Abstract
Introduction
Prior research has demonstrated that platelet count and inflammation are dominant contributors to hypercoagulability. Our objective is to determine whether elevated platelet count and systemic inflammatory response syndrome (SIRS) have an association with the development of venous thromboembolism (VTE) in hospitalized patients with a high clinical index of suspicion for thromboembolic disease.
Methods
We performed a retrospective medical record review of 844 medical and surgical patients with suspected VTE hospitalized from July 2012 to May 2013 who underwent screening by venous duplex and computed tomography pulmonary angiogram. For our purposes, thrombocytosis was arbitrarily defined as platelet count ≥250×109/L.
Results
Venous thromboembolic disease was detected in 229 patients (25.9%). Thrombocytosis was present in 389 patients (44%) and SIRS was present in 203 patients (23%) around the time of imaging. Thrombocytosis and SIRS were positively correlated with VTE (P<0.001). There was no correlation between thrombocytosis and SIRS. Multivariate analysis revealed that SIRS (odds ratio 1.91, 95% confidence interval 1.36–2.68, P<0.001) and thrombocytosis (odds ration 1.67, 95% confidence interval 1.23–2.26, P=0.001) were independently associated with VTE.
Conclusion
Patients at high risk for VTE should be routinely assessed for thrombocytosis (≥250×109/L) and SIRS; if either is present, consideration for empiric anticoagulation should be given while diagnostic imaging is undertaken.
Keywords:
Introduction
In the United States, venous thromboembolism (VTE) affects approximately 900,000 people annually.Citation1 Roughly 300,000 cases are fatal; the 600,000 nonfatal cases result in multiple hospitalizations or extended inpatient stays costing $5.8–$7.8 billion.Citation1,Citation2
Virchow’s triad states that the development of thrombosis can be attributed to the presence of one or more of the following: endothelial injury, stasis of blood flow, and hypercoagulability.Citation3 Multiple studies over the past century have lent credence to Virchow’s theory and identified several modifiable and static risk factors for VTE.Citation4 Prior research demonstrated that platelet count and inflammation are dominant contributors to hypercoagulability.Citation5,Citation6 Platelet count is strongly associated with clot strength and elevated platelet counts increase fibrin production and thrombus generation.Citation6
Inflammatory states are highly prevalent amongst hospitalized patients. Systemic inflammatory response syndrome (SIRS) is present in one-third of the inpatient population and over 50% of all patients admitted to the intensive care unit.Citation7 Evidence regarding platelet count and systemic inflammation in relation to the development of VTE is sparse. Our objective was to determine whether elevated platelet count and SIRS have an association with the development of VTE in hospitalized patients with a high clinical index of suspicion for thromboembolic disease.
Methods
We performed a retrospective medical record review of all medical and surgical patients with clinically suspected VTE admitted to a 448-bed urban level-I trauma center over the course of July 2012 to May 2013 who underwent screening by both venous duplex and computed tomography pulmonary angiogram (CTPA). Institutional review board exemption was obtained prior to data collection and incomplete charts were excluded from analysis.
Data was collected on vital signs, hematology and coagulation profiles, and official imaging reports. The presence or absence of SIRS was determined by white blood cell count, heart rate, respiratory rate, and temperature collected as close to the time of venous duplex as possible. When duplicate imaging was ordered, the results of the first examination were used for data analysis. For our purposes, thrombocytosis was arbitrarily defined as platelet count greater than or equal to 250×109/L.
The sample was stratified by presence or absence of VTE as determined by official imaging reports. Statistical calculations were performed by chi-square analyses and Student’s t-test for categorical and continuous variables, respectively. A bivariate model was also built to calculate odds ratios (OR) with 95% confidence intervals (CI) of thrombocytosis and presence of SIRS.
Results
Our final sample consisted of 884 patients. Venous thromboembolic disease was detected by duplex or CTPA in 229 patients (25.9%). Thrombocytosis was present in 389 patients (44%) and SIRS was present in 203 patients (23%) around the time of imaging.
Mean white blood cell count (15.8±1.4×109/L versus 8.7±0.3×109/L), mean heart rate (98.1±2.1 versus 77.5±1.1 bpm), and mean respiratory rate (21.2±0.5 versus 18.9±0.2 bpm) were significantly higher in patients with SIRS (P<0.001, ). Mean temperature was equivalent across the groups with and without SIRS. Mean platelet count was noted to be significantly higher in patients with SIRS (278.7±21.6×109/L versus 247.4±8.2×109/L, P=0.001).
