?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
One of the main problems associated with the development of osteochondral reparative materials is that the accurate imitation of the structure of the natural osteochondral tissue and fabrication of a suitable scaffold material for osteochondral repair are difficult. The long-term outcomes of single- or bilayered scaffolds are often unsatisfactory because of the absence of a progressive osteochondral structure. Therefore, only scaffolds with gradient pore sizes are suitable for osteochondral repair to achieve better proliferation and differentiation of the stem cells into osteochondral tissues to complete the repair of defects.
Methods
A silk fibroin (SF) solution, chitosan (CS) solution, and nano-hydroxyapatite (nHA) suspension were mixed at the same weight fraction to obtain osteochondral scaffolds with gradient pore diameters by centrifugation, freeze-drying, and chemical cross-linking.
Results
The scaffolds prepared in this study are confirmed to have a progressive structure starting from the cartilage layer to bone layer, similar to that of the normal osteochondral tissues. The prepared scaffolds are cylindrical in shape and have high internal porosity. The structure consists of regular and highly interconnected pores with a progressively increasing pore distribution as well as a progressively changing pore diameter. The scaffold strongly absorbs water, and has a suitable degradation rate, sufficient space for cell growth and proliferation, and good resistance to compression. Thus, the scaffold can provide sufficient nutrients and space for cell growth, proliferation, and migration. Further, bone marrow mesenchymal stem cells seeded onto the scaffold closely attach to the scaffold and stably grow and proliferate, indicating that the scaffold has good biocompatibility with no cytotoxicity.
Conclusion
In brief, the physical properties and biocompatibility of our scaffolds fully comply with the requirements of scaffold materials required for osteochondral tissue engineering, and they are expected to become a new type of scaffolds with gradient pore sizes for osteochondral repair.
Introduction
Sports-related injuries, accidental injuries, and congenital diseases result in various inevitable osteoarticular injuries. Osteochondral defects often occur in osteoarticular injuries involving smooth cartilage and subchondral bone. Because of the limited self-healing ability of osteochondral tissues, especially the large-area osteochondral defects, the injured bone and joint tend to undergo chronic degeneration. Therefore, surgical intervention is often necessary for intra-articular osteochondral defects, and the treatment plan depends on various factors such as the age, diameter, and depth of the lesion.Citation1 Autologous osteochondral transplantation is currently recognized as the clinical gold standard for the treatment of osteochondral defects. However, this technique has many inherent limitations, such as the requirement of a high surgical technique, complicated operating procedures, shortage of graft source, less quantity of grafts, poor matching of graft and host cartilage congruency, sequelae of the graft donor site, incomplete graft–host integration, and degeneration of the transplanted graft.Citation1,Citation2 Therefore, osteochondral tissue engineering has attracted increasing attention. A variety of factors including the scaffold materials, stem cells, and signal factors have been studied for osteochondral repairCitation3 to develop appropriate strategies for the regeneration of damaged cartilage and subchondral bone tissues.
One of the main difficulties in the development of osteochondral biomaterials is to accurately imitate the structure of the natural osteochondral tissue. As previously reported, a scaffold with a single pore diameter has been implanted as a support material in the area of an osteochondral defect. Unfortunately, the long-term results are often unsatisfactory because of a lack of progressive osteochondral structure starting from the cartilage layer to bone layer in the regenerated tissues. This impedes normal metabolism and biomechanical support of the articular cartilage, and causes cell degeneration in the central region of the defect, eventually leading to fragmentation and collapse of the articular cartilage.Citation4,Citation5 Therefore, the new concept of constructing bilayered scaffolds for osteochondral tissue engineering has emerged for repairing osteochondral defects. Some scholars have separately constructed cartilage scaffolds and bone scaffolds and then integrated these two kinds of scaffolds using stitches,Citation6,Citation7 a bio-sealant, or a bio-glue.Citation8–Citation10 There is consequently a clear interface between the bone layer and cartilage layer, and the cells cannot penetrate the interface to form a calcified cartilage, resulting in an unstable bone–cartilage interface. New bone tissues are likely to grow into the cartilage area of the osteochondral defectCitation11 or long-term stratification may appear. With the advancement in the bilayered scaffold research, some inherent flaws in the osteochondral repair have become more obvious; it has come to light that a distinct boundary formed between the cartilage layer and bone layer causes uneven differentiation of the stem cells in the cartilage–bone junction area or produces a distinct band zone,Citation12,Citation13 eventually leading to the failure of bone and cartilage integration. Owing to the particularity of the bone and cartilage structures, only an appropriate osteochondral scaffold can facilitate the proliferation and differentiation of the seed cells into osteochondral tissue in vivo, and thereby complete the osteochondral repair.
Numerous studies have shown that silk fibroin (SF), chitosan (CS), and nano-hydroxyapatite (nHA) have no cytotoxic side-effects and have no special odor. All three materials have good biological and physicochemical properties, and they can be used as good scaffold materials. In our previous study, we confirmed that bone scaffolds based on SF-CSCitation14 and SF-CS-nHA compositesCitation15 with a single pore diameter were successfully prepared by vacuum freeze-drying and chemical cross-linking methods, the SF/CS scaffolds produced with a ratio of 1:1 of SF solution and CS solution, and SF-CS-nHA scaffolds produced with a ratio of 1:1:1 of SF solution, CS solution, and nHA suspension showed the best performance. After extensive investigations, SF-CS and SF-CS-nHA scaffolds were confirmed to have good histocompatibility with no cytotoxicity,Citation16,Citation17 and they could better repair rabbit knee articular cartilage defectsCitation14 and large-segmental radial bone defects.Citation18,Citation19 Herein, inspired by the successful results of SF-CS-nHA scaffolds with a single pore diameter in the reparation of cartilage and bone defects, we combined the freeze-drying method with a centrifugation method to fabricate SF-CS-nHA scaffolds with gradient pore diameter. The physical and biological properties of the scaffolds were evaluated to select a biomimetic composite scaffold that shows optimal performance in the repair of osteochondral defects.
Materials and methods
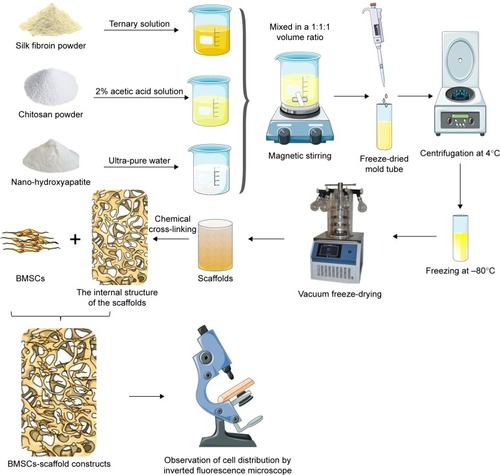
A series of experiments were carried out in the early stage to prepare osteochondral scaffolds with gradient pore diameters by varying different parameters including the optimal ratio of the scaffold raw materials, freezing method, methods to develop pores, and the cross-linking. The finalized optimal scheme is shown in .
