Abstract
Background
Few reports have investigated chatbots in patient care. We aimed to assess the current applications, limitations, and challenges in the literature on chatbots employed in oncological care.
Methods
We queried the PubMed database through April 2022 and included studies that investigated the use of chatbots in different phases of oncological care. The search used five different combinations of the specific terms “chatbot”, “cancer”, “oncology”, and “conversational agent”. Inclusion criteria were chatbot use in any aspect of oncological care—prevention, patient education, treatment, and surveillance.
Results
The initial search yielded 196 records, 21 of which met inclusion criteria. The identified chatbots mostly focused on breast and ovarian cancer (n=8), with the second most common being cervical cancer (n=3). Good patient satisfaction was reported among 14 of 21 chatbots. The most reported chatbot applications were cancer screening, prevention, risk stratification, treatment, monitoring, and management. Of 12 studies examining efficacy of care via chatbot, 9 demonstrated improvements compared to standard care.
Conclusion
Chatbots used for oncological care to date demonstrate high user satisfaction, and many have shown efficacy in improving patient-centered communication, accessibility to cancer-related information, and access to care. Currently, chatbots are primarily limited by the need for extensive user-testing and iterative improvement before widespread implementation.
Introduction
Chatbots are defined as computer programs that process and simulate human conversation by artificially replicating patterns of human interaction through natural language processing.Citation1 Chatbots widely serve as digital assistants to clients, allowing users to express their interests, wishes, and queries naturally by speaking, typing, and pointing.Citation2 They may be implemented through messaging applications, websites, mobile apps, or telephone. The first-ever use of chatbots or related technology started in the 1960s with ELIZA, which used simple keyword matching techniques to try to convince users that they were real humans, giving the illusion of “intelligence.”Citation3 In the following decades, with rapid growth in text and natural-language-based research and improvement in data mining and machine learning techniques, chatbots became more practical, particularly for commercial applications. Voice-based platforms such as Apple’s Siri and IBM’s Watson have been implemented across a variety of social media and technological platforms.Citation4–6 Additionally, other unique real-world applications can be found in conversational artificial intelligence (AI) with Amazon Echo, which implements the voice service Alexa, found in millions of households around the world and generating 4 billion dollars in device revenue in 2020.Citation7 According to UK-based Juniper Research, chatbots are expected to deliver 4 billion dollars in cost savings in the banking sector by 2022.Citation8 The market size for chatbots is expected to expand at a compound annual growth rate of 25.7% over the next 9 years.Citation9
Chatbots remain underutilized in healthcare and its market size in healthcare is expected to proliferate over the next decade. Healthcare chatbots to date have primarily been mobile apps.Citation10–12 The first report of chatbots in healthcare involved an exploratory study in 2010, where the chatbot answered adolescents’ questions related to sex, drugs, and alcohol.Citation13 Since then, development of AI-driven solutions including chatbots into public care had been relatively slow. It was not until the COVID-19 pandemic where utilization of telehealth and health-oriented chatbots significantly increased.Citation14 As a result, scopes have expanded from patient education for common diseases including malignancies.Citation10 Additionally, chatbots have been deployed to suggest behavior, lessen mental health burden, and offer emotional support.Citation15 This high potential for future development can also be supported through the healthcare chatbot market, expected to increase at a compound annual growth rate of 19.16% from 2022 to 2030Citation16 and that chatbots in the healthcare sector are expected to save 3.6 billion dollars globally by 2022.Citation17
Cancer is the second leading cause of death in America.Citation18 With COVID-19 pandemic reducing access to cancer care,Citation19–22 remote and digital cancer care interventions such as chatbots are more relevant than ever before.Citation23 Two scoping reviews in 2019 describe how contemporary chatbots have demonstrated improved accessibility, personalization, and efficiency, with the potential to improve many types of patient care, but only a handful of chatbots are related to cancer care.Citation6,Citation10 There have since been many other studies utilizing chatbots in oncology for preventive screening,Citation24–26 mental health monitoring,Citation27 lifestyle change,Citation28 patient educationCitation6,Citation10,Citation29 etc. Therefore, given the increased number and limited assessment of contemporary chatbot studies particularly in the cancer field as well as the high potential of reducing operating costs, we hereby aimed to provide a more thorough, updated review evaluating the strengths and weaknesses of chatbot studies in oncological care to help guide future technological development.
Methods
Search Strategy
This narrative review consists of searches through PubMed containing biomedical literature from the United States National Institute of Health’s National Library of Medicine. The search used five different combinations of the specific terms “chatbot”, “chat bot”, “cancer”, “oncology”, “disease”, and “conversational agent”. The first combination inputted in the query box on PubMed was “(chat bot) OR (conversational agent)) AND (cancer)”, the second was “((cancer) OR (oncology)) AND ((chatbot) OR (conversational agent))”, the third was “(cancer) AND (chatbot)”, the fourth was “(chatbot) AND (disease)”, and the fifth was “(disease) AND (conversational agent)”. Our five combinations were designed to account for variability in terminology and ensure the comprehensiveness of our search to capture all relevant studies.
