Abstract
Background
The systemic inflammatory response index (SIRI) had been identified as an inflammatory marker and has been linked to determining clinical outcomes in several diseases. We advocated the relationship between the initial SIRI and the prognosis of diabetic maintenance hemodialysis (MHD) patients.
Methods
A total of 153 diabetic MHD patients who accepted regular HD treatment at our hospital were enrolled in this study. SIRI was calculated as neutrophil × monocyte/lymphocyte. All patients were separated into two groups based on the levels of SIRI. LASSO regression and Cox regression analyses were then made to determine the prognostic value of SIRI for diabetic MHD patients.
Results
During a median 33-month follow-up period, 50 (32.7%) patients died. The higher SIRI value (≥ 2.5) had a higher risk of death (adjusted HR=4.00, 95% CI 1.77–9.07, P=0.001) after adjusting for other confounding clinical features. The devised nomogram ground on SIRI value and clinical features had great predictive value for overall survival in diabetic MHD patients. The nomogram proved both prominent calibration competence and therapeutic subservience.
Conclusion
SIRI is a relatively excellent predictor for OS, and the suggested nomogram ground on SIRI leads to an accurate prediction value for diabetic MHD patients.
Introduction
As one of the most common and serious microvascular complications of diabetes, diabetes kidney disease (DKD) has become the central cause of end-stage kidney disease (ESKD), thus the need for renal replacement therapy (RRT) has increased rapidly in the past decades.Citation1,Citation2 Despite the great improvement in the knowledge and facilities, maintenance hemodialysis (MHD) patients, especially patients with diabetes, continue to be associated with a high rate of poor clinical outcomes as well as expensive medical healthcare costs.Citation3,Citation4 Therefore, doctors must prioritize identifying patients at high risk of death for diabetic MHD patients applying biomarkers or prediction algorithms to manage these patients effectively and improve the prognosis of them.
Inflammation plays an important role in the onset, development, and prognosis of patients with kidney disease, and thus, several inflammation-based markers have been set up for the diagnosis and prognosis of these patients.Citation5–8 Nevertheless, previous studies have also demonstrated that the systemic inflammatory response index (SIRI), which was calculated as neutrophil × monocyte / lymphocyte count, might reflect the inflammation status, and have predictive value for the diagnosis and prognosis of different diseases.Citation9–12 Moreover, A recent study showed that SIRI was a promising biomarker of mortality for PD patients.Citation13 However, the association between SIRI and the prognosis of diabetic MHD patients were not been investigated. Therefore, the aim of this study was to discuss the connection between initial SIRI and the prognosis of diabetic MHD patients. We then constructed a nomogram merging SIRI and other clinical features to investigate the prognosis of diabetic MHD patients.
Materials and Methods
Selection of Participants
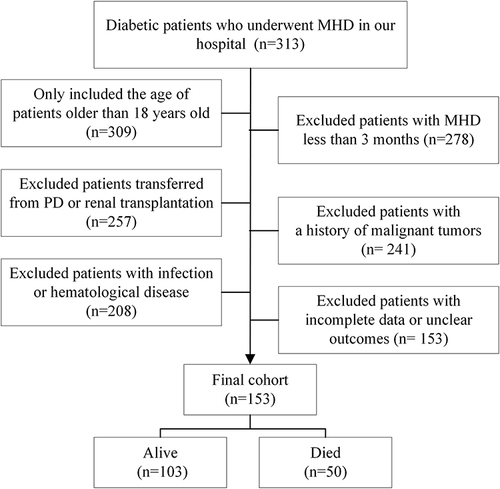
All patients in this retrospective study were collected from the first People’s Hospital of jiangxia district of Wuhan City between January 1, 2014, to December 1, 2019. We included patients who were aged 18 or older at the time of HD therapy and underwent MHD for greater than 3 months, and clinically or pathologically diagnosed DKD patients who had a clear outcome during the follow-up (continue MHD, transfer to peritoneal dialysis or renal transplantation, died). The exclusion criteria included: incomplete data or unclear medical history, transferred from peritoneal dialysis or a history of renal transplantation; patients with acute or chronic infection, malignant tumors, and hematological diseases.
