Abstract
Objective
This study aims to explore the correlates of frailty in hospitalized elderly hypertensive patients and its impact on clinical prognosis, and to construct a predictive model for the occurrence of frailty in this population.
Methods
A cross-sectional and prospective observational cohort study was conducted, involving 312 elderly hypertensive patients diagnosed at the institution from January to June 2022. Frailty was diagnosed using the Fried Frailty Phenotype (FP), while the Charlson Comorbidities Index (CCI) assessed the presence of chronic conditions. Data analysis was performed using SPSS 22.0. Binary logistic regression analysis was conducted with frailty as the dependent variable to identify risk factors. Patients were followed for one year to monitor readmission rates and all-cause mortality.
Results
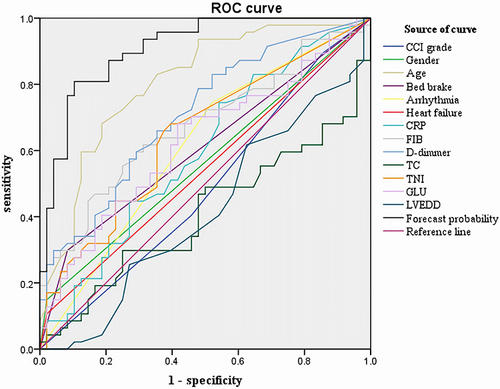
Multivariate logistic regression identified CCI grade (P=0.030), gender (OR=21.618, 95% CI: 4.062–115.061, P < 0.001), age (OR=1.147, 95% CI: 1.086–1.211, P < 0.001), bedridden state (OR=11.620, 95% CI: 3.282–41.140, P < 0.001), arrhythmia (OR=14.414, 95% CI: 4.558–45.585, P < 0.001), heart failure (OR=5.439, 95% CI: 1.029–28.740, P < 0.05), along with several biochemical markers, as independent predictors of frailty. A predictive model was developed, demonstrating a robust discriminative ability with an area under the receiver operating characteristic curve (AUC) of 0.915. Statistically significant differences in readmission rates and all-cause mortality were observed among the frail, pre-frail, and non-frail groups (P<0.001), with the frail group exhibiting the highest incidence of these adverse outcomes. Notably, frailty emerged as a significant predictor of readmission (P<0.05) but not of all-cause mortality in this cohort.
Conclusion
This study establishes a robust frailty prediction model for elderly hypertensive patients, highlighting the influence of CCI grade, gender, age, and other clinical and biochemical factors on frailty. The model offers a valuable tool for healthcare providers to identify at-risk elderly individuals, facilitating targeted intervention strategies for cardiovascular disease management.
Introduction
The Burden of Hypertension in the Geriatric Population
Hypertension is highly prevalent among the elderly population and constitutes one of the most common non-communicable chronic diseases in this group.Citation1 A StudyCitation2 indicate that over half of Chinese individuals aged 60 years and above have hypertension. Foreign epidemiological survey reports reveal that the proportion of hypertension among the elderly over 65 years old has exceeded 60%, and the incidence of hypertension in those over 80 years old has surpassed 70%.Citation3 A systematic review of community-dwelling elderly individuals over 65 years old demonstrated that the prevalence of frailty reached 10%, and the prevalence among those over 85 years old reached 26.1%.Citation4 With the acceleration of population aging and the elongation of human life expectancy, the proportion of elderly hypertensive patients complicated with frailty is gradually escalating, which renders the prognosis assessment and management of elderly hypertension more complex and challenging.Citation5 Elderly patients with hypertension are typically accompanied by a variety of other disorders and are prone to debilitating symptoms. The incidence of frailty rises with age and gradually increases due to physical deterioration and multiple complications.Citation6
Frailty: A Growing Concern in Geriatric Health
Frailty, often accompanying hypertension, is a syndrome with profound implications for health outcomes in the elderly. Its prevalence is on an upward trajectory, linked to physiological decline and the accumulation of comorbid conditions. In the National Health and Nutrition Examination survey of 4352 elderly people, the prevalence of hypertension in the frail elderly was 67.8%, which was higher than that in the pre-frail and non-frail elderly.Citation7 A meta-analysis of 7656 elderly people showed that the prevalence of hypertension was 72% in frail individuals and 14% in hypertensive patients.Citation8 Frailty is a clinical syndrome, referring to a nonspecific state where the physical reserves of the elderly decrease, leading to an increase in weakness and a decline in anti-stress ability, which could result in falls, fractures, hospitalizations, disabilities, lower quality of life, and death, among other negative health outcomes.Citation9–12
The Interconnection Between Frailty and Hypertension
