Abstract
Purpose
To explore the computed tomography (CT) features of bronchopneumonia caused by pepper aspiration to improve the diagnosis.
Materials and Methods
28 adult patients diagnosed with obstructive pneumonia caused by pepper aspiration from January 2016 to September 2022 were enrolled. The CT characteristics of bronchial changes and pulmonary lesions caused by pepper were analyzed and summarized.
Results
Among 28 patients, the most common symptom was cough (26, 92.9%), followed by expectoration (23, 82.1%). Bronchoscopy revealed that peppers were mainly found in the bronchus of the right lower lobe (n = 18, 64.3%), followed by the bronchus of the left lower lobe (n = 5, 17.9%). In combination with bronchoscopy results, the pepper in the bronchus manifested as circular or V/U-shaped high-density, localized soft tissue, and flocculent opacification in 8 (28.6%), 16 (57.1%), and 3 (10.7%) cases on CT images, respectively. The bronchial wall around the pepper was thickened with localized occlusion (n = 19, 67.9%) and stenosis (n = 9, 32.1%). Regarding adjacent bronchi without peppers, extensive wall thickening with stenosis and/or occlusion was found in 23 (82.1%) cases. Distal pulmonary lesions frequently involved two or three segments (21, 75.0%) and mainly presented as patchy consolidation or atelectasis (24, 85.7%).
Conclusion
In combination to a history of eating peppers and clinical symptoms, bronchopneumonia caused by pepper should be highly suspected if U/V-shaped and annular high-density or localized soft tissue density is detected in the bronchi of the lower lobes, accompanied by extensive bronchial wall thickening, stenosis, or occlusion, and consolidation or atelectasis in multiple distal lung segments.
Introduction
Pneumonia is one of the most common acute respiratory infectious diseases and can involve the pulmonary interstitium, distal bronchial tree, and alveoli.Citation1 It includes infectious pneumonia (bacterial, viral, and fungal pneumonia), radiation pneumonitis, aspiration pneumonia, obstructive pneumonia, etc.Citation2–5 Obstructive pneumonia differs significantly from other common infectious pneumonia in terms of clinical manifestations, treatment, and prognosis.Citation6,Citation7 Owing to the presence of persistent obstruction, obstructive pneumonia is seldom completely absorbed, often leading to recurrence or refractory infections.Citation6
Obstructive pneumonia is typically caused by neoplasms or foreign bodies.Citation7–10 Foreign body obstruction is more diverse than obstruction caused by neoplasms. Food items, such as vegetable pieces, fruits, meat, and bones are the most common foreign objects.Citation8,Citation11,Citation12 Other objects included iatrogenic (endotracheal tube appliances, tracheostomy tube segments, endodontic needles, etc.) and miscellaneous (thumbtacks, rivets, pins, etc.) items.Citation13 Among them, a few foreign bodies such as coins, nails, and teeth are radiopaque, thus they appear hyperdense in computed tomography (CT) scan and can be easily detected and identified.Citation8,Citation14–16 However, most organic foreign bodies are radiolucent and unlikely to be detected directly by chest CT.Citation8,Citation12,Citation15,Citation17
In some areas, owing to eating habits and customs, peppers in food may be incidentally aspirated into the lungs, causing obstructive pneumonia.Citation14 The irritable cough caused by the spicy stimulation of pepper makes this type of foreign body easily ignored, and it is easily overlooked on radiological examinations, as the pepper is not radiopaque. This makes diagnosis difficult, and patients may suffer from recurrent or refractory pneumonia for a long time; therefore, obstructive pneumonia caused by this reason requires further understanding.
Previous reports on obstructive pneumonia caused by pepper aspiration are particularly sparse and consist mainly of case reports or small case series; their radiological characteristics have not been well studied.Citation14,Citation18 Therefore, this study retrospectively collected data from 28 patients with confirmed pepper aspiration in Chongqing (a district with a long history of eating pepper), analyzed the CT features of bronchopulmonary abnormalities caused by pepper, and summarized their characteristics for early diagnosis and proper treatment.
