Abstract
Introduction
Spontaneous intracranial hypotension is an infrequent cause of secondary headache due to cerebrospinal fluid (CSF) hypovolemia.
Objective
To describe a case of headache revealing spontaneous intracranial hypotension complicated by subdural hematoma following lumbar puncture.
Observation
A 34-year-old man presented with acute postural headache. The first cerebral computed tomography scan was normal. Lumbar puncture showed hyperproteinorachy at 2 g/L with six lymphocytic cells. The headache became very intense. At admission, clinical examination was normal. Ophthalmological examination did not show any abnormalities. Encephalic magnetic resonance imaging (MRI) showed bilateral subdural hematoma with tonsillar descent simulating Chiari type I malformation. After surgical drainage and symptomatic treatment, the patient was discharged with no recurrence.
Conclusion
Spontaneous intracranial hypotension is associated with simple clinical presentation, orthostatic headache, and characteristic MRI findings. Misdiagnosed, it leads to unnecessary procedures.
Introduction
Spontaneous or idiopathic intracranial hypotension (SIH) is rare.Citation1 Careful history taking and a high level of suspicion are essential to diagnose this syndrome. Brain imaging, especially magnetic resonance imaging (MRI), is very helpful for diagnosis confirmation. Misdiagnosis leads to unnecessary procedures. The authors present this illustrative case of postural headache revealing SIH misdiagnosed and complicated by subdural hematoma following lumbar puncture.
Case report
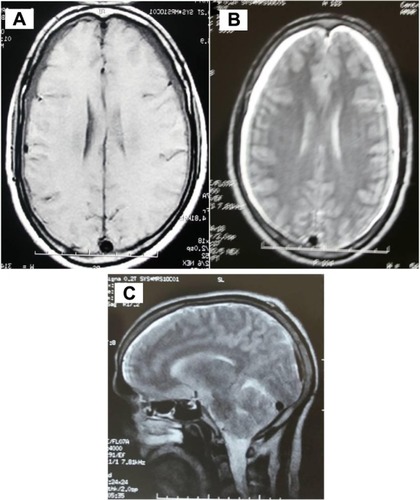
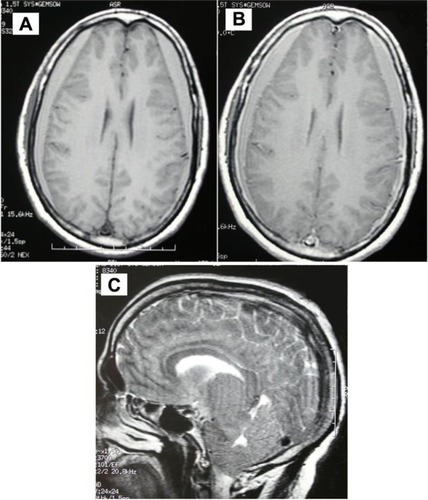
A 34-year-old man without any headache history, cardiovascular risk factor, fever, or antecedent trauma had since September 3, 2010 acute postural headache that occurred within 15 minutes of assuming an upright position; it began as a pain over the vertex, and rapidly became holocephalic, with photophobia, nausea, and vomiting. The headache resolved within 10 minutes of assuming the supine position. The patient did not have aura, visual change, or other neurological symptoms. Clinical examination was normal, and did not found any hyperflexibility of skin or joints. The first cerebral computed tomography scan was normal. A brain MRI with angio-sequences did not show cerebral thrombophlebitis, and was interpreted as normal (). Lumbar puncture was performed, without a measure of cerebrospinal fluid (CSF) pressure, showed hyperproteinorachy at 2 g/L, and six cells with lymphocytosis. The headache became very intense. At admission, clinical examination was normal. Ophthalmological examination did not show any abnormalities. A second brain MRI showed bilateral subdural hematoma with tonsillar descent, simulating Chiari type I malformation (). The patient was treated by surgical drainage of the subdural hematoma and bed rest. The blood patch was not realized. The headache was completely resolved 2 days after surgery. There was no recurrence after 3 years of follow-up.
