin time with a reference range of 18–28 seconds; antiphospholipids with immunoglobulin (Ig)M and IgG anticardiolipin antibodies measured by enzyme-linked immunosorbent assay, levels >20 MPL/GPL considered positive; anti-ß2 glycoprotein I levels measured by enzyme-linked immunosorbent assay, >20 SMU/GMU considered positive; lupus anticoagulant test detected using dilute Russell’s viper venom assay and confirmed with 1:1 dilution of plasma from patients with normal plasma to rule out factor deficiencies and confirm phospholipid dependency; protein C; protein S; antithrombin III, factor V Leiden; homocysteine; and prothrombin gene mutation. The work-up came back negative twice during the patient’s hospitalization. Further investigations for autoimmunity, collagen vascular diseases, hemoglobinopathies, HIV infection, drug or toxin use, and sleep apnea were negative.
At the time of the patient’s admission he was in class IV based on the classification of the New York Heart Association (NYHA). The patient was treated with long-term oxygen therapy, diuretics, and anticoagulants (acenocoumarol) adjusted to a target international normalized ratio between 2.0 and 3.0. An evaluation of the patient was performed in the initial days after the admission, after prompt treatment was administered. At this stage, spirometry results were forced expiratory volume in 1 second 2.55 L (80%), forced vital capacity 3.42 L (83%), total lung capacity 5.27 L (76%), residual volume 2.26 L (92%), functional residual capacity 2.72 L (76%), and carbon monoxide diffusing capacity 14.9 L (54%). The patient’s 6 minute walking distance (6MWT) was 240 meters, and desaturation was from 91% to 85%. His ergospirometry findings were consistent with very poor prognosis (arterial blood pressure fixation and reduced maximum oxygen consumption (42% predicted with no desaturation). The gold standard to properly investigate pulmonary hypertension is with right heart catheterization to assess the pulmonary pressures and pulmonary capillary wedge pressure. The patient had two relative contraindications, the anticoagulant therapy and NYHA IV, but also a complete contraindication of left bundle branch block (due to the risk of complete heart block).
To decrease the pulmonary pressure further, treatment with subcutaneous administration of treprostinil sodium was initiated and titrated to a final dose of 35 ng/kg/minute because efficacy of this treatment had already been demonstrated in previous studies.Citation15–Citation18 The patient demonstrated rapid improvement of his hemodynamic parameters and 6MWT. There was a decrease in RVSP to 60 mmHg and also a further improvement in 6MWT to 450 meters but with a desaturation from 91% to 87%. According to NYHA, the patient at that moment was in class II–III. The patient tolerated the drug well without side effects. His only complaints were of mild erythema and local pain and pain in the lower jaw at the start of mastication for 3 weeks.
After 6 months of medical therapy the patient met the established criteria for PTE, including mean pulmonary artery pressure >25 mmHg, >3 months of effective oral anticoagulation, evidence of surgically accessible thrombi, a beneficial relationship between pulmonary vascular resistance and the anticipated thrombus mass, no comorbidities, and no severe reduction in lung function (). The surgery was successful. The patient no longer needed oxygen therapy, RVSP decreased to 35 mmHg, and 6MWT increased to 490 meters. No further invasive assessments of hemodynamics were performed.
Table 1 Patient’s clinical history
Discussion
Chronic thromboembolism is a frequent cause of progressive hypertension and carries a poor prognosis. In CTEPH, pathological lesions are characterized by organized thrombi tightly attached to the pulmonary arterial medial layer in the elastic pulmonary arteries, replacing the normal intima. These may completely occlude the lumen or form different grades of stenosis, webs, and bands.Citation19 Interestingly, in the nonoccluded areas, a pulmonary arteriopathy indistinguishable from that of pulmonary arterial hypertension (including plexiform lesions) can develop.Citation20 Collateral vessels from the systemic circulation (from bronchial, costal, diaphragmatic, and coronary arteries) can grow to reperfuse, at least partially, the areas distal to complete obstructions.
