Abstract
Purpose
This study aimed to investigate the predictive value of red cell distribution width (RDW) in patients with peripherally inserted central catheter (PICC)-related thrombosis.
Patients and methods
This was a case‒control study. A total of 98 cancer patients undergoing PICC placement from January 2017 to December 2019 at the ICU Venous Access Center of Peking University Cancer Hospital were retrospectively analyzed. These included 47 cases in the thrombosis group and 51 cases in the nonthrombosis group according to the occurrence of PICC-related thrombosis within 90 days after the PICC procedure.
Results
a) RDW was significantly higher in the thrombosis group (15.98±1.93) than in the nonthrombosis group (13.98±1.09). Additionally, the number of smoking histories in the thrombosis group (18, 38.30%) was significantly higher than that in the nonthrombosis group (5, 9.80%). b) Logistic regression analysis indicated that RDW and smoking history were independent risk factors for PICC-related thrombosis (OR: 3.028, P<0.001; OR: 5.640, P=0.023). c) The area under the receiver operating characteristic (ROC) curve of the combination of RDW and smoking history was 86.8%, and the sensitivity and specificity for predicting thrombosis after PICC were 85.1% and 80%, respectively. d) Cox regression analysis revealed that RDW and smoking history were independent risk factors for PICC-related thrombosis (p<0.001). e) Results from Kaplan‒Meier analysis showed that incidence of PICC-related thrombosis in patients with RDW less than 14.75% is significantly lower than those with RDW 14.75% and above (p<0.001). e) Baseline RDW was not different between the two groups (P>0.05), ΔRDW was significantly different between the two groups (p<0.001).
Conclusion
The combined use of RDW and smoking history has early evaluation and predictive value in the diagnosis of PICC-related thrombosis.
Introduction
The application rate of peripherally inserted central catheters (PICCs) in cancer patients is gradually growing during chemotherapy, which can relieve the pain of repeated puncture and reduce the occurrence of drug extravasation. However, as a main complication, PICC-related thrombosis always worries clinical workers, with an incidence rate of 14% to 23%.Citation1 Considering its possible serious consequences, such as patient discomfort, increased economic burden and pulmonary embolism, early identification of PICC-related thrombosis remains an urgent problem in clinical settings. Whole blood cell analysis is a test with accessibility and low cost, among which red cell distribution width (RDW) reflects red blood cell volume heterogeneity and is traditionally used in the diagnosis and classification of anemia.Citation2 In recent studies, RDW has been gradually applied to assess the severity and prognosis of cardiovascular disease,Citation3,Citation4 sepsis,Citation5 cancer,Citation6 pulmonary embolism,Citation7 and other diseases. Although there have been several studies on the correlation between RDW and venous thromboembolism (VTE), its association with PICC-related thrombosis is still poorly understood. This study aimed to discuss the predictive value of RDW for PICC-related thrombosis.
Methods
Study Population
The institutional review board of Peking University Cancer Hospital approved this retrospective study (No. 2017KT56), and all participants or their first-degree relative signed informed consent. A total of 98 cancer patients undergoing PICC placement from January 2017 to December 2019 at the ICU Venous Access Center of Peking University Cancer Hospital were retrospectively analyzed. These included 47 PICC-related thrombosis cases (25 males and 22 females) with a mean age of 55.36±11.91 years and 51 without PICC-related thrombosis cases (26 males and 25 females) with a mean age of 50.52±12.35 years, according to the occurrence of PICC-related thrombosis within 90 days after the PICC procedure. The inclusion criteria were as follows: (1) cancer patients who underwent upper limb PICC; (2) normal coagulation function before the PICC procedure; and (3) signed informed consent. Patients were excluded if (1) they had venous thrombosis before the PICC procedure; (2) they had hematologic disease; or (3) they had long-term use of anticoagulant or antiplatelet aggregation.
Study methods
Data Collection
All patient data were collected from electronic medical records (EMRs), including age, sex, BMI, smoking and drinking history, hypertension and diabetes history.
Observation Indicators
Color Doppler ultrasound on the catheterization side was used for thrombosis diagnosis after the PICC procedure once thrombus-related symptoms occurred, including pain, swelling, increased skin temperature, and paraesthesia at the site of the PICC.Citation8 Venous blood was drawn on the day of definite diagnosis of PICC-related thrombosis, while red blood cell and platelet-related indicators were measured by an automatic hematology analyzer. For patients without PICC-related thrombosis, color Doppler ultrasound on the catheterization side was performed on the 90th day after the PICC procedure, along with complete blood cell analysis.
