Abstract
Chromobacterium violaceum, a proteobacterium, is a facultative anaerobe, which is generally present as the normal flora of water and soil in tropical and subtropical regions. The infection due to Chromobacterium violaceum is rare but mostly fatal. It is responsible for causing fatal cases of septicemia, visceral abscesses, skin and soft tissue infections, meningitis, diarrhea, and rarely urinary tract infection. The bacteria has high propensity to spread causing sepsis. Delayed proper treatment due to limited awareness related to the C. violaceum infection is responsible for the high mortality rate. Here, we describe a rare case of urinary tract infection by C. violaceum in a chronic kidney disease patient, which was managed with timely proper antimicrobial therapy as per the culture sensitivity report.
Introduction
Chromobacterium violaceum is a Gram-negative, facultative anaerobic, oxidase positive, motile bacillus.Citation1 It is ubiquitously present in the water and soil of tropical and subtropical regions. C. violaceum was first identified in 1881, and its pathogenic ability was first described by Woolley in 1905 in a fatal infection of a buffalo.Citation2 It is well-known for producing violacein, a violet colored pigment with antioxidant property.Citation3 C. violaceum rarely infects humans causing skin lesions, sepsis, and liver abscesses that may be fatal.Citation4 Other manifestations are soft tissue infections, urinary tract infections, and diarrhea. The first human case of C. violaceum infection was reported from Malaysia in 1927. Worldwide only 150 cases have been reported, mainly from tropics, including eight cases from neighboring country India.Citation5 Here, we report a case of urinary tract infection caused by C. violaceum in a kidney patient of age 70 years. This is the first case of C. violaceum infection reported from Nepal.
Case report
Written informed consent was obtained from the patient for publication of this case report. A 70-year-old male chronic kidney patient attended the outpatient department of a tertiary care hospital in Kathmandu, Nepal, in November, 2014, with chief complaints of burning micturition, high-grade fever (>102°F) with chills since 10 days, and pain in lower abdomen. The patient had a history of simple nephrectomy (12 years before) and a recent history of recurrent urinary tract infection. Four weeks ago, the patient was treated for urinary tract infection caused by Escherichia coli. A surgery was done approximately 3 weeks ago for urinary tract obstruction followed by urinary catheterization.
The patient was empirically treated with ciprofloxacin for urinary tract infection after suggesting necessary laboratory investigation. The dose for ciprofloxacin was adjusted according to the age and the renal condition of the patient. Laboratory findings showed raised total leukocyte count (15,330 cells/mm3) with neutrophilia (78.5%), raised creatinine (2.1 mg/dL), decreased sodium (132 mmol/L), and decreased hemoglobin (13 g%). There were plenty of pus cells per low power field with bacteriuria in routine examination of urine.
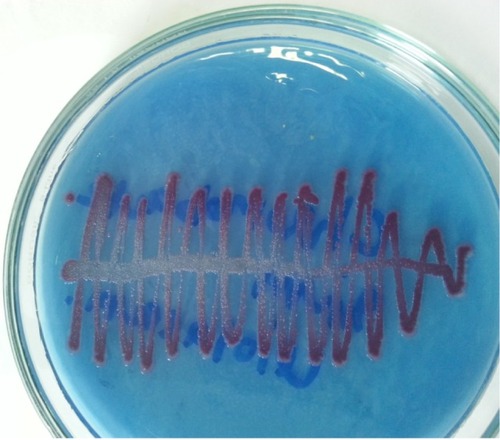
The mid stream urine culture plated on cystine lactose electrolyte deficient agar as shown in below showed significant growth of single type of nonlactose fermenting colonies after overnight aerobic incubation at 37°C. The bacterial colonies grown were around 2–3 mm in diameter with distinctly purple nondiffusible pigment, round, convex with entire margin, opaque, moist, easily emulsifiable, smooth in texture, and dull in appearance. From the colonies grown, the Gram’s stain and biochemical tests were performed. The bacterium was Gram-negative motile rod, catalase and oxidase producing, nitrate reducing. It did not produce indole and urease but utilized citrate. It was nonlactose fermenting in triple sugar iron agar. It fermented glucose, trehalose, n-acetylglucosamine, and gluconate but did not ferment l-arabinose, d-galactose, or d-maltose and decarboxylated arginine. With the help of these biochemical properties, colony characteristics, and pigment production, it was identified as C. violaceum.
Figure 1 Growth of Chromobacterium violaceum in CLED agar.
Antimicrobial susceptibility testing was performed by Kirby Bauer’s disk diffusion technique. The organism was found to be susceptible toward cotrimoxazole, gentamicin, ciprofloxacin, norfloxacin, imipenem, ceftriaxone and resistant toward amoxicillin and clavulanic acid, and nitrofurantoin. Since the organism was found to be sensitive toward ciprofloxacin, the initial antibiotic was continued for 1 week. Blood culture was done to rule out blood stream infection due to the capacity of the organism for easy dissemination, and the blood culture was negative. After 1 week of the antibiotic administration, the clinical symptoms subsided significantly and the repeated urine culture was negative.