The true incidence and prevalence of CTEPH are unknown. Originally, it was believed that 0.1%–0.5% of patients who survive an episode of acute pulmonary embolism develop CTEPH.Citation21–Citation23 Defining the true incidence of CTEPH is hampered by the observation that up to two-thirds of these patients have no history of clinically overt acute pulmonary embolism.Citation15–Citation24 It is not clear to what degree the eventual development of CTEPH is determined by each recurrent thromboembolic event, in situ thrombosis, or other changes in the vasculature distal to the vessels initially obstructed by clot.Citation4
In addition to recanalized clot, histological changes similar to those seen in other forms of pulmonary hypertension have been identified in patients with CTEPH. Patients with CTEPH have symptoms of progressive dyspnea, fatigue, and presyncope or loss of consciousness similar to the symptoms of patients with other forms of pulmonary hypertension.Citation25 Many are unaware of prior venous thromboembolic events, and diagnosis is appreciably delayed while other causes of dyspnea are pursued and possibly treated.Citation8 Findings that might narrow consideration of CTEPH are chronic postphlebitic changes of the lower extremity and the presence of pulmonary flow murmurs, described as high pitched and best heard over the lung fields during an inspiratory breath-hold. Recognition of the diagnosis usually follows identification of pulmonary hypertension on the echocardiogram and evidence of chronic thromboembolic disease by ventilation-perfusion scanning or pulmonary angiography.Citation7 Other techniques include contrast-enhanced magnetic resonance (MR) angiography, MR perfusion imaging, phase-contrast imaging of the great vessels, cine imaging of the heart, and combined perfusion-ventilation MR imaging with hyperpolarized noble gases. It is anticipated that MR imaging will play a central role in the initial diagnosis and follow-up of patients with CTEPH.Citation26
PTE is the definitive treatment for chronic pulmonary hypertension resulting from thromboembolic disease.Citation5,Citation6,Citation9 Pulmonary thromboendarterectomy can markedly reduce and even normalize pulmonary hemodynamics. The majority of patients experience improvements in exercise capacity, gas exchange, World Health Organization functional class, and quality of life. In a retrospective follow-up of more than 500 patients who underwent pulmonary thromboendarterectomy at the University of California, San Diego between 1970 and 1994, the probability of survival beyond 6 years was 75 percent.Citation27 Although direct comparison between populations and centers has not been performed, survival at 5 years of patients who were treated with anticoagulation alone in separate series was less than 30 percent.Citation28,Citation29
However, CTEPH may be inoperable owing to surgically inaccessible thrombi or comorbid diseases that confer an unacceptably high risk. Pharmacotherapies, although not yet approved, may be useful in this situation or for treating residual or recurrent pulmonary hypertension following surgery. Vasodilator drugs for pulmonary hypertension are attracting growing interest as potential treatments for CTEPH, because this disease has recently been labelled as a “dual” pulmonary vascular disorder of major vessel obstruction, and remodelling is combined with small vessel arteriopathy that is histologically indistinguishable from the classical pulmonary arteriopathy observed in pulmonary arterial hypertension. Several uncontrolled clinical studies suggest that prostanoids, endothelin-receptor antagonists, and phosphodiesterase type 5 inhibitors may exert hemodynamic and clinical benefits in patients with CTEPH, regardless of whether these patients were considered operable or inoperable.Citation30–Citation35
The only randomized, placebo-controlled clinical trial that has so far addressed the safety and efficacy of medical treatment was BENEFIT (Bosentan Effects in Inoperable Forms of Chronic Thromboembolic Pulmonary Hypertension Trial). BENEFIT employed the dual endothelin-receptor antagonist bosentan. Although hemodynamics improved significantly, the second component of the primary endpoint, exercise capacity, was not met. More evidence is required to resolve whether vasodilator treatments are beneficial for inoperable CTEPH.Citation15–Citation18,Citation36 Given these limited data, further studies are necessary to obtain reliable long-term data on the effects of medical therapies in patients with CTEPH, and these patients should be treated within clinical trials whenever possible. For the present time, no medical therapy has been approved in Europe or the US for CTEPH.
Conclusion
Recent research suggests that the mechanistic view of CTEPH as a disease caused solely by obliteration of central pulmonary arteries due to organized thrombi may have been too simplistic. Pulmonary embolism, either as a single episode or recurrent phenomena, is still thought to be the initiating event in many patients. However, the mechanisms of progressive pulmonary vascular remodelling are still poorly understood, and treatment of CTEPH requires a multidisciplinary approach.
Acknowledgements
PZ, KP, and MK wrote the manuscript. AM, PT, MK, VZ, and NK were the surgeons who evaluated the patient. EK, EM, and MK were responsible for the patient’s medical care. NC was the radiologist who evaluated the radiographic exams. DP and TK assisted in the revision of the manuscript. KZ provided useful insights. EM was responsible for the patient’s medical treatment and provided useful insights.
Disclosure
The authors report no conflicts of interest in this work.
References
- Developing new guidelines for the diagnosis and treatment of pulmonary hypertensionEur Heart J200930202416241819842237
- Task Force for Diagnosis and Treatment of Pulmonary Hypertension of European Society of Cardiology (ESC); European Respiratory Society (ERS); International Society of Heart and Lung Transplantation (ISHLT)GalièNHoeperMMHumbertMGuidelines for the diagnosis and treatment of pulmonary hypertensionEur Respir J20093461219126319749199
- GalièNHoeperMMHumbertMESC Committee for Practice Guidelines (CPG)Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT)Eur Heart J200930202493253719713419
- DartevellePFadelEMussotSChronic thromboembolic pulmonary hypertensionEur Respir J200423463764815083767
- DahmMMayerEEberleBSurgical aspects of pulmonary thrombendarterectomyZentralbl Chir199712286496549412095
- MasudaMMogiKHayashidaNA successful case of pulmonary thromboendarterectomy for chronic thromboembolic pulmonary hypertension with a thrombus in the right ventricleSurg Today199929547848110333425
- HoeperMMDefinition, classification, and epidemiology of pulmonary arterial hypertensionSemin Respir Crit Care Med200930436937519634076
- HoeperMMBarberàJAChannickRNDiagnosis, assessment, and treatment of non-pulmonary arterial hypertension pulmonary hypertensionJ Am Coll Cardiol200954Suppl 1S85S9619555862
- AndoMOkitaYTagusariOSurgical treatment for chronic thromboembolic pulmonary hypertension under profound hypothermia and circulatory arrest in 24 patientsJ Card Surg199914537738510875595
- CouldenRState-of-the-art imaging techniques in chronic thromboembolic pulmonary hypertensionProc Am Thorac Soc20063757758316963537
- LeySLey-ZaporozhanJPittonMBDiagnostic performance of state-of-the-art imaging techniques for morphological assessment of vascular abnormalities in patients with chronic thromboembolic pulmonary hypertension (CTEPH)Eur Radiol9272011 [Epub ahead of print.]
