Abstract
Purpose
This study aimed to investigate the prevalence of refractive error and visual acuity among school children in the plateau region of Qinghai, China.
Methods
The school-based, cross-sectional study was performed in Menyuan, Qinghai, China. Three kindergartens and three primary schools were randomly enrolled from both rural areas and county towns. The participants had undergone ophthalmic examinations of the intraocular pressure (IOP), uncorrected visual acuity (UCVA), presenting visual acuity (PVA) and best corrected visual acuity (BCVA), cycloplegic refraction, and axial length (AL). Regression analysis was applied to investigate the potential risk factors affecting the prevalence of various refractive errors.
Results
A total of 3770 children were invited to participate, and 3524 (93.5%) had undergone examination. Among the 3524 children (51.8% boys) with a mean age of 8.3±2.3 years, 1049 (29.8%) had myopia, 30 (0.9%) had high myopia, 1692 (48.0%) had mild hyperopia, 152 (4.3%) had medium to marked hyperopia and 925 (26.2%) had astigmatism. The mean SER was −0.16±1.86 D and decreased with age. The AL increased with age from 21.80±0.59 mm at 4-years to 23.53±1.05 mm at 12-years. The myopia prevalence increased with age from 2.0% at 4 years to 62.8% at 12-years. Myopia was associated with increasing age, county town habitation and girls. Among the 723 participants with PVA 20/40 or worse in one eye, 564 (78.0%) were due to uncorrected refractive error, and 83 (22.0%) were due to undercorrected refractive error. Among the 1049 children with myopia, only 254 wore glasses, and 151 children with PVA had a worse BCVA and did not have accurate spectacles.
Conclusion
The prevalence of myopia is very high among school children in Menyuan. Only 24.2% of myopic children wore glasses, and 59.4% of children did not have accurate spectacles. Strategies to improve access to eye care and affordable glasses are needed.
Introduction
Refractive errors such as hyperopia, myopia and astigmatism are the most general ocular disorders requiring spectacles or contact lenses for optimal vision. Refractive error is caused by the mismatch between the various optical elements of the eye, and the eye’s axial length is one reason.Citation1 Uncorrected errors of refraction are the most common causes of visual disability worldwide.Citation2 The prevalence of refractive error varies with sex, geographic location and age.Citation3–Citation6
Myopia is a widespread refractive error among children and teenagers and is globally recognized as a major twenty-first century public health problem.Citation7,Citation8 Dong et al speculated that the myopia prevalence in 2050 among Chinese children and adolescents aged 3 to 19 years will be approximately 84%.Citation9 Myopia causes further vision challenges because high myopia increases the risk of severe and irreversible vision loss, such as cataracts, glaucoma, retinal detachment, and myopic macular degeneration.Citation10 Thus, preventing the occurrence and development of myopia in children and adolescents is crucial.
Myopia is associated with genetic, behavioral, social and environmental factors, including socioeconomic status, educational attainment,Citation11 time spent outdoors,Citation12 outdoor light intensityCitation13 and time spent reading.Citation14 Although previous studies have provided valuable insights into the etiology of myopia, natural environmental factors have largely been neglected. Many reports have investigated the prevalence of myopia in China’s plains,Citation15–Citation18 but few reports are available on the prevalence of myopia in the northwest plateau.
The Qinghai-Tibet Plateau is the largest plateau worldwide. This area is characterized by low temperature, large temperature differences between day and night, long sunshine, strong solar radiation, high altitude, and thin oxygen. The high altitude and special climate on the Qinghai-Tibet Plateau can affect people’s physical and mental health, such as hypertension,Citation19 cardiovascular diseases,Citation20 cognitive impairmentsCitation21 and depression.Citation22 These specific geographical environments also affect eye health,Citation23 including pterygium, cataracts, and dry eye syndrome. Few reports have examined the prevalence of myopia among children on the Qinghai-Tibet Plateau. Only 3 previous reports on Qinghai-Tibet Plateau school children are available to date. The first study reported that from 2008 to 2009, the prevalence of myopia was 11.8% in primary school students in Qinghai.Citation24 The second study reported that in 2014, among children and adolescents aged 7 to 18 years, the prevalence of myopia was 48.2% in Qinghai and 62.9% in Tibet.Citation25 The third study reported that in 2018, the prevalence of myopia in Tibet was 23.83% among children, with a mean age of 12.69 (±2.88) years.Citation26
No epidemiological study has been performed on refractive error in school children in Qinghai in the past 5 years. We selected Menyuan Hui Autonomous County (Menyuan) in Qinghai Province as the study site. Through ocular examination, we analyzed the refractive status and vision acuity in Qinghai Province.
Materials and Methods
Ethics Statement
This study was approved by the ethics committee of the Affiliated Eye Hospital of Shandong University of Traditional Chinese Medicine and Administration of the Education and School Board of Menyuan. This study adhered to the tenets of the Declaration of Helsinki. Additionally, we obtained written informed consent from at least one parent or legal guardian of each participant.