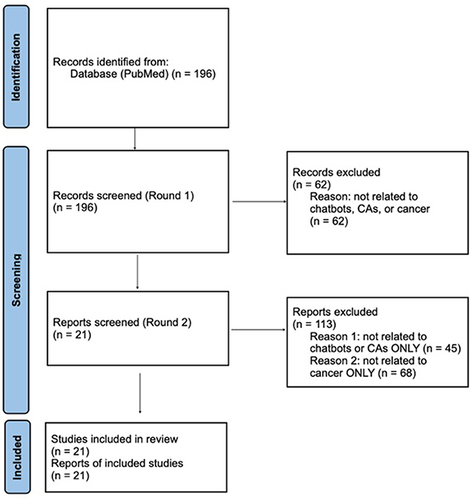
The literature review for these studies began in June 2021 and was collected through April 24, 2022. These studies included where a chatbot was used in any aspect of oncological care – prevention, patient education, treatment, and surveillance. Published articles, abstracts, and ongoing clinical registered on clinicaltrials.gov discussing use of chatbots for medical care were included and noted as such. Excluded were studies used for purposes not related to cancer or chatbots. We explained these specific details and processes in a PRISM diagram (). Data was extracted by one reviewer (AW) and independently verified by another (ZQ).
Figure 1 PRISMA flowchart of literature review process.
Results
The initial search yielded 196 records, 21 of which met inclusion criteria ().
Characteristics of Chatbots
provides the key details of each of the 21 studies included in this review. These key features included phase of oncological care, study period, data source, study design, effect estimates, and key result summaries.
Table 1 Summary Table of Included Studies
Phase of Care and Type of Cancer
The 21 chatbots included in this review were piloted in all phases of clinical care for patients with breast, ovarian, colorectal, cervical, or prostate cancer. Out of these 21 chatbots, 15 of them focused on specific types of cancers with the remaining six chatbots included mixed populations of cancer patients. Eight wchatbots focused on breast cancer,Citation32,Citation33,Citation36,Citation38,Citation43,Citation44,Citation46,Citation48 three of which also included patients with ovarian cancer.Citation36,Citation38,Citation46 Three more chatbots studied cervical cancer,Citation24,Citation30,Citation31 two on colorectal,Citation32,Citation45 one on prostate,Citation25 one on lung,Citation41 and one on head and neck.Citation42
Chatbot Medium
Included chatbots were implemented through different media forms. Nine studies used text and smartphone-based chatbots.Citation33,Citation37–39,Citation41,Citation43,Citation44,Citation47,Citation48 Ten were web-based,Citation24,Citation25,Citation34,Citation35,Citation38,Citation40,Citation42,Citation43,Citation45,Citation46 Three chatbots were voice or speech-based.Citation30–32
Chatbot Objectives
Eleven chatbots were centered on cancer screening, prevention, and risk stratification.Citation24,Citation25,Citation30,Citation31,Citation35,Citation36,Citation38,Citation39,Citation45–47 These chatbots queried patients’ demographic, clinical, and family histories to inform the decision-making process in cancer screening and prevention.Citation24 To narrow the disparity in cervical cancer care among Hispanic women, Wu et al designed a chatbot acting as a virtual educator to close the knowledge gap regarding cervical cancer screening between Hispanic women from rural US and the general US population.Citation24 Owens et al focused on improving a patient’s cancer knowledge, technology use, and cancer screening decision-making through the screening process.Citation25 Sato et al used a chatbot to screen for family history of breast and ovarian cancer and determine if patients met the National Comprehensive Cancer Network BRCA1/2 testing criteria.Citation36 Additionally, five studies focused on genetic or vaccine counseling to help with cancer prevention.Citation30,Citation31,Citation39,Citation46,Citation47 Two of these studies asked patient for their opinions and beliefs on HPV vaccine to improve vaccine uptake for cervical cancer prevention.Citation30,Citation31 Chavez-Yenter et al used a chatbot to educate patients on cancer risk genetic testing and Kaphingst et al used a chatbot for education on testing for inherited cancer syndromes.Citation39,Citation47 Siglen et al performed digital conversations with breast or ovarian cancer patients about genetic BRCA testing.Citation46
Seven chatbots included in this review focused on cancer treatment, monitoring, and management.Citation33,Citation37,Citation41–44,Citation48 These chatbots answered common questions asked by breast and lung cancer patients about their treatments.Citation41,Citation43,Citation44,Citation48 Chatbots from these studies also addressed the concerns of breast cancer patients via designed texts,Citation41 measured medication adherence rates,Citation37,Citation41 and gave out weekly questionnaires.Citation37,Citation42
In addition to treatment and management, two chatbots were designed to educate patients on technology use and oncologists on communication-skills.Citation34,Citation40 Bickmore et al provided a conversational search experience to help individuals with low health and computer literacy find and learn about cancer-related clinical trials.Citation34 Instead of educating patients, Stuij et al used a chatbot to help oncologists learn communication-skills by providing individualized feedbacks.Citation40 Finally, Mlakar et al focused on cancer survivorship. Their chatbot focused on lifestyle modifications, self-efficacy, and patient reported quality of life among cancer survivors.Citation32
Evaluation of Chatbots
Acceptability
