Abstract
Objectives
Restoration of circulation is crucial in the surgical patient management. Colloids and crystalloids are widely used for blood volume therapy. We reviewed recent trials to evaluate efficacy and safety of hydroxyethyl starch (HES) 130/0.4 during surgery.
Material and methods
A subjective, not systematic, review of literature was performed. Papers were searched to answer questions about efficacy of HES, its impact on coagulation and inflammation and its effects on pulmonary mechanics and renal function.
Conclusions
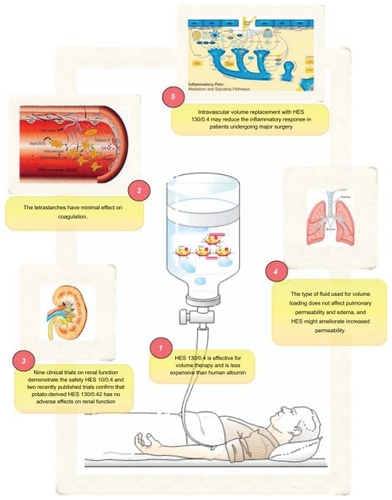
HES 130/0.4 is effective for volume therapy and is less expensive than human albumin. Its effects on coagulation and renal function are manageable; it may ameliorate pulmonary permeability and reduce inflammation.
Hydroxyethyl starch (HES) solutions are synthetic colloids used to correct hypovolemia. HES contains glycogen-like modified natural polysaccharidesCitation1,Citation2 and can be classified according to their molecular weight (MW), concentration, and degree of substitution. Hydroxyethyl starch 130/0.4 (mean molecular weight, 130 kd; degree of substitution, 0.4) is a relatively new medium-molecular-weight HES solution. The development of newer starch-based plasma volume expanders has been driven by the need to improve safety and pharmacological properties while maintaining the volume efficacy of previous HES generations. Reductions in MW and molar substitution (MS) have led to products with shorter half-lives, improved pharmacokinetic and pharmacodynamic properties, and fewer side effects.Citation3 Earlier products were all derived from amylopectin extracted from waxy maize starch but it is inaccurate to refer to HES as if they were only one homogenous product because modifications to MW and the degree and pattern of substitution result in distinct and observable differences between and within the different generations of HES.
The same is true for starches of similar structure that have been derived from different source materials: waxy maize and potato. Two third-generation starches based on these two materials are currently available in various formulations. According to the results of one study, potato and waxy maize-derived HES solutions are not bioequivalent.Citation4 Therefore, findings obtained from studies using one type may not be valid for the other.
Early experimental studies produced reports of increased mortality rates in mice that received HES solutions before an endotoxin challenge and in a rat endotoxin model, HES 10% (200/0.5) was less effective than albumin in preventing lipopolysaccharide- induced myocardial dysfunctionCitation5. There is continuing concern regarding possible adverse effects of HES solutions including coagulopathy, anaphylactoid reactions, and renal impairment.
It has been suggested that the modern generation HES solutions, 6% HES (130/0.4), may be less likely to induce nephrotoxicity and may impair blood coagulation less than other HES solutions and thus, may be used in larger doses without increasing the risk of postoperative bleeding.
In this paper we review some of the relevant articles regarding the use of HES 130/0.4 during surgery, looking for answers to five of the most asked questions on this subject.
Is HES 130/0.4 more efficient in plasma substitution than other colloids?
A recent systematic review of randomized clinical studies on the use of fluid therapy in various types of surgical procedures found no evidence to recommend one type of fluid therapy over another. There was not sufficient evidence to provide guidance on the optimal amount of fluid to use in elective surgical procedures.Citation6 It was therefore concluded that guidelines for perioperative fluid management must be procedure-specific; in the absence of firm evidence for one approach or another, individualized, goal-directed fluid administration should be used. Currently, it appears that a restrictive rather than a liberal fluid regimen is beneficial in patients undergoing colorectal surgery. Conversely, patients suffering from systemic inflammation appear to benefit from aggressive fluid replacement, as demonstrated by Rivers et al.Citation7 This is in line with the conclusion of Brandstrup, who critically evaluated the evidence behind current standard fluid therapy and the effect of fluid therapy on the outcomes of surgery.Citation8 The latter author reported that choice of standard fluid therapy is not generally evidence-based and that methodological flaws during attempts to restrict fluid therapy actually result not in restriction but simply replacement of lost fluids. Therefore, it is recommended to replace lost fluid and avoid fluid overload, which echoes earlier recommendations to adopt goal-directed intraoperative fluid therapy.Citation9
Despite the absence of clear recommendations for any particular fluid therapy, there is plentiful debate about the relative merits of crystalloid or colloid, and even about different types of colloids. As recently remarked by Boldt in an editorial, “Researchers who show crystalloid to be superior always find crystalloid superior, whereas colloid supporters always favor colloids”.Citation10
Adequate restoration of intravascular volume remains the crucial therapeutic maneuver in managing the surgical patient. It is generally believed that three to four times more crystalloid than colloid volume is needed to achieve an equivalent plasma volume expansion. However, in the SAFE trial,Citation11 in which fluid administration was blinded, the ratio of albumin to saline was 1:1.4 and thus much less than expected. While the choice between colloid and crystalloid solutions continues to generate controversy, the dispute has been enlarged to a colloid/colloid debate (eg, dextrans, gelatins, HES solutions).