Methods
Study Population
This study was approved by the Institutional Review Board of the First Affiliated Hospital of Chongqing Medical University. The requirement for written consent was waived because this was a retrospective study conducted at a single center.
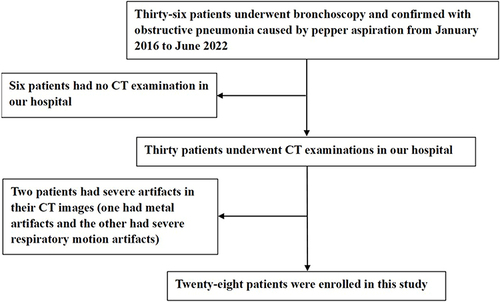
Electronic health records were used to search for patients who underwent bronchoscopy and had confirmed obstructive pneumonia caused by pepper aspiration from January 2016 to June 2022. Chest computed tomography (CT) scans and clinical data were collected and analyzed. The inclusion criteria were as follows: 1) patients with pepper aspiration confirmed by bronchoscopy and 2) patients had complete CT and clinical data. The exclusion criteria were as follows: severe artifacts in chest CT images that affected the evaluation. Finally, twenty-eight patients were included in this study. Selection process is showed in . The patients’ demographic information, clinical symptoms and their duration, history of eating pepper and aspiration, treatment (antibiotic therapy), bronchoscopy results, and chest CT findings were reviewed and recorded.
CT Examinations and Protocols
CT examinations were performed using one of the following scanners: Discovery CT750 HD (GE Healthcare, Milwaukee, WI, USA), SOMATOM Definition Flash (Siemens Healthineers, Erlangen, Germany), or SOMATOM Perspective (Siemens Healthineers). Breathing and holding training were performed on patients prior to image acquisition. The patients were placed in the supine position with both upper limbs raised, and CT images were acquired from the thoracic entrance to the costophrenic angle while holding breath after a single deep inspiration.
The CT parameters for the non-contrast scan images were set as follows: tube voltage, 110–130 kVp; tube current, 50–140 mAs (using automatic tube current modulation technology); pitch, 1.0–1.1; rotation time, 0.5 seconds; slice thickness and interval, 5 mm; and matrix, 512×512. All images were subsequently reconstructed using iterative reconstruction (standard or medium-sharp algorithm) with a slice thickness and an interval of 0.625–1.00 mm. After plain scanning, 17 patients underwent contrast-enhanced CT. The descending aorta was detected using an automatic bolus-tracking method with a threshold of 150 Hounsfield units (HU) and a delay of 6 s was set before scanning. Nonionic iodinated contrast medium (1.5 mL per kilogram) was injected at a flow rate of 3–3.5 mL per second, followed by approximately 30–50 mL of normal saline at the same rate.
Image Analysis
Combined with the results of bronchoscopy, patients’ CT images were reviewed by two radiologists with 5 and 11 years of experience in chest CT, and disagreements in CT findings were eliminated through consensus. The foreign bodies and their morphological features were visualized using axial images (with an adjusted window setting), multiplanar reconstruction (MPR), or volume rendering (VR) images.
The CT characteristics of bronchopulmonary abnormalities in patients were analyzed, including the location of the foreign body in different lobes and bronchi, manifestation of an intraluminal foreign body, bronchial changes around the foreign body, involvement of adjacent bronchi without a foreign body, features and involvement of obstructive pneumonia, pleural effusion (yes or no), hilar and/or mediastinal lymph node enlargement (yes or no), bronchial artery dilatation (present or absent) on enhanced CT images, and concurrent lesions in other lung fields (present or absent).
Results
Patients’ Clinical Characteristics
Among the 28 patients (mean age, 54 ± 11 years; range, 27–70 years), 10 (35.7%) were male and 18 (64.3%) were female. All had a history of eating pepper, but only six (21.4%) individuals had a definite history of pepper aspiration. Regarding patients’ clinical symptoms, the most common one was cough (n = 26, 92.9%), followed by expectoration (n = 23, 82.1%), and fever (n = 3, 10.7%). Their clinical symptoms lasted from 2 weeks to 8 years, and worsened in 14 (50.0%) cases in recent days. Of the 17 patients who underwent antibiotic therapy, clinical symptoms were relieved in 11 (64.7%) after treatment ().