Statistical Analysis
Variables were expressed as the mean±standard deviation and counts (proportion) for continuous and categorical variables, separately. Numerical differences between two groups were assessed by the chi-square test for categorical variables and the t-test or Mann‒Whitney U-test for continuous variables. Significant variables in univariate analysis were further included in the Cox proportional hazards model to analyze the influence of PICC on thrombosis at day 90 after its placement. Kaplan‒Meier curves were plotted for differences in the time of thrombus formation. The threshold for significance was P=0.05. All statistical analyses were conducted using SPSS version 26.0 (SPSS Inc., Chicago, IL, USA).
Results
Univariate Analysis
Univariate analysis was performed on the general condition of the thrombus group and the non-thrombus group, and it was found that there were significant differences in smoking history, HGB, MCV, and RDW ().
Table 1 The General Condition of the Thrombosis Group and the Nonthrombotic Group and the Results of Red Blood Cells and Platelet-Related Indicators ()
Multivariate Logistic Regression Analysis
Significant variables in univariate analysis were included in the logistic regression model. Smoking history and RDW were independent risk factors for PICC-related thrombosis ().
Table 2 Logistic Regression Between the Thrombosis and Nonthrombosis Groups
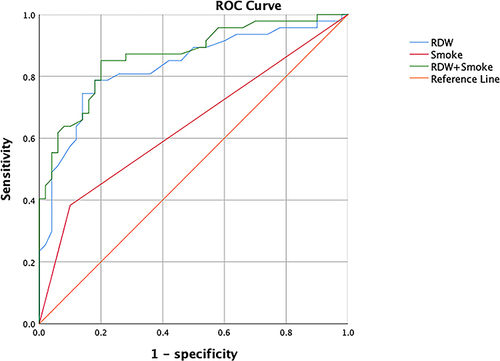
ROC Analysis
ROC analysis was conducted to evaluate the predictive value of smoking history, RDW, and combination of the two on PICC-related thrombosis. The areas under the curve (AUCs) of smoking history and RDW were 0.64±0.06 (p<0.05) and 0.83±0.04 (p<0.05), respectively. The cutoff value was 14.75%, with a sensitivity of 78.7% and a specificity of 82.0% for predicting PICC-related thrombosis. The AUC of the combination of the two was 86.8%, with a sensitivity of 85.1% and a specificity of 80%, as shown in . Compared with their respective prediction performance alone, there was a significant improvement when they were combined (p<0.05).
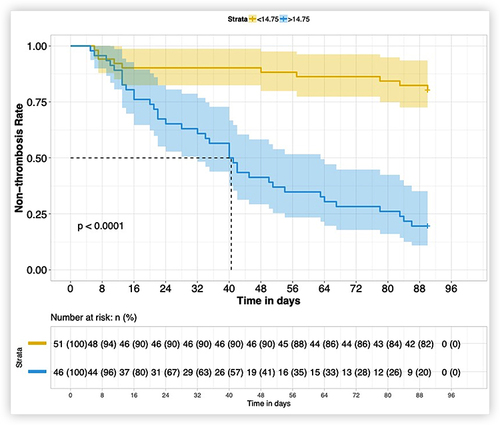
Cox Regression Analysis
All patients were redivided into two groups (RDW< 14.75% and RDW≥14.75%) based on the RDW cutoff value of 14.75%. RDW, smoking history and other significant variables were included in the Cox regression model, showing that RDW and smoking history were independent risk factors for PICC-related thrombosis ().
Table 3 Cox Proportional Hazards Model of PICC-Related Thrombosis in 98 Patients
Kaplan‒Meier Survival Curve
The Kaplan‒Meier curve indicated a significant difference in the time of PICC-related thrombosis between the two RDW groups (p<0.001), suggesting a higher possibility of PICC-related thrombosis in patients with RDW 14.75% and above ().
Data for Baseline RDW Values and ΔRDW
The RDW value before PICC catheterization was used as the baseline RDW for comparison between the two groups, and no significant difference was found between the two groups. The difference between the RDW measured at the outcome and the baseline RDW was defined as ΔRDW, and compared between the two groups, there was a statistical difference ().