This study was conducted according to the Declaration of Helsinki and the Ethics Committee of the first People’s Hospital of jiangxia district of Wuhan City agrees to this study (No. 2021024) and the informed consent was waived considering the confidentiality of patients’ information.
Finally, a total of 153 patients were included in this study, including 85 males (55.6%) and 68 females (44.4%), with an average age of 64.3 ±10.7 (34–89) years old ().
Data Collection
All variables were collected in the first 3 months of MHD treatment in our hospital. Demographic data included age, sex, body mass index (BMI), complications (hypertension, cardiovascular disease, cerebrovascular disease), marital status, education status, vascular access, and the duration of diabetes. All baseline laboratory data including complete blood count were obtained from nonfasting predialysis patients on a midweek day and analyzed using a standardized process.
SIRI was calculated as neutrophil × monocyte / lymphocyte. The estimated glomerular filtration rate (eGFR) was computed by the latest creatinine measurements formerly dialysis according to the CKD-EPI formula.Citation14 Cardiovascular disease (CVD) was considered as one of the following: coronary heart disease, congestive heart failure, cerebrovascular infarcts or hemorrhage, peripheral vascular disease, and sudden cardiac death.Citation15 Cerebrovascular disease was considered as one of the following: hemorrhagic or ischemic stroke, transient ischemic attacks, subarachnoid hemorrhage, and intracranial aneurysm.
Outcomes
All patients in this study were followed up via clinic visits or telephone interviews. The primary end-out point was the overall survival (OS). All patients were followed up until death or December 31, 2022.
Statistical Analysis
All analysis was conducted by R (version 4.1.0) software. The X-tile software was utilized to assure the optimal cutoff value of SIRI. And the least absolute shrinkage and selection operator (LASSO) regression was used for the selection of significant factors for OS in diabetic MHD patients. Multivariable Cox analysis was then used to construct a nomogram for the prognosis of diabetic MHD patients. The predictive performance of the predictive nomogram for OS was assessed using the area under the receiver operating characteristic curves (AUC), and calibration plots as well as decision curve analysis (DCA). A value of P < 0.05 was considered significant.
Results
Characteristics of All Patients
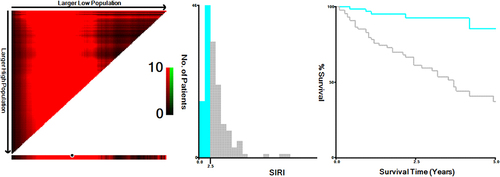
Finally, 153 patients were included in this study altogether, including 85 males (55.6%) and 68 females (44.4%), with an average age of 64.3 ± 10.7 (34–89) years old. All patients fell into two groups by the SIRI value (2.5) according to the X-tile (). The baseline information was given in .
Table 1 The Baseline Characteristics of All Patients
Figure 2 X-tile analyses of SIRI to obtain the optimal cutoff value of SIRI. X-tile plots for patients with diabetic MHD are shown on the left panels; the black circles indicate the optimal cutoff values, which are also presented in histograms (middle panels). Kaplan-Meier curves are shown in the right panels.
The Association Between SIRI and OS for Patients with MHD
Each patient’s SIRI measurement was displayed in . Based on the cut-off value (2.5), patients were split into a high-risk group and a low-risk group (). The AUC of SIRI for OS was 0.782 (95% CI 0.725–0.854, ). DCA demonstrated that SIRI was clinically helpful (). The high-SIRI group had a worse prognosis for patients with MHD than the lower-SIRI group (, P<0.0001).
Figure 3 The waterfall plots and forest plots of the high-SIRI group and low-SIRI group for the prognosis of diabetic MHD patients. The waterfall plot of SIRI for each patient of mortality (A) and the subgroup analysis of the SIRI for the prognosis of individuals with diabetic MHD patients (B).