Sixteen of 21 articles studied the acceptability of their respective chatbots.Citation25,Citation30,Citation33–46,Citation48 Five studies are still awaiting published results to be posted or currently do not have results published online.Citation24,Citation31,Citation32,Citation43,Citation47 Acceptability was high in most studies, with only one demonstrating low satisfaction ratings.Citation41 For example, acceptability of chatbots was evidenced by positive user comments on how convenient the chatbot was to use, high usability scores and compliance rates.Citation37 Chetlen et al even found that 33% of women strongly agreed and 54% of women agreed that a chatbot made it easier for them to understand their upcoming breast biopsy procedure.Citation44 Siglen et al measured the fallback or error rates of the chatbot to determine its efficacy and satisfaction among patients.Citation46 Through the first testing trial, the chatbot showed an expected high fallback rate of 43%, leaving a substantial fraction of wrong answers, but eventually ended with a fallback rate of less than 15% for its fourth and final iteration.Citation46 Bibault et al suggested that chatbots led to higher patient satisfaction score in cancer counseling compared to a control physician.Citation48 Patients in Stuij et al expressed a willingness to continue using a chatbot for cancer education.Citation40 However, if some of the chatbots did not have satisfaction or usability assessments, acceptability was determined by the number of patients that completed the chatbot conversation or the length of time taken to complete chat. Three chatbots had completion rates of at least 67%,Citation37,Citation38,Citation45 and two had low completion rates below 32%,Citation35,Citation39 with one averaging 10–14 min to complete the conversation with the chatbot.Citation35
Performance
In addition to assessing user acceptability and satisfaction among chatbots, 12 studies assessed the effectiveness and usefulness of chatbots.Citation30,Citation34,Citation37–42,Citation44 Five articles discussed howchatbots significantly improved patient monitoring, symptom management, and medication adherence with frequent reminders.Citation33,Citation37,Citation42,Citation44,Citation48 The majority of these studies found chatbots to be helpful with management of chemotherapy, radiation therapy, and other treatment-related symptoms. For instance, Bibault et al designed a chatbot to answer common questions asked by patients with breast cancer about their therapy management. These questions were related to breast cancer stages and causes, whether the cancer is under control, types, benefits, and side effects of treatments, and questions related to care outside of the hospital. 85% of patients found answers helpful compared to 82% with a physician.Citation48 Chaix et al used a chatbot to address questions about breast cancer while also reinforcing medication adherence by providing prescription reminders throughout the conversations. This resulted in 88% of patients reporting that the chatbot provided them with support and helped them follow their treatment effectively.Citation33 Piau et al described a chatbot that collects key patient data such as chemotherapy-related symptoms and adherence to medicine to optimize monitoring of older patients with cancer.Citation37 The primary goal of the chatbot was to free up nurses’ time so that on phone calls, they could focus more on education and support rather than recording symptoms.Citation37 Ma et al utilized a chatbot to aid self-management of symptoms such as pain, nausea, salivary duct inflammation, and xerostomia from radiation therapy in head and neck cancer patients, and 61% of patients reported that the chatbot helped with symptom self-management, reducing the need to call the care team.Citation42 Chetlen et al used a chatbot to provide evidence-based answers to frequently asked questions about breast biopsy. They found that around 25% of women in the study strongly agreed, and 49% of women agreed that the chatbot improved their quality of life and care.Citation44
Other studies defined effectiveness by how much the patient learned through genetic testingCitation39 or improved search ability for clinical trials compared to a control conventional interface (non-AI).Citation34 Stuij et al’s study found that users in a communication skills training program claimed texts between the chatbot were “easier to read than a book” and users liked the generation of reminders.Citation40 However, users preferred a conventional e-learning platform that allowed them to learn skills more comfortably than the somewhat fragmented approach of a chatbot.Citation40 In addition, two studies aimed to improve shared decision-making, one resulting in a statistically significant improvement in knowledge of prostate cancer and technology use,Citation25 and the other influencing patient beliefs in the use of HPV vaccine for cervical cancer prevention.Citation32 While most of these studies demonstrated efficacy as variably defined by the authors, Kataoka et al reported that many times, patients “did not get a proper answer” from its chatbot.Citation41 Thus, the chatbot only had an average satisfaction rating of 54%, adherence was low, and no improvement was seen in knowledge of lung cancer symptom management.Citation41
Discussion
With advances in artificial intelligence and machine learning technology, increasing efforts have been made to use chatbots to automate specific aspects of oncological care. This review provides a more contemporary, extensive evaluation of chatbots in oncological care. We found that chatbots have great acceptability and efficacy in automating and improving aspects of oncological care, mostly due to their ability to engage in personalized conversations and patient-centered communication. Chatbots have high future potential to increase the outcomes of all types of oncological care including cancer screening, prevention and risk stratification, treatment and symptom management, patient education, and survivorship. These improved outcomes include expansion of cancer-related information, treatment to caregivers and doctors, and better oncological care accessibility for minority groups. Given chatbots’ ability to save operating costs and replace many forms of communication throughout all phases of care, they have high marketability and potential for widespread implementation.