Recruitment
The pediatric eye study was a school-based, cross-sectional study of children in the northwest Chinese province of Qinghai conducted in Menyuan in September 2019. The sampling frame was based on 11 kindergartens and 12 primary schools with approximately 18,381 children throughout Menyuan, excluding special schools for the disabled. Three kindergartens and 3 primary schools from both rural areas and county towns were selected randomly.
Ophthalmic Examination
The children had undergone the following examinations: distance visual acuity (VA) testing, intraocular pressure (IOP), cover test, slit-lamp examination, fund examination, cycloplegic autorefraction, and axial length (AL).
Before the VA test, the children were asked whether they wore glasses, contact lenses or orthokeratology contact lenses. For the children not wearing glasses, the uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) were tested for both eyes. For those wearing glasses, presenting visual acuity (PVA) was first measured, and then UCVA was measured after removing the glasses for 30 minutes. BCVA was examined by subjective refraction by experienced optometrists. VA was measured using a tumbling “E” chart (#600722; Good-Lite Co., Elgin, IL, USA) (the VA chart was 3 meters away from the child. The lowest line of the chart was approximately as high as the eye of the child. The children were asked to indicate the direction of the “E” opening starting on the first line of the chart (VA: 20/100) and moving on to the next line if none or one character of the line was incorrect. When the child incorrectly described at least 2 characters, VA was recorded as the value of the previous line. If the children could not read 20/100 lines at a distance of 3 meters, the test was repeated at one meter. If a single line could not be read at this distance, vision was assessed by counting fingers, hand movement or light perception.
The purpose of IOP measurement and slit-lamp examination was to exclude contraindications for mydriasis. Cycloplegia was achieved after instilling one drop of topical anesthetic ((Minims Oxybuprocaine Hydrochloride 0.4% w/v; Santen Pharmaceutical Co., Ltd; Japan) and one drop of cyclopentolate hydrochloride (Minims; 1% w/v; Alcon Laboratories, Inc; USA). The children were administered two drops of cyclopentolate hydrochloride 5 min apart. Once cycloplegia had been established, at least 20 min after instilling the eye drops, autorefraction was performed. Full cycloplegia was considered when the pupil diameter reached 6 mm or more and the light reflex disappeared. The presence of refraction with cycloplegia was assessed using an autorefractor (ARK-1; NIDEK, Tokyo, Japan). AL was measured using an IOL Master-500 (Carl Zeiss Meditec AG, Jena, Germany).
All the above instruments were calibrated before the ocular examination. All the examinations were performed by board-certified ophthalmologists and certified optometrists.
Definitions
Refraction measurements were converted into spherical equivalent refraction (SER), which was calculated as the spherical value plus half of the astigmatism value. Medium to marked hyperopia was defined as >+2.0 dioptres (D), and mild hyperopia was defined as >+0.50 D and ≤+2.0 D, in one or both eyes if neither eye was myopic. Emmetropia was defined as >−0.50 D and ≤+0.50 D, in both eyes. Myopia was defined as≤−0.5 D and high myopia as≤−6.0 D, in one or both eyes. Astigmatism was defined as a myopic cylindrical refractive error≤−0.75 D in either eye. All refractive errors were measured under cycloplegia.
For the students not wearing glasses, PVA is equivalent to UCVA; for those wearing glasses, PVA is equivalent to VA of wearing spectacles.
Statistical Methodology
Statistical analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, IL). For normally distributed continuous variables, the data were expressed as means ± standard deviation (SD). Categorical variables were expressed as frequencies of the total. The risk factors associated with myopia were determined by two-level multivariate logistic regression analysis. First, we performed univariate binary logistic regression analysis to evaluate the potential association. Multivariate logistic regression was then performed to analyze all statistically significant factors found in the univariate analysis. For continuous variables, we conducted univariate analysis to identify correlations and then performed linear regression analysis. In our results, odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to evaluate myopia risk factors. OR<1.0 and P<0.05 demonstrated that a parameter was a protective factor, while OR>1.0 and P<0.05 demonstrated that a parameter was a risky factor. Statistical tests were two-sided, and P<0.05 was considered statistically significant.
Results
Participant Characteristics
During September 2019, 3770 participants were recruited. Of these, 233 (6.18%) children refuse to participate and not signed informed consent, 13 (0.34%) with an IOP≥25 mmHg in one or both eyes were excluded from the study, and 3524 completed the ophthalmic examinations, resulting in a complete examination rate of 93.47%. The demographic characteristics of the study population are described in .
Table 1 The Demographic Characteristics of the Study Participants
The mean age of the 3524 participants was 8.3±2.3 years (4–12 years). Of the 3524 participants, 1798 (51.0%) resided in rural areas, and 1726 (49.0%) resided in county towns. The participants comprised more boys (1825; 51.8%) than girls (1699; 48.2%) among, but no significant difference was found in the sex between participants in rural areas (53.4% boys) and county towns (50.1% boys) (χ2= 3.787; P=0.052).
