Abstract
Background
Patients with unstable angina or myocardial infarction are at risk of acute kidney injury, which may be aggravated by the iodine-containing contrast agent used during coronary angiography; however, the relationship between these two conditions remains unclear.
Objective
The current study investigated the relationship between acute kidney injury and coronary heart disease prior to coronary angiography.
Methods
All patients were evaluated after undergoing coronary angiography in the cardiac catheterization laboratory of the Vinzentius Hospital in Landau, Germany, in 2011. The study group included patients with both acute coronary heart disease and acute kidney injury (as defined according to the classification of the Acute Kidney Injury Group); the control group included patients without acute coronary heart disease. Serum creatinine profiles were evaluated in all patients, as were a variety of demographic and health characteristics.
Results
Of the 303 patients examined, 201 (66.34%) had coronary artery disease. Of these, 38 (18.91%) also had both acute kidney injury and acute coronary heart disease prior to and after coronary angiography, and of which in turn 34 (16.91%) had both acute kidney injury and acute coronary heart disease only prior to the coronary angiography. However, the occurrence of acute kidney injury was not significantly related to the presence of coronary heart disease (P = 0.95, Chi-square test).
Conclusion
The results of this study indicate that acute kidney injury is not linked to acute coronary heart disease. However, physicians should be aware that many coronary heart patients may develop kidney injury while hospitalized for angiography.
Introduction
Physicians often ignore increases – especially minor ones – in the serum creatinine levels of patients with angina pectoris or myocardial infarction.Citation1 However, such increases may be indicative of acute kidney injury, and may therefore be important to investigate in further detail. Unfortunately, there has been little, if any, research on either the relationship between acute kidney injury and acute coronary heart disease or the frequency of acute kidney injury in patients with acute coronary syndrome and acute myocardial infarction.Citation1
Because the diagnosis of acute renal failure has not been standardized, it is difficult to study the outcomes of this condition.Citation1 Rodrigues et al recently reported finding more than 30 definitions of “acute renal failure” in the medical literature;Citation1 this variety causes confusion and makes it difficult to compare the results of multiple studies by different authors.Citation1 For example, although acute renal failure has been described as a complex, multicausal dysfunction with clinical features ranging from small changes in serum creatinine to anuric renal failure, it has also been defined using absolute values or percentile increases in serum creatinine levels or different rates of reduction in urine output.Citation1 Recently, new definitions have been proposed to standardize the diagnosis of acute renal failure.Citation1,Citation2 These establish the concept of acute kidney injuryCitation1 by emphasizing the subtle but important differences between the terms “acute kidney injury” and “acute renal failure.”Citation1 One important distinction between these is that injury precedes failure.Citation1 Several studies have shown that small increases in serum creatinine levels during hospitalization are associated with a worse prognosis for the patient.Citation1
The Acute Kidney Injury (AKIN) group developed a classification system that allows the observation of small changes in serum creatinine over a short period of time to be used in the early diagnosis and treatment of acute kidney injury.Citation1,Citation2 Specifically, the group defined acute kidney injury as a state marked by one of the following three criteria: an absolute increase in serum creatinine level, to >0.3 mg/dL (≥26.4 μmol/L); an increase of more than 50% (or 1.5 times) from baseline over a 48-hour period; or documented oliguria of <0.5 mL/kg/h for >6 hours.Citation1,Citation2 One important feature of this new definition is the concept of staging the severity of acute kidney injury.Citation1
The purpose of the present investigation was to determine the association between the onset of acute kidney injury and acute coronary heart disease. All patients underwent coronary angiography and provided multiple blood samples that could be subjected to a variety of tests, including evaluation of serum creatinine levels, to find out acute kidney injury prior coronary angiography.
Methods
I conducted a retrospective study of all patients (N = 303) admitted to the Vinzentius Hospital (Landau, Germany) in 2011 after undergoing coronary angiography in the cardiac catheterization laboratory. In all, 201 patients were diagnosed with coronary artery disease. The remaining 102 individuals served as the control population; only 19 of these patients suffered from acute kidney injury. Among individuals in the study population, 38 had acute coronary heart disease and were diagnosed with acute kidney injury prior or after to their coronary angiography.