- TorbickiAPerrierAKonstantinidesSGuidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)Eur Heart J2008292276231518757870
- HoeperMMMayerESimonneauGRubinLJChronic thromboembolic pulmonary hypertensionCirculation20061132011202016636189
- RubinLJHoeperMMKlepetkoWCurrent and future management of chronic thromboembolic pulmonary hypertension: from diagnosis to treatment responsesProc Am Thorac Soc2006360160716963541
- Skoro-SajerNBondermanDWiesbauerFTreprostinil for severe inoperable chronic thromboembolic pulmonary hypertensionJ Thromb Haemost20075348348917319903
- IvyDDRosenzweigEBLemariéJCLong-term outcomes in children with pulmonary arterial hypertension treated with bosentan in real-world clinical settingsAm J Cardiol201010691332133821029834
- LangIGomez-SanchezMKneusslMEfficacy of long-term subcutaneous treprostinil sodium therapy in pulmonary hypertensionChest200612961636164316778286
- LangIMManaging chronic thromboembolic pulmonary hypertension: pharmacological treatment optionsEur Respir Rev200918111242820956119
- FedulloPFAugerWRKerrKMRubinLJChronic thromboembolic pulmonary hypertensionN Engl J Med20013451465147211794196
- GalieNKimNHSPulmonary microvascular disease in chronic thromboembolic pulmonary hypertensionProc Am Thorac Soc2006357157616963536
- FedulloPKerrKMKimNHAugerWRChronic thromboembolic pulmonary hypertensionAm J Respir Crit Care Med2011183121605161321330453
- ManeckeGRJrWilsonWCAugerWRJamiesonSWChronic thromboembolic pulmonary hypertension and pulmonary thromboendarterectomySemin Cardiothorac Vasc Anesth20059318920416151552
- FedulloPFAugerWRChannickRNChronic thromboembolic pulmonary hypertensionClin Chest Med19951623533747656546
- LangIMChronic thromboembolic pulmonary hypertension – not so rare after allN Engl J Med2004350222236223815163772
- KählerCMChronic thromboembolic pulmonary hypertension as a cause of dyspnoea in an older patient with a complex historyEur Respir Rev20091811317017320956138
- KreitnerKFKunzRPLeySChronic thromboembolic pulmonary hypertension: assessment by magnetic resonance imagingEur Radiol2007171112116838142
- MadaniMMAugerWRKerretKMPulmonary endarterectomy: a single institution experience in over 2,500 patientsSTS2011 Abstract 89
- JohnsonSRMehtaSGrantonJTAnticoagulation in pulmonary arterial hypertension: a qualitative systematic reviewEur Respir J2006285999100417074918
- MellemkjaerSIlkjaerLBKlaaborgKEPulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. Ten years experience in DenmarkScand Cardiovasc J2006401495316448998
- BresserPFedulloPFAugerWRContinuous intravenous epoprostenol for chronic thromboembolic pulmonary hypertensionEur Respir J20042359560015083760
- NagayaNSasakiNAndoMProstacyclin therapy before pulmonary thromboendarterectomy in patients with chronic thromboembolic pulmonary hypertensionChest200312333834312576349
- HoeperMMKrammTWilkensHBosentan therapy for inoperable chronic thromboembolic pulmonary hypertensionChest20051282363236716236895
- HughesRGeorgePParameshwarJBosentan in inoperable chronic thromboembolic pulmonary hypertensionThorax20056070716061720
- BondermanDNowotnyRSkoro-SajerNBosentan therapy for inoperable chronic thromboembolicpulmonary hypertensionChest20051282599260316236930
- ReichenbergerFVoswinckelREnkeBLong-term treatment with sildenafil in chronic thromboembolic pulmonary hypertensionEur Respir J20073092292717690123
- JaïsXD’ArminiAMJansaPBosentan Effects in iNopErable Forms of chronIc Thromboembolic pulmonary hypertension Study GroupBosentan for treatment of inoperable chronic thromboembolic pulmonary hypertension: BENEFiT (Bosentan Effects in iNopErable Forms of chronIc Thromboembolic pulmonary hypertension), a randomized, placebo-controlled trialJ Am Coll Cardiol200852252127213419095129