Ocular Parameters
A significant difference was found in SER between the right and left eyes (t=2.071; P=0.038). The mean SER of the right eyes was −0.16±1.86 D (median: 0.38 D; range: −16.5 D to +11.75 D) and that of the left eyes was −0.05±1.80 D (median: 0.38 D; range: −13.25 D to +12.00 D). Pearson correlation analysis of the SER showed a high correlation (r=0.914; P=0.000) between the right and left eyes. Therefore, only the SER of the right eyes was analyzed in our study.
The mean SER of children in the county towns (−0.44±2.08 D) showed a greater refractive change toward myopia than that of children in rural areas (0.02±1.68 D) (t=−5.983; P=0.000). The SER decreased within children aged 4 to 12 years in county towns (F=47.385; P=0.000) and rural areas (F=44.944; P=0.000) (). In the county towns, the SERs were 1.25±0.59, 1.19±0.55, 1.26±1.51, 0.41±0.97, 0.16±1.77, −0.62±1.91, −1.19±2.09, −1.72±2.34 and −1.80±1.96 D in children aged 4 to 12 years. In the rural areas, the SERs were 1.18±0.55, 1.17±0.55, 1.09±0.90, 0.81±0.72, 0.42±1.83, 0±1.55, −0.58±1.60, −0.79±1.87 and −0.95±1.72 D in children aged 4 to 12 years.
Figure 1 Spherical equivalent (SE, D) distribution of right eyes, (A) stratified by age and region of habitation, (B) stratified by age and genders in the Qinghai children. The Y axis shows the mean and 95% confidence interval.
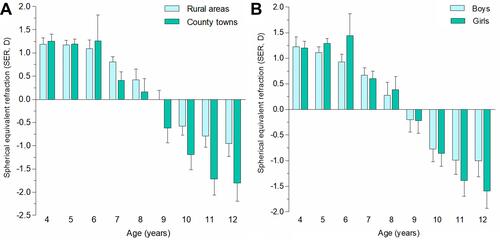
The SER was −0.09±1.79 D in boys and −0.24±1.94 D in girls, and the difference was statistically significant (t=2.040; P=0.041). The SER decreased with age in both boys and girls but was more pronounced in girls (). In boys, the SERs were 1.22±0.68, 1.11±0.59, 0.93±0.64, 0.67±0.85, 0.28±1.83, −0.2±1.69, −0.77±1.8, −0.99±2.11 and −1±1.78 D in those aged 4 to 12 years. In girls, the SERs were 1.201±0.46, 1.29±0.45, 1.44±1.49, 0.6±0.86, 0.39±1.81, −0.22±1.73, −0.86±1.86, −1.39±2.12 and −1.59±1.9 D in those aged 4 to 12 years.
The AL was significantly longer with each older age, from 21.80±0.59 mm in 4-year-olds to 23.53±1.05 mm in 12-year-olds (F=98.006; P=0.000). The AL of children in county towns (23.25±1.20 mm) was longer than that in rural areas (22.81±1.03 mm) (t=−7.156; P=0.000) (). In the county towns, the ALs were 21.8±0.6, 21.93±0.72, 22.37±0.93, 22.72±0.72, 22.84±1.02, 23.36±0.96, 23.62±1.10, 23.92±1.13 and 23.83±1.21 mm in children aged 4 to 12 years. In the rural areas, the ALs were 21.81±0.59, 22.01±0.7, 22.26±0.69, 22.33±0.84, 22.63±1.04, 22.84±0.96, 23.19±0.98, 23.32±1.02 and 23.34±0.89 mm in children aged 4 to 12 years.
Figure 2 Axial length (AL, mm) distribution of right eyes, (A) stratified by age and region of habitation, (B) stratified by age and genders in the Qinghai children. The Y axis shows the mean and 95% confidence interval.
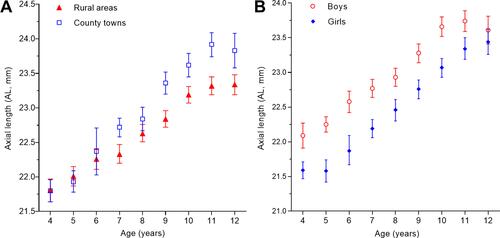
The difference in the AL between boys (23.16±1.07 mm) and girls (22.70±1.11 mm) was statistically significant (t=10.930; P=0.000) (). In boys, the ALs were 22.09±0.61, 22.25±0.57, 22.58±0.64, 22.77±0.77, 22.93±0.95, 23.28±0.96, 23.66±1.00, 23.74±1.09 and 23.61±1.10 mm in those aged 4 to 12 years. In girls, the ALs were 21.59±0.48, 21.58±0.71, 21.88±0.73, 22.19±0.74, 22.46±1.08, 22.76±0.96, 23.07±1.01, 23.34±1.08 and 23.44±0.99 mm in those aged 4 to 12 years.