Overall, most chatbots included in this study were well-received by cancer patients. The high acceptability and satisfaction ratings shared by many included chatbot studies could be related to ever-improving AI technology, making responses by chatbots perceived as personal and caring.Citation30,Citation31,Citation48 Some patients even perceived speaking with a chatbot an easier and more personal experience compared to healthcare providers. For example, patients from Chaix et al interacted with a chatbot named Vik, which used personalized text messages with combinations of questions and actions of contextual information to allow users access to information they would not have thought of and allowing conversations to be more flexible and natural.Citation33 As further support for the success of personalized chatbots, 87% of breast biopsy patients from Stuij et al agreed or strongly agreed that the chatbot made it easier to understand their upcoming procedure, regardless of their perceived technology proficiency.Citation44
Chatbots may also help effectively overcome communication challenges rooted in demographic disparities such as language barriers and low health literacy, increasing access to care for minority groups.Citation30 Bickmore et al showed that 36% of low literacy participants were able to find a correct clinical trial using the chatbot compared to 0% using a conventional search interfaceCitation34 Wu et al specifically targeted Hispanic women from rural agricultural communities and employed a chatbot to increase their knowledge related to cervical cancer and close the knowledge gap between Latina women and the general population.Citation24 With cancer screening and genetic counseling, chatbots have a high potential to improve the efficiency of these processes by being able to access regions outside of a local hospital or town. Heald et al determined that the chatbot from their study allowed more patients to receive genetic counseling and screening services than would have been possible through individual, in-person appointments.Citation45 The chatbot from this study was also able to provide accessible and timely care to patients from broader geographical regions. Therefore, with more people having access to screening appointments, diagnoses can be made earlier and can possibly decrease the risk of death.
Additionally, chatbots are able to improve care outcomes by allowing education related to cancer to be extended to and available to caregivers, families, and even oncologists. For instance, Kataoka et al aimed to educate lung cancer patients and their caregivers on symptom management, but chatbot satisfaction was low.Citation40,Citation41 The use of a standardized chatbot system can save time and effort of in-person oncologists when educating these additional family members. Stuij et al also used a chatbot to train healthcare professionals to more effectively communicate and educate patients; the chatbot did not interface with the patients.Citation40 Oncologists found the chatbot conversations more convenient to read and engaging than a textbook and users liked generation of reminders and personalized support, helping with their communication skills training.Citation40 Because chatbots designed for caretakers and healthcare professionals are limited, more research should be done to explore how chatbots may empower these groups to better care for patients with cancer.
From a system-level perspective, with cancer-attributed costs in the United States projected to increase by 30% from 2015 to 2030,Citation49 rising expenditures caused by an aging and growing US populationCitation50 and increasing treatment costs only create more interest in the cost-saving capabilities of chatbots.Citation24,Citation39,Citation44,Citation48 This creates a significant market for chatbots in oncological care: with cancer being among the top 10 leading causes of death in the worldCitation51 and an extensive marathon process, patient communication is crucial in every phase of care given the limited amount of time doctors often have. Similar to how UberEats has evolved their customer service by changing to a live chat system, which starts with a chatbot response that filters out customer problems and redirects the customer to a human representative, the same counterparts can be used with cancer chatbots;Citation52 by taking care of more basic tasks in educating patients about symptoms, screening for cancer, care coordination, and payments, specialized doctors can be directed to patients for more complex care. One specific way chatbots can be implemented to save operating costs is by automating tedious tasks such as collecting data about medication adherence and symptom management so nurses can devote more time to personalized training and support of patients.Citation37 Piau et al found that one of the most valuable benefits patients received from using a conventional phone monitoring approach was moral support (44%), showing the importance of personalized treatment from nurses.Citation37 By freeing up nurses’ time, chatbots, which are generally free or low cost and can be used at any time opposed to nurses, have the potential to save labor costs, which in 1999 accounted for 31.0% of healthcare expenditures in the United States.Citation53 However, since the COVID-19 pandemic, median labor expenses in hospitals across the US have rose over 37%.Citation54 With chatbots having the potential to save billions of dollars in the healthcare industry,Citation9 they provide a promising avenue for commercialization.