Discussion
This observation describes a case of postural headache revealing SIH misdiagnosed and complicated by subdural hematoma following lumbar puncture. In the literature, there are many studies describing SIH, specifying clinical, paraclinical, and therapeutic characteristics.Citation2 SIH is caused by single or multiple spinal CSF leaks. The incidence has been estimated at five per 100,000 per year, with a peak around 40 years of age. Women are more affected, but not exclusively, as shown in our case.Citation3 A postural headache is the clinical hallmark of SIH, as seen in this case. It occurs or worsens within 15 minutes after sitting or standing, with at least one of the following: one of neck stiffness, tinnitus, hypacusia, photophobia, or nausea.Citation4 Rarely, this condition could happen with a nonpositional headache preceding a typical orthostatic headache.Citation5 The diagnosis is confirmed by encephalic MRI and axial and sagittal T1 sequences, with intravenous administration of gadolinium showing subdural fluid-collection enhancement of the pachymeninges, engorgement of venous structures, pituitary hyperemia, and sagging of the brain.Citation5,Citation6 Although typical, these radiological features may be missed, leading to misdiagnosis of this condition.Citation7,Citation8
That was the case in this patient, for whom subdural fluid collection was neglected in the first MRI, interpreted as normal (), because it did not include gadolinium-enhanced sequences. This may have contributed to the misdiagnosis in this case, as diffuse pachymeningeal enhancement is a very characteristic sign of intracranial hypotension. In some patients with SIH, herniation of the cerebellum and medulla through the foramen magnum occurs simulating Chiari I malformation, similar to this patient’s condition. Other investigations (spinal MRI, radioisotope cisternography, and computed tomographic myelography) are indicated to identify the site of CSF leak.Citation5 For financial reasons, these explorations were not performed in this case.
CSF constituents are usually normal, although a high protein concentration and lymphocytic pleocytosis may be seen, similar to our case, which is probably due to increased permeability of dilated meningeal blood vessels and a decrease of CSF flow in the lumbar subarachnoid space.Citation9 In our case, lumbar puncture could be a plausible explanation of bilateral subdural hematoma, which required emergency surgery. Many cases of SIH resolve spontaneously and do not require any specific therapy.Citation5 Conservative measures consist of bed rest, oral hydration, generous caffeine intake, and use of an abdominal binder.Citation5
The mainstay of treatment is the injection of antilogous blood into the spinal epidural space, the so-called epidural blood patch.Citation10,Citation11 Percutaneous placement of fibrin sealant and surgical CSF leak repair can also be performed, but outcomes have been poorly studied.
Conclusion
SIH is a unique medical syndrome that can be revealed by orthostatic headache and which has established criteria in the International Classification of Headache Disorders. If not diagnosed, it may lead to unnecessary exhaustive investigations and treatments. The prognosis is excellent if precociously and properly diagnosed.
Disclosure
The authors report no conflicts of interest in this work.
References
- PaldinoMMogilnerAYTennerMSIntracranial hypotension syndrome: a comprehensive reviewNeurosurg Focus200315ECP2
- RouxXDe GreslanTSallansonnet-FromentMSyndrome d’hypotension spontanée du liquide cérébrospinal. Revue de la littérature à propos d’un cas [Spontaneous low cerebrospinal fluid pressure syndrome. A case report and literature review]La Rev Med Interne200829652657 French
- SchievinkWIMisdiagnosis of spontaneous intracranial hypotensionArch Neurol20036017131718
- Headache Classification Subcommittee of the International Headache SocietyThe International Classification of Headache Disorders2nd edCephalalgia200424Suppl 11160
- SchievinkWISpontaneous spinal cerebrospinal fluid leaks and intracranial hypotensionJAMA200629522862296
- DillonWPFishmanRASome lessons learned about the diagnosis and treatment of spontaneous intracranial hypotensionAJNR Am J Neuroradiol19981910011002
- SainaniNILawandeMAPungavkarSADesaiMPatkarDPMohantyPHSpontaneous intracranial hypotension: a study of six cases with MR findings and literature reviewAustralas Radiol200650419423
- TrappoliniMClariceAScorzaAA case of spontaneous intracranial hypotension with typical magnetic resonance imagesJ Headache Pain200674446
- MokriBSpontaneous low cerebrospinal pressure/volume headachesCurr Neurol Neurosci Rep2004411712414984683
- SencakovaDMokriBMcClellandRLThe efficacy of epidural blood patch in spontaneous CSF leaksNeurology20015719211923
- BerroirSLoiselBDucrosAEarly epidural blood patch in spontaneous intracranial hypotensionNeurology20046319501951