Abstract
Background
The purpose of this study was to determine the prevalence of hypertension in two rural communities of Osun State, Nigeria.
Methods
A consenting adult population of the Alajue and Obokun rural communities in southwestern Nigeria that presented for the screening exercise participated in this community-based cross-sectional descriptive study. Two hundred and fifty-nine respondents aged older than 18 years completed a standardized, pretested, structured questionnaire as part of activities celebrating World Kidney Day and World Glaucoma Day in 2011. Anthropometric data and blood pressure were recorded, and the data were analyzed using the Statistical Package for Social Sciences version 17.
Results
The mean age of the respondents was 49.7 ± 1.6 years, 100 (38.6%) were males, 84 (32.4%) were farmers, and 111 (42.9%) were traders. The prevalence of hypertension was 13.16% (present in 34 respondents). Seventeen (6.6%) had isolated systolic hypertension, while 11 (4.2%) had isolated diastolic hypertension. Two hundred and thirty-six (91.1%) undertook daily exercise lasting at least 30 minutes and 48 (18.5%) had ever taken antihypertensive drugs on a regular basis. Four respondents (1.6%) claimed a family history of hypertension. The average body mass index (BMI) among respondents was 23.4 ± 4.9 kg/m2, 51 (19.6%) had a BMI of 25.0–29.9, and 30 (11.5%) had a BMI ≥ 30. A significant association existed between age older than 40 years and having hypertension (P < 0.05), while no relationship existed between age and BMI or between gender and hypertension (P > 0.05). Rates of older age and high BMI were significantly higher among hypertensives than among normotensives. Respondents with BMI ≥ 25 had at least a three times greater likelihood of developing hypertension than those with BMI < 25 (odds ratio 2.9, 95% confidence interval 0.007–0.056, P = 0.011).
Conclusion
The prevalence of hypertension is high in this study population and we recommend scaling up primary prevention efforts to reduce this in Nigerian communities.
Introduction
Like many other noncommunicable diseases, hypertension is gradually assuming epidemic dimensions with the dawn of epidemiological transition. It is the most common cardiovascular disorder, affecting approximately one billion people globally and causing approximately 7.1 million deaths annually.Citation1 Hypertension is the most common cardiovascular disease in Africans,Citation2 and congestive cardiac failure is its commonest complication.Citation3 Other complications include stroke, renal failure, atherosclerotic cardiovascular disease, and death.Citation4 According to the World Health Organization, cardiovascular diseases are the leading cause of mortality and morbidity in developed countries and are emerging as a prominent public health problem in developing countries.Citation5 In Nigeria, common cardiovascular diseases reported with a high incidence include heart failure, hypertension, and congenital heart disease, with hypertension being the commonest.Citation6
The Nigerian National Noncommunicable Disease Survey in 1997 reported an adult hypertension prevalence of 11.4%, with a variation of 14.8% and 9.8% in urban and rural areas, respectively.Citation7 The cutoff value of a blood pressure (BP) 160/95 mmHg for hypertension was used, so giving an underestimation of the prevalence of hypertension. This would have been higher if the new cutoff value of 140/90 mmHg was used. The prevalence of hypertension in both rural and urban communities in Nigeria is increasing. Various community surveys in Nigeria have shown an adult prevalence of 15%–36.6%.Citation8–Citation11 Oladapo et al recently reported a prevalence of 20.8% in the rural community of Egbeda, southwest Nigeria.Citation12 The prevalence in semiurban Ile-Ife was 36.6%, while that in Ipetumodu, Osun State, Nigeria, was 26.4% for mild hypertension (BP ≥ 140/90 mmHg) and 11.8% for moderate hypertension (BP ≥ 160/100 mmHg).Citation12
The overall prevalence of hypertension ranges from 14.5% in Nigeria, 16.9% in Cameroon, 28.7% in Accra,Citation13 to 32.6% for blacks in the United States.Citation14 Cross-migration from rural to urban areas and vice versa, the asymptomatic nature of the disease, changing lifestyles, and the environment are contributing to the rising problem of hypertension. Hypertension has been associated with various factors, including age, gender, family history, alcohol consumption, smoking, obesity, level of education, and occupation.Citation15
Hypertension is a silent killer and most patients are detected to have it incidentally when they are admitted to hospital for unrelated disease or subjected to pre-employment or preoperative medical checkups. Many patients are also diagnosed when they seek medical advice because of target organ damage. Target organ damage and associated clinical conditions are very common in newly diagnosed hypertensive patients in Nigeria, with a recently reported prevalence of 66.7%.Citation16 However, the majority of the rural population in Nigeria is marginalized and has inadequate access to health care and quality education.Citation17 A significant number of rural dwellers seek consultations with indigenous and private health care practitioners, where regular screening for hypertension is not practiced. Clinic-based (opportunistic) screening of hypertension may not detect a large proportion of adults with hypertension. Community-based screening can improve the detection and treatment of hypertension. Few studies have demonstrated the occurrence of hypertension and its predisposing risk factors in rural areas of Nigeria. The objective of this study was to determine the prevalence of hypertension in two selected rural communities in southwestern Nigeria.