Vanhoonacker et alCitation12 studied 157 electively scheduled patients randomly allocated to 6% HES (n = 85) or gelatine (n = 72) CPB (cardiopulmonary bypass) priming. According to their data, HES 130/0.4 is a safe alternative to gelatine pump prime with a volume effect persisting longer in the postoperative phase, mandating less volume expansion with artificial colloid during the first 24 postoperative hours. Albumin supplements occurred more frequently in the HES group between 2 and 3 hours postoperatively but total artificial colloid supplement was significantly higher in the gelatin group (13.36 versus 8.96 mL/kg, P < 0.001). There were no differences in the number of packed red cells, fresh frozen plasma, or platelets transfused between the two groups.
Hanart et alCitation13 compared 4% albumin with 6% HES 130/0.4 in 190 children undergoing cardiac surgery, randomized to receive either 4% albumin (n = 59) or 6% HES 130/0.4 (n = 60) for intraoperative fluid volume replacement including the cardiopulmonary bypass priming fluid. Volume of colloid used intraoperatively was similar in both groups.
They concluded that in children undergoing cardiac surgery, 6% HES 130/0.4 may represent an alternative to 4% albumin for intraoperative fluid volume replacement because of its lower cost.
Is blood loss and risk of bleeding increased with HES 130/0.4 during surgery?
The in vitro and in vivo effects of various HES products on coagulation and platelet function have been investigated in a number of studies. Overall, the more rapidly degradable HES products have been found to have a greatly reduced effect on the coagulation process compared to older products.Citation14,Citation15
HES macromolecules interact with platelets and the coagulation cascade, causing a decrease in factors such as Factor VIII and von Willebrand factor but the exact mechanisms have still not been fully elucidated.Citation16 There have been consistent reports of coagulation impairment since slowly degradable HES preparations were introduced into clinical practice. These HES preparations decreased circulating plasma concentrations of coagulation factors in volunteers and patients, even when used below the recommended maximum doses.Citation15,Citation17–Citation22
It is recommended that the maximum doses of HES not exceed 20 and 33 mL/kg per day for high- and medium-molecular- weight HES solutions, respectively.
Treib et al carried out systematic studies of the effects of a range of HES preparations and found that the products with higher MS had a profound effect on coagulation and platelet function but suggested that newer HES preparations should only have minimal effects.Citation23,Citation24 Results of in vitro studies of the coagulation process indicate that the altered pharmacokinetics of the newer generation of HES preparations have led to products with moderate effects on coagulation and platelet function.Citation18,Citation25–Citation27 However, in vitro studies have limitations and may be misleading since, in the absence of the normal compensatory mechanisms, at least part of the observed effects may be attributable to simple hemodilution or to the presence of calcium in the solvents.Citation28,Citation29 The biochemical mechanisms causing dilutional coagulopathy following infusion of hydroxyethyl starch 130/0.4 have been recently studied by Fenger-Eriksen et alCitation30 acquired fibrinogen deficiency constitutes the most important determinant of the coagulopathy.
A total of 20 bleeding patients were examined;Citation30 blood loss was substituted with HES up to a target level of 30% and thromboelastometry, platelet count, thrombin generation, and the activities of von Willebrand factor, coagulation factor II, FVII, FVIII, FIX, FX, and FXIII were measured. All coagulation factor activities were reduced. Ex vivo addition of fibrinogen corrected the coagulopathy completely.
The most useful evidence concerning the safety of waxy maize-derived 6% HES 130/0.4 is derived from extensive clinical studies in many types of major surgery. Although very high doses have been used,Citation31 no adverse effects on coagulation have been reported compared to controls using lower doses.
In one high-dose study, Ellger et alCitation32 found that 6% HES 130/0.4, when given in doses up to 50 mL/kg, had similar effects on coagulation as 30 mL/kg HES 200/0.5 plus gelatin. In this study, 40 patients undergoing elective surgery for urology-related cancer were randomized to receive one of the HES preparations. Coagulation parameters were measured at five time points during and after surgery. The authors noted that there was some deterioration of coagulation during surgery but that this was most likely the result of blood loss and hemodilution. No significant differences were found between groups in terms of hemoglobin, hematocrit, platelet count, coagulation factors (prothrombin time, partial thromboplastin time, von Willebrand factor, Factor VIIIc), or blood loss. Similar results were obtained in a study of 120 patients undergoing elective coronary artery bypass surgery.Citation33 Patients were randomized to volume replacement either with 6% HES 130/0.4 (up to 50 mL/kg) or 6% HES 200/0.5 (up to 33 mL/kg) with volume requirements in excess of these doses being met with gelatin. Despite being used at a median dose of 49 mL/kg, HES 130/0.4 did not increase blood loss and transfusion requirements compared to the lower dose of HES 200/0.5. The authors also noted that patients randomized to be treated with pentastarch received three times as much gelatin as those in the tetrastarch group and speculated that this should, if anything, have biased this group towards reduced blood loss.