Table 4 Comparison of Baseline RDW and ΔRDW Between the Thrombosis Group and the Nonthrombotic Group ()
Discussion
Venous injury, slow blood flow and a hypercoagulable state are the three main factors of VTE formation. A previous study on hemorheology and VTE indicated the role of red blood cells in venous thrombosis. Fibrinogen promotes cell bridges and forms a netlike structure, while red bold cells attach to it after accumulating into 2D structures or 3D clumps, which are difficult to disperse or decompose, thus increasing blood viscosity as well as resistance to blood flow.Citation9 There are many mechanical and physical factors that can affect the aggregation of red blood cells, and factors such as the inherent shape, deformability, and membrane surface substances of red blood cells are susceptible internal factors.Citation10 RDW is a measure of size changes (ie, anisocytosis) in circulating red blood cells, and high RDW refers to a great difference in sizes.Citation11 We detected a significant change in RDW from baseline in the thrombus group, which could be explained by the large variations in red blood cell volumes that increase blood viscosity and accelerate thrombus formation.Citation2
In addition, PICC-related thrombosis is a common complication in post-PICC care. Clinical data suggested that the size of the catheter can influence the incidence of thrombosis, especially in veins with small diameters in the upper extremities, and the placement of a PICC might reduce venous flow by 93%.Citation12 RDW increased significantly in some studies on the nonreflux of arterial thrombosis, which might explain the elevated RDW in the thrombosis group in this study since arterial thrombosis shares the same pathophysiological mechanism with venous thrombosis.Citation13,Citation14
Recently, a growing body of evidence has supported that inflammation mainly contributes to the altered pathophysiology of VTE.Citation15 Some inflammation-related cytokines and chemokines have prothrombotic activity, including IFN-γ, IL-6, IL-17 A, IL-9, IL-1β and TGF-β. Enhanced levels of such cytokines and chemokines can lead to endothelial cell activation and damage, increased platelet aggregation, increased sensitivity to thrombin, and recruitment and activation of leukocytes in the vessel wall, and ultimately, these changes promote local formation of thrombin and fibrin.Citation16 On the other hand, cytokines such as IL-10, TNF-α and IL-8 seem to contribute to thrombus resolution in an advanced stage of VTE.Citation17 Additionally, a prior study proved the correlations between RDW and systemic inflammatory responses, such as CRP, ESRCitation18 and IL-6.Citation19 For studies on the relationship between cancer or coronary artery disease and RDW, it was mentioned that the potential mechanism of its effect on prognosis may be a chronic systemic inflammatory response.Citation20,Citation21 Thus, we suspect that inflammatory cytokines and chemokines may interact with RDW; in other words, a high RDW level reflects a persistent state of chronic inflammation and promotes the generation of thrombosis.
Smoking serves as a major cause of noncommunicable diseases worldwide and a primary risk factor for cardiovascular and pulmonary diseases.Citation22 Several studies in recent years have pointed out a close relationship between smoking and VTE; for example, Osamah Al-Asadi et al proved smoking to be a risk factor for PICC-related thrombosis, which is consistent with the results from our study.Citation23,Citation24 Tobacco is able to increase the risk of VTE by elevating levels of fibrinogen, coagulation factors II, V, VIII, X and XIII, tissue factor and homocysteine while promoting VTE by stimulating activation and platelet aggregation and impairing fibrinolysis.Citation25 The combination of RDW and smoking history had good predictability for PICC-related thrombosis in this study, with an area under the ROC of 86.8%.
In conclusion, RDW level has a positive correlation with PICC-related thrombosis. In addition, the combination of smoking and RDW can improve the diagnostic efficacy of the assessment capacities of PICC-related thrombosis. This study has some limitations, including the relatively short time span and the small sample size. Therefore, a prospective, multicenter, and large-sample study is needed to further confirm the results of this study.
Conclusion
The combined use of RDW and smoking history has early evaluation and predictive value in the diagnosis of PICC-related thrombosis.
Data Sharing Statement
The data of this study can be obtained from the corresponding author upon reasonable request. Confirm that the authors are accountable for all aspects of the work (if applied, including full data access, integrity of the data and the accuracy of the data analysis) in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethical Statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Disclosure
The authors have no conflicts of interest to declare for this work.
Additional information
Funding
References
- Grigorian A, Nahmias JT. Upper extremity deep venous thrombosis. In: StatPearls. StatPearls Publishing; 2022.
- Salvagno GL, Sanchis-Gomar F, Picanza A, et al. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015;52(2):86–105. doi:10.3109/10408363.2014.992064
- Wang Z, Korantzopoulos P, Roever L, et al. Red blood cell distribution width and atrial fibrillation. Biomark Med. 2020;14(13):1289–1298. doi:10.2217/bmm-2020-0041
- Budzianowski J. The role of hematological indices in patients with acute coronary syndrome. Dis Markers. 2017;2017:10.
- Hu Z-D, Lippi G, Montagnana M. Diagnostic and prognostic value of red blood cell distribution width in sepsis: a narrative review. Clin Biochem. 2020;77:1–6.