Studies have shown that the prognosis of elderly patients with hypertension is closely associated with frailty during disease progression.Citation11 In patients whose disease progression is predominantly characterized by frailty, the cause of death is highly correlated with higher blood pressure levels.Citation12 With the extensive mention of the concept of frailty, an increasing number of studies have explored the pathogenesis of frailty and hypertension in the elderly.Citation13,Citation14 A study indicated that frail older adults had higher levels of arterial stiffness, which might contribute to explaining the relationship between frailty and cardiovascular disease.Citation14 A study have discovered that frailty in the elderly is associated with target organ damage of hypertension, and arteriosclerosis may be the common mechanism leading to frailty, hypertension, and target organ damage.Citation15
The Reversible Nature of Frailty and Its Clinical Implications
Despite the adverse outcomes associated with frailty, there is evidence of its reversibility. Early detection and risk factor analysis in the elderly are critical for the implementation of targeted interventions that can potentially reverse or mitigate frailty’s progression, thereby reducing the incidence of adverse health outcomes. This is particularly important for clinicians when assessing treatment risks and making prognostic evaluations. In recent years, although some studies have investigated the potential relationship between frailty and hypertension,Citation16 the risk factors for frailty and the influence of frailty-related risk factors on the clinical prognosis of elderly hypertensive patients remain unclear.
While the relationship between frailty and hypertension has begun to be explored, a thorough understanding of the specific risk factors for frailty in the elderly hypertensive population and their impact on clinical prognosis is still lacking. Therefore, this study intends to clarify the epidemiological characteristics of frailty within the context of hypertension, identify its risk factors, and investigate its impact on all-cause mortality. Additionally, a predictive model for frailty in elderly hypertensive patients hospitalized will be developed, aiming to facilitate the early identification of at-risk populations, assess their prognosis, and inform the development of personalized management strategies for elderly patients with hypertension.
Methods
Participants
A total of 320 older patients with hypertension who were hospitalized in the Second Medical Center of PLA General Hospital from January to June 2022 were studied. 312 patients were eventually included in the study analysis. Six patients did not complete frailty assessment, and 2 patients had incomplete data, which was excluded. Inclusion criteria for the study were: 1) age≥60 years old, 2) Meet the diagnostic criteria of essential hypertension, 3) Regular use of antihypertensive drugs. Exclusion criteria were: 1) secondary hypertension, 2) malignant tumor, 3) severe cognitive dysfunction or mental illness, 4) Personal reasons or inability to cooperate with the completion of comprehensive geriatric assessment (CGA).
Sample Size Calculation
The sample size of logistic regression is generally required to be more than 5–10 times the number of observation indicators. Thirty-seven indexes were included in this study, with a sample size of 185–370. Considering the number of hospitalized patients and shedding, 320 cases were included. During the study, some patients fall off, and eventually were analyzed in 312 cases of patients, satisfies the requirement of data analysis.
Clinical Interview and Assessment
A cross-sectional and prospective observational cohort study was used. All enrolled patients received routine CGA within 1 week of admission (if admitted as an emergency, within 1 week after their condition stabilized). FP scale, which is the most widely used in the world, was adopted and evaluated by geriatric medical staff who had received standardized training, including 5 items (1) unexplained weight loss (2) fatigue (3) decreased grip strength (4) Walking speed decreased (5) decreased physical activity ability (decreased physical activity). Meeting ≥3 items is frail, meeting 1 or 2 items is pre-frail, 0 items is non-frail. The FP scale was used to evaluate frailty in 312 hospitalized older patients with hypertension. According to FP score, patients were divided into three groups, the frail group (150 cases), the pre-frail group (144 cases) and the non-frail group (18 cases). The older patients with hypertension were followed up for one year. Major adverse events (including readmissions and deaths from various causes) were observed and recorded in each group through outpatient visits or telephone calls after discharge. All procedures involving human participants were performed in accordance with the basic principles of the Declaration of Helsinki. Ethical approval was obtained from the PLA General Hospital (No.S2022-262-02). In this study, patients gave informed consent. All patient data were anonymized and maintained with confidentiality.
