Abstract
Aim
We investigated the clinical usefulness of mean corpuscular hemoglobin concentration (MCHC) in patients with pneumoconiosis.
Methods
We retrospectively investigated the medical records from 52 patients with pneumoconiosis, and erythrocyte parameters were analyzed in pneumoconiosis patients with different stages.
Results
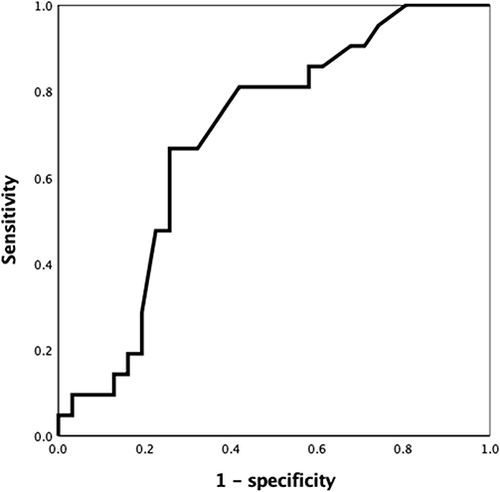
Here, we found that the values of MCHC were significantly lower in III stage pneumoconiosis than those with I/II stage (p = 0.024), and there was no significantly difference in MCHC between smoking pneumoconiosis patients and non-smoking pneumoconiosis patients. A negatively correlation between MCHC and disease stage was observed in patients with pneumoconiosis (r = −0.298, p = 0.032). In multiple linear regression analysis, the MCHC was found to be independently associated with advanced pneumoconiosis in patients with pneumoconiosis (p=0.011). The results of logistic regression analysis indicated that decreased MCHC was an independent risk factor of advanced pneumoconiosis in patients with pneumoconiosis (OR: 0.936, CI95%: 0.877–0.999, p = 0.046). Receiver operating characteristic curve analysis showed that the optimal cutoff value of MCHC was 330 g/L to identify advanced pneumoconiosis with the area under the curve of 0.694 (CI95%:0.550–0.839, p = 0.018).
Conclusion
The decreased MCHC is associated with advanced pneumoconiosis, and MCHC may be used as a monitoring marker for follow-up of pneumoconiosis patients.
Introduction
Pneumoconiosis is an occupational disease resulting from the inhalation of dust, pneumoconiosis has a relatively high morbidity in recent years, and it is still an occupational health problem due to the lack of protective measures.Citation1 Early diagnosis of pneumoconiosis is beneficial to prevent further lung damage for workers with occupational exposure, clinically, the clinical assessment of pneumoconiosis is main based on radiological findings.Citation1 However, few study explores the clinical application of easily available biomarkers in patients with pneumoconiosis.
Mean corpuscular hemoglobin concentration (MCHC) is the hemoglobin concentration of per liter blood.Citation2 The literatures in regard to clinical application of MCHC have been emerging over the years. Several studies have reported that MCHC is associated with various diseases such as depression, hepatorenal syndrome and acute myocardial infarction.Citation3–5 Interesting, MCHC also seem to be associated with pulmonary disease. Lower MCHC has been found to be a risk factor for increased mortality in patients with acute pulmonary embolism,Citation6 and decreased MCHC has an association with unfavorable prognosis of resected lung cancer.Citation7 Recently, the variation of hemoglobin-related parameters has been reported in patients with pneumoconiosis.Citation8 However, the association between MCHC and lung disorders, such as pneumoconiosis, still remains unclear. In this study, we aimed to examine the clinical usefulness of MCHC in patients with pneumoconiosis.
Patients and Methods
A total of 52 patients with pneumoconiosis were included retrospectively. Pneumoconiosis patients were diagnosed according to the history of occupational exposure and radiological features, and the disease stage of pneumoconiosis patients was classified as I, II and III stage according to the radiological severity, the staging criteria is similar to the classification system of International Labor Organization criteria.Citation9–11 We excluded pneumoconiosis patients who had following diseases: coronary heart disease, diabetes mellitus, hypertension, liver disease, kidney disease, autoimmune disease, hemolytic disease, chronic obstructive pulmonary disease, asthma, bronchiectasis, lung abscess and malignancy.
We reviewed the admission examinations of pneumoconiosis patients retrospectively, thereinto, erythrocyte parameters were obtained, including red blood cell, hematocrit, mean corpuscular volume, mean corpuscular hemoglobin and mean corpuscular hemoglobin concentration. The study was approved by the Ethics Committee of The Affiliated Hospital of Youjiang Medical University for Nationalities, and conformed to the Declaration of Helsinki. Informed consent of patients was exempted due to the retrospective design of the study, and patient data confidentiality was rigorously protected in this study.