Safety of HES 130/0.4 in patients with renal dysfunction: comparison with other colloids
Concerns about the possible deleterious effects of HES on renal function were first raised by Legendre et al in a retrospective study investigating the association between HES exposure of organ donors and the subsequent tissue storage in the recipients.Citation34 Cittanova et alCitation35 later found a link between the use of HES 200/0.62 in kidney donors and the subsequent need for hemodialysis in the recipients, but Deman et al could not confirm these results in their retrospective analysis.Citation36 The authors suggested that the nephrotoxicity noted by Legendre et alCitation34 might have resulted from the use of a particular preservation agent. Other researchers also failed to find any deterioration in renal function associated with the use of various HES preparations: 6% HES 200/0.5 and HES 70/0.5,Citation37 6% HES 200/0.5, 6% HES 200/0.62, and 6% HES 450/0.7,Citation38 even when high doses were used.Citation31 In a randomized study of elderly patients undergoing cardiopulmonary bypass surgery, Boldt et al found no difference in the levels of kidney-specific proteins between patients who received 6% HES 130/0.4 and those who received gelatin.Citation39 In another randomized study with similar patients, comparing the same HES agent with 5% albumin, Boldt et al again found no difference in renal function between the two groups.Citation40 In the considerable body of clinical data on the third-generation HES 130/0.4, there have been no reports of adverse effects on renal function over and above those seen in control groups, in patients who are considered to be at particular risk, such as those with previous mild to severe renal dysfunction,Citation41–Citation43 the elderly,Citation44 and those receiving high- dose therapy.Citation31 Fenger- Eriksen et alCitation44 performed studies in the area and found that a colloid-based fluid regime (6% HES 130/0.4) may preserve renal function to a greater extent than crystalloids in patients undergoing spinal surgery. Similarly, Godet et alCitation45 suggested that 6% HES 130/0.4 was as safe as gelatin (Plasmion®; Fresenius France Pharma, Sevres, France) in patients with prior renal dysfunction undergoing abdominal aortic surgery. Although baseline renal function was impaired in all patients (creatinine clearance [CrCl] less than 80 mL/min), no drug-related unfavorable effects on renal function were found using HES 130/0.4 compared to gelatin.
One of the criticisms directed against many earlier studies, is that the follow-up periods have been relatively short.Citation43 Fifty patients undergoing cardiac surgery were randomized to either 6% HES 130/0.4 or 5% human albumin given perioperatively until the second postoperative day. At a 60-day follow up, it was found that kidney function in patients receiving tetrastarch was as preserved as with albumin. Although concentrations of kidney-specific proteins increased after surgery in both groups, there was no difference between groups. None of the patients developed acute renal failure leading to renal replacement therapy, either during hospital stay or in the follow-up period.
Three recently published studies confirm these findings. In a randomized study of 50 patients assigned to either a balanced regimen (6% HES 130/0.42 plus crystalloid solution) or a saline-based regimen (saline plus MS of the HES) kidney integrity was less altered with the HES 130/0.42. Levels of glutathione transferase alpha and neutrophil gelatinase- associated lipocalin were raised in both groups, but less so in the group with the plasma-adapted solutions.Citation46
Another recent publication contains preliminary results of an observational study of pediatric patients aged up to 12 years undergoing various types of surgery while receiving 6% HES 130/0.42. This noncomparative study evaluated the perioperative use of HES 130/0.42 in 1,000 children, with a particular focus on cardiovascular stability, hemodilution, acid-base balance, renal function, blood coagulation, and hypersensitivity. Reports on the first 300 children have shown no serious effects on renal function.Citation47
It has been suggested from perioperative studies in low- risk patients who received cumulative doses in the range of only 50 mL/kg body weight, that HES 130/0.4 may be less likely to induce nephrotoxicity than HES 10%.
In surgical ICU patients, the incidence of ARF was similar in patients who received predominantly HES 130/0.4 fluid therapy and in those who received predominantly gelatin 4%.Citation48,Citation49 In summary, the published data on this topic suggest that there are differences between the older and newer generations of HES and that the reports of adverse effects on renal function should not be extrapolated to newer HES products. Moreover the Cochrane Collaboration Review [Dart AB, Mutter TC, Ruth CA, Taback SP, Hydroxyethyl Starch (HES) versus other fluid therapies: effects on kidney function. Database of Systematic Reviews 2010, Issue 1] concluded that “there is inadequate clinical data to address the claim that safety differences exist between different HES products”.