Limitations of Chatbots
One factor that limits the utility of chatbots is that they may sometimes have difficulty understanding patients and may not be able to provide adequate responses to specific categories of questions at the beginning stages of use or during development. For example, in a study conducted in Japan, the mean satisfaction score was about 30% or more lowerCitation41 than other studiesCitation33,Citation37,Citation42,Citation44,Citation48 mostly because this was the first chatbot educating lung cancer patients compared to previous chatbots mainly dealing with breast cancer.Citation33,Citation37,Citation42,Citation44,Citation48 Additionally, Siglen et al initially had difficulty with chatbot-patient communication and had a high error rate, but this percentage eventually decreased in half after the final iteration of the study.Citation32 However, these inaccuracies were not too significant, because more popular chatbots for breast cancer had very little satisfaction or engagement issues.Citation33,Citation37,Citation42,Citation44,Citation48 Although chatbots are currently improving with more advanced algorithms and expanded databases, their accuracies do not need to be perfect to accomplish basic communication tasks that complement current oncological care. Based on most of the chatbots in this review, they are not expected to replace doctors, but primarily to assist them and improve the overall efficiency of the care process, which should also be the expectation for the near future given the current state of chatbot technology.
Another limitation that chatbots pose is possibly being inequitable and further excluding marginalized populations. Because AI chatbots only learn based on the inputs given to them such as data and algorithms, hidden bias can creep into the chatbots’ performance, decreasing its accuracy and possibly being harmful to patients. For instance, if training data ignore certain target groups such as ones with different types of accents or slang, it will skew the ability for chatbots to understand user responses and may possibly recommend wrong treatments, which can be detrimental. In addition, Microsoft chatbot Tay was quickly taken down by tweeting racist comments in 2016 since it was trained on public Twitter conversations with human biases.Citation55 However, while eliminating this unconscious bias is not straightforward, it can be mitigated is by having a representational set of users and data as well as developers being more aware of humans’ cognitive biases. Aside from AI, despite chatbots being used to expand treatment to minority groups, other underprivileged groups or patients with low tech literacy that may barely be able to manage emails can be left behind, possibly creating challenges for implementation across all types of patients.
This review also demonstrates that the majority of chatbots are text-based or web-based, with only three studies primarily using voice or speech-based platforms. While text- or web-based chatbots may be technologically easier to implement, patients may find typing on a small keyboard or smartphone challenging and time-consuming compared to voice- or speech-based platforms. More research using voice-based chatbots will reveal whether they yield increased usability and satisfaction rates. Furthermore, only three studies included chatbots, which had avatars or visual diagrams to assist the main chatbot interface.Citation24,Citation25,Citation34 Including more realistic visual components to chatbots such as advanced, real-time animations or simulations of virtual clinical environments with relevant equipment can help patients fulfill their needs more efficiently. Additional possible limitations of the included text-based chatbots were high dropout rates and low utilization due to the need for application downloads and regular updates.Citation56 Only one study from France assessed retention rates of users actively using the chatbot, which decreased by about 70% after 8 months.Citation33 However, popular messaging apps such as Facebook Messenger, iMessage, Telegram, WeChat, or WhatsApp do not experience these types of dropout rates since they are commonly used in the general population.Citation10 Thus, future research using chatbots embedded into these types of regularly used platforms can assess whether or not they increase retention rates.
Finally, regulatory and security issues will need to be addressed to fully realize the potential of chatbots in oncological care. While some patients report increased comfort in discussing sensitive matters with chatbots, others report concern about private and sensitive data being shared; Stuij et al found some patients felt vulnerable being recorded and hesitated to share sensitive information until they had additional conversations with the chatbot.Citation40 Businesses and companies of these chatbots will need to find verifiable solutions and transparency to consumers to counteract fear and distrust. In terms of regulation, while the Food and Drug Administration does have a process to regulate AI-enabled products used in health care, only 0.1% of healthcare apps on the market in 2014 were FDA approved.Citation57 This can be problematic for AI chatbot technologies because without human regulation to capture possible biases in training data, the patient can be led with false or missing information, which was the case at the Royal Society of Medicine, where a doctor regular tweeted complaints of Babylon’s health AI chatbot missing potentially significant red flag symptoms.Citation58 In the future, more human intervention will be needed to manage and override suggestions from chatbots and more high-quality assurance regulations will need to be implemented, examining detailed processes on how chatbots make their decisions.
Strengths and Limitations of Review
This review implemented a comprehensive search through the PubMed search engine using a wide range of keywords, yielding a greater number of studies involving chatbots related to oncological care than other reviews to date.Citation6,Citation10,Citation12 While PubMed is a well-established and widely used database for biomedical research, it primarily contains studies conducted in the United States and other high-income countries, which may not include all relevant studies published in non-English languages and other countries that were not indexed. This review is also limited by the quality of available studies, many of which included chatbots that were still in the pilot or feasibility stage, often at single-institutions, with small sample sizes, heterogeneity in acceptability and efficacy data, and no long-term followup.Citation36,Citation41,Citation44,Citation47 Given such limited study of chatbots used in oncological care, the field has enormous potential for improvement as chatbot technologies advance and are increasingly implemented and studied.