For this study, acute kidney injury was defined in one of two ways, both according to the AKIN classification. For patients whose baseline creatinine levels were known, acute kidney injury was defined as an increase of more than 50% (or 1.5 times) within a 48-hour time frame. For patients with unknown baseline creatinine levels, acute kidney injury was defined as an absolute increase of ≥0.3 mg/dL (≥26.4 μmol/L) from the upper-limit value of the normal range of serum creatinine (0.6–1.2 mg/dL) stated in the Clinical Laboratory and Standards Institute guidelines.Citation3 Prior to normalization, serum creatinine was measured several times in patients in whom levels were elevated. The number of different measurements of serum creatinine obtained for each patient was compared in all patients. Thus, the profile of the serum creatinine was controlled for all patients from admission to discharge from the hospital. By monitoring the course of serum creatinine, I was able to determine whether acute kidney injury occurred before or after coronary angiography.
Chronic renal failure was defined and classified based on the Guidelines of the National Kidney Foundation.Citation4 The glomerular filtration rate was used to calculate the level of kidney function and determine the stage of kidney disease. When possible, the glomerular filtration rate was evaluated three times per patient: before hospitalization, on admission, and prior to discharge from the hospital. Patients with poor kidney values received intravenous infusion therapy with 1000 mL 0.9% sodium chloride both before and after coronary angiography.
Iopamidol (Solutrast®, ALTANA Pharma AG, Konstanz, Germany) was used as a contrast medium during coronary angiography. Both the amount of contrast agent used and the duration of the coronary angiography were measured for each patient. The most recent version of the International Classification of Diseases (ICD) was used to define the symptoms and treatments of stable angina, acute coronary syndrome, ST segment elevation myocardial infarction (STEMI), non-STEMI, and chronic coronary heart disease. Patient electrocardiograms were recorded in the emergency room. Changes to these patterns, such as ST-segment elevation, ST-segment depression, left bundle branch block, R-regression, T-negativity, and presence or absence of cardiac markers in the blood, were used to identify myocardial infarctions.
Coronary angiography, which most often combines diagnosis with percutaneous coronary intervention (ie, angioplasty and stenting), was examined in both groups after past and present coronary angiography with the number of stents in each patient and former bypass surgery. The indication for stent or bypass surgery was placed during coronary angiography by the examiner. Coronary heart disease lesions were classified as being 1-, 2-, or 3-vessel; further, examiners visually estimated the extent of stenosis diameter (as a percentage of the cardiac catheter), as per the stenosis morphology classification recommendations of the American College of Cardiology/American Heart Association.Citation5
For all patients, possible adverse events were documented during the coronary angiography. Angiography was obtained urgently for patients with STEMI, persistent chest pain despite maximal medical therapy, or complications (eg, markedly elevated cardiac markers, the presence of cardiogenic shock, acute mitral regurgitation, and unstable arrhythmias). Patients with uncomplicated non-STEMI or unstable angina whose symptoms have resolved typically undergo angiography within the first 24 to 48 hours of hospitalization to detect lesions that may require treatment. After initial evaluation and therapy, coronary angiography was used in patients with stable angina after a positive ergometric evaluation or for assessment of valvular heart diseases. A cardiac ultrasound was used to assess systolic left ventricular function in all patients.
Basic demographic and health information was collected for each patient at the time of admission and of discharge from the hospital; this included age, gender, whether the patient was taking an angiotensin-converting enzyme inhibitor (ACE), duration of hospital stay, and door-to-needle time for the coronary angiography. Because oliguria was not a problem for any of the patients included in this study, this symptom was not closely examined. However, data were collected on the presence of specific cardiovascular risk factors (CVRFs) such as elevated blood pressure, diabetes mellitus, hyperlipidemia, obesity, smoking, and family history of cardiovascular disease.
For the statistical analysis, I calculated the odds ratio and prior probability (odds) that a patient would have both acute kidney and acute coronary syndrome. All results are expressed as means and standard deviations (SDs). A Mann- Whitney U-test was used to investigate differences between the two treatment groups (in age, total number of diagnoses, indications for coronary angiography, heart rhythm, changes in electrocardiogram, use of ACE inhibitors, serum creatinine levels, total number of CVRFs, length of hospital stay, duration of coronary angiography, amount of contrast medium, door-to-needle time, total number of pretreatments, heart failure, ventricular dysfunction, stenting, presence coronary heart disease, and presence of acute kidney injury).
A Chi-square test was used to investigate the differences in gender distribution, number of diagnoses, indications for coronary angiography, heart rhythm, changes in electrocardiogram, use of ACE inhibitors, CVRF, stages of chronic renal failure, number of pretreatments, heart failure, ventricular dysfunction, stenting, coronary heart disease, and acute kidney injury between study and control group.
I also calculated the overall incidence of acute kidney injury associated with coronary artery disease, as well as associated 95% confidence intervals. Survival rates for both treatment groups were calculated using the Kaplan-Maier method. Significance was defined as P < 0.05.