Pulmonary mechanics: comparison of HES 130/0.4 and other fluids
Crystalloids may promote fluid extravasation in the lungs and formation of pulmonary edema since they tend to lower colloid osmotic pressure (COP). In contrast, colloids may decrease pulmonary fluid extravasation and the formation of pulmonary edema because of their capacity to increase COP. The so-called colloid-crystalloid controversy includes the relative propensity of fluid types to evoke pulmonary edema, which is not yet settled in the absence of direct permeability and edema measurements in most studies.Citation50 Indeed, the controversy is complicated by the fact that the potentially protective role of COP may diminish when permeability is increased, while the propensity for edema formation may increase, unless hydrostatic pressure is kept low, as demonstrated in experimental and human studies.Citation51–Citation53
Cardiac and major vascular surgery are often complicated by hypovolemic hypotension, necessitating fluid therapy, but the optimal type of fluid for this purpose is hotly debated.Citation50,Citation54–Citation61 Cardiac and major vascular surgery, involving ischemia and reperfusion, are well known risk factors for a systemic inflammatory response and for acute lung injury/acute respiratory distress syndrome (ALI/ARDS), associated with increased capillary permeability in the lungs in some patients, as measured by a noninvasive double radionuclide technique to detect pulmonary Ga-transferrin extravasation.Citation62–Citation66 This could thus affect the contribution of infusion fluids to pulmonary edema formation. Indeed, researchers have documented an increase in extravascular lung water (EVLW) after cardiac or major vascular surgery and fluid loading, at least transiently in some patients.Citation57–Citation59,Citation67–Citation70 Verheij et alCitation71 hypothesized that colloid fluid loading would aggravate less edema formation in the lungs than saline loading in the treatment of presumed hypovolemia after major surgery, even if complicated by increased pulmonary permeability. They also hypothesized that hydroxyethyl starch (HES) or albumin loading would attenuate pulmonary edema attributable to increased permeability as compared with gelatin loading. They therefore compared filling pressure-guided fluid challengesCitation72 with saline and with the colloids gelatin, HES, and albumin on their effects on pulmonary capillary permeability, EVLW, COP, and the lung injury score (LIS) in 67 presumably hypovolemic patients after cardiac or major vascular surgery. In this study more saline was infused than colloid solutions (P < 0.005). The COP increased in the colloid groups and decreased in patients receiving saline. Cardiac output increased more in the colloid groups. At baseline, pulmonary leak index (PLI) and EVLW were above normal in 60% and 30% of the patients, with no changes after fluid loading, except for a greater PLI decrease in HES than in gelatin-loaded patients. The oxygenation ratio was improved in all groups. In the colloid groups, the LIS was increased because of a decrease in total respiratory compliance, probably associated with an increase in intrathoracic plasma volume. It was concluded that saline or colloids do not affect permeability edema in ALI after cardiac or major vascular surgery, provided that fluid overloading is avoided, and except for HES which may ameliorate increased permeability. The LIS, however, may slightly increase after colloid versus saline loading, because of greater intrathoracic plasma volume expansion decreasing total respiratory compliance, thus indicating that changes in LIS (and respiratory compliance) during fluid loading do not represent only changes in permeability edema.
Does HES 130/0.4 reduce inflammatory response to surgery?
As with all forms of trauma, surgery triggers a systemic inflammatory response with the release of inflammatory mediators into the systemic circulation. Proinflammatory cytokines, such as interleukin-6 (IL-6) and IL-8, play an important role in regulating the acute inflammatory phase. Cell adhesion molecules, such as E-selectin, endothelial leukocyte adhesion molecule-1 (ELAM-1), and intercellular adhesion molecule-1 (ICAM-1) regulate the interaction away immune cells with the endothelium and the extracellular matrix. It has been demonstrated that release of IL-6 correlates with the severity of surgery.Citation72 In particular, surgery of the intestine is associated with a greater inflammatory response than other types of surgery,Citation73 and the elderly population may also show an enhanced inflammatory response.Citation74,Citation75 It is, therefore, of interest to assess the effects of volume replacement solutions on the mediators of inflammation.
In a study of patients undergoing abdominal surgery, Lang et alCitation76 found a significantly lower increase of the proinflammatory cytokines IL-6 and IL-8 in patients receiving 6% HES 130/0.4 compared to those receiving lactated Ringer’s solution. There were also significantly lower serum concentrations of soluble ICAM-1 (sICAM-1) in the HES group.