Data Collection
General Information
Basic data were collected and recorded, including age, gender, smoking, drinking, Charlson comorbidity index, and past medical history (coronary heart disease, arrhythmia, valvular heart disease, cardiomyopathy, heart failure, diabetes, chronic lung disease, and chronic kidney disease). According to the range of CCI scores, suggestions from clinicians and literature reports,Citation17 the degree of complications was divided into three grades. Grade 0 is no/mild comorbidities (CCI score 0~1), grade 1 is moderate comorbidities (CCI score 2~3), and grade 2 is severe comorbidities (CCI score≥4).
Echocardiography
After admission, all patients underwent echocardiography to measure left ventricular ejection fraction (LVEF), left ventricular posterior wall diastole (LVPWD), interventricular septal thickness at diastole (IVSD), left ventricular end-diastolic diameter (LVEDD) and left ventricular end-systolic diameter(LVESD).
Laboratory Examination
The enrolled patients received fasting blood on the day of admission or the next day. Hemoglobin, red blood cell count, white blood cell count, platelet count, NT-proBNP, serum albumin, urea nitrogen, creatinine, fasting blood glucose and so on were measured and recorded.
Hypertension Criteria
In accordance with the 2019 Chinese Guidelines for the Management of Hypertension in Older Adults,Citation18 hypertension is diagnosed when systolic and/or diastolic blood pressure reaches or exceeds 140 mmHg and/or 90 mmHg, respectively, as recorded during three separate clinical visits while the patient is not receiving antihypertensive medication. Isolated systolic hypertension is defined by a systolic blood pressure (SBP) of 140 mmHg or greater and a diastolic blood pressure (DBP) of less than 90 mmHg. Furthermore, individuals with a documented history of hypertension who are undergoing treatment with antihypertensive medications are considered hypertensive, even if their blood pressure readings fall below the threshold of 140/90 mmHg.
Statistical Analysis
Statistical analyses were conducted using SPSS 22.0. The Kolmogorov–Smirnov test was applied to ascertain whether all variables conformed to normal distributions, while the Levene test assessed the homogeneity of variances. Continuous variables with a normal distribution were detailed as mean ± standard deviation and analyzed using Analysis of Variance (ANOVA). For those continuous variables that did not adhere to a normal distribution, the Kruskal–Wallis test was employed. Categorical variables were presented as frequencies and percentages and analyzed using the Chi-Square Test. Univariate analysis was performed on both frail and non-frail subgroups of cardiac inpatients to uncover the risk factors associated with frailty. To further investigate the relationship between frailty and cardiac disease, binary logistic regression analysis was conducted on factors that showed significant differences post-univariate analysis, with frailty set as the dependent variable. The significance threshold was established at p < 0.05.
Quality Control
According to the criteria for the inclusion and exclusion of cases, completed unified data collection forms were used to screen and collect cases that met the study criteria. Double data entries and logic verification were used to ensure data accuracy. Upon completion, all data were checked, missing data were completed, and duplicated or erroneous data were removed.
Results
Frailty Incidence in Older Hypertensive Patients
In this study, the results showed that the incidence of frailty was 48.1%.
Univariate Analysis of Factors Related to Frailty in Older Patients with Hypertension
The normality test of continuous variables showed that all variables did not conform to normal distribution, so the rank sum test was adopted. Categorical variable grouping belongs to ordered grouping, and rank sum test is used to test the difference among the three groups. The results showed that patients in the three groups had significant differences in gender, age, bedridden, smoking, drinking, coronary heart disease, Hb, RBC, LVEF, IVSD and so on showed statistical difference (P < 0.05), as shown in .