Preparation of scaffolds
First, a series of solutions of SF and CS, and suspensions of nHA were prepared at three different concentrations, as follows:
SF solution
SF (1 g) (Huzhou Xintiansi Biotechnology Co., Ltd., Zhejiang, China) was immersed in a ternary mixture (10 mL) consisting of CaCl2 (MACKLIN, Shanghai, China), H2O (Ultrapure Water Preparation System, EMD Millipore, Billerica, MA, USA), and ethanol (Tianjin Kemiou Chemical Reagent Co., Ltd., Tianjin, China) at a molar ratio of 1:8:2, and stirred at 80°C using a C-MAG HS4 magnetic heating stirrer (300 r/min; IKA, Staufen, Germany) for 1 hour. After the dissolution of SF, the solution was transferred to a dialysis bag with a molecular weight cutoff of 3500 D (Biosharp, Anhui, China), dialyzed for 2 days against tap water and 1 day against deionized water. The effect of dialysis was detected using a 5% Na2CO3 solution. Then, an SF solution was prepared after filtration, 10 mL filtered SF solution were taken, placed in a beaker, dried at 60°C for 72 hours, and then weighed. W1 is the weight of SF solution and beaker after drying, M0 is the weight of the beaker, and V is the volume of SF solution. The mass fraction of SF solution was calculated using the following formula: mass fraction =(M1−M0)/V×100%. The SF solution was thereafter concentrated or diluted to a concentration of 2, 3, or 4%, and stored at 4°C.
CS solution
CS (degree of deacetylation >95%, viscosity =100–200 MPa.s; Aladdin, Shanghai, China) was mixed with 2% acetic acid (purity >99.9%; Aladdin), and magnetically stirred at a speed of 300 r/min at 100°C for 1 hour until its complete dissolution. 10 mL filtered CF solution were taken, placed in a beaker, dried at 60°C for 72 hours, and then weighed. W1 is the weight of CF solution and beaker after drying, M0 is the weight of the beaker, and V is the volume of CF solution. The mass fraction of CF solution was calculated using the following formula: mass fraction =(M1−M0)/V×100%. The prepared CS solutions were concentrated or diluted to concentrations of 2, 3, and 4%, and stored at 4°C until use.
nHA suspension
The nHA (biomedical grade, 98%, <0.2 μm; Aladdin) was mixed in ultrapure water and magnetically stirred at room temperature to obtain suspensions with concentrations of 2, 3, and 4%. The nHA suspension was prepared freshly before use.
Preparation of the scaffold
Three different mixtures with 2, 3, and 4% of each of the constituents were prepared by thoroughly mixing the SF solution, CS solution, and nHA suspension with the same given concentration at a volume ratio of 1:1:1 via magnetic stirring. Then, the mixtures were pipetted out into prepared mold grooves (1.8-mL standable extorsion cryopreservation tubes, Corning Incorporated, Corning, NY, USA) and centrifuged (500 r/min) at 4°C for 5 minutes using a cryogenic centrifuge (centrifuge 5424R, Eppendorf, Hamburg, Germany), and frozen in a refrigerator at −80°C (DW86L630, AUCMA, China) for 24 hours. Then, the frozen scaffolds were quickly taken out and sealed with parafilm (Parafilm, Neenah, WI, USA), pores were made in the sealing film using a 5-mL sterile syringe needle (22G, outer diameter 0.7 mm, inner diameter 0.4 mm, Chengdu Xinjin Shifeng Medical Apparatus & Instrument Co., Ltd, Chengdu, China) for breathability, and for preventing failure, displacement of scaffold components during vacuum freeze-drying. The scaffolds were then shaped into cylinders in a vacuum dryer (Thermo Fisher Scientific, Waltham, MA, USA) for 24 hours and the dried scaffolds were immersed in a solution containing 75% methanol (Tianjin Kemiou Chemical Reagent Co., Ltd.) and 1 mol/L NaOH (≥98.0%; Aladdin) at a volume ratio of 1:1, and allowed to cross-link at 4°C for 24 hours. Subsequently, the scaffolds were ultrasonically cleaned with ultra-pure water in an ultrasonic cleaning instrument (Kunshan Ultrasonic Instruments Co., Ltd., Kunshan, China) three times, for 5 minutes each time, and dried under vacuum for another 24 hours for second shaping. The dried scaffolds were subsequently immersed in a cross-linking agent containing 50 mmol/L of 1-ethyl-(3-dimethylaminopropyl) carbodiimide hydrochloride (EDC, 98%; Aladdin) and 20 mmol/L of N-hydroxysuccinimide (NHS, 98%; Aladdin) and cross-linked at 4°C for 24 hours. The scaffolds were thereafter ultrasonically cleaned (thrice) and vacuum-dried for 24 hours for final shaping. The so-prepared scaffolds were collected, sealed, and stored in a refrigerator at 4°C until use. The process of preparation is shown in .
Evaluation of the physical properties of the scaffold
Measurement of the scaffold size
The diameter and height of the scaffold were measured using an accurate digital caliper (accuracy 0.01 mm; Aladdin).
Determination of the porosity of the scaffold
The porosity of the scaffold was determined by a modified liquid displacement method. The scaffold was immersed in a 5-mL measuring barrel containing ethanol for 10 minutes until the air overflowed completely. The volume of ethanol was measured before and after immersion, and recorded as V1 and V2, respectively. The scaffold was then taken out and the volume of residual ethanol was recorded as V3. The porosity is calculated as follows:
Determination of the water swelling rate
The scaffold was immersed in double-distilled water for 24 hours and taken out. The excess water on the scaffold surface was sucked off with absorbent gauze and the scaffold was weighed as m1. Then, the scaffold was dried and its weight was measured as m2. The water swelling ratio is calculated as follows: Pwater absorption=(m1−m2)/m2*100%.
Determination of the dissolution rate in hot water
The weight of the scaffold was first measured as m1, and it was immersed in 1× phosphate buffered solution (PBS) and continuously shaken at a constant temperature of 37°C. The scaffold was taken out after 1, 2, 3, 4, and 5 weeks, respectively, followed by ultrasonic cleaning (thrice). Thereafter, the scaffold was dried in vacuum and weighed as m2 using an electronic balance (AS220.R2, RADWAG, Radom, Poland). The dissolution rate in hot water is calculated as follows: Pdissolved=(m1−m2)/m2*100%. Then, the dissolution rate was plotted as a function of time, and linear regression analysis was performed to analyze the dissolution rate of the scaffold in hot water with time.
Mechanical testing
The conventional compressive mechanical properties of the scaffold were tested using an Instron 5969 mechanical testing machine (USA) with a preload force of 0.1 N, a load speed of 0.1 N/min, and a loading rate of 2 mm/min. The stress-strain curve was then plotted to evaluate the mechanical properties of the scaffold.
Determination of the water swelling rate of the scaffolds after compression
According to the 2015 report on Chinese nutrition and chronic disease,Citation20 average weights are 66.2 kg for males and 57.3 kg for females. Therefore, the maximum pressure of 66.2 kg (662 N, 10 N/kg) was chosen, the scaffolds were placed vertically, and an Instron 5969 mechanical testing machine (USA) was used to compress the scaffolds. After compression, the scaffolds were taken out and placed into double-distilled water for 24 hours. The excess water on the scaffold surface was sucked off with absorbent gauze, and the scaffold was weighed as m1. Then, the scaffold was dried and its weight was measured as m2. The water swelling ratio of the scaffolds before and after compression was determined using the following equation: Pcompression=(m1−m2)/m2*100%. The recovery ability of the scaffolds after applying compression was measured.