Statistics
The continuous variables are expressed as the mean ± standard deviation for normal distribution and median (interquartile range) for non-normal distribution, categorical variables are expressed as percentage. The continuous variables were compared with Student’s t-test or Mann–Whitney U-test when needed, whereas, the categorical variables with compared with Chi-square test or Fisher’s exact test appropriately. Pearson’s or Spearman correlation analysis was used for the correlation between parameters appropriately. The determinants of the dependent variable were revealed by multiple linear regression analysis and logistic regression analysis. Finally, the discriminating performance for advanced pneumoconiosis was estimated by receiver operating characteristic curve analysis. The statistical analysis was performed by SPSS 25.0 software version. Statistical significance was defined as a p value <0.05.
Results
The Characteristics in Pneumoconiosis Patients with Different Stage
The characteristics of pneumoconiosis patients are presented in . Pneumoconiosis with III stage is clinically defined as advanced pneumoconiosis; thus, the differences of characteristics were compared between I/II stage pneumoconiosis and III stage pneumoconiosis. The results found that MCHC was significantly decreased in III stage pneumoconiosis compared to those with I/II stage (p = 0.024), from this, the MCHC was further analyzed.
Table 1 The Characteristics in Patients with Different Stage Pneumoconiosis
The Characteristics in Pneumoconiosis Patients with Smoking and Non-Smoking
Cigarette smoking has effects on hematological parameters including hematocrit levels, mean corpuscular volume and MCHC,Citation12 thus, we further compared the differences in hematological parameters between smoking pneumoconiosis patients and non-smoking pneumoconiosis patients. The results showed that red blood cell, hemoglobin, hematocrit, mean corpuscular volume, mean corpuscular hemoglobin and MCHC had no significantly differences between the two groups, furthermore, there were significantly differences between the two groups in sex, age, body mass index, pulmonary tuberculosis history and pneumoconiosis with stage I/II vs III.
The Multiple Linear Regression Analysis Between MCHC and Advanced Pneumoconiosis in Patients with Pneumoconiosis
The MCHC was negatively correlated with disease stage (r = −0.298, p = 0.032), and the MCHC was positively correlated with body mass index (r = 0.349, p = 0.011), hemoglobin (r = 0.571, p < 0.001), hematocrit (r = 0.304, p = 0.029) and mean corpuscular hemoglobin (r = 0.629, p < 0.001) in patients with pneumoconiosis, as shown in . Multiple linear regression analysis was further performed for adjustment of underlying confounding factors, the MCHC showed an independent association with advanced pneumoconiosis (p=0.011), with adjustment for gender, age, body mass index, smoking history, pulmonary tuberculosis history, hemoglobin, hematocrit and mean corpuscular hemoglobin ().
Table 2 The Correlation Between MCHC and Continuous Parameters in Patients with Pneumoconiosis
Table 3 The Multiple Linear Regression Analysis Associated with MCHC in Patients with Pneumoconiosis
The Logistic Regression Analysis Associated with Advanced Pneumoconiosis in Patients with Pneumoconiosis
We performed logistic regression analysis to identify the independently association with advanced pneumoconiosis (), when potential confounding factors associated with disease stage including gender, age, body mass index, smoking history and pulmonary tuberculosis history were considered as adjusted variables in logistic regression analysis, the results showed that MCHC was the only variable independently associated with advanced pneumoconiosis (OR: 0.936, CI95%: 0.877–0.999, p = 0.046).
Table 4 The Logistic Regression Analysis Associated with Advanced Pneumoconiosis Patients
The Receiver Operating Characteristic Curve Analysis of MCHC in Patients with Pneumoconiosis
To analyze the ability of MCHC to determine advanced pneumoconiosis in patients with pneumoconiosis, the receiver operating characteristic curve analysis was used, as shown in . We found that the area under the curve of MCHC was 0.694 (CI95%: 0.550–0.839, p = 0.018) to determine advanced pneumoconiosis, we also examined the optimal cutoff value of MCHC in identifying advanced pneumoconiosis, the optimal cutoff value of MCHC was 330 g/L with sensitivity 66.7% and specificity 74.2%.
