Abstract
Purpose
The burden of kidney dysfunction (KD) is rapidly increasing in developing countries due to an ongoing epidemic of hypertension and diabetes. We aimed to evaluate the prevalence and associated factors of KD among population with hypertension and/or diabetes from primary care setting.
Methods
This study was part of a cross-sectional study conducted in Northwest China, which aimed to investigate the epidemiological status of hypertension and other chronic noninfectious diseases. Subjects aged ≥18 years old with hypertension and/or diabetes were included in this study. KD was defined as estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73m2. Least absolute shrinkage and selection operator and multivariable logistic regression were used to identify factors associated with KD. Sensitivity analysis was performed by comparing the results of different estimated equations for GFR.
Results
A total of 8899 participants with hypertension and/or diabetes were included. Prevalence of KD was 8.69% (n=144) among patients with both hypertension and DM, 3.36% (n=198) among patients with only hypertension, and 5.22% (n=70) among patients with only diabetes. Women showed higher prevalent KD than men. Modifiable factors independently associated with KD among patients with hypertension and/or diabetes included physical activity, duration of hypertension or DM, anemia, fasting plasma glucose and triglyceride. Results of different estimated equations showed similar trends of difference in the prevalence of KD among groups.
Conclusion
KD is common in patients with hypertension and/or DM in Northwest China. More attention should be paid to high-risk patients, especially to those with co-existence of hypertension and DM. Control of blood glucose and triglyceride may further improve KD management in this patient population.
Introduction
Chronic kidney disease (CKD) has been shown to be a risk factor for cardiovascular diseases and death.Citation1 Early-stage CKD is usually asymptomatic and is often ignored.Citation2 Most patients detected for CKD are already in an irreversible stage, which leads to occurrence of complications, and some of them have even progressed to end-stage renal disease (ESRD), requiring renal replacement therapy. Hence, the burden of CKD has become a huge public health challenge worldwide.
Prevalence of CKD varies widely among geographic regions, partly due to different lifestyles and economic conditions. Previous studies have shown a heavy burden of CKD in developing countries and low- and middle-income regions (LMIRs), which is responsible for more than two thirds of overall CKD,Citation3 with the prevalence of 17.95% in Iran, and 8.66% and 13.1% in Africa and South Asia, respectively.Citation4 Prevalence of CKD is about 10.8% in the general population of China,Citation5 and even higher in the elderly.Citation6 With changes in lifestyle and acceleration of aging, incidence of CKD is increasing as well, and risk factors are also changing, with an increasing trend of metabolic disease-related kidney disease.Citation7 Studies have demonstrated that hypertension and diabetes mellitus (DM) play strong roles in kidney disease. More than 40% of diabetic patients in America and JapanCitation8,Citation9 and 25% of hypertensive patients in TurkeyCitation10 are reported to be affected by kidney damage. Diabetic kidney disease and hypertensive nephropathy account for more than 40% of CKD in Chinese hospitalized patients.Citation7 Furthermore, it is noteworthy that hypertension and DM have become leading causes of CKD in Chinese elderly.Citation11 Rapid increase in incidence of hypertension and DM, even at younger age, over the past two decadesCitation12 indicates that prevalence of CKD at population level may have been affected.
Kidney dysfunction (KD) is an important component of CKD. Although the prevalence of KD has previously been reported, few studies have focused on the population with hypertension and DM, especially in developing countries and LMIRs. Therefore, we aimed to investigate the prevalence and the related factors of KD in the population with hypertension and/or DM from the primary care setting of Xinjiang, a less-developed region in Northwest China, where hypertension and DM are highly prevalent and poorly managed (low awareness, treatment, and control rates).Citation13,Citation14
Materials and Methods
Study Design and Population
This study is part of a cross-sectional study conducted in Emin county between March and November 2019, and aimed to investigate epidemiological status of hypertension and other chronic noninfectious diseases. Emin county, in Northern Xinjiang, is home to a total population of over 160,000, living in urban, agricultural, and stock-raising settings. Economic level of Emin county is close to the average of Xinjiang, making the study population characteristics well representative.