Table 1 Characteristics of patients with and without SIRS
Of the entire population, 655 patients (74.1%) were found to be negative for VTE (). Thrombocytosis was positively associated with venous thromboembolic disease (P<0.001, ) and mean platelet count was significantly higher in patients with VTE (291.5±18.8×109/L versus 241.7±8.5×109/L, P<0.001). The presence of SIRS was also positively associated with development of VTE (P<0.001).
Figure 1 Comparison of subjects with and without VTE as determined by venous duplex and CTPA.
Abbreviations: CTPA, computed tomography pulmonary angiogram; SIRS, systemic inflammatory response syndrome; VTE, venous thromboembolism.
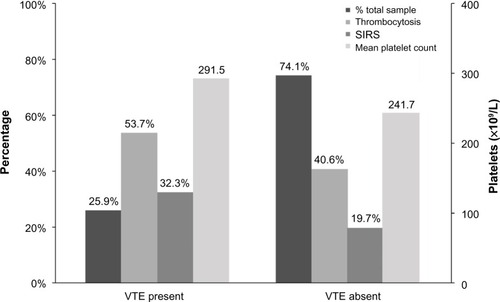
Table 2 Characteristics of patients with and without VTE
Bivariate analysis revealed that SIRS (OR 1.91, 95% CI 1.36–2.68, P<0.001) and thrombocytosis (OR 1.67, 95% CI 1.23–2.26, P=0.001) were associated with venous thromboembolic disease.
Discussion
VTE is a major public health issue. While once considered a primarily postoperative or malignancy-related complication, multiple investigations into the pathophysiology, prevention, and treatment of VTE have led to increased clinical awareness over the past 2 decades.Citation1,Citation4 Most health care institutions currently utilize protocol checklists to be completed on admission to ensure preventive measures for VTE. Recent recommendations by the American College of Chest Physicians state that patients hospitalized for acute medical illness, trauma, or major surgical procedures should receive VTE prophylaxis with low-molecular-weight heparin, low-dose unfractionated heparin, or fondaparinux.Citation8 There has been much debate regarding the appropriate timing, method, and dosage of pharmacoprophylaxis; however, it has been established that hospitalized patients are at significantly increased risk of VTE compared to the general population.Citation1
SIRS is present in more than 30% of all hospitalized patients.Citation7 The association between SIRS/sepsis and disseminated intravascular coagulation has been extensively studiedCitation5,Citation9,Citation10 yet there is little information on the link between systemic inflammation and VTE. A systematic review by Fox and Kahn found no correlation between serum inflammatory markers and VTE.Citation11 It has been postulated that the relationship between inflammation and coagulation is bidirectional,Citation5 although there is no definitive evidence supporting a linear relationship suggesting inflammatory response is predictive of VTE. We hypothesize that systemic inflammation places patients at increased risk for VTE, the occurrence of which potentiates the inflammatory response.
Platelets are recognized as dominant contributors to overall clot strength. Serum platelet count and fibrinogen levels are important factors in the development of thrombosis.Citation12 Meta-analyses published within the past 20 years reported that antiplatelet therapy significantly reduces the occurrence of VTE; antiplatelet VTE prophylaxis with low-dose aspirin was studied in orthopedic patients and was found to proportionally reduce the incidence of pulmonary embolisms and symptomatic deep vein thrombosis by 43% and 29%, respectively.Citation13–Citation15 Aspirin has also been found to reduce the incidence of recurrent VTE in patients with first-time unprovoked VTE without an apparent increase in the risk of major bleeding.Citation16
This paper focused on examining the potential association between platelet count, systemic inflammation, and VTE in hospitalized patients already clinically suspected of suffering from VTE who were screened by both venous duplex and CTPA. We found that thrombocytosis (platelet count ≥250×109/L) and SIRS were positively associated with imaging-confirmed VTE and mean platelet count was significantly higher in patients with VTE.