Results
There were 303 patients included in the current study: 191 (63.04%) men and 112 (36.96%) women. The average age across all study participants was 69.64 ± 12.12 years.
The study group comprised 38 (12.54%) patients who were, on average, 76.90 ± 7.64 years old and who had both acute kidney injury and acute coronary disease during the whole hospital stay. Thirty-four patients (16.91%) had both acute kidney injury and acute coronary disease prior to undergoing a coronary angiography (N = 201). Over half the patients (163, or 53.80%) had acute coronary disease without acute kidney injury; 108 (66.26%) of these were men and 55 (33.74%) were women.
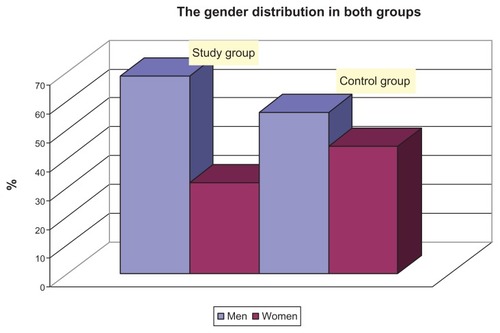
A total of 102 patients (or 33.66%) composed the control group (N = 303). The average age of the control patients was 69.08 ± 13.09. The average age was significantly higher in the study group than in the control group (P = 0.002), but the gender distribution was similar in both groups (P = 0.18) ().
Figure 1 Gender distribution in the study and control groups.
The prior probability (odds) for the occurrence of acute kidney injury in coronary heart disease was found to be 66% (95% CI, 64%–69%). The odds ratio for the occurrence of acute kidney in acute coronary syndrome was 1.0184 (95% CI, 0.5529–1.8759; P = 0.95). No statistical association was found between acute kidney injury and acute coronary syndrome (χ2 = 0.0034, df = 1, P = 0.95).
Stable angina pectoris, sinus rhythm, and T-negativity were more commonly found on the electrocardiograms of patients in the control group than on those of patients in the study group (P = 0.0002, P = 0.02, and P = 0.013, respectively) (). There was only a marginal statistical difference in the number of CVRFs reported for the two groups (P = 0.041) ().
Table 1 Diagnoses and clinical and medical characteristics of patients in the study and control groups
Table 2 Cardiovascular risk factors (CVRF) and their distribution across the study population
Patients in both groups had similar numbers of pretreatments, heart failure, ventricular function, stenting, and acute kidney injury (all P > 0.11) (). However, acute coronary heart disease was more common in the study group (P < 0.01), while patients in the control group were more likely to have chronic coronary heart disease or no heart disease at all (P < 0.01) ().
Table 3 Heart and kidney characteristics of patients in the study and control groups
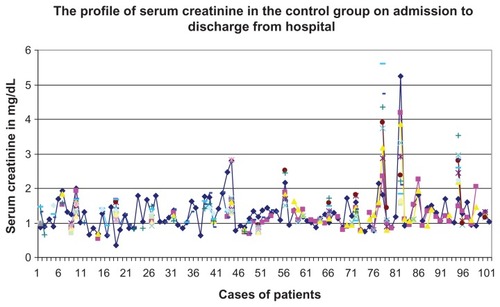
Patients in the study group had significantly higher levels of serum creatinine (1.98 ± 0.92 mg/dL) than those in the control group (1.23 ± 0.57 mg/dL) (P < 0.001) ( and ). The mean value of the number of controls of serum creatinine was 5.67 (SD = 3.89) times in the study group and 3.97 (SD = 4.93) times in the control group. More controls of serum creatinine for each patient were conducted in the study group (P < 0.01).
Figure 2 Serum creatinine profiles of patients in the study group, from hospital admission to discharge.
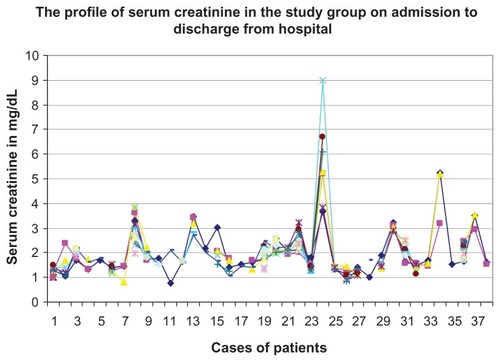
Figure 3 Serum creatinine profiles of patients in the control group, from admission to discharge from hospital.