Discussion
Due to rare infections caused in human by this organism, the awareness of the diseases by C. violaceum is limited.Citation6 In general, the illness is followed by contaminated inoculation site, which leads to localized disease, regional lymphadenopathy, then hematogenous spread to visceral organs.Citation7 It may be responsible for pneumonia, gastrointestinal infection, localized cutaneous lesions, localized or metastatic abscesses, osteomyelitis, meningitis, peritonitis, brain abscess, endocarditis, hemophagocytic syndrome, respiratory distress syndrome, and fulminant sepsis.Citation8 Rapid progression to sepsis and multiorgan dysfunction with high mortality rate is a characteristic of C. violaceum infection. Urinary tract infection caused by this organism is rarely reported as in 81-year-old male chronic kidney disease patientCitation9 and 19-year healthy male. It is considered as a bacterium of low virulence causing infection in immunocompromised patients.Citation10 In our case also, the patient was immunocompromised chronic kidney disease patient.
Being mesophilic and ubiquitous in tropical and subtropical areas, it causes infection in summer months in these areas. In addition, this microorganism may not be confined to a narrow geographic range (between latitudes 35°N and 35°S) as previously considered because of the effect of global climate change.Citation3,Citation11,Citation12 The usual route of the bacteria into the body is through skin trauma or ingestion of contaminated water and seafood. Unusual routes include infection after scuba diving or near drowning, after breast surgery, and appendicectomy.Citation10 In our case, the patient had undergone surgery for urinary tract obstruction followed by catheterization. So these may be the causes for the bacterium to get into the urinary tract of the patient. Although antimicrobial susceptibility data on C. violaceum remain very limited because this pathogen is rarely isolated from clinical specimens, results of susceptibility testing vary in different clinical settings.Citation8 C. violaceum is usually sensitive to fluoroquinolones, cotrimoxazole, imipenem, gentamicin,Citation13 and extremely resistant to penicillins and cephalosporins.Citation10 In our study also, the organism was found to be sensitive to cotrimoxazole, gentamicin, ciprofloxacin, norfloxacin, imipenem and resistant toward amoxicillin and clavulanic acid.
If the accurate diagnosis is not established promptly and the required treatment is not given in time, the complication may develop and the outcome may be fatal. However, in our case, the patient got well without developing any complications due to timely identification of the causative agent and prompt start of proper antimicrobial therapy as suggested by the urine culture and sensitivity report.
Conclusion
C. violaceum infection is an emerging infection. If not treated appropriately, it may develop into fatal sepsis. So, the clinician should be aware of this infection and its effective treatment. Urinary tract infection is rarely caused by C. violaceum, but the prognosis may be bad if not managed promptly. So early diagnosis with optimal and adequate antimicrobial therapy for adequate duration is the key to successful treatment.
Disclosure
The authors report no conflicts of interest in this work.
References
- CampbellJILanNPQuiPTDung leTFarrarJJBakerSA successful antimicrobial regime for Chromobacterium violaceum induced BacteraemiaBMC Infect Dis201313423286235
- WoolleyPGBacillus violaceous manila, a pathogenic organismBull Johns Hopkins Hosp1905168993
- PonteRJenkinsSGFatal Chromobacterium violaceum infections associated with exposure to stagnant watersPediatr Infect Dis J19921175835861528650
- SneathPHWhelanJPBhagwan SinghREdwardsDFatal infection by Chromobacterium violaceumLancet1953265678027627713085740
- RayPSharmaJMarakRSChromobacterium violaceum septicaemia from North IndiaIndian J Med Res2004120652352615654137
- ChattopadhyayAKumarVBhatNRaoPChromobacterium violaceum infection: a rare but frequently fatal diseaseJ Pediatr Surg200237110811011781998
- FisherRGGruberWCBoyceTGMiscellaneous non-enterobacteriaceae fermentative bacilliFeiginRDCherryJDDemmlerGJKaplanSLTextbook of Pediatric Infectious Diseases5th edPhiladelphiaSaunders200415391540
- YangCHLiYHChromobacterium violaceum infection: a clinical review of an important but neglected infectionJ Chin Med Assoc2011741043544122036134
- MaTShiWChengJChromobacterium violaceum infection in China: three case reports and literature reviewsAfr J Microbiol Res201152030963102
- SwainBOttaSSahuKKPandaKRoutSUrinary tract infection by Chromobacterium violaceumJ Clin Diagn Res20148812
- KoburgerJAMaySOIsolation of Chromobacterium spp. from foods, soil, and waterAppl Environ Microbiol1982446146314657159087
- ByamukamaDFarnleitnerAHKansiimeFManafiMBurtscherMMachRLContrasting occurrence of Chromobacterium violaceum in tropical drinking water springs of UgandaJ Water Heath200533229238
- AldridgeKEValainisGTSandersCVComparison of the in vitro activity of ciprofloxacin and 24 other antimicrobial agents against clinical strains of Chromobacterium violaceumDiagn Microbiol Infect Dis198810131393168426