Internal structure of the scaffold and the pore size
The scaffold was cut straight in the middle, and the longitudinal section was coated with Au using an ion sputtering apparatus (E-1010, HITACHI, Tokyo, Japan). A scanning electron microscope (SEM; S-3400N, HITACHI) was used to observe the pore structure and morphology of the scaffold. The scaffold was divided into four layers from top to bottom, the size of 100 pores per layer was counted using SEM analysis software, and the average pore size of each layer was then calculated.
Determination of the biocompatibility of the scaffold
Culture of rat bone marrow mesenchymal stem cells (BMSCs)
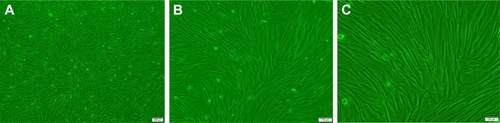
The cryopreserved cells, taken out from liquid nitrogen as reported previouslyCitation21 (), were immediately placed in a constant temperature water bath at 37°C, oscillated, and resuscitated within 1 minute. The mixture was then centrifuged at 1,000 r/min for 5 minutes and the supernatant was discarded. A complete medium [Dulbecco’s Modified Eagle’s Medium/F12 (DMEM/F12; Gibco, Carlsbad, CA, USA)+10% fetal bovine serum (Gibco)+1% streptomycin (HyClone, Logan City, UT, USA)] was used to adjust the cell concentration to 1×105/mL, and the cells were inoculated in a 25-cm2 angled neck cell culture flask with a vent cap (Corning) placed in a 5% CO2 incubator (MCO-18AC, Panasonic, Osaka, Japan) at 37°C. The medium was changed every 2 days. When the cells covered 80% of the bottom of the cell culture flask, the cells were digested with 0.25% trypsin (HyClone). Subsequently, the cell concentration was adjusted to 1×105 cell/mL, and the cells were then seeded in a cell culture flask (5 mL/flask), and culture was continued.
Construction and in vitro culture of BMSC-scaffold complex
According to the physical properties, an appropriate scaffold was selected as a cell carrier. The prepared scaffolds were sterilized with ethylene oxide, pre-treated with sterile 1×PBS, and placed in 24-well culture plates (Corning). Rat BMSCs were inoculated onto the scaffold at a density of 5×104. Rat BMSCs were uniformly seeded at a density of 5×104/scaffold into each layer (L1–L4) of the scaffolds with a pipette (Eppendorf). After 2 hours of culture, a complete medium was added and the BMSC-scaffold complex was placed in the 5% CO2 constant temperature incubator at 37°C. The complete medium was replaced every day.
Cell proliferation in the BMSC-scaffold complex
The BMSC-scaffold complex was taken out after 1, 3, 5, 7, 9, and 11 days of culture and was equally stratified into four layers from top to bottom under aseptic conditions. The layers were transferred into a 96-well plate (Corning) and the cell proliferation in each layer of the BMSC-scaffold complex was evaluated using cell counting kit-8 (CCK-8; Biosharp Biotechnology Co., Ltd., Anhui, China). The complete medium (200 μL) and CCK-8 solution (20 μL) were added into the plate and the complex was incubated at 37°C, in the 5% CO2 constant-temperature incubator for 3 hours and fully shaken with a microplate fast oscillator (QB-9002; Qilinbeier Instrument Manufacturing Co., Ltd., Jiangsu, China). The supernatant (110 μL) was transferred to a fresh 96-well plate and the optical density (OD) of each well was measured at the wavelength of 450 nm using a continuous wavelength plate reader (Synergy HTX, Bio Tek, Winooski, VT, USA) and the cell proliferation curve per layer was plotted.
Cell distribution in the BMSC-scaffold complex
The cell distribution in the BMSC-scaffold complex was observed by nuclear fluorescence staining and SEM. According to the results of the CCK-8 test, the BMSC-scaffold complex prepared over the most optimal time was selected and fixed at room temperature in a 4% paraformaldehyde solution (Biosharp Biotechnology Co., Ltd.) for 30 minutes. The complex was then longitudinally cut into 1–2 mm-thick sections, then the sections were rinsed thrice with 1×PBS, dyed with 4,6-diamidino-2-phenylindole (DAPI, 10 μg/mL, Soleil Biotech Co. Ltd., Beijing, China) for 10 minutes, and photographed using an inverted fluorescence microscope (IX53, Olympus Corporation, Tokyo, Japan) to observe the stratified distribution of the cells in the BMSC-scaffold complex (there were four layers from top to bottom). The sections were rinsed thrice with ultrapure water, transferred to a 2 mL EP tube, and frozen in a −80°C refrigerator for 24 hours. The frozen BMSCs-scaffold complex was then vacuum-dried for another 24 hours and cut longitudinally. The longitudinal sections were coated with Au using the ion sputtering apparatus. The cell morphology and distribution in each layer of BMSCs-scaffold complex were observed by SEM.
Statistical analysis
The data were analyzed using SPSS18.0 and are expressed as mean±standard deviation (SD). Comparison between different groups was performed using t-test, and multi-group comparison was carried out using one-way analysis of variance. A value of P<0.05 is considered significant.
Results
Global observation of the scaffold
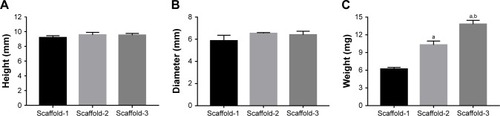
As shown in , the white scaffold is approximately cylindrical with a regular shape. It is extremely light, has no special odor, and has obvious pressure resistance and elasticity. As shown in and , the heights of scaffolds prepared using 2, 3, and 4% solutions of its constituents (hereafter referred to as Scaffold-1, Scaffold-2, and Scaffold-3, respectively) were found to be 9.20±0.26, 9.55±0.35, and 9.53±0.23 mm, respectively, with no significant differences among the groups (F=1.964, P=0.198, n=4). Further, the average diameters of Scaffold-1, Scaffold-2, and Scaffold-3 were estimated to be 5.86±0.50 mm, 6.53±0.07 mm, and 6.40±0.32 mm, respectively; once again, there are no significant differences among the groups (F=4.200, P=0.051, n=4). However, the mean weights of Scaffold-1, Scaffold-2, and Scaffold-3 were found to be 6.21±0.27, 10.29±0.65, and 13.80±0.66 mg, respectively, with the differences among the groups being statistically significant (F=371.673, P=0.000, n=4). These results reveal that only the weight of the scaffold changed over a certain proportion, with no significant changes in the scaffold size, indicating that the scaffold was shaped well.
Table 1 Height, diameter, and weight of the silk fibroin/chitosan/nano-hydroxyapatite scaffolds with gradient pore diameters (mean±SD, n=4)
Porosity of the scaffold
As shown in and , the porosities of Scaffold-1, Scaffold-2, and Scaffold-3 were determined to be 91.30±3.35, 89.50±3.11, and 82.58%±1.47%, respectively. Whereas the porosities of Scaffold-1 and Scaffold-2 (P=0.452, n=4) are not significantly different, the porosity of Scaffold-3 decreased significantly (F=12.154, P4-2=0.001, P4-3=0.004, n=4) in comparison. This indicates that the three kinds of scaffolds are highly porous and the porosity decreases with increasing concentrations of the scaffold.