Materials and methods
This was a community-based, descriptive, cross-sectional study carried out in two rural communities in Osun state in southwestern Nigeria. The two rural communities were Alajue and Ibokun, with a total population of 5000 people. The majority of the dwellers there are farmers and many are traders. Factors predisposing to a western lifestyle appeared minimal in these communities, although they have roads making the communities accessible to town and cities. All members of the communities aged 18 years and older constituted the target population.
This study was carried out as a part of a community-based screening program to raise awareness of the 2011 World Kidney Day celebrations. Entry commenced with holding a series of meetings with kings, traditional chiefs, politicians, heads of households, and other gatekeepers in the community. The rationale for the screening exercise was communicated to community members at these meetings. Community town hall meetings were organized for each of the communities to mobilize and sensitize community members further. At these meetings, community members eligible for screening were encouraged to come out en masse, with the assurance that all those who came out and consented to the exercise would be screened. The two communities were mobilized and sensitized regarding the importance of screening for noncommunicable diseases, in particular, hypertension and diabetes. All consenting adults who participated in the screening exercise had their BP recorded, in addition to anthropometric measurements. An interviewer administered a pretested questionnaire to collect basic data pertaining to sociodemographic characteristics and risk factors for hypertension among the respondents.
Ethical approval to conduct the study was obtained from the ethical research committee of Osun State University College of Health Sciences. A limitation of this study was its inability to study complications associated with hypertension in these rural communities, although this was actually beyond the scope of the present study.
Training of survey team
To standardize survey measurements and procedures, ten research assistants were trained using specially prepared survey manuals that conformed to recommended noncommunicable disease survey protocols.Citation18 Before the main study, a field test was carried out to fine-tune instruments and procedures.
Operational definitions
Hypertension was defined as systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg, based on the guidelines of the International Society of Hypertension/World Health OrganizationCitation19 and the Seventh Joint National Committee on Hypertension,Citation20 or being on regular antihypertensive drugs. Overweight/obesity was defined as BMI ≥ 25 kg/m2 and ≥30 kg/m2, respectively. A standardized calibrated mercury column type sphygmomanometer, stethoscope, common weighing machine, and measuring tape were used for physical examination.
Measurements
Informed verbal consent was obtained before measuring BP. The subjects rested quietly for 10 minutes, and BP was measured in the sitting posture with an appropriate-sized cuff encircling the arm. With the left arm of the subject held at the level of the heart, the maximum inflation level was determined using a mercury sphygmomanometer, using a 15 cm stethoscope and a cuff of appropriate size (a cuff of larger width was used for large arms).
BP was measured to the nearest 2 mmHg on two occasions at an interval of one minute. BP measurements were made using the left arm of each study subject. Subjects were not permitted to smoke. In cases where the two readings differed by over 10 mmHg, a third reading was obtained, and the three measurements were averaged. The pressures at which sounds appeared and disappeared were taken as systolic BP and diastolic BP, respectively. BP was classified as normal, hypertensive, or isolated systolic or diastolic hypertension.
Body weight was measured (to the nearest 0.5 kg) with the subject standing motionless on the calibrated weighing scale, with feet about 15 cm apart and weight equally distributed on each leg. Subjects were instructed to wear minimum outerwear (as culturally appropriate) and no footwear while the weight was being measured. Height was measured (to the nearest 0.5 cm) using a calibrated tape and with the subject standing in an erect position against a vertical surface, and the head positioned so that the top of the external auditory meatus was level with the inferior margin of the bony orbit.
Calculations
BMI was calculated as weight in kilograms divided by height in meters squared. Based on their BMI, individuals were classified into four groups, ie, thin (BMI < 18.5), normal (BMI 18.5–24.9), overweight (BMI 25.0–29.9), or obese (BMI > 30.0), according to WHO classification.
