Abstract
Background
Titanium (Ti) implants are widely used clinically, but peri-implantitis remains one of the most common and serious complications. Healthy integration between gingival tissue and the implant surface is critical to long-term success in dental implant therapy. The objective of this study was to investigate how different concentrations of immobilized fibroblast growth factor 2 (FGF2) on the titania nanotubular surface influence the response of human gingival fibroblasts (HGFs).
Methods
Pure Ti metal was anodized at 20 V to form a vertically organized titanium dioxide nanotube array on which three concentrations of FGF2 (250 ng/mL, 500 ng/mL, or 1000 ng/mL) were immobilized by repeated lyophilization. Surface topography was observed and FGF2 elution was detected using enzyme-linked immunosorbent assay. The bioactivity changes of dissolvable immobilized FGF2 were measured by methyl-thiazolyl-tetrazolium assay. Behavior of HGFs was evaluated using adhesion and methyl-thiazolyl-tetrazolium bromide assays.
Results
The FGF2 remained for several days on the modified surface on which HGFs were cultured. Over 90% of the dissolvable immobilized FGF2 had been eluted by Day 9, whereas the FGF2 activity was found to diminish gradually from Day 1 to Day 9. The titania nanotubular surface with an optimal preparing concentration (500 ng/mL) of FGF2 immobilization exhibited improved HGF functions such as cellular attachment, proliferation, and extracellular matrix-related gene expression. Moreover, significant bidirectional as well as concentration- and time-dependent bioactivity was observed.
Conclusion
Synergism of the FGF2-impregnated titanium dioxide nanotubular surface revealed good gingival-implant integration, indicating that these materials might have promising applications in dentistry and other biomedical devices.
Introduction
Titanium (Ti) and its alloys are widely used in dental implant therapy to treat edentulous patients but may suffer from failure due to peri-implantitis and other complications.Citation1–Citation3 Archival evidence supports the view that the long-term retention of an osseointegrated implant is influenced mainly by proper marginal soft tissue sealingCitation4 of the alveolar bone below.Citation5,Citation6 Furthermore, the proper dimensions and function of the soft tissue seal are prerequisite to therapeutic success.Citation7,Citation8 Recent studies have revealed specific differences between the microbial profiles of healthy and diseased dental implants,Citation9,Citation10 indicating that the loss of balance between the known periodontal pathogens and host-compatible microbial complexes may contribute to peri-implantitis and reinfection of the subgingival sites.Citation10 A well-formed soft tissue seal reduces the exposed area of the subgingival part of the implant and may reduce the formation and growth of a biofilm without disturbing the microbial balance around the implant.
Although polished Ti (PT) and Ti alloys are used in the transgingival part of conventional dental implants, they contact only the surrounding soft tissues and do not form a healthy seal at the soft tissue-implant interface by themselves. Manipulating the structure of Ti is a possible way to enhance soft tissue compatibility on Ti dental implants. The shape, surface topography, design, physicochemical properties, and even the method used to sterilize the Ti implant may affect the integration between the implant and soft tissues.Citation11,Citation12 The method is quite promising for tissue regeneration, due to the well-organized and porous Ti nanostructure that forms the biocompatible surface.
A titanium dioxide (TiO2) nanotubular structure can be formed on Ti by anodization of a relatively large surface area to enable bioactive factor absorption.Citation13,Citation14 According to previous studies, the TiO2 nanotubular structure can affect functions such as adhesion, orientation, proliferation, and gene expression in various types of cells.Citation14–Citation17 In addition, the TiO2 nanotubular surface with a tube size of ~120 nm exhibits better electrochemical stability in artificial saliva as well as improved adhesion and proliferation of human gingival fibroblasts (HGFs).Citation18
Fibroblast growth factors (FGFs) are a large family of polypeptide growth factors that regulate the secretion of various extracellular matrix (ECM) proteins, which contribute to the formation of new blood vessels.Citation19,Citation20 Fibroblast growth factor 2 (FGF2) is a potent mitogen in a variety of cells and is effective in regulating the proliferation and ECM-related gene expression of fibroblasts,Citation21,Citation22 the most common cell type in peri-implant gingival connective tissue.