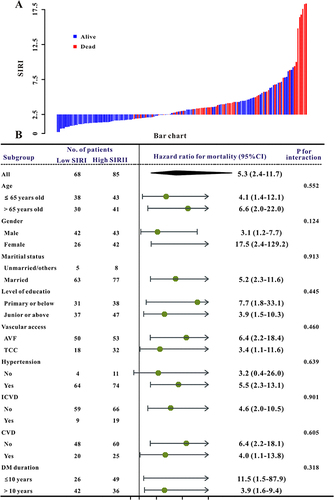
Figure 4 The SIRI was established to detect the overall mortality of patients with diabetic MHD. All patients were distinguished into high and low risk based on the SIRI (A), the relationship between survival time and prognosis of patients in the two corresponding groups (B), and the heatmap of other markers between the two groups (C). Receiver operating characteristic (ROC) curve analysis of the SIRI for overall mortality (D), Decision curve analysis of the risk score for the overall mortality (E). Kaplan-Meier curves show the overall mortality of groups with different risks (F).
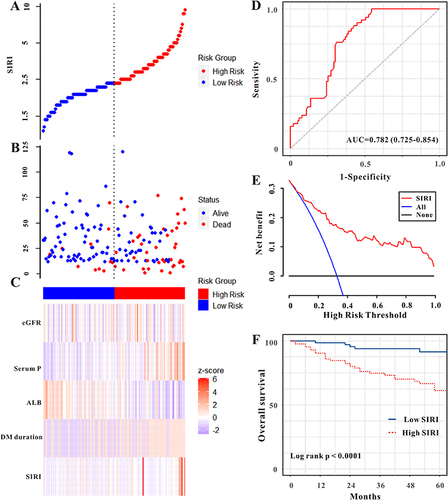
During a median 33-month follow-up period, 50 (32.7%) patients died, the high-SIRI patients had a higher risk of mortality even after adjusting for other variables (). And patients with SIRI < 2.5 had a lower risk of mortality than those with SIRI ≥ 2.5 group in almost all subgroups ().
Table 2 Univariate and Multivariate Cox Regression Analysis for All-Cause Mortality
Development and Verification of the Predictive Nomogram
LASSO regression for OS demonstrated that seven risk factors were finally included in this study ( and ). Moreover, multivariable Cox analysis was then used to build a nomogram for OS in diabetic MHD patients. As shown in , DM duration, eGFR, serum albumin, serum phosphate, and SIRI were finally included in this nomogram ().
Figure 5 Selection of significant factors associated with OS in diabetic MHD patients by LASSO Cox regression model. (A) The selection process of the optimum value of the parameter λ in the Lasso regression model by cross-validation method; (B) the variation characteristics of the coefficient of variables.
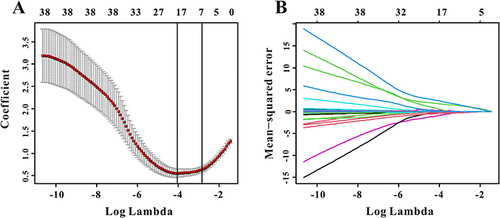
Figure 6 The established nomogram for OS in patients with diabetic MHD (A), the 1-year, 3-year, and 5-year calibration curves of the nomogram for OS (B), decision curve analysis of the nomogram for OS (C), and the time-dependent ROC curves for the 1-year, 3-year, and 5-year OS in patients with diabetic MHD (D).
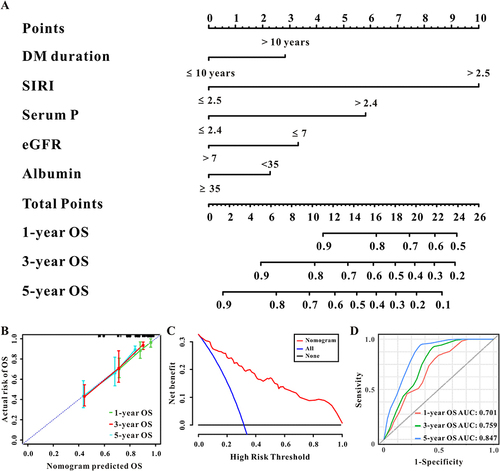
Furthermore, the 1-, 3-, and 5-year AUC of the predictive nomogram for OS was 0.701 (95% CI 0.613–0.809), 0.759 (95% CI 0.678–0.841), and 0.847 (95% CI 0.768–0.906), respectively (). The calibration curves also demonstrated a great agreement between predicted OS and actual OS (). Furthermore, DCA demonstrated that the predictive nomogram was helpful for decision-making ().