Table 1 Univariate Analysis of Factors Related to Frailty in Old Patients with Hypertension
Logistic Regression Analysis of Factors Related to Frailty in Older Patients with Hypertension
The ordered logistic multifactor analysis was conducted for the indicators with statistical significance in univariate analysis, and the Test of parallel lines was selected, χ2=66.112, P= 0.000, indicating that the hypothesis of parallelism was not valid, that is, the regression equations were not parallel to each other. An ordered Logistic procedure cannot be used for analysis. In this study, whether patients were frailty or not was divided into frail group and non-frail group as dependent variable segmentation points, and binary Logistic regression was performed. The factors with statistical significance in univariate analysis, including age, were analyzed by binary logistic regression, the model was selected for backward (wald model) stepwise regression, and the CCI grade was treated with dummy variables. The significance level of the selected variable was set at 0.05, and the significance level of the retained variable was set at 0.10. After comparison, it was found that there were statistically significant differences in CCI grade(X0)(P<0.05), gender(X1)(OR=21.618, P<0.001), age(X2)(OR=1.147, P<0.001), bedridden(X3)(OR=11.620, P<0.001), arrhythmia(X4)(OR=14.414, P<0.001), heart failure(X5)(OR=5.439, P<0.05), CRP(X6)(OR=0.625, P<0.05), FIB(X7)(OR=2.562, P<0.05), D-dimmer(X8)(OR=5.079, P<0.05), TC(X9)(OR=0.344, P<0.05), TNI(X10)(OR=1.300, P<0.05), GLU(X11)(OR=1.489, P<0.05) and LVEDD(X12)(OR=0.913, P<0.05) between the two groups (P < 0.05), which were the related factors for the weakness of older patients with hypertension, as shown in .
Table 2 Logistic Regression Analysis of Factors Related to Frailty in Old Hypertension Patients
Establish Logistic Regression Prediction Model
Logistic Regression Prediction Model of Frailty in Older Hypertensive Patients
| (1) | CCI grade 0: P=1/(1+exp(16.069–3.074X1-0.137X2-2.453X3-2.668X4-1.694X5+0.470X6-0.941X7-1.625X8+1.067X9-0.262X10-0.398X11+0.091X12)) | ||||
| (2) | CCI grade 1: P=1/(1+exp(16.069+0.014X0-3.074X1-0.137X2-2.453X3-2.668X4-1.694X5+0.470X6-0.941X7-1.625X8+1.067X9-0.262X10-0.398X11+0.091X12)) | ||||
| (3) | CCI grade 2: P=1/(1+exp(16.069+1.014X0-3.074X1-0.137X2-2.453X3-2.668X4-1.694X5+0.470X6-0.941X7-1.625X8+1.067X9-0.262X10-0.398X11+0.091X12)) | ||||
This model is used for preliminary prediction of frailty in older hypertensive patients to predict whether frailty will occur in older hypertensive patients. The closer the P-value is to 1, the more likely the patient is to have frailty. The closer the P-value is to 0, the less likely the patient is to have frailty.
Prediction Effect Evaluation of Logistic Regression Models
| (1) | Wald test was used, χ2= 9.617, df=1, P=0.002, the coefficient of regression equation was statistically significant. | ||||
| (2) | Goodness of fit test of Logistic regression equations.The Hosmer-Lemeshow goodness of fit test results obtained χ2=12.287, df=8, P=0.139, indicating a good fit of the model. | ||||
| (3) | Discriminant ability of logistic regression equations. | ||||
The ROC curve was drawn with “1-specificity” as the abscissa and “sensitivity” as the ordinate. When 0.5≤the area under the curve (AUC) <0.7, it was considered that the discriminant value of the model was acceptable When 0.7≤AUC<0.9, it was considered that the discriminant value of the model was favorable. When 0.9≤AUC, the value of the model was considered outstanding.
The results of this study show that the AUC of the prediction probability of the new variable was 0.915, indicating that the discriminant effect of the model was very good. The AUC of the comprehensive index was higher than that of other indices (P<0.05), indicating that the comprehensive index more accurately identified frailty, and performed better than that of the single index for the identification of frailty ( and ).
Table 3 Area Under Curve
Analysis of Clinical Prognosis of Follow-Up Patients
Difference in Clinical Prognosis of Patients
The patients were followed up and 273 patients were discharged. There were 51 cases (51.5%) in the frail group, 27 cases (23.1%) in the pre-frail group, and none in the non-frail group. The difference between the three groups was statistically significant (χ2 = 26.442, P<0. 001) (see ). There were 24 (16%) all-cause deaths in the frail group, 6 (4.2%) in the pre-frail group, and no deaths in the non-frail group. The mortality difference among the three groups was statistically significant (P= 0.001) (see ).