Prevalence of Refractive Errors
The prevalence of myopia was 29.8% (95% CI: 20.7%, 39.0%) in the 3524 children (). The prevalence of myopia increased with age from 2.0% (95% CI: −1.7%, 6.2%) in 4-year-olds to 62.8% (95% CI: 42.6%, 83.6%) in 12-year-olds ( and ). Univariate binary logistic regression analysis demonstrated that the prevalence of myopia was significantly associated with girls (P=0.043), increasing age (P=0.000) and habitation in county towns (P=0.000). The results of multivariate binary regression analysis revealed that the prevalence of myopia was higher in female students than in male students, and female students had a 1.22-fold higher risk of myopia than male students [OR: 1.22 (95% CI: 1.03, 1.45); P=0.043]. The results also indicated that the prevalence of myopia increased with age [OR: 1.84 (95% CI: 1.75, 1.93); P=0.000]. Furthermore, children living in county towns [OR: 1.53 (95% CI: 1.29, 1.80); P=0.000] had a higher risk of myopia than those living in rural areas.
Table 2 Distribution of Prevalence of Various Refractive Error in Different Genders and Regions
Table 3 Distribution of Prevalence of Various Refractive Errors at Different Ages Between 4–12 Years Old
Figure 3 Prevalence of high myopia, myopia, emmetropia, mild hyperopia and medium to marked hyperopia, stratified by age in the Qinghai children. Participants were classified according to SER into high myopia (SER≤−6.0D), myopia (SER≤−0.5 D), emmetropia (SER>−0.50 D and ≤+0.5 D), mild hyperopia (SER>+0.50 D and ≤+2.0 D), and medium to marked hyperopia (>+2.0 D).
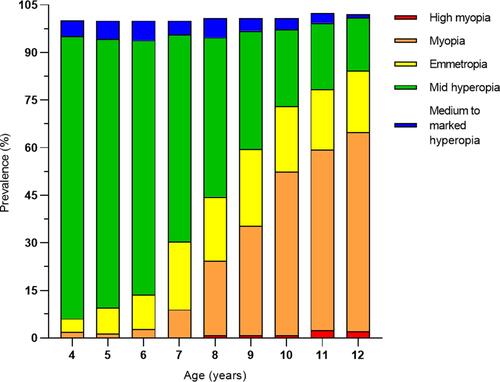
The prevalence of high myopia was 0.9% () in total and increased from 0% in the 4-year-old group to 2.1% in the 12-year-old group (). In univariate binary logistic regression analysis, the prevalence of high myopia was significantly associated with increasing age (P=0.000), but it was not significantly associated with region of habitation (P=0.229) or sex (P=0.191). As the children became older, their risk of high myopia increased [OR: 1.67 (95% CI: 1.33, 2.09); P=0.000].
The prevalence of mild hyperopia was 48.0% in total () and decreased from 89.1% in the 4-year-old group to 16.7% in the 12-year-old group (). Univariate binary logistic regression analysis showed that the prevalence of mild hyperopia was significantly associated with increasing age (P=0.000), but it was not significantly associated with region of habitation (P=0.512) or sex (P=0.970). As the children became older, their risk of mild hyperopia decreased (OR: 0.60 [95% CI: 0.57, 0.62]; P=0.000).
The prevalence of medium to marked hyperopia was 4.3% in total () and decreased from 5% in the 4-year-old group to 1.0% in the 12-year-old group (). Univariate analysis showed that the prevalence of medium to marked hyperopia was significantly associated with increasing age (P=0.001), but was not associated with region of habitation (P=0.672) or sex (P=0.405). As children became older, their risk of medium to marked hyperopia decreased (OR: 0.89 [95% CI: 0.83, 0.95]; P=0.001).
The prevalence of astigmatism was 26.2% in total (), and the mean value of astigmatism was 0.43±0.51 D (median: −0.25 D; range: −7.00 D to 0 D). Univariate analysis showed that the prevalence of astigmatism was significantly associated with age [regression coefficient B=−0.02; standardized coefficients beta=−0.10; P=0.000; (95% CI: −0.03, −0.02)], region of habitation (P=0.009), sex (P=0.033) and myopic refractive error [regression coefficient B=0.02; standardized coefficients beta=0.07; P=0.000; (95% CI: 0.01, 0.03)]. In binary regression analysis, older age [OR: 1.09 (95% CI: 1.04, 1.13); P=0.000], habitation in county towns [OR: 1.19 (95% CI: 1.02, 1.39); P=0.000], and more myopic refractive error [B=−1.06; OR: 0.90 (95% CI: 0.86, 0.94); P=0.000] were associated with a higher astigmatism prevalence. Girls [OR: 0.85 (95% CI: 0.73, 0.99); P=0.035] were associated with a lower prevalence of astigmatism.
Visual Acuity and Glasses Wear
In high myopia, myopia and medium to marked hyperopia, the uncorrected visual acuity (UCVA) and presenting visual acuity (PVA) were significantly lower than those in emmetropia, while no difference was found in UCVA (P=0.105) and PVA (P=0.193) between mild hyperopia and emmetropia. The best corrected visual acuity (BCVA) in high myopia (P=0.000) and medium to marked hyperopia (P=0.000) was significantly lower than that in emmetropia, but no difference was found in the BCVA in mild hyperopia (P=0.866), myopia (P=0.283) and emmetropia. High myopia and medium to marked hyperopia affected the children’s vision.