Discussion
Our study examined the role of MCHC in patients with pneumoconiosis, the independent association between MCHC and advanced pneumoconiosis was found in patients with pneumoconiosis. Multiple mechanisms may underlie the association in patients with pneumoconiosis, thereinto, one possible mechanism is involved in the anemia of inflammation in chronic inflammatory disease. Inflammatory cytokines play the critical role in the pathogenesis of pneumoconiosis, serum tumor necrosis factor-α (TNF-α) and interleukin-8 (IL-8) levels have been reported to be increased in patients with pneumoconiosis compared with controls,Citation13 the levels of TNF-α and interleukin-1 (IL-1) secretion by alveolar macrophages from patients with pneumoconiosis are higher than healthy controls,Citation14 a relationship between serum interleukin-6 (IL-6) and severity of pneumoconiosis has been suggested by Zhai et al.Citation15 It is well known that the erythropoietin resistance is an important mechanism for the anemia of inflammation,Citation16 and systemic inflammation has been shown to increase erythropoietin resistance.Citation17 In addition, chronic inflammation can alter erythropoiesis by inflammatory cytokines such as TNF-α and IL-1.Citation18 Thus, chronic inflammation may decrease MCHC by increased erythropoietin resistance in pneumoconiosis. Moreover, iron deficiency is prevalent in patients with chronic inflammatory disease,Citation19 pneumoconiosis is no exception, iron deficiency has long been confirmed in patients with pneumoconiosis, an early study has reported that serum iron is reduced in patients with pneumoconiosis, and it has a negative correlation with disease progress of pneumoconiosis,Citation20 not surprisingly, iron deficiency is an important factor to reduce MCHC, the relation between MCHC and iron deficiency has been demonstrated.Citation21 Therefore, we consider that iron deficiency may also contribute to the decreased MCHC in patients with pneumoconiosis.
Blood routine test is one of the admission examinations for patients with pneumoconiosis, MCHC is easily obtained from the blood routine test clinically, the blood routine test time may not be shorter than X-ray; however, frequent X-ray examination has radiological damage for follow-up of pneumoconiosis patients. We found that lower MCHC was associated with advanced pneumoconiosis, and we obtained an optimal cutoff value of MCHC 330 g/L to determine advanced pneumoconiosis by receiver operating characteristic curve analysis, that is, when MCHC is lower than the cutoff value, patients may have advanced pneumoconiosis. Thus, MCHC may be a useful monitoring marker for follow-up of pneumoconiosis patients, which is beneficial to the clinical management of pneumoconiosis patients. However, the sensitivity and specificity of MCHC for the identification of patients with advanced pneumoconiosis are relatively low in receiver operating characteristic curve analysis. There are two possible main reasons. First, the small sample size may be a main factor. Second, iron deficiency is an important factor to reduce the MCHC,Citation21 while the potential confounding factors associated with iron metabolism may affect iron levels in patients with pneumoconiosis, which may decrease the ability of MCHC to determine advanced pneumoconiosis in receiver operating characteristic curve analysis.
It has been reported that hemoglobin and hematocrit are significantly decreased in workers with dust cement exposure,Citation22 and significantly higher hemoglobin and hematocrit have been observed patients with silicosis than patients without silicosis.Citation8 However, the hemoglobin levels have no significant differences in patients with different stages.Citation23 In our study, there were no significant differences in hemoglobin and hematocrit between I/II stage pneumoconiosis and III stage pneumoconiosis. We consider that these discrepant results may be attributed to different occupational exposure factors and time in patients with pneumoconiosis.
The present study has some limitations. First, a relatively small sample size is among the limitation of this study, additional studies with large samples are needed in the future. Second, our study did not examine the levels of iron, ferritin and erythropoietin resistance in patients with pneumoconiosis, so, the possible mechanism that directly leads to reduction in MCHC was not elucidated in patients with pneumoconiosis. Third, iron is an important factor to promote hemoglobin production, our study did not assess the effects of additional factors that may influence iron metabolism such as medication use, diet and individual differences of iron absorption on iron levels in patients with pneumoconiosis.
Conclusions
The decreased MCHC has an association with advanced pneumoconiosis in patients with pneumoconiosis, and MCHC may be a useful monitoring marker for follow-up of pneumoconiosis patients, which is beneficial to the clinical management of pneumoconiosis patients.
Ethics Approval Statement
The study was approved by the Ethics Committee of The Affiliated Hospital of Youjiang Medical University for Nationalities, and conformed to the Declaration of Helsinki. Informed consent of patients was exempted due to the retrospective design of the study, and patient data confidentiality was rigorously protected in this study.
Disclosure
The authors have no conflicts of interest to declare.
Additional information
Funding
References
- Qi XM, Luo Y, Song MY, et al. Pneumoconiosis: current status and future prospects. Chin Med J. 2021;134(8):898–907.