In the original investigation, we used multistage stratified random sampling method to obtain study population. At the first stage, six districts were randomly selected in Emin county. At the second stage, we selected 10 villages/communities from each of district. At the third stage, individuals were randomly chosen from each village/community. Local inhabitants (residing at current address for ≥6 months) aged ≥15 years and agreed to participate and sign an informed consent form were investigated. The study was conducted in accordance with Declaration of Helsinki and approved by the Ethics Committee at the People’s Hospital of Xinjiang Uygur Autonomous Region.
Eligibility Criteria in the Present Study
In this study, participants were included if they were aged ≥18 years with hypertension and/or diabetes. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, and/or diastolic blood pressure (DBP) ≥90 mmHg, and/or use of antihypertensive agents within two weeks, and/or self-reported history of hypertension. Diabetes mellitus was defined as self-reported history of diabetes and/or a FPG ≥7 mmol/L.
Data Collection and Measurement
Data were collected by trained investigators using standardized questionnaires, including demographic characteristics, socioeconomical status, health-related behaviors, and medical history.
Before blood pressure (BP) measurement, each participant was asked to avoid alcohol, cigarettes, coffee or tea consumption. BP was measured thrice using with the OMRON HBP-1300 Professional Portable Blood Pressure Monitor (OMRON, Kyoto, Japan) on the right arm positioned at heart level after the participant was sitting at rest for five minutes, with 30 seconds between each measurement. The average of the three readings was used for analysis. Height and weight were measured to the nearest 0.1 cm and 0.1 kg, respectively, with participants in lightweight clothing and without shoes. Body mass index (BMI) was calculated by dividing weight by height-squared (kg/m2). Waist circumference was measured at the midpoint between the lower rib and upper margin of the iliac crest to the nearest 0.1 cm at the end of a normal expiration.
All subjects were fasted for ≥8 hours, and a 5-mL fasting blood sample was collected. Serum creatinine was measured by enzymatic method (sarcosine oxidase enzymatic analysis). Fasting plasma glucose (FPG) was tested using glucose oxidase method. Total cholesterol (TC) and triglycerides (TG) were measured with commercially available reagents.
Definition of KD
KD was defined as eGFR <60 mL/min/per 1.73m2. eGFR was calculated using modified modification of diet in renal disease (MDRD) equation on the basis of data from Chinese adults.Citation15 As a sensitivity analysis, we also examined eGFR calculated using chronic kidney disease epidemiology collaboration (CKD-EPI) creatinine equation.Citation16
Other Variables
Additional variables included age, gender, duration of hypertension and DM (years), smoker (yes/no), alcohol intake (yes/no), living regions (agricultural, stock-raising, or urban setting), educational level (primary and lower, junior high, or senior high and higher), occupational (manual or intelligent), ethnicity (Han, Kazakh, or others), marital status (single, married, or separated). Participants who have smoked at least 20 packets of cigarettes in their lifetime were defined as smoker. Alcohol intake was defined as consuming alcoholic beverage at least once per week in the past month. Central obesity was defined as waist circumference ≥85 cm for women and ≥90 cm for men. A positive cardiovascular disease (CVD) was considered as any self-reported myocardial infarction, coronary revascularization or stroke. Anemia was defined if hemoglobin <120 g/L for men or <110 g/L for women. Physical activity was evaluated by the Global Physical Activity Questionnaire and divided into three categories based on WHO’s (2010) physical activity recommendations.Citation17 Sleep quality was assessed using Pittsburgh Sleep Quality Index (PSQI), and classified into very good, fair good, fair bad and very bad categories if PSQI score of 0–4, 5–9, 10–14, and ≥15, respectively.Citation18
Statistical Analysis
Continuous variables were summarized as mean ±standard deviation (SD) or median (interquartile range) and compared using Student's t-test or Mann–Whitney U-test, whereas categorical variables were expressed as absolute numbers with percentage and compared using chi-squared test. To evaluate associated factors of KD in patients with different disease status, data was divided into three analytic sets: set 1 including participants with both hypertension and DM; set 2 including those with hypertension alone; set 3 including those with DM alone. First, we used least absolute shrinkage and selection operator (LASSO) regression to identify predictive features of KD. Then, multivariable logistic regression model including those variables was fitted to identify factors associated independently with KD, with results presented as odds ratio (OR) with 95% confidence interval (CI). CKD-EPI equation is also commonly used to estimate GFR and has been well confirmed for epidemiological investigation and clinical practice.Citation16 Therefore, we redefined KD based on CKD-EPI and repeated the above analysis process as sensitivity analysis for prevalence and associated factors of KD. Statistical analyses were conducted using SPSS 20.0 for Windows (IBM Corporation, Armonk, NY, USA) and R version 4.0.3. A two-sided P<0.05 was considered to be significant.