The VA results are presented in . Refractive errors were the main reason for UCVA 20/40 or worse. Of the 3524 participants, 2917 (82.8%) had a UCVA of 20/30 or better in at least one eye, 607 (17.2%) had a UCVA of 20/40 or worse in the better eye, and 411 (11.7%) had a PVA of 20/40 or worse in the better eye. With best correction, VA 20/40 or worse in the better eye decreased to 40 (1.1%). Among the 891 participants with UCVA 20/40 or worse in one eye, 812 (91.1%) were caused by uncorrected refractive error. Among the 723 participants with PVA 20/40 or worse in one eye, 564 (78.0%) were caused by uncorrected refractive error, and 83 (22.0%) were caused by undercorrected refractive error.
Table 4 The Uncorrected, Present and Best Corrected Visual Acuity (UCVA, PVA and BCVA) Distribution
All the participants were asked to bring their spectacles to the school on the day of the ocular examination. In the 3524 participants with reliable VA, glasses were only used by 288 (8.2%). Two hundred fifty-four participants wore glasses due to myopia, which was the main reason for them to wear glasses. Additionally, among the 1049 myopic participants, 795 (75.8%) participants presented without glasses. Furthermore, 302 (38.0%) participants without glasses had a UCVA of 20/40 or worse in the better eye (). Among 254 (24.2%) myopic participants who wore glasses, 44 (17.3%) had a PVA 20/40 or worse in the better eye, and 151 (59.4%) presenting with PVA had a worse BCVA and did not have accurate spectacles.
Table 5 The Distribution of Presenting Visual Acuity (PVA) and Best Corrected Visual Acuity (BCVA) Among Myopic Participants
Discussion
Menyuan is located on the high-altitude Qinghai-Tibet Plateau, and the environment is expected to affect the eye health of children living there, but little is known about the prevalence of refractive error in the northwest plateau region. Therefore, we investigated the characteristics of refractive error among school-aged children.
In our study, the boys living in the county town and with older age had longer eyes. Higher AL was related to older age of the children.Citation27 In the current study, the AL became significantly longer with each older age from 21.80±0.59 mm in 4-year-olds to 23.53±1.05 mm in 12-year-olds. Male sex was a significant and independent factor for a longer axial length.Citation28 In the present data, the AL was longer in boys than in girls, a finding that agrees with a previous study.Citation28,Citation29 The mean AL in our study was 23.61±1.10 mm for boys and 23.44±0.99 mm for girls at 12 years old. The values were slightly shorter than the ALs obtained in one Eastern Chinese study on children of the same age (boys: 24.14±1.01 mm; girls: 23.69±1.10 mm). We found the same phenomenon as in previous studiesCitation29 and at the same age: boys have longer ALs and higher refractive power than girls; however, the reasons must be further clarified.
The prevalence of myopia among 4- to 12-year-old children in Qinghai was 29.8%. Qian et alCitation26 reported that the prevalence of myopia was 23.83% in Tibet (12.69±2.88 years old). Xie et alCitation30 defined VA<20/20 and SER<−0.5D as myopia and found that the myopia prevalence of children aged 7–13 years in Chongqing was 33.1%. Wang et alCitation16 defined myopia as SER≤−0.5 D and UCVA≤20/25 and reported that the myopia prevalence was 41.4% in Yiwu among 5- to 12-year-old children. Both Qinghai and Tibet are economically backward plateau regions, and they have similar myopia prevalences. The prevalence of myopia in Qinghai is not significantly lower than that in Chongqing and Yiwu economically developed areas. Our study, together with previous studies in school children, suggests that myopia is a serious public health problem in China, including plateau regions. The government should be aware of these findings and adopt measures to prevent myopia among children in China’s plateau regions.
Qinghai is characterized by low temperature, large temperature differences between day and night, long sunshine, and strong solar radiation, making children spend relatively less time in outdoor activities and increasing the possibility of myopia. Studies have shown that scleral hypoxia is one cause of myopia.Citation31 The high altitude of Menyuan and low oxygen content in the air affect the oxygen supply of the eyes, a factor that may also affect myopia in children.
Myopia was significantly associated with increasing age, county town region of habitation and girls, findings that are consistent with previous study findings.Citation3–Citation5 The learning burden increases with age, leading to more hours on near work activities and reduced time on outdoor activities, a situation considered to be an important risk factor for the occurrence of myopia.Citation32,Citation33 The environment is an important factor in the prevalence of myopia, and county town children have a higher risk of myopia than rural area children subjected to the county town environment and learning pressure.Citation3,Citation17 Regarding sex differences, girls tend to spend more time reading and writing and perform less outdoor activities, making them more vulnerable to developing myopia.Citation34
As children become older, their risk of high myopia increases. The prevalence of high myopia increased from 0.8% in 8-year-old patients to 2.1% in 12-year-old patients. In 12-year-olds, the prevalence of high myopia was lower than that in Beijing,Citation35 Qingdao,Citation36 Yiwu and Hong Kong,Citation16,Citation37 and similar to that in Mongolia.Citation38 In our study, the prevalence of high myopia began to increase between the ages of 11 and 12 years in Qinghai, beginning later than in the developed plains areas of Beijing,Citation35 Qingdao,Citation26 Yiwu,Citation16 and Hong Kong,Citation37 but close to the same age in the underdeveloped plains areas of YunnanCitation39 and Mongolia.Citation38 Early myopia onset generally leads to rapid and longer duration for myopia progression and, consequently, a higher risk of becoming high myopic later in life.