Table 2 Porosity, hot-water dissolution rate, and water swelling rate of the silk fibroin/chitosan/nano-hydroxyapatite scaffolds with gradient pore diameters (mean±SD, %, n=4)
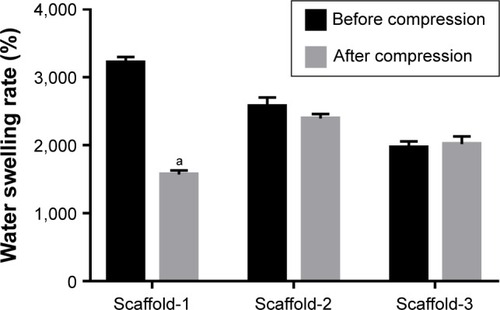
Water swelling rate of the scaffold
As shown in and , the water swelling rates of Scaffold-1, Scaffold-2, and Scaffold-3 are 3,218.53±84.37, 2,573.83±132.51, and 1,969.50%±90.01%, respectively, with the intergroup differences being statistically significant (F=142.829, P=0.000, n=4). This indicates that the three kinds of scaffolds strongly absorb water, and the water swelling rate decreases with increasing concentrations of the scaffold.
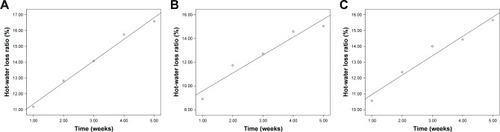
Dissolution rate of the scaffold in hot water
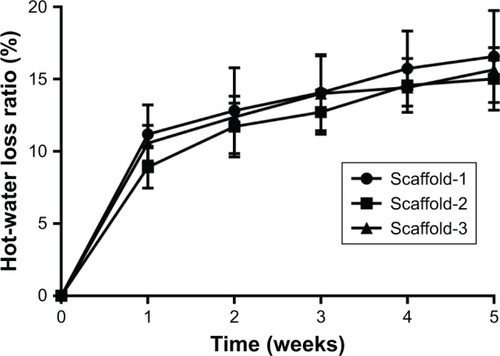
As shown in and , the hot-water dissolution rate of Scaffold-1, Scaffold-2, and Scaffold-3 oscillated at 37°C for 5 continuous weeks is 16.57±3.18, 15.03±2.17, and 15.65%±0.68%, respectively, with no significant difference between the groups (F=0.425, P=0.668, n=4). The hot-water dissolution rate was then plotted as a function of time; the trend of the hot-water dissolution rate shows no significant difference among different groups (). After the first week, the dissolution rate was faster, and tended to be stable from the second to fifth weeks, which might be related to the loss of nHA during the rinsing of the scaffold after the first week. These findings suggest that the degradability of the scaffold is good, and the hot-water dissolution rate of the scaffold is less affected by the material concentration in the range of 2%–4%. Moreover, the hot-water dissolution rate shows a linear relationship with the dissolution time (). Linear regression analysis reveals that the correlation coefficients of the hot-water dissolution rate and the dissolution time of each group are R2%=0.995, R3%=0.970, and R4%=0.980, indicating that there is a high correlation between the hot-water dissolution rate and the dissolution time. The adjusted R2 values of Scaffold-1, Scaffold-2, and Scaffold-3 are 0.990, 0.921, and 0.947, respectively, indicating that the dissolution time could be used to predict the hot-water dissolution rate of the scaffold in a certain range. All the P-values are less than 0.05, indicating a statistically significant regression relationship between the hot-water dissolution rate and the dissolution time. Therefore, the one-way regression equations relating the hot-water dissolution rate and the dissolution time of the scaffold are, Y2%=1.367X2%+9.979, Y3%=1.509X3%+8.067, and Y4%=1.222X4%+9.739 (unit: %). When Y=100%, X2%=65.85, X3%=60.92, X4%=73.86, that is, the three scaffolds can be completely dissolved in vitro within 65.85, 60.92, and 73.86 weeks, respectively.
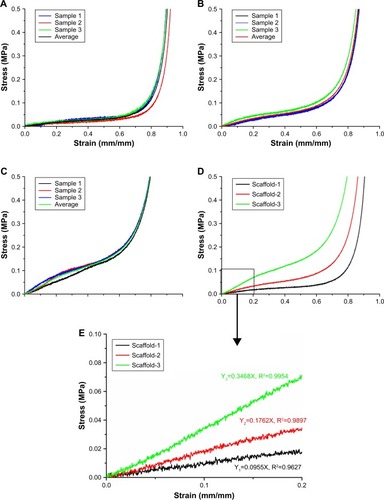
Mechanical properties
The stress–strain curves of the scaffold shown in indicate that the stress gradually increases with the gradual increase in strain, and the compressive performance of the scaffold increases remarkably with an increase in the material concentration. As shown in , the elastic moduli of Scaffold-1, Scaffold-2, and Scaffold-3 were 0.0955, 0.1762, and 0.3468 MPa, respectively. In addition, when the strain reaches 0.80, the compressive stresses of Scaffold-1, Scaffold-2, and Scaffold-3 are 0.12, 0.26, and 0.53 MPa, respectively. These findings indicate that the scaffold has good compression resistance and can withstand certain external pressures.
Water swelling rate of the scaffolds after compression
As shown in and , the water swelling rates of Scaffold-1, Scaffold-2, and Scaffold-3 after compression are 1,587.27±63.09, 2,379.53±77.04, and 1,989.53%±118.90%, respectively. Compared with the water swelling rate of Scaffold-1 before compression, the water swelling rate was significantly reduced after compression. No significant change in the water swelling rates of the Scaffold-2 and Scaffold-3 groups was found before and after compression. This indicates that the three kinds of scaffolds have excellent water absorption capacity. After an external force equal to the average weight of Chinese adults was applied, Scaffold-2 and Scaffold-3 had good recovery from compression. Scaffold-1 may have poor compression resistance and mechanical stability due to its low material concentration, which causes irreversible changes in the structure of Scaffold-1 after compression.