To control the responses of cells and tissues toward biomaterials, modification of surfaces and immobilization of biomolecules have been widely studied.Citation23 FGF2 can be immobilized on Ti surfaces pretreated with oxygen plasma,Citation24 and the TiO2 nanotubular surface benefits drug control releaseCitation25 and immobilization of other growth factors such as, bone morphogenetic protein 2 as well.Citation14 Hence, a TiO2 nano-tubular surface and FGF2 may be used together to improve early gingival tissue-implant integration by enhancing the functions of surrounding HGFs. However, according to previous studies, the effects of FGF2 may depend on the concentration of FGF2 in the culture medium, suggesting that improper amounts of FGF2 on the Ti surface may spur adverse effects.Citation26 Although the behavior of some cells on surfaces with different topographies has been investigated, the relationship between the behavior of HGFs around dental implants and variable FGF2 immobilization has not been systematically studied.Citation27–Citation29 Hence, a better understanding of this issue will help to mimic natural gingival tissue-implant integration.
In the work reported here, Ti samples were anodized at 20 V to form a vertically organized TiO2 nanotubular surface, and FGF2 solutions of three different concentrations were used to immobilize FGF2 on the nanotubular surface by repeated lyophilization. The objectives of this study are to investigate how different concentrations of immobilized FGF2 on the titania nanotubular surface influence the response of HGFs, and to determine the associated mechanism.
Materials and methods
Sample preparation
Pure Ti foils (99.9%, 1000 × 500 × 0.6 mm3, supplied by Northwest Institute for Nonferrous Metal Research, Xi’an, People’s Republic of China) were cut into 10 × 10 × 0.6 mm3 pieces, polished with 400- to 1500-grit silicon carbide sandpaper in running water, and ultrasonically cleaned in acetone, 70% ethanol, and doubly distilled water for 10 minutes sequentially. They were then dried at 50°C for 20 minutes under flowing nitrogen. The PT samples were anodized in an electrolyte solution containing 0.5% ammonium fluoride and 1 M ammonium sulfate at 20 V for 45 minutesCitation18 using a Ti anode and a PT cathode. During anodization, the electrolyte was stirred constantly, and afterwards the samples were ultrasonically cleaned and dried as described previously to obtain the nanotube (NT) samples.
Immobilization of FGF2
The NT samples were sterilized by ultraviolet A (peak wavelength 365 nm, Philips TL-D 18 WBL, the Netherlands) and C (peak wavelength 253.7 nm, Philips TUV 15W, Poland) irradiation at a distance of 30 mm for 2 hours each, because ultraviolet sterilization inactivates bacteria without organic contamination and decomposes existing organic species on the titania surface by photocatalysis.Citation30 The Escherichia coli source recombinant human FGF2 (Peprotech, UK) was reconstituted in Tris-HCl buffered solution (pH 7.6, Sigma-Aldrich, St, Louis, MO) with 0.1% bovine serum album (Gibco, US). The FGF2 was diluted to 250 ng/mL, 500 ng/mL, or 1000 ng/mL. The NT samples were divided into three groups designated as NT-F-L, NT-F-M, and NT-F-H, corresponding respectively to the FGF2 concentrations. Each group was incubated in the appropriate FGF2 solution for 10 minutes at 4°C in an orbital shaker (45 rpm, MaxQ 8000, Thermo, US) and then lyophilized (Alpha 1–4 LSC, Chirst, Germany) at −50°C overnight to obtain three types of FGF2-immobilized samples. The immobilization procedures were repeated thrice.