The prevalence of astigmatism varies according to geographical position and population. The astigmatism prevalence (26.2%, ≤−0.75 D, 4–12 years of age) was higher in Yunnan (12.7%, ≤−0.75 D, 13–14 years of age),Citation40 Beijing (10%, ≤−0.75 D, 5–15 years of age),Citation41 and Wenzhou (20.3%, ≤−0.75 D, 6–9 years of age).Citation42 Our prevalence was lower than that in other studies, where the prevalence was 42.7% in Guangzhou (≤−0.75 D, 5–15 years old) and 36.3% in Shandong (≤−0.75 D, 4–18 years of age).Citation4,Citation43 Different studies have reported contradictory findings, and we detected correlations with age, region of habitation, sex and myopia refractive error, unlike those reported by Zhao et al, Lin et al and Fotouhi et al.Citation41,Citation42,Citation44
Uncorrected/undercorrected refractive error (particularly myopia) is the main reason for UCVA/PVA 20/40 or worse.Citation43,Citation45,Citation46 This type of vision problem can be easily solved by prescribing a pair of suitable spectacles. In the present study, only 24.2% of myopia students wore glasses, and 59.4% of them did not have accurate spectacles. Our finding was comparable to another study by Chin MP and colleagues, in which 64% of Chinese children in remote areas did not have appropriate correction.Citation15 The wearing glass rate was lower than that in developed provinces of China (70.1% among those aged 5–18 years).Citation16 In Menyuan, many children are “left-behind children” whose parents are too busy to care about their children’s eye health. The price of glasses is more expensive, and the inconvenience of wearing glasses may also be the reason for not wearing glasses among myopic children. Another potential reason for glasses nonwear among myopic children may be related to the widespread misunderstanding in China that young children wearing glasses might damage their visual acuity.Citation47 The lower appropriate rate of glasses use among Qinghai children may also be associated with poor access to health services.Citation48,Citation49
The projected number of children and adolescents 7 to 18 years of age affected by reduced visual acuity is approximately 152 million in 2020 and approximately 180 million in 2030.Citation50 Visual impairment affects an individual’s quality of life and impedes access to education and employment.Citation51 Therefore, in Qinghai, we should adopt certain measures and strategies, such as strengthening children’s vision screening, improving the local medical level, popularizing the knowledge of eye care, enhancing the awareness of children and parents of eye care, and providing optician subsidies, to reduce and delay the occurrence of myopia in children and adolescents.
Our study has potential limitations. Children aged 4–6 years are young, and many parents refuse to participate in the eye study because of concerns about pupil dilation. Therefore, relatively few children were included, which may have affected the calculation of the prevalence of refractive error. Additionally, astigmatism was related to sex, place of residence, age, and myopia, but some studies differ from ours, likely because of the different age groups and different criteria for astigmatism definition.
Conclusion
Refractive error in 4- to 12-year-old children, particularly children with myopia, is common in Northwest Plateau China. In our study, 29.8% of 4- to 12-year-old children had myopia, 0.9% had high myopia, 4.3% had medium to marked hyperopia, and 26.2% had astigmatism. Uncorrected/undercorrected refractive error (especially myopia) was the main reason for PVA 20/40 or worse. A total of 75.8% of myopic children did not wear glasses, and 59.4% of myopic children had inaccurate spectacles. The prevention and treatment of myopia are critical. We should focus more on the eyesight health of children in the northwest plateau region to further explore opportunities and methods to prevent and control myopia.
Data Sharing Statement
Please contact author for data requests.
Ethics Approval and Consent to Participate
The ethics committee of Affiliated Eye Hospital of Shandong University of Traditional Chinese Medicine.
Consent for Publication
The authors consent for publication.
Patient Consent
Obtained.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to acknowledge the support and participation of the Affiliated Eye Hospital of Shandong University of Traditional Chinese Medicine, the Administration of the Education and School Board of Menyuan, the schools, the children, and their parents and guardians in the China Eye Study.
Disclosure
The authors declare no conflicts of interest.