Likewise, in patients undergoing major abdominal surgery, Boldt et alCitation77 reported a similar attenuation of plasma levels of IL-6 in patients receiving 6% HES 130/0.4 compared to those receiving 5% albumin. Plasma levels of endothelial adhesion molecules (sELAM-1, sICAM-1) were also significantly lower in the HES group, returning to normal on the day after surgery and remaining elevated in patients receiving albumin. In a study of elderly patients undergoing cardiac surgery, inflammatory response was similar in groups receiving 5% albumin and those receiving 6% HES 130/0.4, whereas endothelial activation was lower in the HES group.Citation40 Boldt speculates that the beneficial effect of HES 130/0.4 on inflammation and endothelial activation may be the result of some direct, substance-specific effects on endothelial cells resulting in reduced release of adhesion molecules.Citation77 Using endothelial cell cultures, Collis et alCitation78 found that lipopolysaccharide-stimulated expression of adhesion ligand P-selectin was inhibited by HES.
Volta et alCitation79 reported that HES 130/0.4 was able to selectively inhibit the activity of matrix metalloproteinase-9 (MMP-9) in vitro compared to lactated Ringer’s solution. This was confirmed in 36 patients scheduled for colon cancer surgery who were randomized to 6% HES 130/0.4, 3.4% polygeline or lactated Ringer’s solution. After surgery, plasma levels of MMP-9 and tissue inhibitor of MMP-9 (TIMP-9) were higher in all three groups, but they were significantly lower in the tetrastarch group than in the other two groups.
In a number of in vitro and animal studies light has been shed on the possible mechanisms by which HES might affect the inflammatory process. Using cultured human microvascular endothelial cells and mice, Dieterich et alCitation80 found that physiologically relevant concentrations of tetrastarch were able to reduce neutrophil adhesion in vitro, while vascular leakage and pulmonary edema induced by hypoxia exposure were reduced in animals treated with HES. Nohé et alCitation81 studied the expression of adhesion molecules on native and cytokine-activated endothelium from umbilical veins after pretreatment with gelatin and various preparations of dextran and HES. The authors concluded that synthetic colloids inhibit neutrophil adhesion by a neutrophil-dependent mechanism rather than interfering with endothelial cell activation.
Conclusion
The evidence base for HES 130/0.4 is strong; overall, there are more than 50 published studies reporting on the coagulation effects of waxy maize-derived HES 130/0.4, including more than 20 Phase II to IV studies. These studies confirm that, unlike earlier generation HES preparations, the tetrastarches have minimal effects on coagulation.
Results of nine clinical trials on renal function support the safety of HES 130/0.4, and two recently published trials confirm that potato-derived HES 130/0.42 has no adverse effects on renal function, but there are inadequate clinical data to address the claim that safety differences exist between different HES products. Intravascular volume replacement with HES 130/0.4 may reduce the inflammatory response in patients undergoing major surgery compared to a crystalloid-based volume therapy. Finally, the type of fluid used for volume loading does not affect pulmonary permeability and edema, and HES may ameliorate increased permeability ().
Disclosure
The authors report no conflicts of interest.
References
- TreibJBaronJFGrauerMTStraussRGAn international view of hydroxyethyl starchesIntensive Care Med19992525826810229159
- BrunkharstFMEngelCBlossFMeier-HellmannARagallerMWeilerNIntensive Insuline therapy and pentasterch resuscitation in severe sepsisN Engl J Med200835812513918184958
- SommermeyerKCechFSchossowRDifferences in chemical structures between waxy maize- and potato-starch-based hydroxyethyl starch volume therapeuticsTransfus Altern Transfus Med20079127133
- LehmannGMarxGFörsterHBioequivalence comparison between hydroxyethyl starch 130/0.42/6:1 and hydroxyethyl starch 130/0.4/9:1Drugs RD20078229240
- WalleyKRMcDonaldTEWangYDaiSRussellJAAlbumin resuscitation increases cardiomyocyte contractility and decreases nitric oxide synthase II expression in rat endotoxemiaCrit Care Med20033118719412545014
- HolteKKehletHFluid therapy and surgical outcomes in elective surgery: A need for reassessment in fast-track surgeryJ Am Coll Surg200620297198916735213
- RiversENguyenBHavstadSEarly goal-directed therapy in the treatment of severe sepsis and septic shockN Engl J Med20013451368137711794169