Table 4 Follow-Up Readmissions of Old Patients with Hypertension
Table 5 Follow-Up Outcomes of Old Patients with Hypertension
Analysis of Factors Influencing the Clinical Prognosis of Older Hypertensive Patients
The factors influencing readmissions in older patients with hypertension were studied, and the single factors with statistical significance were analyzed by binary logistic regression (backward Wald). It was found that frailty score, coronary heart disease, left ventricular ejection fraction, and statistically significant differences in left ventricular end-diastolic diameter were independent risk factors influencing readmissions in older patients with hypertension ( and ). The factors affecting the death of older patients with hypertension were studied, and the single factors with statistical significance were analyzed by binary logistic regression (backward Wald), and statistically significant differences were found in age, length of hospital stay, smoking, LVEF, LVEDD and LVESD ( and ).
Table 6 Univariate Analysis of Readmissions and All-Cause Death in Old Patients with Hypertension
Table 7 Logistic Analysis of Readmissions Risk Factors in Old Patients with Hypertension
Table 8 Logistic Analysis of All-Cause Mortality Risk Factors in Old Patients with Hypertension
Discussion
Hypertension is recognized as a significant factor influencing the health of older adults. Antihypertensive treatments can reduce strokes, cardiovascular events, and mortality in older hypertensive patients. However, managing blood pressure in older adults is complex due to the coexistence of geriatric syndromes like frailty and other comorbidities. Recent guidelinesCitation19 recommend considering the functional status of older individuals when setting blood pressure targets, underscoring the importance of understanding and controlling frailty risk factors to improve the prognosis of older adults with hypertension. Managing hypertension in frail older patients presents unique challenges. Current hypertension guidelines have suggested frailty screening among older hypertensive patients, with new recommendations for blood pressure-lowering treatment in the frail population. However, the quality and consistency of these guidelines, as well as the supporting evidence for antihypertension treatment recommendations for frail older patients, are still unclear. A systematic reviewCitation20 of existing guidelines found considerable variations in methodology and reporting quality, and the recommendations were varied and inconsistent. This points to an urgent need for further trials to optimize treatment and develop specific guidelines for managing frail older hypertensive patients. A systematic review and meta-analysisCitation8 aimed to understand the association between hypertension and frailty in observational studies. The review, which included 27 studies out of an initial 964 articles, provided conflicting results. While some studies reported a significantly higher prevalence of frailty in hypertensive participants, others found no significant association. The pooled prevalence of hypertension in frail individuals was 72%, and the prevalence of frailty in individuals with hypertension was 14%. These findings indicate that frailty is common in persons with hypertension, and highlight the importance of assessing frailty in hypertensive patients due to its potential influence on the risk-benefit ratio of hypertension treatment.
In this study, the FP scale was used to evaluate frailty in 312 hospitalized older patients with hypertension, and the results showed that the detection rate of frailty was 48.1%. A meta-analysis of 23 cross-sectional studies showed that the prevalence of frailty was 14% in people over 60 years of age with hypertension.Citation11 In recent years, relevant domestic studies have found that the detection rate of frailty in hospitalized patients in the geriatric department is 50%-80%,Citation21 while the detection rate of frailty in Chinese community older people with hypertension is 19.6%.Citation22 The reason for the high frailty detection rate in this study may be that the included patients were older, with more older patients and skewed age distribution. In addition, in this study, the detection rate of pre-frail was as high as 46.2%. Over time, patients may transition between different stages of frailty (non-frail, pre-frail, frail), with their condition potentially deteriorating, improving, or remaining stable A studyCitation23 by Fudan University on the transitions in frailty status found that during the follow-up period, the proportion of older individuals who remained in the pre-frail stage was 34.39%, while those transitioning to frailty and death were 28.14% and 27.27%, respectively. Among those in the frail stage, 30.69% remained frail, with 9.38% reverting to pre-frailty and 58.24% leading to death. Therefore, early identification and intervention for these patients are crucial to avoid or delay the progression of frailty. Because frailty is reversible, studies have found that frailty can be improved or prevented with appropriate interventions. For example, proper nutrition is essential to prevent and improve frailty. Studies have shown that protein and vitamin D supplementation can improve muscle mass and function.Citation24 Regular physical exercise, especially the combination of resistance training and aerobic exercise, can significantly improve the physical function of frail elderly people.Citation25 Through pharmacological intervention, certain medications may help improve frailty-related symptoms, such as sarcopenia.Citation26 Other studies have found that social support and psychological intervention can improve the quality of life and functional status of the debilitated elderly. However, frailty is a complex problem with many influencing factors, so how to develop personalized and targeted intervention measures for patients with frailty is very important. In this study, a frailty prediction model for older hypertensive patients was developed. This risk prediction model can assist healthcare professionals in identifying high-risk older individuals, guiding the formulation of personalized intervention measures, in hopes of achieving an early reversal of the frailty status.