Table 1 Patients’ Clinical Characteristics and Bronchoscopy Findings (n = 28)
Bronchoscopy Findings
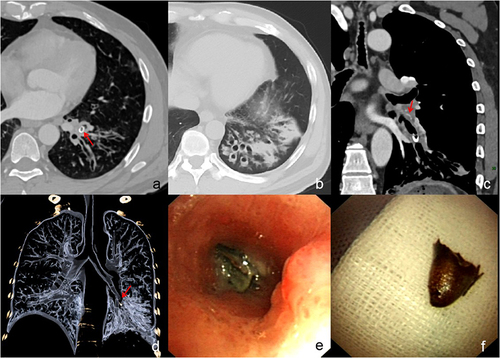
Bronchoscopy revealed that peppers were frequently distributed in the right lower lobe (18 cases, 64.3%), followed by the left lower lobe (5 cases, 17.9%), right middle lobe (4 cases, 14.3%), and left upper lobe (1 case, 3.6%), mainly located in the segmental bronchus (18 cases, 64.3%), lobar bronchus (6 cases, 21.4%), and sub-segmental bronchi (4 cases, 14.3%). In the involved bronchi, complete pepper shell and pepper fragments were found in 22 (78.6%) and six (21.4%) cases, respectively. Granulation tissue around the pepper, purulent secretion ( and ), and swelling of the adjacent bronchi were detected in 24 (85.7%), 11 (39.3%), and 12 (42.9%) cases, respectively ().
Figure 2 A 56-year-old woman with cough and expectoration for 2 years and no definite history of pepper aspiration. Axial (a) and coronal (b) CT images show annular (red arrow) and V-shaped (red arrow) high density in the outer basal segment bronchus of the right lower lobe and atelectasis. Sagittal enhanced CT image shows the thickened bronchial wall adjacent to foreign body and bronchiectasis with mucus plugs (arrows) in atelectasis (c). Bronchoscopy examination shows purulent secretion (d, arrow) and white foreign body (e, arrow) in the opening of the bronchus. Finally, the foreign body is revealed as pepper shell (f).
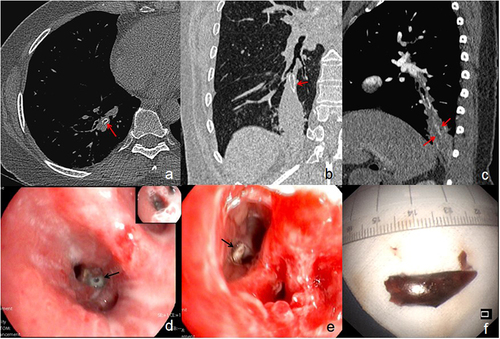
Figure 3 A 47-year-old man with cough and expectoration for 8 years and definite history of pepper aspiration. Axial CT images show annular (red arrow) high density in the antero-medial basal segment bronchus of the left lower lobe (a) and bronchiectasis and consolidation (b). Coronal enhanced CT image (c) shows thickened bronchial wall adjacent to U-shaped high density foreign body and bronchial artery dilatation (arrows). Volume rendering image (d) shows occlusion of the bronchus with foreign body (arrow) and distal extensive bronchiectasis. Bronchoscopy examination shows purulent secretion mixed with red foreign body (e) in the opening of the bronchus. Finally, the foreign body is revealed as pepper shell (f).