Data management
The Statistical Package for Social Sciences (SPSS) software version 17 (SPSS Inc, Chicago, IL, USA) was used for data entry and analysis. Validity of data was ensured by double entry and random checks for errors and outlier values. Relevant frequency distribution tables and summary indices were generated. The Chi-square test was used to demonstrate relationships between categorical variables. Multivariate logistic regression analysis was done using systolic and diastolic BP as the dependent variable and risk factors identified to be significant in the bivariate analysis as independent variables. The level of significance was set at P values ≤ 0.05 for all inferential analysis of categorical variables.
Results
shows that the age group 50–69 years constitutes the highest proportion (n = 109, 42.0%) among respondents. The mean age of the respondents was 49.7 ± 1.6 years. One hundred (38.6%) were males, 111 (42.9%) were traders, and 84 (32.4%) were farmers by occupation. shows that the prevalence of hypertension was 13.16% (34 respondents). Seventeen (6.6%) had isolated systolic hypertension, 11 (4.2%) had isolated diastolic hypertension, and 189 (73.0%) were normotensive. Two hundred and thirty-six (91.1%) undertook daily exercises lasting at least 30 minutes. Forty-eight (18.5%) had ever taken antihypertensive drugs, mostly the centrally acting agent, alpha methyldopa, and the diuretic combination of amiloride and hydrochlorothiazide. Four (1.6%) claimed a family history of hypertension and 48 (18.5%) had ever taken antihypertensive drugs on a regular basis.
Table 1 Sociodemographic data of respondents
Table 2 Pattern of hypertension in rural communities
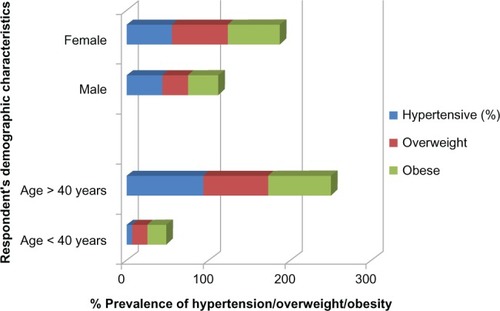
The prevalence of overweight and obesity in the study population was as follows: 51 respondents (19.6%) had a BMI of 25.0–29.9 while 30 (11.5%) had a BMI of ≥30. Mean BMI in the respondents was 23.4 ± 4.9. shows that more females (n = 19) were hypertensive as compared with males (n = 15). Similarly, more females were overweight or obese (n = 35 and n = 19, respectively) than males (n = 16 and n = 11). A significant association existed between age older than 40 years and having hypertension (P < 0.05), while no relationship existed between age and BMI or between gender and hypertension (P > 0.05). Respondents with BMI ≥ 25 had a three times greater likelihood of developing hypertension compared with those having a BMI < 25 (odds ratio 2.9, 95% confidence interval 0.007–0.056, P = 0.011). Older age and increased BMI were significantly more common in hypertensive respondents than in their normotensive counterparts.
Figure 1 Association between demographic characteristics and hypertension and BMI.
Abbreviation: BMI, body mass index.
Discussion
The mean age of the respondents was about 49 years. This compares well with another study showing a mean age of about 42 years in rural communities in Nigeria.Citation21 Just over 10% of the rural respondents we screened were hypertensive. This is consistent with the finding of a 10% prevalence in a typical community in rural India.Citation22 However, the prevalence in our study is lower than that reported by other studies from Nigeria (14.5%) and Cameroon (16.9%,Citation23 18.3%,Citation24 and 19.04%).Citation25 It is also much lower when compared with other studies reporting prevalences of 25.4%,Citation21 28.3%,Citation13 28.7%,Citation26 30.5%,Citation27 and 37.7%.Citation28 However, our figure is slightly higher than that from a study conducted in Sudan, which reported a prevalence of 7.5%.Citation29 In this study, about 6.6% had isolated systolic and 4.2% diastolic hypertension, which is similar to another study reporting isolated systolic hypertension in 10.5% and isolated diastolic hypertension in 9.0% of subjects.Citation30
A diverse pattern in the prevalence of hypertension can be said to exist in rural populations around the world. Typical rural populations, being marginalized and vulnerable communities in Nigeria, show a pattern of people migrating to urban areas or still living rurally but working in urban areas. In the process, some may be adopting the western lifestyle in the form of diet and physical activity related to urbanization and modernization, and western lifestyle has been identified as a risk factor for hypertension.Citation31 Like many other developing countries, disparity exists between rural and urban populations in terms of health facilities, education, and economic pursuits.Citation15 For the same reason, about 10% of our rural population had taken antihypertensive drugs, mostly methyldopa and a combination of amiloride and hydrochlorothiazide, and were not on newer antihypertensive drugs for reasons of affordability and accessibility. Further, the primary health care centers that serve this rural population only stock first-line antihypertensive drugs requiring minimal biochemical monitoring. This changing epidemiology may be affecting the pattern of hypertension found in Africa.