- Hu L, Li M, Ding Y, et al. Prognostic value of RDW in cancers: a systematic review and meta-analysis. Oncotarget. 2017;8(9):16027. doi:10.18632/oncotarget.13784
- Xing X, Deng Y, Zhu Y, et al. Red cell distribution width for prognosis in patients with pulmonary embolism: a systematic review and meta-analysis. Clin Respir J. 2020;14(10):901–907. doi:10.1111/crj.13227
- Sartori M, Migliaccio L, Favaretto E, et al. Whole-arm ultrasound to rule out suspected upper-extremity deep venous thrombosis in outpatients. JAMA Intern Med. 2015;175(7):1226–1227. doi:10.1001/jamainternmed.2015.1683
- Vayá A, Suescun M. Hemorheological parameters as independent predictors of venous thromboembolism. Clin Hemorheol Microcirc. 2013;53(1–2):131–141. doi:10.3233/CH-2012-1581
- Saldanha C, De Almeida J. Erythrocyte as a link between basic and clinical research. Clin Hemorheol Microcirc. 2011;49(1–4):463–472. doi:10.3233/CH-2011-1496
- May JE, Marques MB, Reddy VVB, et al. Three neglected numbers in the CBC: the RDW, MPV, and NRBC count. Cleve Clin J Med. 2019;86(3):167–172. doi:10.3949/ccjm.86a.18072
- Nifong TP, McDevitt TJ. The effect of catheter to vein ratio on blood flow rates in a simulated model of peripherally inserted central venous catheters. Chest. 2011;140(1):48–53. doi:10.1378/chest.10-2637
- Isik T. The impact of admission red cell distribution width on the development of poor myocardial perfusion after primary percutaneous intervention. Atherosclerosis. 2012;224(1):143–149. doi:10.1016/j.atherosclerosis.2012.06.017
- Poredoš P. Interrelationship between venous and arterial thrombosis. Int Angiol. 2017;36(4):295–298. doi:10.23736/S0392-9590.17.03820-2
- Branchford BR, Carpenter SL. The role of inflammation in venous thromboembolism. Front Pediatr. 2018;6:142. doi:10.3389/fped.2018.00142
- Vazquez-Garza E, Jerjes-Sanchez C, Navarrete A, et al. Venous thromboembolism: thrombosis, inflammation, and immunothrombosis for clinicians. J Thromb Thrombolysis. 2017;44(3):377–385. doi:10.1007/s11239-017-1528-7
- Najem MY, Couturaud F, Lemarié CA. Cytokine and chemokine regulation of venous thromboembolism. J Thromb Haemost. 2020;18(5):1009–1019. doi:10.1111/jth.14759
- Lippi G, Targher G, Montagnana M, et al. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch Pathol Lab Med. 2009;133(4):628–632. doi:10.5858/133.4.628
- Emans ME, van der Putten K, van Rooijen KL, et al. Determinants of red cell distribution width (RDW) in cardiorenal patients: RDW is not related to erythropoietin resistance. J Card Fail. 2011;17(8):626–633. doi:10.1016/j.cardfail.2011.04.009
- Wang P-F, Song S-Y, Guo H, et al. Prognostic role of pretreatment red blood cell distribution width in patients with cancer: a meta-analysis of 49 studies. J Cancer. 2019;10(18):4305. doi:10.7150/jca.31598
- Bujak K, Wasilewski J, Osadnik T, et al. The prognostic role of red blood cell distribution width in coronary artery disease: a review of the pathophysiology. Dis Markers. 2015;2015:1–12. doi:10.1155/2015/824624
- Münzel T, Hahad O, Kuntic M, et al. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur Heart J. 2020;41(41):4057–4070. doi:10.1093/eurheartj/ehaa460
- Cheng Y-J, Liu Z-H, Yao F-J, et al. Current and former smoking and risk for venous thromboembolism: a systematic review and meta-analysis. PLoS Med. 2013;10(9):e1001515. doi:10.1371/journal.pmed.1001515
- Al-Asadi O, Almusarhed M, Eldeeb H. Predictive risk factors of venous thromboembolism (VTE) associated with peripherally inserted central catheters (PICC) in ambulant solid cancer patients: retrospective single Centre cohort study. Thromb J. 2019;17(1):1–7. doi:10.1186/s12959-019-0191-y
- Al-Nasser B. Influence of tobacco smoking on perioperative risk of venous thromboembolism. Turk J Anaesthesiol Reanim. 2020;48(1):11. doi:10.5152/TJAR.2019.08683