CT Findings of Pepper and Adjacent Bronchi
The CT characteristics of the peppers and the adjacent bronchi are presented in . In combination with bronchoscopy Results, intraluminal peppers in one patient (3.6%) could not be located on CT images, while those in other patients were shown as circular or U/V-shaped high-density (8 cases, 28.6%) (median [interquartile range] duration of symptoms: 365 [2069] days), localized soft tissue (16 cases, 57.1%), and flocculent (3 cases, 10.7%) opacification (240 [275] days). Wall thickening, occlusion, and stenosis of the bronchi with peppers were detected in 28 (100%), 19 (67.9%), and 9 (32.1%) patients, respectively (). For adjacent segmental or subsegmental bronchi without peppers, wall thickening with stenosis and/or occlusion was detected in 23 (82.1%) patients.
Table 2 CT Characteristics of Pepper and Adjacent Bronchi
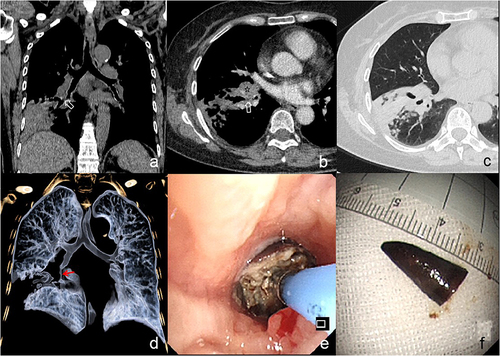
Figure 4 A 70-year-old woman with cough and expectoration for 6 months and definite history of pepper aspiration. Coronal CT image shows localized soft tissue density opacification (arrow) at the opening of anterior basal segment bronchus of the right lower lobe (a). On axial CT image, it has no significant enhancement (arrow), and enlarged lymph node (asterisk) at right hilum (b) as well as distal consolidation and nodules could be detected (c). Volume rendering image (d) shows occlusion and stenosis (arrow) of the right lower lobe bronchi and distal bronchiectasis. Bronchoscopy examination shows red foreign body containing secretion (e) in the opening of the bronchus. Finally, the foreign body is revealed as pepper shell (f).
CT Findings of Obstructive Pulmonary Lesions
Obstructive pulmonary lesions involved 1, 2, 3, and 4 segments in 6 (21.4%), 10 (35.7%), 11 (39.3%), and 1 (3.6%) patients, respectively (). Among the involved segments, the lateral basal segment of the lower lobe (20 [71.4%]) was the most commonly involved. The main CT manifestations of obstructive pulmonary lesions included consolidation or atelectasis, bronchiectasis with or without infection, and strip-shaped opacification in 24 (85.7%), 3 (10.7%), and 1 (3.6%) patient, respectively (). Among 24 patients with consolidation or atelectasis, 12 (50.0%) had bronchiectasis with mucus plugs in the lesions.
Table 3 Characteristics of Obstructive Pneumonia and Other Features on CT
Other Findings on Chest CT
Pleural effusion, enlargement of the hilar and/or mediastinal lymph nodes, and concurrent inflammation in other lung fields were detected in 2 (7.1%), 22 (78.6%), and 2 (7.1%) cases, respectively (). Among the eight patients with simultaneous hilar and mediastinal lymph node enlargement (), six (75.0%) had only subcarinal lymph node enlargement in the mediastinum. Bronchial artery dilatation was detected in 11 (64.7%) of 17 patients with enhanced CT data.
Discussion
As for foreign body aspiration, clear history of aspiration and special clinical manifestations are helpful in confirming the diagnosis. However, a few patients in the present study had an exact history of aspiration, and their clinical manifestations were atypical because eating peppers could also cause cough; thus, a definite diagnosis was difficult. Although the clinical manifestations are atypical, they tend to gradually worsen in some patients, and some may show poor results with conventional treatment. Therefore, the possibility of obstructive pneumonia should also be considered. The bronchopulmonary abnormalities caused by pepper aspiration were found to have some characteristics on CT images, which mainly manifested as U/V-shaped or annular high-density or localized soft tissue density in the bronchus of the lower lobes, extensive wall thickening with stenosis or occlusion in the surrounding bronchi, and consolidation or atelectasis in multiple distal lung segments.