A BP survey of 20 rural Ghanaian villages in 1973 found a hypertension prevalence of 2%–5%, and concluded that hypertension was not a significant health problem in rural Ghanaians.Citation32 Thus, an increase in the prevalence of hypertension can be said to be occurring in rural populations undergoing modernization. This supports the fact that hypertension, which was considered to be nonexistent or extremely rare in most African societies, particularly in rural communities, is now emerging as a public health problem in sub-Saharan Africa,Citation32,Citation33 and its prevalence will increase even further unless broad and effective preventive measures are implemented.Citation34 There is a need for primary prevention efforts targeted to all communities, both rural and urban. Furthermore, the clinical significance of our findings is that, given that hypertension is now on the rise in rural areas of southwestern Nigeria, and probably related to the recent rise in occurrence of modifiable risk factors of hypertension occasioned by adoption of lifestyle changes in these rural populations, it is imperative that health policy-makers give priority to improved allocation of health resources to rural health facilities for effective management of hypertension.
In this study, hypertension was associated with advancing age. This supports a study in which hypertension has been found to be associated with older age,Citation29 and yet others finding an association in people older than 40 years.Citation25,Citation35–Citation38 It had been reported that the age-standardized prevalence of hypertension is significantly higher in urban than in rural areas for both men and women.Citation39 In this study, hypertension was associated with being overweight and obese, and corroborates similar studies showing that BMI is strongly and independently associated with systolic and diastolic BP.Citation40–Citation42 In fact, overweight and obesity are no longer rare in rural residents.Citation13,Citation43
Conclusion
The prevalence of hypertension is on the increase in rural areas, contrary to speculation, and is associated with certain sociodemographic factors and BMI. Hence, there is a need for primary prevention efforts targeted at modifiable risk factors on a large scale.
Acknowledgments
The authors wish to thank the kings and members of the communities where the data were collected. We also thank our research secretariat for their efforts, and the ethical review committee of Osun State University for granting approval for us to conduct this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- BrundtlandGHFrom the World Health Organization. Reducing risks to health, promoting healthy lifeJAMA2002288197412387638
- AkinkugbeOOWorld epidemiology of hypertension in blacksHallWDSaundersEShulmanNBHypertension in BlacksPhiladelphia, PAChicago Year Book Publishers1985
- AkinkugbeOOHigh Blood Pressure in the AfricanEdinburg, ScotlandChurchill Livingstone1972
- BlochMJBasileJNHypertension in the elderlyBlackHRElliotWJHypertension: A Companion to Braunwald’s Heart Disease1st edPhiladelphia, PASaunders2007
- World Health OrganizationThe World Health Report – Reducing Risks, Promoting Healthy LifestylesGeneva, SwitzerlandWorld Health Organization2002
- MukadasAOMisbauUIncidence and patterns of cardiovascular disease in north western NigeriaNiger Med J2009505557
- AkinkugbeOONational Expert Committee on Non-Communicable Diseases in NigeriaFinal Report of National SurveyLagos, NigeriaFederal Ministry of Health and Social Services1997
- AkinkugbeOOCurrent epidemiology of hypertension in NigeriaArch Ibad Med1999134
- AkinkugbeOONon-communicable disease, the next epidemic: Nigeria’s preparednessNig J Clin Pract200033742
- KadiriSTracking cardiovascular disease in AfricaBMJ200533171171216195264
- AdedoyinRAMbadaCEBalogunMOPrevalence and pattern of hypertension in a semiurban community in NigeriaEur J Cardiovasc Prev Rehabil20081568368719177626
- OladapoOOSalakoLSodiqOShoyinkaKAdedapoKFalaseAOA prevalence of cardiometabolic risk factors among a rural Yoruba South-Western Nigerian population: a population based surveyCardiovasc J Afr201021263120224842
- AmoahAGBHypertension in Ghana: a cross-sectional community prevalence study in Greater AccraEthn Dis20031331031512894954
- OlatunbosunSTKaufmanJSCooperRSBellaAFHypertension in a Black population: prevalence and biosocial determinants of high blood pressure in a group of urban NigeriansJ Hum Hypertens20001424925710805050