In current research,Citation27,Citation28 the prevalence of frailty exhibits inconsistencies and may be underestimated. It is a multifactorial syndrome associated with many factors. Studies show that frailty increases with the number of health deficits and the presence of multiple comorbidities. A 2023 systematic review with meta-analysisCitation29 examined the risk factors associated with (pre)frailty in this population. The authors included only 14 articles and concluded that frailty and prefrailty are prevalent in community dwelling older adults with hypertension, but limited risk factors were identified. This study further clarifies the influencing factors of this population and provides a basis for the development of targeted and individualized intervention measures. In this study, by binary logistic regression analysis, it was found that Charson’s grade, gender, age, whether or not to immutate, arrhythmia, heart failure, CRP, FIB, Ddimmer (D-dimer), TC, TNI, GLU and LVEDD were related factors affecting the weakness of older patients with hypertension (P < 0.05). Frailty in the older people and many chronic diseases, such as hypertension, arrhythmias, and heart failure, often interact with each other, forming a complex network of interactions. Delving into the relationship between frailty in the older people and cardiovascular diseases helps to understand the interactions and comorbid mechanisms between the two. A large-scale prospective cohort studyCitation30 investigated 5015 community-dwelling individuals aged 55 and above, free of cardiovascular disease (CVD), over a 10-year period. The study found that pre-frailty and frailty were significantly associated with an increased overall risk of CVD. The research indicates that frailty often coexists with cardiovascular diseases such as coronary artery disease (CAD), heart failure, and atrial fibrillation.Citation31 Frail patients undergoing revascularization for CAD have higher complication rates. A studyCitation32 of 1432 older adults aged 65 to 88 years from the Longitudinal Aging Study examined the bidirectional longitudinal association between CVD and frailty over 17 years. It found that patients with HF had a significantly increased risk of frailty after a median follow-up of 8.4 years, independent of potential confounders like age, sex, and several comorbidities. The functional decline caused by cardiovascular diseases can lead to reduced blood flow, affecting the supply of oxygen and nutrients to various parts of the body. This, in turn, may result in a decrease in muscle mass and function, which is one of the primary manifestations of frailty in the older people. Cardiovascular diseases are often accompanied by chronic inflammatory responses, and chronic inflammation is an important factor in frailty. For example, inflammatory markers such as C-reactive protein and white blood cells are typically higher in patients with cardiovascular diseases, and this is also associated with the development of frailty in the older patients. Patients with cardiovascular diseases often have limited mobility, which can lead to reduced physical activity, thereby accelerating the loss of muscle mass and the progression of frailty. There is a complex interrelationship between frailty and cardiovascular diseases, and these findings are significant for improving the treatment and management of patients with cardiovascular diseases.
Existing researchCitation29–34 has confirmed that frailty is an important risk factor for adverse health outcomes such as falls, death, and hospitalization, although the impact of frailty on the life expectancy of the older people is not fully clear. In this study, by following up on readmission and all-cause mortality in older patients with hypertension, it was found that the rate of readmission was significantly higher in the frail and pre-frail groups compared to the non-frail group, with a statistically significant difference. Multivariate logistic regression analysis confirmed that frailty is an independent risk factor for readmission in older hypertensive patients. When older hypertensive patients are frail, adverse events such as cognitive decline, falls, and malnutrition may occur, reducing their daily living abilities and quality of life, increasing the risk of illness, and further leading to readmission. This study also found that frailty is not an independent risk factor for all-cause mortality in patients. This conclusion may be inconsistent with existing research, possibly due to the shorter duration of the follow-up period.