- Cascio MJ, DeLoughery TG. Anemia: evaluation and diagnostic tests. Med Clin North Am. 2017;101(2):263–284. doi:10.1016/j.mcna.2016.09.003
- Lee JM, Nadimpalli SB, Yoon JH, Mun SY, Suh I, Kim HC. Association between mean corpuscular hemoglobin concentration and future depressive symptoms in women. Tohoku J Exp Med. 2017;241(3):209–217. doi:10.1620/tjem.241.209
- Sheng X, Chen W, Xu Y, Lin F, Cao H. Higher mean corpuscular hemoglobin concentration is associated with worse prognosis of hepatorenal syndrome: a multicenter retrospective study. Am J Med Sci. 2022;363(1):25–32. doi:10.1016/j.amjms.2021.06.026
- Huang YL, Hu ZD. Lower mean corpuscular hemoglobin concentration is associated with poorer outcomes in intensive care unit admitted patients with acute myocardial infarction. Ann Transl Med. 2016;4(10):190. doi:10.21037/atm.2016.03.42
- Ruan Z, Li D, Hu Y, Qiu Z, Chen X. The association between mean corpuscular hemoglobin concentration and prognosis in patients with acute pulmonary embolism: a retrospective cohort study. Clin Appl Thromb Hemost. 2022;28:10760296221103867. doi:10.1177/10760296221103867
- Qu X, Zhang T, Ma H, Sui P, Du J. Lower mean corpuscular hemoglobin concentration is associated with unfavorable prognosis of resected lung cancer. Future Oncol. 2014;10(14):2149–2159. doi:10.2217/fon.14.121
- Milovanović APS, Milovanović A, Srebro D, Pajic J, Stanković S, Petrović T. Serum concentration of prostaglandin E2 as a diagnostic biomarker in patients with silicosis: a case-control study. J Occup Environ Med. 2023;65(7):546–552.
- National Health and Family Planning Commission of the People’s Republic of China. Diagnosis of occupational pneumoconiosis (GBZ 70-2015); 2015.
- Hodous TK, Chen RA, Kinsley KB, et al. A comparison of pneumoconiosis interpretation between Chinese and American readers and classifications. J Tongji Med Univ. 1991;11(4):225‐229. doi:10.1007/BF02888156
- International Labour Office. Guidelines for the Use of the ILO International Classification of Radiographs of Pneumoconioses. Revised ed. Geneva: International Labour Office; 2011.
- Ergun DD, Karis D, Alkan FA, Cakmak G, Yenigun M, Ercan M. Effects of cigarette smoking on hemorheologic parameters, plasma osmolality and lung function. Clin Hemorheol Microcirc. 2016;63(4):313–324. doi:10.3233/CH-152018
- Kim KA, Lim Y, Kim JH, et al. Potential biomarker of coal workers’ pneumoconiosis. Toxicol Lett. 1999;108(2–3):297–302. doi:10.1016/S0378-4274(99)00101-0
- Lassalle P, Gosset P, Aerts C, et al. Abnormal secretion of interleukin-1 and tumor necrosis factor alpha by alveolar macrophages in coal worker’s pneumoconiosis: comparison between simple pneumoconiosis and progressive massive fibrosis. Exp Lung Res. 1990;16(1):73–80. doi:10.3109/01902149009064700
- Zhai R, Liu G, Ge X, et al. Serum levels of tumor necrosis factor-alpha (TNF-alpha), interleukin 6 (IL-6), and their soluble receptors in coal workers’ pneumoconiosis. Respir Med. 2002;96(10):829–834. doi:10.1053/rmed.2002.1367
- Nairz M, Theurl I, Wolf D, Weiss G. Iron deficiency or anemia of inflammation?: differential diagnosis and mechanisms of anemia of inflammation. Wien Med Wochenschr. 2016;166(13–14):411–423. doi:10.1007/s10354-016-0505-7
- Bárány P. Inflammation, serum C-reactive protein, and erythropoietin resistance. Nephrol Dial Transplant. 2001;16(2):224–227. doi:10.1093/ndt/16.2.224
- Macdougall IC, Cooper AC. Erythropoietin resistance: the role of inflammation and pro-inflammatory cytokines. Nephrol Dial Transplant. 2002;17(Suppl 11):39–43. doi:10.1093/ndt/17.suppl_11.39
- Cacoub P, Choukroun G, Cohen-Solal A, et al. Iron deficiency screening is a key issue in chronic inflammatory diseases: a call to action. J Intern Med. 2022;292(4):542–556.
- Niculescu T, Dumitru R, Burnea D. Changes of copper, iron, and zinc in the serum of patients with silicosis, silicotuberculosis, and active lung tuberculosis. Environ Res. 1981;25(2):260–268. doi:10.1016/0013-9351(81)90027-X
- Cai J, Wu M, Ren J, et al. Evaluation of the efficiency of the reticulocyte hemoglobin content on diagnosis for iron deficiency anemia in Chinese adults. Nutrients. 2017;9(5):450. doi:10.3390/nu9050450
- Mojiminiyi FB, Merenu IA, Ibrahim MT, Njoku CH. The effect of cement dust exposure on haematological and liver function parameters of cement factory workers in Sokoto, Nigeria. Niger J Physiol Sci. 2008;23(1–2):111–114. doi:10.4314/njps.v23i1-2.54945
- Uygur F, Ornek T, Tanriverdi H, et al. Platelet indices in patients with coal workers’ pneumoconiosis. Lung. 2016;194(4):675–679. doi:10.1007/s00408-016-9883-2