Table 3 Water swelling rate of the silk fibroin/chitosan/nano-hydroxyapatite scaffolds with gradient pore diameters before and after compression (mean±SD, %, n=4)
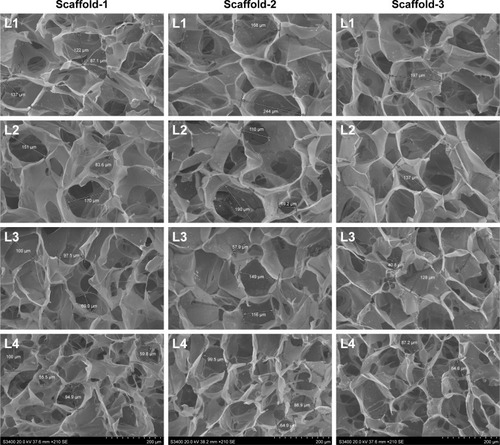
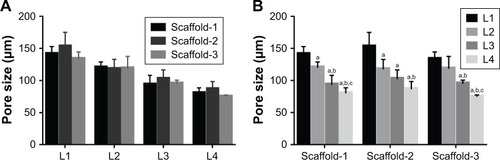
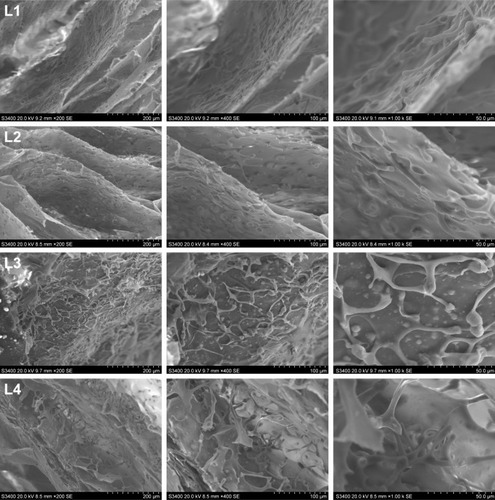
Internal structure of the scaffold and pore size
The SEM images show a honeycomb-like internal structure of the scaffold, with polygonal and circular pores and highly inter-connected gaps (). The pores are densely distributed from the upper part to the lower part of the scaffold, and the pore diameter gradually decreases from the upper part to the lower part of the scaffold. The nHA content increased gradually from the upper part to the lower part of the scaffold. The inner wall of the scaffold gradually thickened with an increase in the material content corresponding to Scaffold-1, Scaffold-2, and Scaffold-3, respectively. As shown in and , the pore size of each scaffold shows a different degree of decrease from layer 1 (L1) to layer 4 (L4) (F2%=22.973, P=0.000; F3%=11.709, P=0.001; F4%=20.151, P=0.016; n=4). Scaffold-2 shows a uniform pore distribution, and the pore size from top to bottom changed slightly, followed by Scaffold-1, and Scaffold-3 shows uneven pore distribution, an obviously changed pore size, and fewer pores. In addition, the pore size of the scaffolds corresponding to the same layer showed no significant differences from L1 to L4 (FL1=1.458, P=0.283; FL2=0.027, P=0.973; FL3=0.598, P=0.570; FL4=1.780, P=0.223; n=4); this may be associated with the differences in pore size and uneven pore distribution throughout the three scaffolds. These findings indicate that, within the material concentration of 2%–4% in the precursor solutions, a progressive change in the pore size and local accumulation of nHA may occur in the resulting scaffold, owing to the centrifugal force.
Table 4 Pore size of the different layers of the silk fibroin/chitosan/nano-hydroxyapatite scaffolds with gradient pore diameters (mean±SD, μm, n=4)
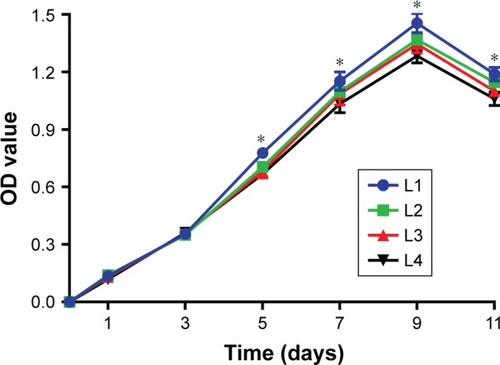
Cell proliferation in the BMSC-scaffold complex
As shown in and , the cells in each layer of the BMSC-scaffold complex began to proliferate logarithmically after 3 days of culture, and then they proliferated at a stable rate after 9 days of culture. After 1 and 3 days of culture, there was no significant difference in the cell proliferation between the layers (F1d=1.168, P=0.363; F3d=0.407, P=0.751; n=4). After 5, 7, 9, and 11 days of culture, significant differences were observed in the cell proliferation among the different layers of the complex (F5d=12.432, P=0.001; F7d=4.474, P=0.025; F9d=13.250, P=0.000; F11d=17.830, P=0.000; n=4). These findings reveal that BMSCs can grow normally in the scaffold, there was no obvious slowing of cell proliferation and decreased cell activity. The BMSCs proliferated well in the scaffold with time, implying that the scaffolds have good biocompatibility. Moreover, the cell proliferation was slightly faster in the upper part of the scaffold than in the lower part, which might have resulted from the growth environment. Remarkably, the rate of cell proliferation was not inhibited in any of the layer.
Table 5 Optical density of the cells in different layers of the silk fibroin/chitosan/nano-hydroxyapatite scaffolds (mean±SD, n=4)
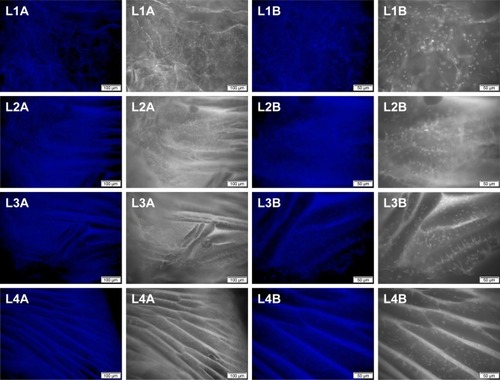
Cell distribution in the BMSC-scaffold complex
The number of cells in the BMSC-scaffold complex was highest after 9 days of culture, during which the scaffold was assessed for cell distribution. As shown in , the cells in the different layers of the scaffold were evenly distributed with uniform morphology of the nucleus, and without metachromatic nuclei, indicating that there were no obvious apoptosis and mutation of stem cells. Moreover, the cell density in the scaffolds from layer 1 to layer 4 decreased slightly. Unfortunately, quantitative analysis could not be performed because of the fluorescence background. These experimental findings reveal that BMSCs can be stably attached to the scaffold and grow well, indicating that the scaffold has good biocompatibility. In addition, more cells were found distributed in the upper layers with larger pores, indicating that the pore size or growing space might have a certain impact on the cell growth and proliferation. As shown in , a large amount of cells were adherent to the inner wall of each layer of the scaffold, and the cells were uniform in shape and closely arranged in a long spindle shape. There was no obvious cell disruption or morphological abnormality, indicating that the scaffold has good biocompatibility and no cytotoxicity, and cannot cause apoptosis, malformation, mutation, and rupture of the cells. Under the SME, more cells were also found distributed in the upper layers with larger pores, consistent with the DAPI fluorescence staining findings.
Discussion
Current research on osteochondral repair materials has led to great results. Seed cells and scaffold materials are two focal points of current research, and scaffold materials with good performance can provide stable growth and differentiation space for the seed cells.Citation22,Citation23 However, there is no widely accepted ideal osteochondral scaffold material to date, especially for large-area osteochondral defects. The main prevalent issues are the safety, biomechanical properties, degradability, porosity, and histocompatibility of the scaffold materials as well as the influence of the degradation products on the surrounding tissues. Moreover, it is especially important to ensure consistency between the structure of the scaffold material and the normal osteochondral tissue,Citation24 and further extensive investigations are still required on this aspect.