Previous studies have reported that foreign body in adult patients was more frequently located in the right bronchial tree, especially in the bronchus of right lower lobe.Citation11,Citation14,Citation15,Citation19,Citation20 In the present study, the bronchus of the right lower lobe was the most common site of pepper impaction. The larger diameter, vertical nature, and greater airflow through the right main bronchus, which may lead to the higher frequency of aspiration into the right bronchial tree.Citation19,Citation21 In addition, pepper segments but not pepper fragments were found in most cases. This may be related to the different sizes of peppers; bigger pepper segments are more difficult to cough than smaller fragments.
The duration and degree of obstruction as well as the location and size of the foreign object may result in varying clinical manifestations of foreign object aspiration.Citation12 The most common symptom is cough, other symptoms include choking, vomiting, cyanosis, wheezing, stridor, dyspnea, chest pain, hemoptysis, sneezing, fever, and sputum.Citation12–15,Citation22,Citation23 In this study, cough and sputum were the most common symptoms, whereas others were relatively rare. This may be because of the active ingredients of pepper, which may also cause respiratory symptoms. Moreover, peppers are soft and hollow, and small fragments or cone-shaped peppers rarely remain in the trachea or main bronchi, resulting in few symptoms, such as choking and wheezing. In addition, after antibiotic treatment, chronic respiratory symptoms may recur or do not improve significantly. Owing to neglect or ignorance, accidental aspiration events may be masked by coughing, which is mistakenly caused by pepper stimulation. Therefore, it is difficult to make a diagnosis based on the symptoms alone; however, there is a possibility of obstructive pneumonia.
The positive detection rate of foreign bodies on CT images largely depends on the image slice thickness and physical nature of the aspirated objects.Citation16 Substances like radiopaque materials are more easily detected, such as metals and bones.Citation8 The most common aspirated foreign objects are organic food.Citation13,Citation24 Owing to their radiolucent nature, they cannot be directly detected on CT.Citation8,Citation13 In this study, in combination with bronchoscopy findings, it was revealed that a small proportion of peppers showed circular or U/V-shaped high density, which may be related to the occurrence of calcification in it. This manifestation is more specific because the shape of the pepper can be described. In contrast, more intraluminal peppers showed localized soft tissue density or flocculent opacification, which may be a manifestation of peppers mixed with the surrounding granulation tissue and containing secretions. This non-specific manifestation can be distinguished from that of early bronchogenic carcinomas. Previous studies have found that the latter mostly has a hilar location and commonly manifests as an endobronchial nodular protrusion without extensive bronchial thickening.Citation25–27 Additionally, persistent endobronchial focal soft tissue density or flocculent opacification without enhancement should also be considered as a possibility of foreign body obstruction.
In addition to the pepper itself, changes in the surrounding structures must also be considered. In this study, the bronchi adjacent to the pepper were extensively involved and presented with significant bronchial wall thickening with lumen stenosis or occlusion. These changes may be related to long-lasting stimulation of peppers and recurrent inflammation. Moreover, the obstructive pulmonary lesions were consistent with bronchial involvement, which manifested as multiple segmental consolidation or atelectasis with or without bronchiectasis. Previous studies have also reported that obstructive pneumonia includes bronchiectasis and bronchiolectasis with mucous plugging, a variety of parenchymal inflammatory changes, and significant atelectasis.Citation5 Therefore, when looking for the cause of protracted segmental consolidation or atelectasis with or without bronchiectasis, more attention should be paid to the proximal bronchi and their patency.
Previous studies have reported that other features caused by foreign bodies include hilar lymph node enlargement and pleural effusion, especially the former,Citation11,Citation14–16,Citation28 which are most likely secondary to long-term recurrent infection.Citation29 Most patients in the present study also had regional lymph node enlargement, whereas a few patients had pleural effusion. Bronchiectasis usually occurs secondary to chronic or recurrent infections, which can lead to bronchial artery dilatation.Citation30 In this study, bronchial artery dilatation was observed in most patients who underwent an enhanced CT scan, which also indicated a chronic process of pulmonary lesions. Therefore, pulmonary lesions with regional lymph node enlargement and bronchial artery dilatation indicate a high risk of chronic inflammation.