Discussion
In this study, we found a robust association between SIRI and prognosis for diabetic MHD patients. And the predictive nomogram based on SIRI and other clinical features exhibited great calibration, discrimination, and clinically useful. Thus, SIRI was a reliable prognostic marker for diabetic MHD patients, and the suggested nomogram based on SIRI leads to an accurate prediction for diabetic MHD patients.
DM is currently the leading cause of ESKD in many countries as well as in China, and the ones with DM are known to have the worst clinical outcomes in patients with MHD. The reason for this phenomenon is partly at least for the underlying metabolic disturbances, such as oxidative stress and inflammation, and so on. Yen et al retrospectively collected 212 diabetic MHD patients and found that the 1.5-year OS rate was 85.7%.Citation16 Recently, an observational study that included 263 diabetic MHD patients demonstrated that the 1-, and 5-year OS rates were 90.9%, and 53.9%, respectively.Citation17 Similar to these studies, in this study, we included patients in our hospital and found that the 1-, and 5-year OS rates for diabetic MHD patients were 86.9%, and 67.3%, respectively. Therefore, a reliable and novel predictor or model for the prognosis of diabetic MHD patients for the clinicians to risk stratification and then timely and effective therapies might be taken to improve the prognosis of these patients and lead to lower healthcare costs.
SIRI is one of the most effective inflammatory markers based on the complete blood count and the association between SIRI and clinical outcomes had been found in previous studies with different diseases. Using the data from the MIMIC-III database, Zhang et al calculated the levels of different inflammatory indicators and concluded that SIRI was a good marker for stroke patients.Citation11 Similar results had also been demonstrated in patients with acute ischemic stroke and laryngeal squamous cell carcinoma.Citation10,Citation18 As for renal diseases, SIRI could also have prognostic value for patients with renal cell carcinoma in previous studies.Citation9,Citation19 Moreover, a recent study also found that SIRI could serve as a novel and efficient indicator for the early diagnosis of catheter-related bloodstream infection in patients undergoing MHD.Citation20 However, as far as we know, this is the first study to explore the association between initial SIRI and prognosis of diabetic MHD patients and we demonstrated that SIRI could be a great marker for OS of them.
As we all know that inflammation plays an important role in the onset, development, and prognosis of patients with CKD or ESKD.Citation8 White blood cells and subtypes are the most common and easy-to-use methods for clinicians to determine the inflammation status of patients. Thus, several white blood cells-based indicators had been introduced to play a vital role in the diagnosis and prognosis of kidney disease.Citation6,Citation21,Citation22 Moreover, A high SIRI represents a high neutrophil and monocyte and a low lymphocyte content. In previous studies, increased neutrophil and monocyte or decreased lymphocyte counts have been demonstrated to be good predictors for the prognosis of patients with kidney disease. A recent study enrolled 646 peritoneal dialysis patients and demonstrated that after a median 31-month follow-up period, and higher SIRI (1.28) level was significantly associated with increased all-cause mortality and CVD mortality.Citation13 Similar results had also been found in another study with 369 incident PD patients and they concluded that SIRI was independent indicator for all-cause mortality in PD patients and could provide comparable predictive value and assist clinicians to ameliorate PD management.Citation23 Alike with this, in the current study, we collected 153 diabetic MHD patients and concluded that a higher SIRI (2.5) level was significantly associated with elevated all-cause mortality. However, the exact mechanism of the SIRI that affects all-cause mortality in diabetes MHD patients is unclear. We believe that except for inflammation, these might at least also explain by malnutrition. A significant negative correlation between SIRI and nutritive indexes (serum albumin, triglyceride, and total cholesterol) was found in this study and it is well-acknowledged that malnutrition had prognostic values for patients with ESKD.Citation24,Citation25
Given that the readily accessible for the nomogram, which may be more easy-to-use for physicians to decide the diagnosis or the prognosis of a specific patient, we developed a predictive nomogram that combines the SIRI value and other clinical factors selected by LASSO regression to make the prediction accurate, and then, doctors could early identify diabetic MHD patients at high risk of death along with a timely and effective clinical intervention to improve the prognosis of these patients. And unsurprisingly, in the present investigation, our predictive nomogram displayed high predictive value and was clinically useful for diabetic MHD patients.