Conclusion
Studies evaluating chatbots are still rare in healthcare and especially oncology. However, recent years have shown a sharp rise in the number of these studies, with benefits for patients, caregivers, and oncologists. This review summarizes the extant literature to date, demonstrating that chatbots are highly acceptable to patients as well as effective in automating tasks related to cancer screening, prevention, and risk stratification, treatment and symptom management, and survivorship. By facilitating patient-centered communication, increasing access to care, reducing operating costs, and saving time for nurses and doctors, chatbots have great potential for future implementation and commercialization. However, because of technological complexity of AI technology, a great deal of user testing and iterative improvements are needed to optimize user satisfaction and acceptability before widespread implementation is possible. Therefore, over time, chatbots will need to have access to richer data sets to increase their knowledge of medical terms, symptoms, and treatments for potential widespread and more independent use.
Disclosure
QDT reports personal fees from Astellas, Bayer, and Janssen, outside the scope of the submitted work. QDT reports research funding from the American Cancer Society, the Defense Health Agency, and Pfizer Global Medical Grants. APC reports research funding from the American Cancer Society and Pfizer Global Medical Grants. LB reports personal fees from Delfina Inc outside the scope of the submitted work and research funding from the Office of Scholarly Engagement at Harvard Medical School. LOR reports research funding from J. William Fulbright Foreign Scholarship and Brazilian National Council for Scientific and Technological Development – CNPq, Research Productivity: 304747/2018-1 and 310135/2022-2. The authors report no other conflicts of interest in this work.
References
- Expert.ai. Chatbot: what is a chatbot? Why are chatbots important? Available from: https://www.expert.ai/blog/chatbot/. Accessed 24 April 2023.
- Shawar BA, Atwell E. Chatbots: are they really useful? 2007. Available from: https://www.researchgate.net/publication/220046725_Chatbots_Are_they_Really_Useful. Accessed April 23, 2022.
- Weizenbaum J. ELIZA—a computer program for the study of natural language communication between man and machine. Commun ACM. 1966;9(1):36–45. doi:10.1145/365153.365168
- Onlim Blog. The history of chatbots - from ELIZA to ALEXA. Available from: https://onlim.com/en/the-history-of-chatbots/. Accessed March 18, 2022.
- Dilmegani C. Top 60 chatbot companies in 2022: in-depth guide. Ai multiple; 2017. Available from: https://research.aimultiple.com/chatbot-companies/. Accessed July 8, 2022.
- Bibault JE, Chaix B, Nectoux P, Pienkowsky A, Guillemasse A, Brouard B. Healthcare ex machina: are conversational agents ready for prime time in oncology? Clin Transl Radiat Oncol. 2019;16:55–59. doi:10.1016/j.ctro.2019.04.002
- Business Insider. Amazon echo Alexa Add $11 billion in revenue by 2020. Available from: https://www.businessinsider.com/amazon-echo-alexa-add-11-billion-in-revenue-by-2020-2016-9. Accessed July 8, 2022.
- Chatbots to deliver $8 billion in conversation cost savings by 2022. Available from: https://www.juniperresearch.com/resources/analystxpress/july-2017/chatbot-conversations-to-deliver-8bn-cost-saving. Accessed July 8, 2022.
- Grand View Research. Chatbot market size, share & growth report, 2022–2030 [Internet]; 2022c. Available from: https://www.grandviewresearch.com/industry-analysis/chatbot-market. Accessed April 19, 2023.
- Car LT, Dhinagaran DA, Kyaw BM, et al. Conversational agents in health care: scoping review and conceptual analysis. J Med Internet Res. 2020;22(8):e17158. doi:10.2196/17158
- Hall AK, Cole-Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Ann Rev Public Health. 2015;36:393–415. doi:10.1146/annurev-publhealth-031914-122855
- Safi Z, Abd-Alrazaq A, Khalifa M, Househ M. Technical aspects of developing chatbots for medical applications: scoping review. J Med Internet Res. 2020;22(12):e19127. doi:10.2196/19127
- Crutzen R, Peters GJY, Portugal SD, Fisser EM, Grolleman JJ. An artificially intelligent chat agent that answers adolescents’ questions related to sex, drugs, and alcohol: an exploratory study. J Adolesc Health. 2011;48(5):514–519. doi:10.1016/j.jadohealth.2010.09.002
- Parviainen J, Rantala J. Chatbot breakthrough in the 2020s? An ethical reflection on the trend of automated consultations in health care. Med Health Care Philos. 2022;25(1):61–71. doi:10.1007/s11019-021-10049-w
- JCL; XLSLLKC. Chatbot for health care and oncology applications using artificial intelligence and machine learning: systematic review [Internet]. JMIR cancer. U.S. National Library of Medicine; 2023. Available from: https://pubmed.ncbi.nlm.nih.gov/34847056/. Accessed April 19, 2023.
- Healthcare chatbots market size, share, trends, opportunities & forecast [internet]. Verified Market Research. Available from: https://www.verifiedmarketresearch.com/product/healthcare-chatbots-market/. Accessed July 8, 2022.
- Xenioo. Healthcare chatbot: the future of the health industry through AI [Internet]. Xenioo; Available from: https://www.xenioo.com/healthcare-chatbot-the-future-of-the-health-industry-through-ai/. Accessed July 8, 2022.