- KapoorSTyagiRSalujaKChaturvediAKapoorAKEmerging health threats among a primitive tribal group of Central IndiaJournal of Public Health and Epidemiology201021319
- AyodeleOEAlebiosuCOAkinwusiPOAkinsolaAMejuiniATarget organ damage and associated clinical conditions in newly diagnosed hypertensives attending a tertiary health facilityNiger J Clin Pract20071031932518293643
- DoleaCStormontLBraichetaJMEvaluated strategies to increase attraction and retention of health workers in remote and rural areasBull World Health Organ20108837938520461133
- World Health OrganizationPhysical status: The use and interpretation of anthropometryTechnical report series. Report No 854Geneva, SwitzerlandWorld Health Organization1995 Available from: http://www.who.int/childgrowth/publications/physical_status/en/index.htmlAccessed March 5, 2013
- World Health Organization Guidelines subcommittee1999 WHO/ISH guidelines for the management of hypertensionJ Hypertens19991715118310067786
- ChobanianAVBakrisGLBlackHRNational High Blood Pressure Education Programme Coordinating Committee: Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII)Hypertension2003421206125214656957
- AddoJAmoahGBKoramKAThe changing patterns of hypertension in Ghana: a study of four rural communities in the Ga districtEthn Dis20061689489917061743
- GuptaRTrends in hypertension epidemiology in IndiaJ Hum Hypertens200418737814730320
- CooperRRotimiCAtamanSThe prevalence of hypertension in seven populations of West African originAm J Public Health1997871601689103091
- YuvarajBYNagendra GowdaMRUmakanthaAGPrevalence, awareness, treatment, and control of hypertension in rural areas of DavanagereIndian J Community Med20103513814120606939
- KokiwarPRGuptaSSPrevalence of hypertension in a rural community of Central IndiaInt J Biol Med Res20112950953
- CappuccioFPMicahFBLynseyEPrevalence, detection, management, and control of hypertension in Ashanti, West AfricaHypertension2004431017102215037552
- WamalaJFKaryabakaboZNdungutseDGuwatuddeDPrevalence factors associated with Hypertension in Rukungiri District, Uganda – a community-based studyAfr Health Sci2009915316020589143
- EdwardsRUnwinNMugusiFHypertension prevalence and care in an urban and rural area of TanzaniaJ Hypertens20001814515210694181
- AddoJSmeethLLeonDAHypertension in sub-Saharan Africa: a systematic reviewHypertension2007501012101817954720
- SayeedMABanuAKhanAHussainMZPrevalence of diabetes and hypertension in a rural population of BangladeshDiabetes Care1995185555587497870
- WillJCCigarette smoking and diabetes mellitus: evidence of a positive association from a large prospective cohort studyInt J Epidemiol20013054054611416080
- PobeeJOLarbiEBBelcherDWWurapaFKDoduSRBlood pressure distribution in a rural Ghanaian populationTrans R Soc Trop Med Hyg1977716672860316
- van der SandeMAMilliganPJNyanOABlood pressure patterns and cardiovascular risk factors in rural and urban Gambian communitiesJ Hum Hypertens20001448949610962516
- MahmoodSESrivastavaAShrotriyaVPShaifaliIMishraPNational prevalence and epidemiological correlates of hypertension among labour populationJ Community Med201124348
- GhannemHFredjAHEpidemiological transition and cardiovascular risk factors in TunisiaRev Epidemiol Sante Publique199745286292 French9380909
- AmoahAGObesity in adult residents of Accra, GhanaEthn Dis2003132 Suppl 2S97S10113677422
- SteynKFourieJLombardCKatzenellenbogenJBourneLJoostePHypertension in the Black community of the Cape Peninsula South AfricaEast Afr Med J1996737587638997869
- WheltonPKEpidemiology of hypertensionLancet19943441011067912348
- MbanyaJCNMinkoulouEMSalahaJNBalkaubBThe prevalence of hypertension in rural and urban CameroonInt J Epidemiol1998271811859602396
- BovetPRossAGGervasoniJPMkambaMMtasiwaDMDistribution of blood pressure, body mass index and smoking habits in the urban population of Dar es Salaam, Tanzania, and associations with socioeconomic statusInt J Epidemiol20023124024711914327
- OnalAEErbilSOzelSAciksariKTumerdemYThe prevalence of and risk factors for hypertension in adults living in IstanbulBlood Press200413313615083638
- AgyemangCRural and urban differences in blood pressure and hypertension in Ghana, West AfricaPublic Health200612052553316684547
- AmoahAGSocio-demographic variations in obesity among Ghanaian adultsPublic Health Nutr2003675175714641945