Treatment for VTE consists of rapid initial anticoagulation and long-term maintenance anticoagulation.Citation17 Rapid anticoagulation is initiated to prevent further extension of VTE and possibly fatal complications. Based on our findings, we believe that screening for thrombocytosis and SIRS while pending confirmatory imaging may help identify high-risk patients necessitating immediate anticoagulation.
Limitations
While this study has several strengths, the most prominent of which was our sample size, it also faced limitations associated with its retrospective single-center design. Our primary focus was not on initial prophylaxis; we chose to evaluate patients clinically suspected of venous thromboembolic disease for the possible association between thrombocytosis, SIRS, and imaging-confirmed presence of VTE. Laboratory results and vital signs were collected as close to time of imaging as possible but there is no way to determine when the patient started manifesting symptoms. Our bivariate model did not include known risk factors for VTE such as age, sex, past medical history, and admission diagnosis since this data was not collected on initial review. However, our sample consisted of all hospitalized patients clinically suspected of having venous thromboembolic disease who had undergone screening by both venous duplex and CTPA; it is likely safe to assume the study population would be considered high-risk.
Our findings suggest that thrombocytosis and SIRS in patients clinically suspected of VTE are suggestive of VTE occurrence. Further large-scale prospective studies are necessary to determine whether our findings can be extrapolated to the inpatient population.
Conclusion
Patients at high risk for VTE should be assessed for thrombocytosis (≥250×109/L) and SIRS; if either is present, diagnostic imaging should be undertaken in a timely fashion.
Disclosure
The authors report no conflicts of interest in this work.
References
- HeitJAThe epidemiology of venous thromboembolism in the communityArterioscler Thromb Vasc Biol20082837037218296591
- SpyropoulosACLinJDirect medical costs of venous thromboembolism and subsequent hospital readmission rates: an administrative claims analysis from 30 managed care organizationsJ Manag Care Pharm20071347548617672809
- KumarDRHanlinERGlurichIMazzaJJYaleSHVirchow’s contribution to the understanding of thrombosis and cellular biologyClin Med Res201083–416817220739582
- AndersonFAJrSpencerFARisk factors for venous thromboembolismCirculation2003107I9I1612814980
- LeviMvan der PollTBüllerHRBidirectional relation between inflammation and coagulationCirculation20041092698270415184294
- HarrJNMooreEEChinTLPlatelets are dominant contributors to hypercoagulability after injuryJ Trauma Acute Care Surg201374756762 discussion 762–76523425732
- Brun-BuissonCThe epidemiology of the systemic inflammatory responseIntensive Care Med200026Suppl 1S64S7410786961
- GuyattGHAkiEACrowtherMGuttermanDDSchuünemannHJAmerican College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis PanelExecutive summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest2012141Suppl 27S47S22315257
- LeviMDisseminated intravascular coagulation or extended intravascular coagulation in massive pulmonary embolismJ Thromb Haemost201081475147620412432
- IbaTGandoSMurataAPredicting the severity of systemic inflammatory response syndrome (SIRS)-associated coagulopathy with hemostatic molecular markers and vascular endothelial injury markersJ Trauma20076351093109817993956
- FoxEAKahnSRThe relationship between inflammation and venous thrombosis. A systematic review of clinical studiesThromb Haemost20059436236516113826
- KornblithLZKutcherMERedickBJCalfeeCSVilardiRFCohenMJFibrinogen and platelet contributions to clot formation: Implications for trauma resuscitation and thromboprophylaxisJ Trauma Acute Care Surg2014762255256 discussion 262–26324458031
- ClagettGPAndersonFAJrGeertsWPrevention of venous thromboembolismChest1998114Suppl 5531S560S9822062
- No authors listedCollaborative overview of randomized trials of antiplatelet therapy – III: Reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. Antiplatelet Trialists’ CollaborationBMJ19943082352468054013
- CollinsRBaigentCSandercockPPetoRAntiplatelet therapy for thromboprophylaxis: the need for careful consideration of the evidence from randomized trials. Antiplatelet Trialists’ CollaborationBMJ1994309121512177987156
- BecattiniCAgnelliGSchenoneAAspirin for preventing the recurrence of venous thromboembolismN Engl J Med2012366211959196722621626
- GrossPLWeitzJINew anticoagulants for treatment of venous thromboembolismArterioscler Thromb Vasc Biol200828338038618296593