Results
Prevalence of Kidney Dysfunction Based on MDRD Equation
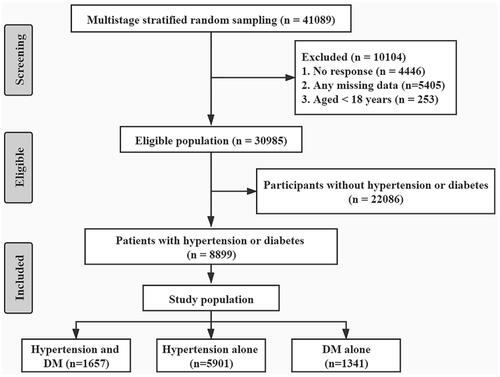
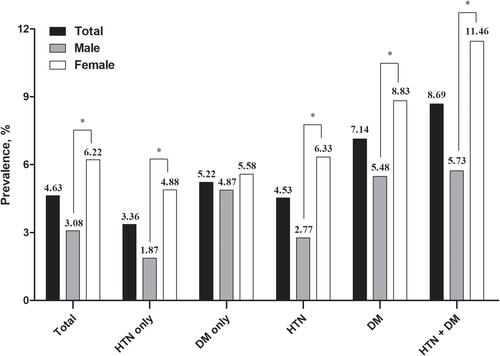
A total of 41,089 people were recruited in the original investigation and 36,643 completed the survey with a response rate of 89.2%. After exclusion, we finally included 8899 participants with hypertension and/or DM in this study (). Among the included participants, 5901 (66.3%) had hypertension alone, 1341 (15.1%) had DM alone, and 1657 (18.6%) had both hypertension and DM. KD was detected in 412 (4.63%) of study participants. As shown in , prevalence of KD was as high as 8.69% (n=144) among patients with both hypertension and DM, 3.36% (n=198) among those with hypertension alone and 5.22% (n=70) among those with DM alone. Women had higher prevalent KD than men. Prevalence of KD in participants from both genders, different age groups, living region, ethnicity and educational status groups were shown in .
Table 1 Prevalence of Kidney Dysfunction in the Study Population
Subject Characteristics
Among included participants, 7558 (84.9%) had hypertension and 2998 (33.7%) had DM. Mean age of all participants was 56.61±12.11 years, mean BMI was 27.22±4.33 kg/m2 and almost two thirds (65.1%) had central obesity and 49.3% participants were women. 881 (9.9%) participants reported a positive history of CVD. Compared with non-KD participants, patients with KD were older and had higher proportion of women (48.5% vs 66.3%, P<0.001). Proportion of coexistent hypertension and DM was higher in those with KD. Patients with KD were more likely to be diabetic and have higher FPG level. History of CVD and dyslipidemia were also higher in KD group. Details of characteristics for study population were shown in . Moreover, among participants with hypertension alone, treatment and control rates of hypertension were 46.1% and 18.5%, respectively; median duration of hypertension was 4.38 years. Among participants with DM alone, median duration of DM was 2.66 years.
Table 2 Characteristics of Participants with Hypertension and/or Diabetes
Associated Factors of KD
LASSO regression generated 15, 17, and six factors for analytic set 1 (for coexistent hypertension and DM), 2 (for hypertension alone) and 3 (for DM alone), respectively. In multivariable logistic regression models by including parameters produced by LASSO regression, among participants with both hypertension and DM, factors associated with KD included age, gender, duration of hypertension, anemia, FPG and TG (). Among participants with hypertension alone, age, gender, living region, physical activity, duration of hypertension and FPG were independently associated with KD (). Among participants with DM alone, associated factors for KD were duration of DM, living region and physical activity ().