However, there were also some limitations in this retrospective study. Firstly, this retrospective analysis was a single-center study with limited samples, which might have potential bias. Secondly, only the initial SIRI value at the first three months of HD therapy was included in this study and we did not analyze changes of them throughout their MHD therapy. Thirdly, there were some important inflammatory markers, such as interleukin, and tumor necrosis factor were missed in this study. Finally, the predictive nomogram did not validate in independent cohorts, and further prospective multicenter studies are needed to corroborate our findings.
Conclusions
In the present study, we first concluded that the initial SIRI, which is simple access and cost-effective parameter, could act as a credible predictor for diabetic MHD patients. Moreover, the suggested nomogram based on the SIRI serves as an effective means for recognizing patients at high risk of death for diabetic MHD patients and could offer a therapeutic cue for patients suffering from particularly inflamed DKD.
Disclosure
The authors declared that there is no conflict of interest.
Additional information
Funding
References
- Selby NM, Taal MW. An updated overview of diabetic nephropathy: diagnosis, prognosis, treatment goals and latest guidelines. Diabetes Obes Metab. 2020;22(Suppl 1):3–15. doi:10.1111/dom.14007
- Ma R. Epidemiology of diabetes and diabetic complications in China. Diabetologia. 2018;61:1249–1260. doi:10.1007/s00125-018-4557-7
- Sadeghi M, Behdad S, Shahsanaei F. Infective endocarditis and its short and long-term prognosis in hemodialysis patients: a systematic review and meta-analysis. Curr Probl Cardiol. 2021;46:100680. doi:10.1016/j.cpcardiol.2020.100680
- Yarragudi R, Gessl A, Vychytil A. New-onset diabetes mellitus in peritoneal dialysis and hemodialysis patients: frequency, risk factors, and prognosis-a review. Ther Apher Dial. 2019;23:497–506. doi:10.1111/1744-9987.12800
- Muto R, Kato S, Lindholm B, et al. Increased monocyte/lymphocyte ratio as risk marker for cardiovascular events and infectious disease hospitalization in dialysis patients. Blood Purif. 2022;51:747–755. doi:10.1159/000519289
- Oguz EG, Yeter HH, Akcay OF, et al. Predictive value of neutrophil-to-lymphocyte ratio in terms of need for intensive care unit and mortality in maintenance hemodialysis patients with COVID-19. Hemodial Int. 2022;26:377–385. doi:10.1111/hdi.13001
- Lu H, Wu H, Yang Y, et al. Relationship between chronic periodontitis and inflammatory cytokines in patients undergoing maintenance hemodialysis. Clin Oral Investig. 2022;26:6699–6709. doi:10.1007/s00784-022-04629-0
- Mihai S, Codrici E, Popescu ID, et al. Inflammation-related mechanisms in chronic kidney disease prediction, progression, and outcome. J Immunol Res. 2018;2018:2180373. doi:10.1155/2018/2180373
- Lv Z, Feng HY, Wang T, Ma X, Zhang X. Preoperative systemic inflammation response index indicates poor prognosis in patients treated with resection of renal cell carcinoma with inferior vena cava tumor thrombus. Urol Oncol. 2022;40:167–169. doi:10.1016/j.urolonc.2021.11.030
- Wang T, Zhang D, Tang D, Heng Y, Lu LM, Tao L. The role of systemic inflammatory response index (SIRI) and tumor-infiltrating lymphocytes (TILs) in the prognosis of patients with laryngeal squamous cell carcinoma. J Cancer Res Clin Oncol. 2022;2022:1.