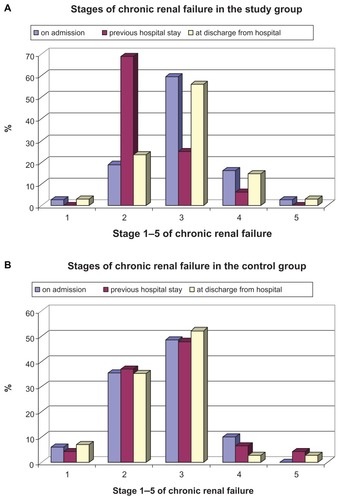
Chronic renal failure was equally common in the control and study groups at admission (Stage 1: P = 0.43; Stage 2: P = 0.06; Stage 3: P = 0.25; Stage 4: P = 0.32; Stage 5: P = 0.10) and during previous hospital stays with statistically significant difference in Stage 2 (Stage 1: P = 0.40; Stage 2: P = 0.03; Stage 3: P = 0.11; Stage 4: P = 0.97; Stage 5: P = 0.40). Statistically significant difference between the groups was found at discharge from the hospital; specifically, the study group had higher levels of Stage 4 chronic renal failure (Stage 1: P = 0.40; Stage 2: P = 0.23; Stage 3: P = 0.72; Stage 4: P = 0.022; Stage 5: P = 0.97) (). No patients suffered an oliguria of <0.5 mL/kg/h for more than 6 hours.
Figure 4 Stages of chronic renal failure in the study (A) and control (B) groups, from admission to discharge from hospital.
Length of hospital stay was significantly greater for patients in the study group (9.45 ± 6.28 days) than for those in the control group (7.24 ± 6.03 days) (P = 0.01). Likewise, door-to-needle time was longer in the study group (52.30 ± 66.24 hours) than in the control group (22.84 ± 39.18 hours) (P = 0.0016).
No adverse events were observed in any of the patients examined. Although more contrast agent was required for patients in the study group (108.37 ± 53.37 mL) than in the control group (93.19 ± 33.67 mL), this difference was not significant (P = 0.32). Also nonsignificant was the difference in duration of coronary angiography (P = 1.0), which was the same, up to 120 minutes, in both groups.
Three patients died during the study; one of these was from the study group (2.63% of the total), and the other two were from the control group (1.96% of the total). Mortality rates were similar in the two groups (P = 0.81). However, survival rates were better in the control group (98.04% [95% CI, 95.32–100.76%]) than in the study group (97.37% [95% CI, 92.21%–102.53%]).
Discussion
Among the patients examined in the current study, one in five suffered from both acute coronary heart disease and acute kidney injury. Nearly all individuals were hypertensive, and many patients displayed multiple risk factors for acute coronary heart disease. Patients in the study group were more likely to have myocardial infarction and acute coronary heart disease. Further, study individuals possessed significantly higher levels of serum creatinine, though the only significance in chronic renal failure was found at hospital discharge and previous hospital stay, and only for individuals with Stage 2 and 4 failure. Cumulatively, these results indicate that kidney damage is a real threat for angina pectoris and heart attack patients, and that care must be taken to minimize risk to these individuals during medical treatment.
In a prospective study of STEMI patients, Goldberg et al found that 9.6% of individuals suffered worsening renal injury (defined arbitrarily as a >0.5 mg/dL elevation of the serum creatinine level at any point during the hospital stay) during their hospital stay.Citation6 In the current study, however, the incidence of STEMI was only slightly higher among patients with acute kidney injury and coronary heart disease, indicating that there is no association between acute kidney injury and acute coronary heart disease. This apparent lack of association between the two diseases, one linking acute renal injury and acute heart disease, was also suggested by the results of a Chi-square analysis (P = 0.95). The discrepancies between this and the Goldberg et al studyCitation6 may stem from the fact that the previous work did not use AKIN criteria for classifying acute kidney injury and, further, there was no specific period of time during which worsening renal function or acute kidney injury were evaluated. The absence of a defined focal period increases the potential for other, unrelated, causes of acute renal injury (such as sepsis during hospitalization) to affect the results.Citation1 In addition, Goldberg et alCitation6 did not routinely collect creatinine measurements after the third day of hospitalization, which may have led to an underestimation of acute kidney injury.Citation1 Goldberg et alCitation6 reported a higher incidence of kidney problems than was found in the current study; thus, they underestimated kidney injury. They collected additional creatinine measurements – and therefore they potentially identified more kidney injuries – so actually their results are even more different from this study than they already seem.