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. doi:10.3322/CAAC.21708
- Labaki C, Schmidt AL, Bakouny Z, et al. Temporal changes in the screening, diagnosis and surgical treatment of genitourinary (GU) malignancies during the COVID-19 pandemic. J Clin Oncol. 2022;40(6_suppl):281. doi:10.1200/JCO.2022.40.6_SUPPL.281
- Sokas C, Kelly M, Sheu C, et al. ASO visual abstract: cancer in the shadow of COVID: early-stage breast and prostate cancer patient perspectives on surgical delays due to COVID-19. Ann Surg Oncol. 2021;28(S3):545. doi:10.1245/S10434-021-10343-0
- Sokas C, Kelly M, Sheu C, et al. Cancer in the shadow of COVID: early-stage breast and prostate cancer patient perspectives on surgical delays due to COVID-19. Ann Surg Oncol. 2021;28(13):8688–8696. doi:10.1245/s10434-021-10319-0
- Tan WS, Marchese M, Paciotti M, et al. Delay in surgery for cT1b-2 kidney cancer beyond 90 days is associated with poorer survival: implications for prioritization during the COVID-19 pandemic. Minerva Urol Nefrol. 2021;73(3):404–406. doi:10.23736/S2724-6051.20.04197-1
- Briggs LG, Labban M, Alkhatib K, Nguyen DD, Cole AP, Trinh QD. Digital technologies in cancer care: a review from the clinician’s perspective. J Comp Eff Res. 2022;11(7):533–544. doi:10.2217/CER-2021-0263
- Wu Y, Samant D, Squibbs K, Chaet A, Morshedi B, Barnes LE. Design of interactive cancer education technology for latina farmworkers. Proc IEEE Syst Inf Eng Des Symp. 2014;2014:1–5. doi:10.1109/SIEDS.2014.6829908
- Owens OL, Felder T, Tavakoli AS, et al. Evaluation of a computer-based decision aid for promoting informed prostate cancer screening decisions among African American men: iDecide. Am J Health Promot. 2019;33(2):267–278. doi:10.1177/0890117118786866
- Kobori Y, Osaka A, Soh S, Okada H. Novel application for sexual transmitted infection screening with an AI chatbot. J Urol. 2018;199(Suppl 4):e218. doi:10.1016/j.juro.2018.02.516
- Morris RR, Kouddous K, Kshirsagar R, Schueller SM. Towards an artificially empathic conversational agent for mental health applications: system design and user perceptions. J Med Internet Res. 2018;20(6):e10148. doi:10.2196/10148
- Zhang J, Oh YJ, Lange P, Yu Z, Fukuoka Y. Artificial intelligence chatbot behavior change model for designing artificial intelligence chatbots to promote physical activity and a healthy diet: viewpoint. J Med Internet Res. 2020;22(9):e22845. doi:10.2196/22845
- Rebelo N, Sanders L, Li K, et al. Learning the treatment process in radiotherapy using an artificial intelligence–assisted chatbot: development study [Internet]. JMIR Form Res. 2022;6(12):e39443. doi:10.2196/39443
- Amith M, Lin R, Cunningham R, et al. Examining potential usability and health beliefs among young adults using a conversational agent for HPV vaccine counseling - PubMed. AMIA Summits Transl Sci Proc. 2020;2020:7–16. doi:10.1145/3380991.3383937
- Amith M, Lin R, Cui L, et al. An ontology-powered dialogue engine for patient communication of vaccines - PubMed. CEUR Workshop Proc. 2019;2539:55–60. PMID: 32704245.
- Mlakar I, Lin S, Aleksandraviča I, et al. Patients-centered SurvivorShIp care plan after Cancer treatments based on big data and artificial intelligence technologies (PERSIST): a multicenter study protocol to evaluate efficacy of digital tools supporting cancer survivors. BMC Med Inform Decis Mak. 2021;21(1):39. doi:10.1186/s12911-021-01603-w
- Chaix B, Bibault JE, Pienkowski A, et al. When chatbots meet patients: one-year prospective study of conversations between patients with breast cancer and a chatbot. JMIR Cancer. 2019;5(1):e12856. doi:10.2196/12856
- Bickmore TW, Utami D, Matsuyama R, Paasche-Orlow MK. Improving access to online health information with conversational agents: a randomized controlled experiment. J Med Internet Res. 2016;18(1):e1. doi:10.2196/JMIR.5239
- Welch BM, Allen CG, Ritchie JB, Morrison H, Hughes-Halbert C, Schiffman JD. Using a chatbot to assess hereditary cancer risk. JCO Clin Cancer Inform. 2020;4(4):787–793. doi:10.1200/CCI.20.00014
- Sato A, Haneda E, Suganuma N, Narimatsu H. Preliminary screening for hereditary breast and ovarian cancer using a chatbot augmented intelligence genetic counselor: development and feasibility study. JMIR Form Res. 2021;5(2):e25184. doi:10.2196/25184
- Piau A, Crissey R, Brechemier D, Balardy L, Nourhashemi F. A smartphone chatbot application to optimize monitoring of older patients with cancer. Int J Med Inform. 2019;128:18–23. doi:10.1016/J.IJMEDINF.2019.05.013