Table 3 Factors Associated with Kidney Dysfunction Among Patients with Hypertension and Diabetes
Table 4 Factors Associated with Kidney Dysfunction Among Patients with Only Hypertension
Table 5 Factors Associated with Kidney Dysfunction Among Patients with Only Diabetes
Sensitivity Analysis
Sensitivity analysis was performed by redefined KD based on CKD-EPI equation; results were shown as supplementary Materials. In CKD-EPI analysis, prevalence of KD was higher than MDRD analysis (7.09% vs 4.63%), and the lowest prevalence was found in patients with hypertension alone (5.37%), while the highest was in patients with both hypertension and DM (12.61%). Results of the two equations showed similar trends in difference in the prevalence of KD among groups (Figure S1 and ). In multivariable analysis based on CKD-EPI, most of the associated factors identified by MDRD analysis remained consistent and significant (Tables S1–S3). Moreover, in CKD-EPI analysis, occupation, CVD and physical activity were significantly associated with KD among patients with both hypertension and DM; alcohol intake was associated with KD among patients with hypertension alone; age and female were associated with KD among patients with DM alone.
Discussion
To our knowledge, this is the first study with large sample size to investigate the prevalence and associated factors of KD on population with hypertension and/or DM in a primary care setting in Northwest China. The present study showed that prevalence of KD was higher in the population with both hypertension and DM than in the population with hypertension or DM alone. There were significant differences between genders, with higher prevalence in women. Age was positively correlated with KD. In addition, there were also differences of the prevalence of KD among population from different living regions and ethnic groups. Age, gender, living region, physical activity, duration of hypertension or DM, anemia, FPG and TG were independently associated with KD in the population with hypertension and/or DM.
Previous studies investigating kidney disease in China focused mainly on general or elderly population. Zhang et al reported in a nationally representative investigation that prevalence of eGFR <60 mL/min/per 1.73m2 in Chinese aged ≥18 years is 1.7%.Citation5 It is 1.7% and 2.1% in population from BeijingCitation19 and Tibet,Citation20 respectively. This is similar to other developing countries,Citation21,Citation22 whereas lower than developed countries (6.11% in Sweden and 6.5% in America).Citation23,Citation24 Hypertension and DM have been demonstrated as the main pathologies contributing to kidney disease.Citation25 In the past two decades, hypertension and DM has increased rapidly in China,Citation12 indicating that prevalence of kidney diseases at population level may have been affected. Cao et al reported that diabetes and hypertension have become leading causes of CKD in elderly Chinese patients.Citation11 It can be expected that prevalence of CKD will increase rapidly, with the acceleration of aging and the expansion of patients with hypertension and DM. Screening of CKD is cost-effective for patients with DM or hypertension in the US.Citation26 Therefore, it may be effective for reducing public health burden in the primary care-setting to take screening and preventative measures for kidney disease in this high-risk population in developing countries, such as China.
Age has been indicated to be independently associated with CKD in the general population; it is also an independent risk factor for KD in patients with hypertension and DM in our study. In normal individuals, there is progressive deterioration of renal function as decrease in renal mass and increased incidence of sclerotic glomeruli with age;Citation27 and this will be exacerbated when complicated with hypertension or DM. Moreover, extension of duration of hypertension and DM can also aggravate kidney damage. Further studies to evaluate effects of management of hypertension and DM on occurrence and development of kidney disease in this population are needed.
Consistent with previous studies in other countries, which reported that women have a higher prevalence of KD, gender difference is also observed in our study. However, gender-different mechanism in KD remains unclear still. Difference in hormone metabolism and glomerular structure and hemodynamics between male and female may serve as part of the reason.Citation28 Moreover, imbalance in obesity between genders may also play a role. A meta-analysis showed that obesity in females is associated with a higher risk of kidney disease than in males.Citation29 In the present study, proportion of obesity is higher in women than in men as well (41.2% vs 35.3%).