This study had several limitations. This study only included older hypertensive patients hospitalized in the geriatric department of our hospital, mostly male patients, with a small sample size, there is a certain bias, and more multi-center, large-sample studies are needed to confirm. The current research on how to effectively intervene in the frailty state of hypertensive patients may not be sufficient, and the long-term effectiveness and safety of intervention measures still need further verification. Hypertension and frailty may be related to other health conditions and lifestyle factors, and accurately separating and controlling the impact of these factors on research results is a challenge. There is insufficient long-term tracking research on the frailty status of hypertensive patients, which limits a deeper understanding of the development process and outcomes of frailty.
Conclusion
In 312 hospitalized elderly patients with hypertension, the frailty detection rate was 48.1%. Frailty is associated with readmission in older patients with hypertension, but not with all-cause mortality. The CCI grade, gender, age, bedridden, arrhythmias, heart failure, CRP, LVEDD, etc., are closely related to frailty in older hypertensive patients. A frailty prediction model for older hypertensive patients has been established. This risk prediction model can help healthcare professionals identify high-risk older individuals. It aids in the development of specific intervention measures for cardiovascular disease patients, focusing on high-risk patients and influential factors. Molecular biological research is being conducted to explore the molecular and cellular mechanisms between age-related frailty and chronic diseases, such as inflammatory pathways, insulin signaling, and oxidative stress responses. These studies contribute to a better understanding of the complex relationships associated with aging.
Ethical Approval
The ethical approval was obtained from the PLA General Hospital(No.S2022-262-02).
Disclosure
The authors report no conflicts of interest in this work.
References
- Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294(4):66–72. doi:10.1001/jama.294.4.466
- Sheng C, Liu M, Kang Y, et al. Prevalence, awareness, treatment and control of hypertension in elderly Chinese. Lancet. 2013;36(9):4–8.
- Jayaraman MV, McTaggart RA, Sachs GM, Doberstein CE. Cerebellar pial arteriovenous malformations presenting with medullary venous hypertension: imaging and endovascular treatment. J Neurointerv Surg. 2010;2(1):38–40. doi:10.1136/jnis.2009.000471
- Collard R, Boter H, Schoevers R, et al. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):87–92. doi:10.1111/j.1532-5415.2012.04054.x
- Topcuoglu MA, Rocha EA, Siddiqui AK, et al. Isolated upper limb weakness from ischemic stroke: mechanisms and outcome. J Stroke Cerebrovasc Dis. 2018;27(10):2712–2719. doi:10.1016/j.jstrokecerebrovasdis.2018.05.050
- Faruqui AA. EVOLVE (nebivolol evaluation for efficacy and safety in the treatment of hypertension) postmarketing surveillance study. J Indian Med Assoc. 2007;105(5):276–277. PMID: 17915798.
- Kang MG, Kim SW, Yoon SJ, et al. Association between frailty and hypertension prevalence, treatment, and control in the elderly Korean population. Sci Rep. 2017;7(1):7542. doi:10.1038/s41598-017-07449-5
- Vetrano DL, Palmer KM, Galluzzo L, et al. Joint Action ADVANTAGE WP4 group. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8(12):e024406. doi:10.1136/bmjopen-2018-024406
- Kojima GJD. Frailty as a predictor of disabilities among community-dwelling older people: a systematic review and meta-analysis. Disabil Rehabil. 2017;39(19):897–908. doi:10.1080/09638288.2016.1212282
- Vermeiren S, Vella-Azzopardi R, Beckwée D, et al. Frailty and the prediction of negative health outcomes: a meta-analysis. J AmMed Dir Assoc. 2016;17(12):1163.e1–e17. doi:10.1016/j.jamda.2016.09.010
- Hu K, Zhou Q, Jiang Y, et al. Association between frailty and mortality, falls, and hospitalization among patients with hypertension: a systematic review and meta-analysis. Biomed Res Int. 2021;2021:269–296.
- Dent E, Martin F, Bergman H, et al. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):76–86. doi:10.1016/S0140-6736(19)31785-4
- Bastos-Barbosa RG, Ferriolli E, Coelho EB, et al. Association of frailty syndrome in the elderly with higher blood pressure and other cardiovascular risk factors. Am J Hypertens. 2012;25(11):56–61. doi:10.1038/ajh.2012.99
- Orkaby AR, Lunetta KL, Sun FJ, et al. Cross-sectional association of frailty and arterial stiffness in community-dwelling older adults: the Framingham Heart Study. J Gerontol a Biol Sci Med Sci. 2019;74(3):3–9.