- BrandstrupBFluid therapy for the surgical patientBest Pract Res Clin Anaesthesiol20062026528316850777
- GanTJSoppittAMaroofMGoal-directed intraoperative fluid administration reduces length of hospital stay after major surgeryAnesthesiology20029782082612357146
- BoldtJPro use of colloids in cardiac surgeryJ Cardiothorac Vasc Anesth20072145345617544907
- FinferSBellomoRBoyceNFrenchJMyburghJNortonRA comparison of albumin and saline for fluid resuscitation in the intensive care unitN Engl J Med20043502247225615163774
- VanhoonackerJOngenaeMVanoverscheldeHDonadoniRHydroxyethyl starch 130/0.4 versus modified fluid gelatin for cardiopulmonary bypass priming: the effects on postoperative bleeding and volume expansion needs after elective CABGActa Anaesthesiol Belg2009602919719594090
- HanartCKhalifeMDe VilléAOtteFDe HertSVan der LindenPPerioperative volume replacement in children undergoing cardiac surgery: albumin versus hydroxyethyl starch 130/0.4Crit Care Med200937269670119114887
- MacIntyreEMackieIJHoDTinkerJBullenCMachinSJThe haemostatic effects of hydroxyethyl starch (HES) used as a volume expanderIntensive Care Med1985113003032418087
- ClaesYvan HemelrijckJvan GervenMInfluence of hydroxyethyl starch on coagulation in patients during the perioperative periodAnesth Analg19927524301377457
- Kozek-LangeneckerSEffects of hydroxyethyl starch solutions on hemostasisAnesthesiology200510365466016129993
- GandhiSDWeiskopfRBJungheinrichCVolume replacement therapy during major orthopaedic surgery using Voluven (hydroxyethyl starch 130/0.4) or hetastarchAnesthesiology20071061120112717525586
- De JongeELeviMBüllerHRBerendsFKaseciogluJDecreased circulating levels of von Willebrand factor after intravenous administration of a rapidly degradable hydroxyethyl starch (HES 200/0.5/6) in healthy human subjectsIntensive Care Med2001271825182911810130
- JamnickiMBombeliTSeifertBLow- and medium-molecular- weight hydroxyethyl starches: Comparison of their effect on blood coagulationAnesthesiology2000921231123711046211
- KapiotisSQuehenbergerPEichlerHEffect of hydroxyethyl starch on the activity of blood coagulation and fibrinolysis in healthy volunteers: comparison with albuminCrit Care Med1994226066127511495
- JonesSBWhittenCWDespotisGJMonkTGThe influence of crystalloid and colloid replacement solutions in acute normovolemic hemodilution: a preliminary survey of hemostatic markersAnesth Analg20039636336812538178
- ConroyJMFishmanRLReevesSTPinsokyMLLazarchickJThe effects of desmopressin and 6% hydroxyethyl starch on factor VIIICAnesth Analg1996838048078831325
- TreibJHaassAPindurGHES 200/0.5 is not HES 200/0.5. Influence of the C2/C6 hydroxyethylation ratio of hydroxyethyl starch (HES) on hemorheology, coagulation and elimination kineticsThromb Haemost199574145214568772219
- TreibJHaassAPindurGTreibWWenzelESchimrigkKInfluence of intravascular molecular weight of hydroxyethyl starch on plateletsEur J Haematol1996561681728598237
- FranzABräunlichPGamsjägerTThe effects of hydroxyethyl starches of varying molecular weights on platelet functionAnesth Analg2001921402140711375812
- EntholznerEKMielkeLLCalatzisANFeyhJHippRHargasserSRCoagulation effects of a recently developed hydroxyethyl starch (HES 130/0.4) compared to hydroxyethyl starches with higher molecular weightActa Anaesthesiol Scand2000441116112111028733
- KonradCJMarklTJSchuepferGKSchmeckJGerberHRIn vitro effects of different medium molecular hydroxyethyl starch solutions and lactated Ringer’s solution on coagulation using SONOCLOTAnesth Analg20009027427910648306
- JamnickiMZollingerASeifertBPopovicDPaschTSpahnDRCompromised blood coagulation: an in vitro comparison of hydroxyethyl starch 130/0.4 and hydroxyethyl starch 200/0.5 using thromboelastographyAnesth Analg1998879899939806670
- DeuschEThalerUKozek-LangeneckerSAThe effects of high molecular weight hydroxyethyl starch solutions on plateletsAnesth Analg20049966566815333389
- Fenger-EriksenCTønnesenEIngerslevJSørensenBMechanisms of hydroxyethyl starch-induced dilutional coagulopathyJ Thromb Haemost2009771099110519422451
- NeffTADoelbergMJungheinrichCSauerlandASpahnDRStockerRRepetitive large-dose infusion of the novel hydroxyethyl starch 130/0.4 in patients with severe head injuryAnesth Analg2003961453145912707149
- EllgerBFreyhoffJVan AkenHBookeMMarkusMAHigh dose volume replacement using HES 130/0.4 during major surgery. Impact on coagulation and incidence of postoperative itchingNeth Tijdschr Anesth2006196368
- KasperSMMeinertPKampeSLarge-dose hydroxyethyl starch 130/0.4 does not increase blood loss and transfusion requirements in coronary artery bypass surgery compared with hydroxyethyl starch 200/0.5 at recommended dosesAnesthesiology200399424712826840