National investigation in China showed that prevalence of CKD in rural regions is lower than that in urban regions.Citation5 Similar results are found in our study, which suggests that living regions may be associated with KD. Environmental factors may be part of the explanation for the higher prevalence in urban region. It has been demonstrated in cohort studies that increase in the PM2.5 is associated with higher risk of CKD and ESRD.Citation30,Citation31 A study from Taipei also shows that there is positive association between traffic-related air pollution and kidney damage.Citation32 In addition, differences in lifestyle and dietary habits between living regions may also be involved in the process.
The relationship between physical activity and KD remains inconsistent, and it is varied among different patient groups in the present study. Exercise may protect renal function by lowering BMI and reducing the risk of hypertension and DM,Citation33 and this indirect effect may be attenuated in patients who have been suffering from hypertension and DM. Recently, a cohort study shows that highly active people have lower risk for developing CKD, compared with inactive people.Citation34 However, Tannor et al reported that there is no independent association between physical activity and CKD in Ghanaian patients with hypertension and DM.Citation35 Among the nondiabetic population, FPG and prediabetes are significantly associated with coronary artery disease and stroke.Citation36 It is noteworthy that FPG is independently associated with CKD in hypertensive patients who are without DM in the present study. Glycemic control can help prevent onset of CKD in individuals with DM.Citation37 However, it needs to be further explored in hypertensive patients. Consistent with a previous study performed in elderly population,Citation38 the present study observed that anemia is significantly associated with KD. Anemia is a common comorbidity in patients with chronic kidney disease, mainly due to impaired production of erythropoietin by kidney damage; hepcidin and other factors are also involved.Citation39 Patients with anemia should be aware of presence of kidney disease. In addition, the association between anemia and the risk of incident CKD needs to be verified in a longitudinal study.
As expected, prevalence of KD in our study is significantly higher for CKD-EPI analysis than for MDRD analysis. In sensitivity analysis, occupation, history of CVD and alcohol intake are significantly associated with KD, which may be due to the larger sample size of KD cases based on CKD-EPI equation. These factors have been shown to be directly or indirectly associated with KD in patients with DM or kidney diseases.Citation40,Citation41
Limitations
Although multistage random sampling in general population with a good sample size, several limitations warrant discussion for our study. First, causal inference between associated factors and KD needs to be further explored, because of the cross-sectional design of the present study. Second, only one county was selected, limiting the generalization of the results, although the county has a good representation. Third, single measurements of serum creatinine without repeated examination may have resulted in misclassification of individuals with KD. Fourth, because of the lack of urine test, we were only able to report prevalence of KD defined by eGFR, regardless of urinary protein. Fifth, although LASSO regression was used for screening potential factor, it is difficult to find all associated factors for KD; in addition, mediating effects between variables were also failed to resolve. Future study needs to take this into account. Sixth, although recognized methods applied for blood pressure and glucose measurements, diagnosis of hypertension and DM might be biased due to lack of repeated measurements from different days. In addition, oral glucose tolerance test should also be considered for DM diagnosis in future investigations.
Conclusion
There is high prevalence of KD among patients with hypertension and DM in the primary care setting in Northwest China. Modifiable factors associated with KD among patients with hypertension and/or DM include living region, physical activity, anemia, FPG and TG, which may provide clues for prevention and intervention for kidney disease in this population in order to reduce the burden of public health care in less-developed regions.
Data Sharing Statement
The datasets are available from the corresponding author upon reasonable request.
Ethical Approval
The present study was approved by the Ethics Committee at the People’s Hospital of Xinjiang Uygur Autonomous Region (IRB approval number: 2019020327). Informed consent was obtained from all individual participants included in the study.