SF is a natural material consisting of three proteins extracted from silk. In its structure, a heavy chain with a relative molecular mass of 350–390 kDa is linked to a light chain with a relative molecular weight of ~26 kDa through a disulfide bond. The third small glycoprotein with a relative molecular mass of ~30 kDa is referred to as P25 protein; it binds by non-covalent hydrophobic interaction.Citation25,Citation26 SF can be easily chemically modified, and it has bactericidal activity, thermal stability, and controllable degradability. Moreover, SF can provide enough strength, toughness, elasticity, and environmental stability when applied to artificial ligaments, cartilage, bone, and nerve tissues.Citation27–Citation29 CS is a derivative formed by the deacetylation of chitin using chemical or deacetylase inhibitors. It is a natural, high-molecular-weight polysaccharide mainly composed of β-(1,4)-N-acetyl-D-glucose and partially repeated β-(1,4)-D-glucosamine,Citation30 and it has a structure similar to that of the cartilage matrix, glycosaminoglycan. Glucosamine monomer, the degradation product of CS, has good mechanical properties, better biocompatibility, and low immunogenicity, which can enhance bone regeneration together with other materials, such as nHA.Citation31 Furthermore, CS also has antibacterial, anti-oxidant, and anti-tumor activities and has been widely used in biomedicine.Citation32–Citation34 nHA is a bioactive ceramic with the chemical formula, [Ca5(OH)(PO4)3]x, that has a similar density to that of human teeth and bones. As an inorganic mineral, nHA has a typical apatite crystal structure and has similar inorganic components as the bone. nHA with good biocompatibility is beneficial for bone conduction, bone tissue growth, and pro-osteogenic differentiation of stem cells,Citation35 which is considered an ideal material for repairing bone defects.Citation36 nHA has been used in various ways, such as a coating material for enhancing the biocompatibility of simple materialsCitation37,Citation38 and synthetic hydroxyapatite bone cement, a material for compensating bone loss in orthopedic surgery.Citation39 However, there are some shortcomings in scaffolds made of simple SF, CS, or nHA. The SF scaffold is fragile, with poor osteoinductivity, and has weak water absorption. The CS scaffold is less easily absorbed, with slow degradation, and poor cell adhesion. The simply synthesized nHA materials have low strength and low porosity after molding; however, some research findings reveal that composite materials consisting of nHA are promising for applications in mechanics and biology.Citation36,Citation40–Citation42 Therefore, the three materials, SF, CS, and nHA, can complement one another to satisfy the requirements of tissue-engineered scaffolds. In this study, SF, CS, and nHA were blended at a certain ratio, and the mixture was processed to obtain the SF/CS/nHA composite scaffolds, which not only compensates for their respective shortcomings, but could be prepared controllably to achieve desired properties.
Scaffolds that have highly interconnected pores with porosity greater than 70% are considered to provide good space for cell survival and channels for nutrient transport to maintain cell growth.Citation43 The porosity of all the scaffolds prepared in this study is above 80%. Although there is no consensus on the optimal pore size of a porous cell scaffold for cell growth and mass transfer, in general, the scaffold should have a pore size of 100–300 μmCitation43,Citation44 to facilitate cell growth and reproduction. The average pore size of the three kinds of scaffolds with gradient pore sizes prepared in this study is above 100 μm. The pores were densely distributed from the top to bottom layers, and the pore size gradually decreased from top to bottom. Scaffold-2, which had evenly distributed pores with a smooth gradient, yielded better results (). In the early days, some scholars used single- or double-layered scaffolds to repair osteochondral defects. However, the lack of a gradient structure led to the collapse or stratification of the repair area, eventually resulting in the failure of repair. The progressive gradient scaffold fabricated in this study provides a good support via the densely distributed pores in the lower layer (bone layer) of the scaffold, which can prevent the collapse of the upper layer (cartilage layer) of the scaffold. This scaffold with gradient pore diameters can enable better transition and integration between the cartilage layer and bone layer. Moreover, SEM images show that the nHA content in the scaffold gradually increases from top to bottom, which can further strengthen the mechanical strength of the lower part of the scaffold. With the advantages of osteogenic induction and bone growth promotion, nHA at a higher concentration in the lower part of the scaffold can induce and promote osteogenesis, while nHA at a lower concentration in the upper part of the scaffold exerts little effects on the cartilage formation. Moreover, owing to the gradient change in the concentration of nHA in the upper and lower parts of the scaffold, the cartilage layer and the bone layer can well transition and integrate. Therefore, the scaffolds prepared in this study not only have suitable porosity and pore size, but also have progressively varying pores and nHA concentration, which can strengthen the supporting capacity of the lower part of the scaffold, while facilitating the formation of bone tissues in the lower part of the scaffold as well as the transition and integration between the cartilage and bone layers of the scaffold.
The chemical cross-linking under the action of light, heat, high-energy radiation, mechanical force, ultrasonic wave, or cross-linking agents enables the formation of a network or a bulk structure between the linear or branched polymers. Therefore, this method can improve the material tension and stability.Citation45,Citation46 Methanol-mediated cross-linking can transform the water-soluble α-helical structure or disc-like structure of SF into a stable β-sheet structure, rendering it water-insoluble. When SF is mixed with CS, active amino groups in the CS can form hydrogen bonds not only with the carboxyl groups in CS, but also with the carboxyl groups in SF, further making the composite scaffold more stable.Citation47,Citation48 EDC and NHS, as two non-toxic and biocompatible cross-linking agents, can promote the cross-linking of SF and CS via the formation of amide cross-linking bonds between the carboxyl groups and the amine groups, and also ester bonding between the activated carboxyl groups and the hydroxyl groups, thereby altering the molecular covalent structure within the scaffold and, thus, enhancing the biostability of the scaffold. Moreover, the cross-linking degree of the scaffold can be controlled by changing the concentration of EDC/NHS.Citation49–Citation51 In general, autologous transplantation can significantly restore the joint function and quality-of-life or enable better bone regeneration and remodeling in patients with joint and cartilage injury within 1 year.Citation52–Citation57 Therefore, the scaffold materials for osteochondral defects should completely degrade in ~1 year. The hot-water dissolution rate vs time curves of the prepared scaffolds suggested that all the scaffolds have a faster dissolution rate in the first week, which might be related to the exfoliation of nHA during the oscillation and excessive loss of nHA during the ultrasonic cleaning. However, the dissolution rates of all the scaffolds tended to be stable and showed no significant differences in the second to fifth week. Regression analysis revealed that the hot-water dissolution rate of the scaffold could increase within a certain range over time, and the theoretical time for the complete dissolution of the scaffold is greater than 1 year, which is close to the time required for significant osteochondral repair. These results indicate that chemical cross-linking can maintain the stability of the scaffold over a long time, which can provide a stable space for seed cells to proliferate and differentiate in the scaffold. Further, the scaffold can gradually degrade and get absorbed during osteochondral repair and remodeling.
A good osteochondral tissue scaffold should have a certain ability to resist external pressure. The stress-strain curves of the scaffolds prepared in this study indicate that each scaffold has good compressive performance, which increases with the increase in the material content. This suggests that the scaffolds can resist a certain degree of external pressure and provide a stable space for cell survival, however, the mechanical properties of the scaffolds are insufficient when compared to the natural boneCitation58–Citation60 and cartilageCitation61,Citation62 tissue. Nutrients are essential for the cells to grow normally in the scaffold, and, therefore, the scaffold should have the ability to absorb a sufficient amount of nutrients. The scaffolds prepared in this study have strong water absorption. Although they can be deformed under a certain external force, the scaffolds will be restored quickly within 1–2 seconds after immersion in water; the shape and size of the scaffolds showed no significant changes. Moreover, after an external force equal to the average weight of Chinese adults was applied to the scaffolds, no significant changes in the water swelling rate and recovery ability of Scaffold-2 and Scaffold-3 was observed, which can compensate for the lack of sufficient compression resistance of the scaffold. This also indicates that the scaffolds have strong water absorption ability and good plasticity, and the external pressure does not affect the structure of the scaffolds as well as the ability to absorb nutrients. All these findings reveal that the scaffolds can provide sufficient nutrients and a stable space for cell growth.