This study has several limitations. First, some peppers without normal shapes or colors were difficult to identify, which led to a relatively small sample size in present study. Second, not all peppers could be visualized on CT images directly unless calcification occurred because they were frequently surrounded by granulation tissue. Thus, the present findings may be more applicable to the districts or individuals with specific dietary histories. Third, the value of enhanced CT images in identifying bronchopulmonary lesions caused by peppers is unclear, because enhanced CT scans were not performed in all patients.
Conclusion
In Conclusion, bronchopulmonary abnormalities caused by pepper aspiration have several characteristics. In a district where peppers are popular, in combination with a history of eating pepper and clinical symptoms, obstructive pneumonia due to pepper aspiration should be suspected if there is U/V-shaped or annular high-density or localized soft tissue density in the bronchus of the lower lobes, with extensive wall thickening, stenosis, and occlusion of the surrounding bronchi, and consolidation or atelectasis in multiple distal lung segments. For suspected patients, further bronchoscopic examination may be appropriate for confirming, treating, or excluding other possibilities.
Ethics Approval and Consent to Participate
This study conformed to the Declaration of Helsinki on Human Research Ethics standards and was approved by the institutional review board of the First Affiliated Hospital of Chongqing Medical University (number 2019–062). The need for written, informed consent was waived by the institutional review board of the First Affiliated Hospital of Chongqing Medical University because of the retrospective design.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
Data Sharing Statement
The datasets used and/or analyzed during the current study are not publicly available because the cases are from the Picture Archiving and Communicating System of our Hospital but are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Torres A, Cilloniz C, Niederman MS, et al. Pneumonia. Nat Rev Dis Primers. 2021;7(1):25. doi:10.1038/s41572-021-00259-0
- Lanks CW, Musani AI, Hsia DW. Community-acquired pneumonia and hospital-acquired pneumonia. Med Clin North Am. 2019;103(3):487–501. doi:10.1016/j.mcna.2018.12.008
- Neill S, Dean N. Aspiration pneumonia and pneumonitis: a spectrum of infectious/noninfectious diseases affecting the lung. Curr Opin Infect Dis. 2019;32(2):152–157. doi:10.1097/QCO.0000000000000524
- Bledsoe TJ, Nath SK, Decker RH. Radiation Pneumonitis. Clin Chest Med. 2017;38(2):201–208. doi:10.1016/j.ccm.2016.12.004
- Burke M, Fraser R. Obstructive pneumonitis: a pathologic and pathogenetic reappraisal. Radiology. 1988;166(3):699–704. doi:10.1148/radiology.166.3.3340764
- Rolston KVI, Nesher L. Post-obstructive pneumonia in patients with cancer: a review. Infect Dis Ther. 2018;7(1):29–38. doi:10.1007/s40121-018-0185-2
- Abers MS, Sandvall BP, Sampath R, et al. Postobstructive pneumonia: an underdescribed syndrome. Clin Infect Dis. 2016;62(8):957–961. doi:10.1093/cid/civ1212
- Bajaj D, Sachdeva A, Deepak D. Foreign body aspiration. J Thorac Dis. 2021;13(8):5159–5175. doi:10.21037/jtd.2020.03.94
- Rolston KV. Postobstructive pneumonia in cancer patients. Clin Infect Dis. 2016;63(5):707–708. doi:10.1093/cid/ciw368
- Valvani A, Martin A, Devarajan A, et al. Postobstructive pneumonia in lung cancer. Ann Transl Med. 2019;7(15):357. doi:10.21037/atm.2019.05.26