Acknowledgments
The authors are very much grateful to all study participants for their kind cooperation/participation in the study.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Herzog CA, Asinger RW, Berger AK, et al. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2011;80(6):572–586. doi:10.1038/ki.2011.223
- Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–272. doi:10.1016/S0140-6736(13)60687-X
- Mills KT, Xu Y, Zhang W, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88(5):950–957. doi:10.1038/ki.2015.230
- Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease - A systematic review and meta-analysis. PLoS One. 2016;11(7):e0158765. doi:10.1371/journal.pone.0158765
- Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379(9818):815–822. doi:10.1016/S0140-6736(12)60033-6
- Wei H, Yan Y, Gong J, Dong J. Prevalence of kidney damage in Chinese elderly: a large-scale population-based study. BMC Nephrol. 2019;20(1):341. doi:10.1186/s12882-019-1525-5
- Huang YM, Xu D, Long J, et al. Spectrum of chronic kidney disease in China: a national study based on hospitalized patients from 2010 to 2015. Nephrology. 2019;24(7):725–736. doi:10.1111/nep.13489
- Laliberté F, Bookhart BK, Vekeman F, et al. Direct all-cause health care costs associated with chronic kidney disease in patients with diabetes and hypertension: a managed care perspective. J Manag Care Pharm. 2009;15(4):312–322. doi:10.18553/jmcp.2009.15.4.312
- Ohta M, Babazono T, Uchigata Y, Iwamoto Y. Comparison of the prevalence of chronic kidney disease in Japanese patients with Type 1 and Type 2 diabetes. Diabet Med. 2010;27(9):1017–1023. doi:10.1111/j.1464-5491.2010.03049.x
- Altun B, Süleymanlar G, Utaş C, et al. Prevalence, awareness, treatment and control of hypertension in adults with chronic kidney disease in Turkey: results from the CREDIT study. Kidney Blood Press Res. 2012;36(1):36–46. doi:10.1159/000339025
- Cao Y, Li W, Yang G, Liu Y, Li X. Diabetes and hypertension have become leading causes of CKD in Chinese elderly patients: a comparison between 1990–1991 and 2009–2010. Int Urol Nephrol. 2012;44(4):1269–1276. doi:10.1007/s11255-012-0194-0
- Zhang L, Wang H. Chronic kidney disease epidemic: cost and health care implications in China. Semin Nephrol. 2009;29(5):483–486. doi:10.1016/j.semnephrol.2009.06.012
- Zhou M, Astell-Burt T, Bi Y, et al. Geographical variation in diabetes prevalence and detection in China: multilevel spatial analysis of 98,058 adults. Diabetes Care. 2015;38(1):72–81. doi:10.2337/dc14-1100
- Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi:10.1161/CIRCULATIONAHA.117.032380
- Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–2944. doi:10.1681/ASN.2006040368
- Lv JC, Zhang LX. Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. 2019;1165:3–15.
- World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: World Health Organization Copyright © World Health Organization 2010; 2010.
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
- Zhang L, Zhang P, Wang F, et al. Prevalence and factors associated with CKD: a population study from Beijing. Am J Kidney Dis. 2008;51(3):373–384. doi:10.1053/j.ajkd.2007.11.009
- Chen W, Liu Q, Wang H, et al. Prevalence and risk factors of chronic kidney disease: a population study in the Tibetan population. Nephrol Dial Transplant. 2011;26(5):1592–1599. doi:10.1093/ndt/gfq608
- Varma PP, Raman DK, Ramakrishnan TS, Singh P, Varma A. Prevalence of early stages of chronic kidney disease in apparently healthy central government employees in India. Nephrol Dial Transplant. 2010;25(9):3011–3017. doi:10.1093/ndt/gfq131
- Alam A, Amanullah F, Baig-Ansari N, Lotia-Farrukh I, Khan FS. Prevalence and risk factors of kidney disease in urban Karachi: baseline findings from a community cohort study. BMC Res Notes. 2014;7(1):179. doi:10.1186/1756-0500-7-179