- Nazareth S, Hayward L, Simmons E, et al. Hereditary cancer risk using a genetic chatbot before routine care visits. Obstet Gynecol. 2021;138(6):860–870. doi:10.1097/AOG.0000000000004596
- Chavez-Yenter D, Kimball KE, Kohlmann W, et al. Patient interactions with an automated conversational agent delivering pretest genetics education: descriptive study. J Med Internet Res. 2021;23(11):e29447. doi:10.2196/29447
- Stuij SM, Drossaert CHC, Labrie NHM, et al. Developing a digital training tool to support oncologists in the skill of information-provision: a user centred approach. BMC Med Educ. 2020;20(1):81. doi:10.1186/S12909-020-1985-0
- Kataoka Y, Takemura T, Sasajima M, Katoh N. Development and early feasibility of chatbots for educating patients with lung cancer and their caregivers in Japan: mixed methods study. JMIR Cancer. 2021;7(1):e26911. doi:10.2196/26911
- Ma D, Orner D, Ghaly MM, et al. Automated health chats for symptom management of head and neck cancer patients undergoing radiation therapy. Oral Oncol. 2021;122:105551. doi:10.1016/j.oraloncology.2021.105551
- Chaix B, Delamon G, Guillemassé A, Brouard B, Bibault JE. Psychological distress during the COVID-19 pandemic in France: a national assessment of at-risk populations. Gen Psychiatr. 2020;33(6):e100349. doi:10.1136/GPSYCH-2020-100349
- Chetlen A, Artrip R, Drury B, Arbaiza A, Moore M. Novel use of chatbot technology to educate patients before breast biopsy. J Am Coll Radiol. 2019;16(9Pt B):1305–1308. doi:10.1016/j.jacr.2019.05.050
- Heald B, Keel E, Marquard J, et al. Using chatbots to screen for heritable cancer syndromes in patients undergoing routine colonoscopy. J Med Genet. 2021;58(12):807–814. doi:10.1136/jmedgenet-2020-107294
- Siglen E, Vetti HH, Lunde ABF, et al. Ask Rosa - the making of a digital genetic conversation tool, a chatbot, about hereditary breast and ovarian cancer. Patient Educ Couns. 2022;105(6):1488–1494. doi:10.1016/j.pec.2021.09.027
- Kaphingst KA, Kohlmann W, Chambers RL, et al. Comparing models of delivery for cancer genetics services among patients receiving primary care who meet criteria for genetic evaluation in two healthcare systems: BRIDGE randomized controlled trial. BMC Health Serv Res. 2021;21(1):494. doi:10.1186/S12913-021-06489-Y
- Bibault JE, Chaix B, Guillemassé A, et al. A chatbot versus physicians to provide information for patients with breast cancer: blind, randomized controlled noninferiority trial. J Med Internet Res. 2019;21(11):e15787. doi:10.2196/15787
- Cancer Care Costs. AACR | news releases; 2022. Available from: https://www.aacr.org/about-the-aacr/newsroom/news-releases/cancer-care-costs-in-the-united-states-are-projected-to-exceed-245-billion-by-2030/. Accessed April 19, 2023.
- Financial Burden of Cancer Care. Cancer trends progress report [Internet]; 2022. Available from: https://progressreport.cancer.gov/after/economic_burden. Accessed April 19, 2023.
- World Health Organization. The top 10 causes of death [Internet]; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed April 19, 2023.
- All topics | restaurants - uber help [Internet]; 2022. Available from: https://help.uber.com/ubereats/restaurants. Accessed April 19, 2023.
- Woolhandler S, Campbell T, Himmelstein DU. Costs of health care administration in the United States and Canada. N Engl J Med. 2003;349(8):768–775. PMID: 12930930. doi:10.1056/NEJMSA022033
- Hospitals’ per patient labor spend increased 37% from 2019 to Q1 2022 [Internet]. Fierce Healthcare; 2022. Available from: https://www.fiercehealthcare.com/providers/hospitals-patient-labor-spend-increased-37-2019-q1-2022. Accessed April 19, 2023.
- Zemčík T. Failure of chatbot tay was evil, ugliness and uselessness in its nature or do we judge it through cognitive shortcuts and biases? AI Soc. 2020;36(1):361–367. doi:10.1007/s00146-020-01053-4
- Lee K, Kwon H, Lee B, et al. Effect of self-monitoring on long-term patient engagement with mobile health applications. PLoS One. 2018;13(7):e0201166. doi:10.1371/journal.pone.0201166
- Cortez N, Cohen IG, Kesselheim AS. FDA regulation of mobile health technologies [Internet]. Social Science Research Network; 2014. Available from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2512458. Accessed April 19, 2023.
- Iacobucci G. Row over Babylon’s chatbot shows lack of regulation. BMJ. 2020;368:m815. PMID: 32156741. doi:10.1136/bmj.m815