The osteochondral scaffold should have good biocompatibility and no cytotoxicity. In this study, the cells could be closely attached to the prepared scaffolds and stably grown and proliferated, with no presence of malformation, mutation, and rupture, indicating that the scaffolds are non-cytotoxic and biocompatible. In addition, findings from the cell counting kit-8, DAPI fluorescent staining, and SEM observation indicate that the different pore sizes or the internal structure of the scaffold might have certain effects on the cell growth and proliferation; however, interestingly, there was no significant effect on the cell proliferation rate, which might be related to insufficient nutrient content around the cells owing to the different growth space, and the concentration of the nutrient solution in the smaller pores reduced faster during the cell proliferation and absorption.
Conclusion
The SF/CS/nHA osteochondral scaffold with a progressively gradient pore size prepared in this study has high porosity, highly interconnected pores, and progressively increasing pore distribution. The pore size of the scaffold varied progressively, and the nHA concentration of the scaffold increased gradually from the upper to the lower part of the scaffold. Moreover, the scaffold has strong water absorption, a suitable degradation rate, space suitable for cell growth and proliferation, and good structural stability. BMSCs inoculated into the scaffold could closely attach to the scaffold and then grow stably and proliferate, indicating that the scaffold is non-cytotoxic and biocompatible. These excellent properties provide sufficient nutrients and space for the stem cell growth, proliferation, and migration. The physical properties and biocompatibility of the scaffold fully meet the requirements of tissue-engineered scaffolds for osteochondral repair. However, the application of SF/CS/nHA scaffold for osteochondral repair still needs to be further investigated in in vitro and in vivo studies.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
This study was supported by the National Natural Science Foundation (No. 81660367), the Science and Technology Foundation of Guizhou Province (No. (2016)1420), the Fund of Guizhou Provincial Health and Family Planning Committee (No. gzwjkj2018-2-005) the Youth Fund of Guizhou Provincial People’s Hospital (No. GZSYQN[2015]04).
Disclosure
The authors report no conflicts of interest in this work.
References
- LevingstoneTJMatsikoADicksonGRO’BrienFJGleesonJPA biomimetic multi-layered collagen-based scaffold for osteochondral repairActa Biomater20141051996200410.1016/j.actbio.2014.01.00524418437
- ShermanSLThyssenENuelleCWOsteochondral autologous transplantationClin Sports Med201736348950010.1016/j.csm.2017.02.00628577708
- SeoSJMahapatraCSinghRKKnowlesJCKimHWStrategies for osteochondral repair: focus on scaffoldsJ Tissue Eng20145 204173141454185010.1177/2041731414541850
- GuoXWangCDuanCRepair of osteochondral defects with autologous chondrocytes seeded onto bioceramic scaffold in sheepTissue Eng20041011–121830184010.1089/ten.2004.10.183015684691
- WangXGroganSPRieserFTissue engineering of biphasic cartilage constructs using various biodegradable scaffolds: an in vitro studyBiomaterials200425173681368810.1016/j.biomaterials.2003.10.10215020143
- ChenGTanakaJTateishiTOsteochondral tissue engineering using a PLGA–collagen hybrid meshMat Sci Eng200626112412910.1016/j.msec.2005.08.042
- SchaeferDMartinIShastriPIn vitro generation of osteochondral compositesBiomaterials200021242599260611071609
- GaoJDennisJESolchagaLAAwadallahASGoldbergVMCaplanAITissue-engineered fabrication of an osteochondral composite graft using rat bone marrow-derived mesenchymal stem cellsTissue Eng20017436337110.1089/1076327015243642711506726
- KreklauBSittingerMMensingMBTissue engineering of biphasic joint cartilage transplantsBiomaterials199920181743174910503975
- NiederauerGGSlivkaMALeatherburyNCEvaluation of multiphase implants for repair of focal osteochondral defects in goatsBiomaterials200021242561257411071606
- HunzikerEBDriesangIMFunctional barrier principle for growth-factor-based articular cartilage repairOsteoarthritis Cartilage200311532032712744937
- DormerNHBerklandCJDetamoreMSEmerging techniques in stratified designs and continuous gradients for tissue engineering of interfacesAnn Biomed Eng20103862121214110.1007/s10439-010-0033-320411333
- KonEDelcoglianoMFilardoGBusaccaMDi MartinoAMarcacciMNovel nano-composite multilayered biomaterial for osteochondral regeneration: a pilot clinical trialAm J Sports Med20113961180119010.1177/036354651039271121310939
- DengJSheRHuangWDongZMoGLiuBA silk fibroin/chitosan scaffold in combination with bone marrow-derived mesenchymal stem cells to repair cartilage defects in the rabbit kneeJ Mater Sci Mater Med20132482037204610.1007/s10856-013-4944-z23677433
- YePTianRYHuangWLMaLKDengJSilk fibroin/chitosan/nano hydroxyapatite complicated scaffolds for bone tissue engineeringZhongguo Zuzhi Gongcheng Yanjiu2013172952695274
- DengJSheRFHuangWLYuanCMoGFibroin protein/chitosan scaffolds and bone marrow mesenchymal stem cells culture in vitroGenet Mol Res20141335745575310.4238/2014.July.29.125117332
- MaLKYePDengJHuangWLTianRYLvXFThe cytotoxicity of silk fibroin/chitosan/nano hydroxyapatite bone tissue engineering scaffolds in vitroXibu Yixue2014268975977980
- RuanSQDengJYanLHuangWLComposite scaffolds loaded with bone mesenchymal stem cells promote the repair of radial bone defects in rabbit modelBiomed Pharmacother20189760060610.1016/j.biopha.2017.10.11029101803
- YePYuBDengJSheRFHuangWLApplication of silk fibroin/chitosan/nano-hydroxyapatite composite scaffold in the repair of rabbit radial bone defectExp Ther Med20171465547555310.3892/etm.2017.523129285090
- National Health and Family Planning CommissionChinese Citizens Nutrition and Chronic Disease Report 2015Beijing (China)People’s Medical Publishing House2015
- LiuDBHanXSHuangWLDengJSheRFStudy on the differentiation of rat bone marrow mesenchymal stem cells into chondrocytes induced by TGF-beta 3Zhonghua Yi Xue Za Zhi201797362860286510.3760/cma.j.issn.0376-2491.2017.36.01729050153
- IulianADanLCameliaTClaudiaMSebastianGSynthetic materials for osteochondral tissue engineeringAdv Exp Med Biol20181058315210.1007/978-3-319-76711-6_229691816
- MaiaFRCarvalhoMROliveiraJMReisRLTissue engineering strategies for osteochondral repairAdv Exp Med Biol2018105935337110.1007/978-3-319-76735-2_1629736582
- ShimomuraKMoriguchiYMurawskiCDYoshikawaHNakamuraNOsteochondral tissue engineering with biphasic scaffold: current strategies and techniquesTissue Eng Part B Rev201420546847610.1089/ten.TEB.2013.054324417741
- HardyJGScheibelTRComposite materials based on silk proteinsProg Polym Sci20103591093111510.1016/j.progpolymsci.2010.04.005