Additional information
Funding
References
- Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96(3):301–309. doi:10.1111/aos.13603
- Bourne RR, Stevens GA, White RA, et al. Causes of vision loss worldwide 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339–349. doi:10.1016/S2214-109X(13)70113-X
- Pan CW, Wu RK, Li J, Zhong H. Low prevalence of myopia among school children in rural China. BMC Ophthalmol. 2018;18(1):140. doi:10.1186/s12886-018-0808-0
- Wu JF, Bi HS, Wang SM, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS One. 2013;8(12):e82763. doi:10.1371/journal.pone.0082763
- Czepita M, Czepita D, Safranow K. Role of gender in the prevalence of myopia among polish schoolchildren. J Ophthalmol. 2019;2019:9748576. doi:10.1155/2019/9748576
- Tideman JW, Polling JR, Voortman T, et al. Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur J Epidemiol. 2016;31(5):491–499. doi:10.1007/s10654-016-0128-8
- Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi:10.1016/j.ophtha.2016.01.006
- Hopf S, Pfeiffer N. Epidemiology of myopia. Ophthalmologe. 2017;114(1):20–23. doi:10.1007/s00347-016-0361-2
- Dong L, Kang YK, Li Y, Wei WB, Jonas JB. prevalence and time trends of myopia in children and adolescents in china: a systemic review and meta-analysis. Retina. 2020;40(3):399–411. doi:10.1097/IAE.0000000000002590
- Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157(1):9–25.e12. doi:10.1016/j.ajo.2013.08.010
- Ghorbani Mojarrad N, Plotnikov D, Williams C, Guggenheim JA; UK Biobank Eye and Vision Consortium. Association between polygenic risk score and risk of myopia. JAMA Ophthalmol. 2019;138(1):7–13. doi:10.1001/jamaophthalmol.2019.4421
- Lingham G, Mackey DA, Lucas R, Yazar S. How does spending time outdoors protect against myopia? A review. Br J Ophthalmol. 2020;104(5):593–599. doi:10.1136/bjophthalmol-2019-314675
- Wu PC, Chen CT, Lin KK, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125(8):1239–1250. doi:10.1016/j.ophtha.2017.12.011
- Lin Z, Gao TY, Vasudevan B, et al. Near work, outdoor activity, and myopia in children in rural China: the Handan Offspring Myopia Study. BMC Ophthalmol. 2017;17(1):203. doi:10.1186/s12886-017-0598-9
- Chin MP, Siong KH, Chan KH, Do CW, Chan HH, Cheong AM. Prevalence of visual impairment and refractive errors among different ethnic groups in schoolchildren in Turpan, China. Ophthalmic Physiol Opt. 2015;35(3):263–270. doi:10.1111/opo.12193
- Wang J, Ying GS, Fu X, et al. Prevalence of myopia and vision impairment in school students in Eastern China. BMC Ophthalmol. 2020;20(1):2. doi:10.1186/s12886-019-1281-0
- Hu M, Zhou Y, Huang S, et al. Population prevalence of myopia, glasses wear and free glasses acceptance among minority versus Han schoolchildren in China. PLoS One. 2019;14(4):e0215660. doi:10.1371/journal.pone.0215660
- Thorn F, Chen J, Li C, et al. Refractive status and prevalence of myopia among Chinese primary school students. Clin Exp Optom. 2020;103(2):177–183. doi:10.1111/cxo.12980
- Shen Y, Chang C, Zhang J, Jiang Y, Ni B, Wang Y. Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: a Cross-Sectional Study. Environ Health Prev Med. 2017;22(1):19. doi:10.1186/s12199-017-0634-7
- Riley CJ, Gavin M. Physiological changes to the cardiovascular system at high altitude and its effects on cardiovascular disease. High Alt Med Biol. 2017;18(2):102–113. doi:10.1089/ham.2016.0112
- Yan X. Cognitive impairments at high altitudes and adaptation. High Alt Med Biol. 2014;15(2):141–145. doi:10.1089/ham.2014.1009
- Wang J, Zhou Y, Liang Y, Liu Z, Large Sample A. Survey of Tibetan people on the Qinghai-Tibet plateau: current situation of depression and risk factors. Int J Environ Res Public Health. 2019;17(1):289. doi:10.3390/ijerph17010289
- Jha KN. High altitude and the eye. Asia Pac J Ophthalmol (Phila). 2012;1(3):166–169. doi:10.1097/APO.0b013e318253004e
- Xie HL, Xie ZK, Ye J, Yang XJ, Qu J. Analysis of correlative factors and prevalence on China’s youth myopia. Zhonghua Yi Xue Za Zhi. 2010;90(7):439–442.
- Dong YH, Liu HB, Wang ZH, Xu RB, Yang ZP, Ma J. The epidemic status and secular trends of myopia prevalence for Chinese children and adolescents aged 7–18 years from 2005 to 2014. Zhonghua Yu Fang Yi Xue Za Zhi. 2017;51(4):285–289.