- Zhang Y, Xing Z, Zhou K, Jiang S. The predictive role of Systemic Inflammation Response Index (SIRI) in the prognosis of stroke patients. Clin Interv Aging. 2021;16:1997–2007. doi:10.2147/CIA.S339221
- Gu L, Ma X, Wang L, et al. Prognostic value of a systemic inflammatory response index in metastatic renal cell carcinoma and construction of a predictive model. Oncotarget. 2017;8:52094–52103. doi:10.18632/oncotarget.10626
- Li J, Li Y, Zou Y, et al. Use of the systemic inflammation response index (SIRI) as a novel prognostic marker for patients on peritoneal dialysis. Ren Fail. 2022;44:1227–1235. doi:10.1080/0886022X.2022.2100262
- Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi:10.7326/0003-4819-150-9-200905050-00006
- Herzog CA, Asinger RW, Berger AK, et al. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int. 2011;80:572–586. doi:10.1038/ki.2011.223
- Yen TH, Lin JL, Lin-Tan DT, Hsu CW, Chen KH, Hsu HH. Blood cadmium level’s association with 18-month mortality in diabetic patients with maintenance haemodialysis. Nephrol Dial Transplant. 2011;26:998–1005. doi:10.1093/ndt/gfq448
- Chen Y, Wang Y, Shen Y, et al. A dynamic nomogram for predicting survival among diabetic patients on maintenance hemodialysis. Ther Apher Dial. 2023;27:39–49. doi:10.1111/1744-9987.13901
- Ma X, Yang J, Wang X, Wang X, Chai S. The clinical value of systemic inflammatory response index and inflammatory prognosis index in predicting 3-month outcome in acute ischemic stroke patients with intravenous thrombolysis. Int J Gen Med. 2022;15:7907–7918. doi:10.2147/IJGM.S384706
- Mao W, Sun S, He T, et al. Systemic inflammation response index is an independent prognostic indicator for patients with renal cell carcinoma undergoing laparoscopic nephrectomy: a multi-institutional cohort study. Cancer Manag Res. 2021;13:6437–6450. doi:10.2147/CMAR.S328213
- Yang J, Wang H, Hua Q, Wu J, Wang Y. Diagnostic value of systemic inflammatory response index for catheter-related bloodstream infection in patients undergoing haemodialysis. J Immunol Res. 2022;2022:7453354. doi:10.1155/2022/7453354
- Cao W, Ren H, Song B, Liao Z, Li H. Red cell distribution width and Glasgow coma scale score as predictors of in-hospital mortality in maintenance hemodialysis patients diagnosed with spontaneous intracerebral hemorrhage. Medicine. 2022;101:e31094. doi:10.1097/MD.0000000000031094
- Zhan X, Pan D, Wei X, Wen D, Yan C, Xiao J. Monocyte to high-density lipoprotein ratio and cardiovascular events in patients on peritoneal dialysis. Nutr Metab Cardiovasc Dis. 2020;30:1130–1136. doi:10.1016/j.numecd.2020.03.011
- Yang Y, Xu Y, Liu S, Lu P, Zhou H, Yang M. The systemic inflammation indexes predict all-cause mortality in peritoneal dialysis patients. Ren Fail. 2023;45:2160348. doi:10.1080/0886022X.2022.2160348
- Maraj M, Kusnierz-Cabala B, Dumnicka P, et al. Malnutrition, Inflammation, Atherosclerosis Syndrome (MIA) and diet recommendations among end-stage renal disease patients treated with maintenance hemodialysis. Nutrients. 2018;10:69. doi:10.3390/nu10010069
- Zhang J, Xiao X, Wu Y, et al. Prognostic nutritional index as a predictor of diabetic nephropathy progression. Nutrients. 2022;14:1.