- Blanco Ramos M, Botana-Rial M, García-Fontán E, et al. Update in the extraction of airway foreign bodies in adults. J Thorac Dis. 2016;8(11):3452–3456. doi:10.21037/jtd.2016.11.32
- Tseng H-J, Hanna TN, Shuaib W, et al. Imaging foreign bodies: ingested, aspirated, and inserted. Ann Emerg Med. 2015;66(6):570–582.e5. doi:10.1016/j.annemergmed.2015.07.499
- Risal R, Aung HM, Jahir T, et al. Endobronchial foreign bodies presenting as intermittent chest pain and productive cough. Cureus. 2022;14(9):e29599. doi:10.7759/cureus.29599
- Lin L, Wang Y, Zha X, et al. Cayenne aspiration: an unusual type of lower airway foreign-body aspiration. Clin Interv Aging. 2014;9:2019–2025. doi:10.2147/CIA.S73985
- Hewlett JC, Rickman OB, Lentz RJ, et al. Foreign body aspiration in adult airways: therapeutic approach. J Thorac Dis. 2017;9(9):3398–3409. doi:10.21037/jtd.2017.06.137
- Lin L, Lv L, Wang Y, et al. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging. 2014;9:1613–1618. doi:10.2147/CIA.S70924
- Sumanth TJ, Bokare BD, Mahore DM, et al. Management of tracheobronchial foreign bodies: a retrospective and prospective study. Indian J Otolaryngol Head Neck Surg. 2014;66(Suppl 1):60–64. doi:10.1007/s12070-011-0302-y
- Lai Y, Huang J, Zhou X, et al. Regional dietary characteristics and bronchial foreign body: a repeated misdiagnosis caused by a red pepper. J Thorac Dis. 2017;9(3):E180–E2. doi:10.21037/jtd.2017.03.35
- Sehgal IS, Dhooria S, Ram B, et al. Foreign body inhalation in the adult population: experience of 25,998 bronchoscopies and systematic review of the literature. Respir Care. 2015;60(10):1438–1448. doi:10.4187/respcare.03976
- Reddy RZ, Carter YM, Hsia DW. Successful removal of a chronic aspirated foreign body after twelve years. Case Rep Pulmonol. 2018;2018:8241591. doi:10.1155/2018/8241591
- Ramos MB, Fernández-Villar A, Rivo JE, et al. Extraction of airway foreign bodies in adults: experience from 1987–2008. Interact Cardiovasc Thorac Surg. 2009;9(3):402–405. doi:10.1510/icvts.2009.207332
- Ma W, Hu J, Yang M, et al. Application of flexible fiberoptic bronchoscopy in the removal of adult airway foreign bodies. BMC Surg. 2020;20(1):165. doi:10.1186/s12893-020-00825-5
- Ng J, Kim S, Chang B, et al. Clinical features and treatment outcomes of airway foreign body aspiration in adults. J Thorac Dis. 2019;11(3):1056–1064. doi:10.21037/jtd.2018.12.130
- Dong Y-C, Zhou G-W, Bai C, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med. 2012;51(18):2515–2519. doi:10.2169/internalmedicine.51.7672
- Gupta A, Shah A. Bronchial anthracofibrosis: an emerging pulmonary disease due to biomass fuel exposure. Int J Tuberc Lung Dis. 2011;15(5):602–612. doi:10.5588/ijtld.10.0308
- Byrd RB, Carr DT, Miller WE, et al. Radiographic abnormalities in carcinoma of the lung as related to histological cell type. Thorax. 1969;24(5):573–575. doi:10.1136/thx.24.5.573
- Choi JA, Kim JH, Hong KT, et al. CT bronchus sign in malignant solitary pulmonary lesions: value in the prediction of cell type. Eur Radiol. 2000;10(8):1304–1309. doi:10.1007/s003300000315
- Zissin R, Shapiro-Feinberg M, Rozenman J, et al. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol. 2001;11(4):606–611. doi:10.1007/s003300000619
- Torres de Amorim e Silva CJ, Fink AM. Case 137: pneumonia and bronchiectasis secondary to unrecognized peanut impaction. Radiology. 2008;248(3):1080–1082. doi:10.1148/radiol.2483050725
- Walker CM, Rosado-de-Christenson ML, Martínez-Jiménez S, et al. Bronchial arteries: anatomy, function, hypertrophy, and anomalies. Radiographics. 2015;35(1):32–49. doi:10.1148/rg.351140089