- RockwoodDNPredaRCYücelTWangXLovettMLKaplanDLMaterials fabrication from Bombyx mori silk fibroinNat Protoc20116101612163110.1038/nprot.2011.37921959241
- LevengoodSLZhangMChitosan-based scaffolds for bone tissue engineeringJ Mater Chem B20142213161318410.1039/C4TB00027G24999429
- KohLDChengYTengCPStructures, mechanical properties and applications of silk fibroin materialsProg Polym Sci2015468611010.1016/j.progpolymsci.2015.02.001
- WrayLSHuXGallegoJEffect of processing on silk-based biomaterials: reproducibility and biocompatibilityJ Biomed Mater Res B Appl Biomater20119918910110.1002/jbm.b.3187521695778
- YounesIRinaudoMChitin and chitosan preparation from marine sources. Structure, properties and applicationsMar Drugs20151331133117410.3390/md1303113325738328
- LiZYubaoLAipingYXuelinPXuejiangWXiangZPreparation and in vitro investigation of chitosan/nano-hydroxyapatite composite used as bone substitute materialsJ Mater Sci Mater Med200516321321910.1007/s10856-005-6682-315744612
- VeleirinhoBCoelhoDSDiasPFMaraschinMRibeiro-do-ValleRMLopes-da-SilvaJANanofibrous poly(3-hydroxybutyrate-co-3- hydroxyvalerate)/chitosan scaffolds for skin regenerationInt J Biol Macromol201251434335010.1016/j.ijbiomac.2012.05.02322652216
- FratterAFrareCUrasGNew chitosan salt in gastro-resistant oral formulation could interfere with enteric bile salts emulsification of diet fats: preliminary laboratory observations and physiologic rationaleJ Med Food201417672372910.1089/jmf.2013.013124827073
- HamedIOzogulFRegensteinJMIndustrial applications of crustacean by products (chitin, chitosan, and chitooligosaccharides): a reviewTrends Food Sci Tech201648405010.1016/j.tifs.2015.11.007
- ChengHChabokRGuanXSynergistic interplay between the two major bone minerals, hydroxyapatite and whitlockite nanoparticles, for osteogenic differentiation of mesenchymal stem cellsActa Biomater20186934235110.1016/j.actbio.2018.01.01629366976
- RatnayakeJTBMucaloMDiasGJSubstituted hydroxyapatites for bone regeneration: a review of current trendsJ Biomed Mater Res B Appl Biomater201710551285129910.1002/jbm.b.3365126991026
- DiezMKangMHKimSMKimHESongJHydroxyapatite (HA)/poly-L-lactic acid (PLLA) dual coating on magnesium alloy under deformation for biomedical applicationsJ Mater Sci Mater Med20162723410.1007/s10856-015-5643-826704551
- KimSMJoJHLeeSMHydroxyapatite-coated magnesium implants with improved in vitro and in vivo biocorrosion, biocompatibility, and bone responseJ Biomed Mater Res A2014102242944110.1002/jbm.a.3471823533169
- RabieeSMMoztarzadehFSolati-HashjinMSynthesis and characterization of hydrox-yapatite cementJ Mol Struct20109691–317217510.1016/j.molstruc.2010.01.068
- WłodarskiKHWłodarskiPKGalusRBioactive composites for bone regeneration. ReviewOrtop Traumatol Rehabil200810320121018552757
- ChiuCKFerreiraJLuoTJGengHLinFCKoCCDirect scaffolding of biomimetic hydroxyapatite-gelatin nanocomposites using aminosilane cross-linker for bone regenerationJ Mater Sci Mater Med20122392115212610.1007/s10856-012-4691-622669282
- VenkatesanJKimSKNano-hydroxyapatite composite biomaterials for bone tissue engineering – a reviewJ Biomed Nanotechnol201410103124314025992432
- PuppiDChielliniFPirasAMChielliniEPolymeric materials for bone and cartilage repairProg Polym Sci201035440344010.1016/j.progpolymsci.2010.01.006
- PrananingrumWNaitoYGalliSBone ingrowth of various porous titanium scaffolds produced by a moldless and space holder technique: an in vivo study in rabbitsBiomed Mater201611101501210.1088/1748-6041/11/1/01501226836201
- VanherckKKoeckelberghsGVankelecomICrosslinking polyimides for membrane applications: a reviewProg Polym Sci201338687489610.1016/j.progpolymsci.2012.11.001
- XuJLiuXRenXGaoGThe role of chemical and physical crosslinking in different deformation stages of hybrid hydrogelsEur Polym J2018100869510.1016/j.eurpolymj.2018.01.020
- ZhangXZSituFMPengPJiaoYPChitosan improves the crystallization of silk fibroin: a three-dimensional scaffold material with better mechanical stabilityZhongguo Zuzhi Gongcheng Yanjiu20151218581863
- ZengSLiuLShiYCharacterization of silk fibroin/chitosan 3D porous scaffold and in vitro cytologyPLoS One2015106e012865810.1371/journal.pone.012865826083846
- YanCRInfluence of crosslinking on the biological and physical properties of collagenZhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu20093521524
- EveraertsFTorrianniMHendriksMFeijenJBiomechanical properties of carbodiimide crosslinked collagen: influence of the formation of ester crosslinksJ Biomed Mater Res A200885254755510.1002/jbm.a.3152417729260
- BaxDVDavidenkoNGullbergDFundamental insight into the effect of carbodiimide crosslinking on cellular recognition of collagen-based scaffoldsActa Biomater20174921823410.1016/j.actbio.2016.11.05927915017
- MengYLinZLLiuSZWangSZZhuJQArthroscopic osteochondral autologous transplantation for femoral cartilage defect treatment: a 1 to 4 years follow-up studyZhongguo Zuzhi Gongcheng Yanjiu2009133160556058
- BarberFAChowJCArthroscopic chondral osseous autograft transplantation (COR procedure) for femoral defectsArthroscopy2006221101610.1016/j.arthro.2005.08.04016399455
- MarcacciMKonEDelcoglianoMFilardoGBusaccaMZaffagniniSArthroscopic autologous osteochondral grafting for cartilage defects of the knee: prospective study results at a minimum 7-year follow-upAm J Sports Med200735122014202110.1177/036354650730545517724094
- KrychAJHarnlyHWRodeoSAWilliamsRJ3rdActivity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative studyJ Bone Joint Surg Am2012941197197810.2106/JBJS.K.0081522637203
- MummeMBarberoAMiotSNasal chondrocyte-based engineered autologous cartilage tissue for repair of articular cartilage defects: an observational first-in-human trialLancet2016388100551985199410.1016/S0140-6736(16)31658-027789021
- ChadliLCottalordaJDelpontMMazeauPThouveninYLouahemDAutologous osteochondral mosaicplasty in osteochondritis dissecans of the patella in adolescentsInt Orthop201741119720210.1007/s00264-016-3198-z27118373
- WangQLiRCWangFWangQGWangDMRelationship between mineral density and elastic modulus of human cancelluous boneYiyong Shengwu Lixue2014295456470
- BrownTDVrahasMSThe apparent elastic modulus of the juxtarticular subchondral bone of the femoral headJ Orthop Res198421323810.1002/jor.11000201066491796
- DayJSDingMvan der LindenJCHvidISumnerDRWeinansHA decreased subchondral trabecular bone tissue elastic modulus is associated with pre-arthritic cartilage damageJ Orthop Res200119591491810.1016/S0736-0266(01)00012-211562141
- ObeidEMAdamsMANewmanJHMechanical properties of articular cartilage in knees with unicompartmental osteoarthritisJ Bone Joint Surg Br19947623153198113301
- PetersAEAkhtarRComerfordEJBatesKTThe effect of ageing and osteoarthritis on the mechanical properties of cartilage and bone in the human knee jointSci Rep201881593110.1038/s41598-018-24258-629651151