- LegendreCThervetEPageBPercheronANoelLKreisHHydroxyethylstarch and osmotic-nephrosis-like lesions in kidney transplantationLancet1993342238239
- CittanovaMLLeblancILegendreCMouquetCRiouBCoriatPEffect of hydroxyethyl starch in brain-dead kidney donors on renal function in kidney-transplant recipientsLancet1996348162016228961992
- DemanAPeetersPSennesaelJHydroxyethyl starch does not impair immediate renal function in kidney transplant recipients: a retrospective, multicentre analysisNephrol Dial Transplant1999141517152010383017
- KumleBBoldtJPiperSSchmidtCSuttnerSSalopekSThe influence of different intravascular volume replacement regimens on renal function in the elderlyAnesth Analg1999891124113010553822
- DehneMMuhlingJSablotzkiADehneKSuckeNHempelmannGHydroxyethyl starch (HES) does not directly affect renal function in patients with no prior renal impairmentJ Clin Anesth20011310311111331169
- BoldtJBroschCRöhmKPapsdorfMMengistuAComparison of the effects of gelatin and a modern hydroxyethyl starch solution on renal function and inflammatory response in elderly cardiac surgery patientsBr J Anaesth200810045746418305082
- BoldtJBroschCRöhmKLehmannAMengistuASuttnerSIs albumin administration in hypoalbuminemic elderly cardiac surgery patients of benefit with regard to inflammation, endothelial activation, and long-term kidney function?Anesth Analg20081071496150318931204
- JungheinrichCScharpfRWargenauMBepperlingFBaronJFThe pharmacokinetics and tolerability of an intravenous infusion of the new hydroxyethyl starch 130/0.4 (6%, 500 ml) in mild-to-severe renal impairmentAnesth Analg20029554455112198032
- SakrYPayenDReinhartKEffects of hydroxyethyl starch administration on renal function in critically ill patientsBr J Anaesth20079821622417251213
- BoldtJBroschCDuckeMPapsdorfMLehmannAInfluence of volume therapy with a modern hydroxyethylstarch preparation on kidney function in cardiac surgery patients with compromised renal function: a comparison with human albuminCrit Care Med2007352740274617893629
- Fenger-EriksenCRasmussenCHJensenTKRenal effects of hypotensive anaesthesia in combination with acute normovolaemic haemodilution with hydroxyethyl starch 130/0.4 or isotonic salineActa Anaesthesiol Scand20054996997416045658
- GodetGLehatJJJanvierGSteibAde CastroVCoriatPSafety of HES 130/0.4 (Voluven®) in patients with preoperative renal dysfunction undergong abdominal aortic surgery: A prospective, randomized, controlled, parallel-group multicentre trialEur J Anaesthesiol20082598699418492315
- BoldtJSuttnerSBroschCLehmannARöhmKMengistuAThe influence of a balanced volume replacement concept on inflammation, endothelial activation, and kidney integrity in elderly cardiac surgery patientsIntensive Care Med20093546247018807007
- SümpelmannRKretzFJGäblerRHydroxyethyl starch 130/0.42/6:1 for perioperative plasma volume replacement in children: preliminary results of a European Prospective Multicenter Observational Postauthorization Safety Study (PASS)Paediatr Anaesth20081892993318647272
- SchabinskiFOishiJTucheFEffects of a predominantly hydroxyethyl starch (HES)-based and a predominantly non HES-based fluid therapy on renal function in surgical ICU patientsIntensive Care Med2009351539154719533095
- RobertsIAldersonPBunnFChinnockPKerKSchierhoutGColloid versus crystalloids for fluid resuscitation in critically ill patientsCochrane Database Syst Rev20074CD00056717943746
- SibbaldWJDriedgerAAWellsGAMyersMLLefcoeMThe short-term effects of increasing plasma colloid osmotic pressure in patients with non-cardiac pulmonary edemaSurgery1983936206366845168
- FinchJSReidCBandyKFickleDCompared effects of selected colloids on extravascular lung water in dogs after oleic acid-induced lung injury and severe hemorrhageCrit Care Med1983112672706831896
- PearlRGHalperinBDMihmFGRosenthalMHPulmonary effects of crystalloid and colloid resuscitation from hemorrhagic shock in the presence of oleic-induced pulmonary capillary injury in the dogAnesthesiology19886812203337363
- SkillmanJJRestallSSalzmanEWRandomized trial of albumin vs electrolyte solutions during abdominal aortic operationsSurgery1975782913031154272
- BoutrosARRuessROlsonLHoytJLBakerWHComparison of hemodynamic, pulmonary, and renal effects of use of three types of fluid after major surgical procedures on the abdominal aortaCrit Care Med19797913367709
- VirgilioRWRiceCLSmithDECrystalloid vs colloid resuscitation: is one better?Surgery197985129139419454