- Qian X, Liu B, Wang J, et al. Prevalence of refractive errors in Tibetan adolescents. BMC Ophthalmol. 2018;18(1):118. doi:10.1186/s12886-018-0780-8
- Ip JM, Huynh SC, Robaei D, et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11–15-year-old Australian children. Eye (Lond). 2008;22(5):649–656. doi:10.1038/sj.eye.6702701
- Terasaki H, Yamashita T, Yoshihara N, Kii Y, Sakamoto T. Association of lifestyle and body structure to ocular axial length in Japanese elementary school children. BMC Ophthalmol. 2017;17(1):123. doi:10.1186/s12886-017-0519-y
- Lu TL, Wu JF, Ye X, et al. Axial length and associated factors in children: the Shandong Children Eye Study. Ophthalmologica. 2016;235(2):78–86. doi:10.1159/000441900
- Xie Z, Long Y, Wang J, Li Q, Zhang Q. Prevalence of myopia and associated risk factors among primary students in Chongqing: multilevel modeling. BMC Ophthalmol. 2020;20(1):146. doi:10.1186/s12886-020-01410-3
- Wu H, Chen W, Zhao F, et al. Scleral hypoxia is a target for myopia control. Proc Natl Acad Sci USA. 2018;115(30):E7091–E7100. doi:10.1073/pnas.1721443115
- He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–1148. doi:10.1001/jama.2015.10803
- Ho CL, Wu WF, Liou YM. Dose-response relationship of outdoor exposure and myopia indicators: a systematic review and meta-analysis of various research methods. Int J Environ Res Public Health. 2019;16(14):E2595. doi:10.3390/ijerph16142595
- Li Y, Liu J, Qi P. The increasing prevalence of myopia in junior high school students in the Haidian District of Beijing, China: a 10-year population-based survey. BMC Ophthalmol. 2017;17(1):88. doi:10.1186/s12886-017-0483-6
- Guo Y, Duan JL, Liu LJ, et al. High myopia in greater Beijing school children in 2016. PLoS One. 2017;12(11):e0187396. doi:10.1371/journal.pone.0187396
- Sun JT, An M, Yan XB, Li GH, Wang DB. Prevalence and related factors for myopia in school-aged children in Qingdao. J Ophthalmol. 2018;2018:9781987. doi:10.1155/2018/9781987
- Lam CS, Lam CH, Cheng SC, Chan LY. Prevalence of myopia among Hong Kong Chinese schoolchildren: changes over two decades. Ophthalmic Physiol Opt. 2012;32(1):17–24. doi:10.1111/j.1475-1313.2011.00886.x
- Guo K, Yang DY, Wang Y, et al. Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert Children Eye Study. Ophthalmol Vis Sci. 2015;56(3):1769–1774. doi:10.1167/iovs.14-15737
- Qian DJ, Zhong H, Li J, Niu Z, Yuan Y, Pan CW. Myopia among school students in rural China (Yunnan). Ophthalmic Physiol Opt. 2016;36(4):381–387. doi:10.1111/opo.12287
- Pan CW, Ke C, Hu DN, Li J, Zhong H. Iris colour and astigmatism among Chinese teenagers. Br J Ophthalmol. 2019;103(12):1810–1814.
- Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: results from Shunyi District, China. Am J Ophthalmol. 2000;129(4):427–435. doi:10.1016/S0002-9394(99)00452-3
- Lin Y, Jiang D, Li C, et al. Simultaneous changes in astigmatism with noncycloplegia refraction and ocular biometry in Chinese primary schoolchildren. J Ophthalmol. 2019;2019:5613986. doi:10.1155/2019/5613986
- He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci. 2004;45(3):793–799. doi:10.1167/iovs.03-1051
- Fotouhi A, Hashemi H, Yekta AA, Mohammad K, Khoob MK. Characteristics of astigmatism in a population of schoolchildren, Dezful, Iran. Optom Vis Sci. 2011;88(9):1054–1059. doi:10.1097/OPX.0b013e318221727d
- Signes-Soler I, Hernández-Verdejo JL, Estrella Lumeras MA, Tomás Verduras E, Piñero DP. Refractive error study in young subjects: results from a rural area in Paraguay. Int J Ophthalmol. 2017;10(3):467–472.
- Signes-Soler I, Piñero DP, Murillo MI, Tablada S. Prevalence of visual impairment and refractive errors in an urban area of Mexico. Int J Ophthalmol. 2019;12(10):1612–1617. doi:10.18240/ijo.2019.10.14
- Li L, Lam J, Lu Y, et al. Attitudes of students, parents, and teachers toward glasses use in rural China. Arch Ophthalmol. 2010;128(6):759–765. doi:10.1001/archophthalmol.2010.73
- Jing F. Health sector reform and reproductive health services in poor rural China. Health Policy Plan. 2004;19(suppl 1):i40–49. doi:10.1093/heapol/czh044
- Wong HT, Guo YQ, Chiu MY, Chen S, Zhao Y. Spatial illustration of health-care workforce accessibility index in China: how far has our 2009 health-care reform brought us? Aust J Rural Health. 2016;24(1):54–60. doi:10.1111/ajr.12198
- Sun HP, Li A, Xu Y, Pan CW. Secular trends of reduced visual acuity from 1985 to 2010 and disease burden projection for 2020 and 2030 among primary and secondary school students in China. JAMA Ophthalmol. 2015;133(3):262–268. doi:10.1001/jamaophthalmol.2014.4899
- Selvarajah S, Dunt DR, Marella M, et al. Vision impairment and refractive errors in refugees presenting to community optometry clinics in Victoria, Australia. Clin Exp Optom. 2020;103(5):668–674. doi:10.1111/cxo.13010