- Tabara Y, Masaki M, Ikezoe T, et al. Small degree of lumbar lordosis as an overlooked determinant for orthostatic increases in blood pressure in the elderly: the nagahama study. Am J Hypertens. 2019;32(1):61–69. doi:10.1093/ajh/hpy137
- Fabbian F, De Giorgi A, Cappadona R, et al. Hypertension, abnormal blood pressure circadian pattern, and frailty: data from the literature. J Geriatric Cardiol. 2018;15(12):747–750. doi:10.11909/j.issn.1671-5411.2018.12.002
- Zhang XH, Zhang ZH, Xu Y, et al. Influence of complications on early survival of patients with localized or locally advanced prostate cancer. J Tianjin Med Univ. 2014;20(5):379–382.
- Hypertension Branch of Chinese Geriatrics Society. National clinical research center for geriatric diseases - Chinese alliance of geriatric cardiovascular disease. 2019 Chinese guidelines for the management of hypertension in the elderly. Chin J Cardiovasc Med. 2019;24(1):1–23.
- Liu P, Li Y, Zhang Y, et al. Frailty and hypertension in older adults: current understanding and future perspectives. Hypertens Res. 2020;43(12):1352–1360. doi:10.1038/s41440-020-0510-5
- Hu K, Zhou G, Jiang M, et al. Hypertension treatment in frail older adults: a systematic review and appraisal of guidelines. Drugs Aging. 2023;40(10):881–893. doi:10.1007/s40266-023-01053-1
- Wu CQ, Hu SJ, Shen YY. Relationship between frailty syndrome and cognition and psychological factors in hospitalized elderly patients. Shanghai Nur. 2018;18(7):28–31.
- Ma L, Zhang L, Sun F, et al. Frailty in Chinese older adults with hypertension: prevalence, associated factors, and prediction for long-term mortality. J Clin Hypertens. 2018;20(11):1595–1602. doi:10.1111/jch.13405
- Gao J, Wang Y, Xu J, et al. Life expectancy among older adults with or without frailty in China: multistate modelling of a national longitudinal cohort study. BMC Med. 2023;21(1):101. doi:10.1186/s12916-023-02825-7
- Cheng H, Kong J, Underwood C, et al. Systematic review and meta-analysis of the effect of protein and amino acid supplements in older adults with acute or chronic conditions. Br. J. Nutr. 2018;119(5):527–542. doi:10.1017/S0007114517003816
- Cadore EL, Casas-Herrero A, Zambom-Ferraresi F, et al. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age. 2014;36(2):773–785. doi:10.1007/s11357-013-9586-z
- Obbia P, Graham C, Duffy FJR, et al. Preventing frailty in older people: an exploration of primary care professionals’ experiences. Int J Older People Nurs. 2020;15(2):e12297. doi:10.1111/opn.12297
- Siriwardhana DD, Hardoon S, Rait G, et al. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2018;8(3):e018195. doi:10.1136/bmjopen-2017-018195
- Rohrmann S. Epidemiology of frailty in older people. Adv Exp Med Biol. 2020;1216:21–27.
- Li Q, Duan AY, Jiang JQ, et al. Prevalence and risk factors of frailty in elderly hypertensive patients in the community: a Meta-analysis. J Hunan Norm Univers. 2023;20(06):151–156.
- Liu X, Tou NX, Gao Q, et al. Frailty and risk of cardiovascular disease and mortality. PLoS One. 2022;17(9):e0272527. doi:10.1371/journal.pone.0272527
- Uchikado Y, Ikeda Y, Ohishi M. Current understanding of the role of frailty in cardiovascular disease. Circ J. 2020;84(11):1903–1908. doi:10.1253/circj.CJ-20-0594
- Kleipool EE, Hoogendijk EO, Trappenburg MC, et al. Frailty in older adults with cardiovascular disease: cause, effect or both? Aging Dis. 2018;9(3):489–497. doi:10.14336/AD.2017.1125
- Cui LL, Wang Y, Sun MY, et al. Effect of frailty on the prognosis of elderly patients with atrial fibrillation. Chin J Cardiovasc Med. 2022;27(1):23–27.
- Li YY, Liang YD, Yao SM, et al. Impact of frailty on prognosis of elderly inpatients with cardiovascular disease. Chin J Cardiovasc Med. 2021;26(1):16–20.