- ShiresGTPeitzmanABAlbertSAResponse of extravascular lung water to intraoperative fluidsAnn Surg19831975155196847271
- GallagherJDMooreRAKernsDEffects of colloid or crystalloid administration on pulmonary extravascular lung water in the postoperative period after coronary bypass graftingAnesth Analg1985647537582409845
- KarankoMSKlossnerJALaaksonenVORestoration of volume by crystalloid versus colloid after coronary bypass: hemodynamics, lung water, oxygenation, and outcomeCrit Care Med1987155595662436856
- LondonMJHoJSTriedmanJKA randomized clinical tria of 10% pentastarch (low molecular weight hydroxyethyl starch) versus 5% albumin for plasma volume expansion after cardiac operationsJ Thorac Cardiovasc Surg1989977857972468978
- TølløfsrudSSvennevigJLBreivikHFluid balance and pulmonary functions during and after coronary artery bypass surgery: Ringer’s acetate compared with dextran, polygeline, or albuminActa Anaesthesiol Scand1995396716777572019
- RaijmakersPGHMGroeneveldABJSchneiderAJTransvascular transport of 67Ga in the lungs after cardiopulmonary bypass surgeryChest1993104182518328252972
- RaijmakersPGHMGroeneveldABJRauwerdaJATransient increase in interleukin-8 and pulmonary microvascular permeability following aortic surgeryAm J Respir Crit Care Med19951516987057881659
- GroeneveldABJRaijmakersPGHMThe 67Gallium-transferrin pulmonary leak index in patients at risk for the acute respiratory distress syndromeCrit Care Med1998266856919559605
- PararajasingamRNicholsonMLBellPRFSayersRDNon- cardiogenic pulmonary oedema in vascular surgeryEur J Vasc Endovasc Surg1999179310510063402
- NgCSHWanSYimAPCArifiAAPulmonary dysfunction after cardiac surgeryChest20021211269127711948063
- ByrickRJKayJCNobleWHExtravascular lung water accumulation in patients following coronary artery surgeryCan Anaesth Soc J197724332345301424
- SivakEDStarrNJGravesJWCosgroveDMBorshJEstafanousGEExtravascular lung water values in patients undergoing coronary artery bypass surgeryCrit Care Med1982105935966980772
- LumbPDA comparison between 25% albumin and 6% hydroxyethyl starch solutions on lung water accumulation during and immediately after cardiopulmonary bypassAnn Surg1987262102132440391
- WahbaASendtnerEStrotzerMWildKBirnbaumDEFluid therapy with Ringer‘s solution versus Haemacel following coronary artery bypass surgeryActa Anaesthesiol Scand199640122712338986187
- VerheijJvan LingenARaijmakersPGEffect of fluid loading with saline or colloids on pulmonary permeability, oedema and lung injury score after cardiac and major vascular surgeryBr J Anaesth200696213016311279
- WeilMHHenningRJNew concepts in the diagnosis and fluid treatment of circulatory shock. Thirteenth Annual Becton, Dickinson and Company Oscar Schwidetsky Memorial LectureAnesth Analg197958124132571235
- KuntzCKienlePSchmedingMBennerAAutschbachFSchwalbachPComparison of laparoscopic versus conventional technique in colonic and liver resection in a tumor-bearing small animal modelSurg Endosc2002161175118112189479
- LevyMMDellingerRPTownsendSR(on behalf of the Surviving Sepsis Campaign)The Surviving Sepsis Campaign: Results of an international guideline based performance improvement program targeting severe sepsisCritical Care Medicine20103836737420035219
- MeissnerMTschaikowskyKHutzlerASchlickCSchüttlerJPost- operative plasma concentrations of prop-calcitonin after different types of surgeryIntensive Care Med1998246806849722037
- RinkLCakmanIKirchnerHAltered cytokine production in the elderlyMech Ageing Dev19981021992099720652
- LangKSuttnerSBoldtJKumleBNagelDVolume replacement with HES 130/0.4 may reduce the inflammatory response in patients undergoing major abdominal surgeryCan J Anaesth2003501009101614656778
- BoldtJSchölhornTMayerJPiperSSuttnerSThe value of an albumin-based intravascular volume replacement strategy in elderly patients undergoing major abdominal surgeryAnesth Analg200610319119916790652
- CollisRECollinsPWGutteridgeCNThe effect of hydroxyethyl starch and other plasma volume substitutes on endothelial cell activation: an in vitro studyIntensive Care Med19942037417513003
- VoltaCAAlvisVCampiMInfluence of different strategies of volume replacement on the activity of matrix metalloproteinases: an in vitro and in vivo studyAnesthesiology2007106859117197849
- DieterichH-JWeissmüllerTRosenbergerPEltzschigHKEffect of hydroxyethyl starch on vascular leak syndrome and neutrophil accumulation during hypoxiaCrit Care Med2006341775178216625120
- NohéBJohannesTReutershanJSynthetic colloids attenuate leukocyte-endothelial interactions by inhibition of integrin functionAnesthesiology200510375976716192768