- Gasparini A, Evans M, Coresh J, et al. Prevalence and recognition of chronic kidney disease in Stockholm healthcare. Nephrol Dial Transplant. 2016;31(12):2086–2094. doi:10.1093/ndt/gfw354
- Wang F, He K, Wang J, et al. Prevalence and risk factors for CKD: a comparison between the adult populations in China and the United States. Kidney Int Rep. 2018;3(5):1135–1143. doi:10.1016/j.ekir.2018.05.011
- Nugent RA, Fathima SF, Feigl AB, Chyung D. The burden of chronic kidney disease on developing nations: a 21st century challenge in global health. Nephron Clin Pract. 2011;118(3):c269–c277. doi:10.1159/000321382
- Hoerger TJ, Wittenborn JS, Segel JE, et al. A health policy model of CKD: 2. The cost-effectiveness of microalbuminuria screening. Am J Kidney Dis. 2010;55(3):463–473. doi:10.1053/j.ajkd.2009.11.017
- Lindeman RD, Tobin J, Shock NW. Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc. 1985;33(4):278–285. doi:10.1111/j.1532-5415.1985.tb07117.x
- Silbiger SR, Neugarten J. The role of gender in the progression of renal disease. Adv Ren Replace Ther. 2003;10(1):3–14. doi:10.1053/jarr.2003.50001
- Wang Y, Chen X, Song Y, Caballero B, Cheskin LJ. Association between obesity and kidney disease: a systematic review and meta-analysis. Kidney Int. 2008;73(1):19–33. doi:10.1038/sj.ki.5002586
- Chan TC, Zhang Z, Lin BC, et al. Long-term exposure to ambient fine particulate matter and chronic kidney disease: a cohort study. Environ Health Perspect. 2018;126(10):107002. doi:10.1289/EHP3304
- Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. Particulate matter air pollution and the risk of incident CKD and progression to ESRD. J Am Soc Nephrol. 2018;29(1):218–230. doi:10.1681/ASN.2017030253
- Chen SY, Chu DC, Lee JH, Yang YR, Chan CC. Traffic-related air pollution associated with chronic kidney disease among elderly residents in Taipei City. Environ Pollut. 2018;234:838–845. doi:10.1016/j.envpol.2017.11.084
- Park S, Lee S, Kim Y, et al. Causal effects of physical activity or sedentary behaviors on kidney function: an integrated population-scale observational analysis and Mendelian randomization study. Nephrol Dial Transplant. 2021. doi:10.1093/ndt/gfab153
- Parvathaneni K, Surapaneni A, Ballew SH, et al. Association between midlife physical activity and incident kidney disease: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2021;77(1):74–81. doi:10.1053/j.ajkd.2020.07.020
- Tannor EK, Sarfo FS, Mobula LM, Sarfo-Kantanka O, Adu-Gyamfi R, Plange-Rhule J. Prevalence and predictors of chronic kidney disease among Ghanaian patients with hypertension and diabetes mellitus: a multicenter cross-sectional study. J Clin Hypertens. 2019;21(10):1542–1550. doi:10.1111/jch.13672
- Mutie PM, Pomares-Millan H, Atabaki-Pasdar N, et al. An investigation of causal relationships between prediabetes and vascular complications. Nat Commun. 2020;11(1):4592. doi:10.1038/s41467-020-18386-9
- James MT, Hemmelgarn BR, Tonelli M. Early recognition and prevention of chronic kidney disease. Lancet. 2010;375(9722):1296–1309. doi:10.1016/S0140-6736(09)62004-3
- Ji A, Pan C, Wang H, et al. Prevalence and associated risk factors of chronic kidney disease in an elderly population from Eastern China. Int J Environ Res Public Health. 2019;16(22):22. doi:10.3390/ijerph16224383
- Atkinson MA, Warady BA. Anemia in chronic kidney disease. Pediatr Nephrol. 2018;33(2):227–238. doi:10.1007/s00467-017-3663-y
- Moazzeni SS, Arani RH, Hasheminia M, Tohidi M, Azizi F, Hadaegh F. High incidence of chronic kidney disease among Iranian diabetic adults: using CKD-EPI and MDRD equations for estimated Glomerular Filtration Rate. Diabetes Metab J. 2021;45(5):684–697. doi:10.4093/dmj.2020.0109
- Kaze FF, Maimouna M, Beybey AF, et al. Prevalence and determinants of chronic kidney disease in urban adults’ populations of northern Cameroon. Clin Exp Nephrol. 2021;25(7):718–726. doi:10.1007/s10157-021-02036-5