Among elderly patients discharged after hospitalization for acute myocardial infarction, small changes in serum creatinine levels have previously been associated with a higher risk of end-stage renal disease and death.Citation7 Unfortunately, as in the Goldberg et al study,Citation6 the authors of this work did not use AKIN criteria for diagnosing acute kidney injury.Citation1 Thus, it is difficult to compare these previous results with those found in the current study. Further, while all patients in the current study underwent an immediate coronary angiography and tended to be elderly, neither of these conditions was true in the research performed by Newsome et al.Citation7 Another group evaluated the clinical and prognostic relevance of acute kidney injury (defined as a 25% increase over baseline serum creatinine levels) in STEMI complicated by cardiogenic shock. In their study, 55% of patients developed acute kidney injury during their stay in the intensive care unit.Citation8 Again, it is difficult to compare these results to those of the current study, as AKIN criteria were not used to diagnose acute kidney injury.Citation1 Additionally, cardiogenic shock was not observed in any of the patients studied here.
Rather than employing AKIN criteria, Parikh et al defined acute kidney injury as an absolute change in serum creatinine levels;Citation9 they classified the resulting injury as mild (0.3–0.4 mg/dL), moderate (0.5–0.9 mg/dL), or severe (>1.0 mg/dL). Using these criteria, they identified acute kidney injury in 19.4% (7.1% mild, 7.1% moderate, 5.2% severe) of their patients.Citation9 However, the validity of these results has been questioned because the left ventricular ejection fraction was unavailable in 39.4% of the patients without acute kidney injury; multivariate analysis has demonstrated that the ventricular ejection fraction is a strong predictor of long-term survival after an acute myocardial infarction.Citation1,Citation10 In the present investigation, heart failure was more commonly observed in patients with both acute kidney injury and acute coronary heart disease.
Acute kidney injury increases morbidity and mortality, particularly in patients who are critically ill.Citation11 Recognition of this has led to recent efforts (eg, AKIN and RIFLECitation12 [risk, injury, failure, loss, and end-stage renal failure]) to standardize definitions of acute kidney injury; one particularly important goal has been the identification of biomarkers of early kidney injury, as these should facilitate early interventions and prevention of progression to the acute stage of kidney injury.Citation10 Unfortunately, there are currently no data comparing the use of RIFLE and AKIN criteria in patients with acute coronary syndrome or myocardial infarction; further, it is difficult to compare these classification schemes, since the RIFLE criteria, unlike those in the AKIN classification, involve five stages.Citation1 It is also important to note that, while the RIFLE and AKIN criteria are easy to use in a variety of clinical and research settings, they have several limitations.Citation11 For instance, both sets of criteria focus on increases in serum creatinine levels from a hypothetical baseline value, in conjunction with a decrease in urine output. However, these surrogate markers of renal impairment manifest relatively late, after injury has occurred; further, they do not reflect the nature or site of the kidney injury.Citation12
Conclusion
This study shows that acute kidney injury occurs relatively frequently in patients with coronary heart disease, but that the association between these diseases is not statistically significant. However, physicians should still monitor their patients – especially those with angina pectoris and myocardial infarction – for acute kidney injury after the administration of contrast medium.
Disclosure
The author reports no conflicts of interest in this work.
References
- RodriguesFBBruettoRGTorresUSEffect of kidney disease on acute coronary syndromeClin J Am Soc Nephrol201051530153620576827
- BellomoRRoncoCKellumJAAcute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) GroupCrit Care20048R204R21215312219
- HahnJMCheckliste Innere Medizin4th edStuttgartThieme2003
- LeveyASCoreshJBalkENational Kidney FoundationNational Kidney Foundation practice guidelines for chronic kidney disease evaluation, classiffication, and stratificationAnn Intern Med200313913714712859163
- LevineGNBatesERBlankenshipJC2011 ACCF/AHA/SCAI guideline for percutaneous corony intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and InterventionsCirculation2011124257460922064598
- GoldbergAHammermanHPetcherskiSInhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarctionAm Heart J200515033033716086939
- NewsomeBBWarnockDGMcClellanWMLong-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarctionArch Intern Med200816860961618362253
- MarenziGAssanelliECampodonicoJAcute kidney injury in ST-segment elevation acute myocardial infarction complicated by cardiogenic shock at admissionCrit Care Med20103843844419789449
- ParikhCRCocaSGWangYLong-term prognosis of acute kidney injury after acute myocardial infarctionArch Intern Med200816898799518474763
- Bouzas-MosqueraAVázquez-RodríguezJMPeteiroJAcute kidney injury and long-term prognosis after acute myocardial infarctionArch Intern Med20091698719139330
- ChoudhuryDAcute kidney injury: current perspectivesPostgrad Med2010122294021084779
- RicciZCruzDNRoncoCClassification and staging of acute kidney injury: beyond the RIFLE and AKIN criteriaNat Rev Nephrol2011720120821364520