Surface analysis
The FGF2 on the NT-F-L/M/H samples was examined by an immunofluorescence assay.Citation24 After FGF2 immobilization, the samples were gently washed thrice with phosphate buffered saline (PBS, pH = 7.4) for 5 minutes, treated with rabbit anti-bFGF polyclonal antibody (1:200; Sigma-Aldrich) as the primary antibody at 4°C overnight, and washed thrice with PBS. The samples were then treated with fluorescein isothiocyanate-labeled goat antirabbit immunoglobulin G (1:200; Bois, People’s Republic of China) for 1 hour at 37°C and washed thrice in PBS (pH = 7.4). The samples were inspected by laser confocal microscopy (Olympus FV-1000, Japan). In order to evaluate the remaining FGF2 on the nanotubular surface over a specific time interval, a portion of the FGF2 immobilized samples was incubated in PBS at 37°C for 9 days (with a change in PBS every 3 days), and then the immunofluorescence procedures were repeated as described previously.
To measure the elution of FGF2 versus time, samples were immersed in PBS (1 mL per sample) at 4°C (to preserve the activity of FGF2) for 1 day, 2 days, 3 days, 4 days, 6 days, 9 days, 15 days, 21 days, or 30 days. Utilizing the standard curve of FGF2, the FGF2 concentrations in the extracts were determined by the enzyme-linked immunosorbent assay (Quantikine® Human FGF Basic Immunoassay, R&D, US), and the amounts of dissolved FGF were also calculated.
Surface characterization
Surface and material characterization was conducted on five types of samples. Field emission scanning electron microscopy (FE-SEM; JSM-6460, JEOL, Japan) and atomic force microscopy (AFM; SPM400, SEIKO, Japan) were employed to observe and measure (Adobe Photoshop CS2) the surface microstructure as well as surface roughness.
Behavior of HGFs
The HGFs were obtained from three periodontally healthy patients (aged 19 years, 33 years, and 46 years) undergoing crown-lengthening surgery. Ethical approval and consent was obtained from all three volunteers. The gingival tissues were washed in PBS containing 100,000 U penicillin/gentamicin twice and incubated in 1 U/mL Dispase® II solution (Roche, US) overnight to separate the connective tissues from the epithelium. The tissues were then sheared into 1.0 mm3 cubes cultured in Dulbecco’s modified Eagle’s medium (DMEM, Gibco) with 10% fetal calf serum (FCS, Gibco) and 100,000 U penicillin/gentamicin (Roche) and incubated in a humidified atmosphere of 5% CO2 at 37°C.
HGFs at passage 4 were used for further analysis. The 1 mL HGF suspension was seeded on each sample (serum-free) at the density 1 × 105 cells/mL (~5 × 104 cells/cm2) and cultured for 30 minutes, 60 minutes, or 120 minutes to allow attachment. At each time interval, the samples were washed with PBS to remove nonattaching cells. Afterwards, the attached cells were fixed in 4% formalin and stained with 4′,6′-diamidino-2-phenylindole (DAPI; 1 μg/mL; Roche).Citation12 The images were captured from the four corners and the center of each sample (2.60 mm × 1.94 mm, five fields per sample) using a fluorescence microscope (Leica DMI6000B, Germany). Three of five images were randomly selected (by random number table). Image J software (National Institutes of Health) was employed to convert the original images to binary images, and black particles were counted to obtain the number of attached cells. The results were calculated as relative cell attachment rates (RCARs) to balance the height of data bars among groups as follows:
RCAR,% = (COUNTT/COUNTP) × 100%, where COUNTT represents the mean value of the cell number counted on the tested samples and COUNTP is the mean value of the cell number on the PT control.
Cell proliferation was evaluated by the methyl-thiazolyl-tetrazolium (MTT) bromide assay. Briefly, five groups of samples (three samples per group) were placed in a 24-well dish (Costar 3524, US) and 4 × 104 HGF cells were seeded in each well and cultured in DMEM with 10% bovine calf serum. On Day 1, Day 3, Day 6, and Day 9, the samples were gently washed three times with PBS and placed on a new 24-well dish. The MTT-PBS (Amresco, US) solutions (5 mg/mL) were prepared and filter sterilized. The MTT solution (200 μL) and serum-free/phenol red-free DMEM (800 μL) were added to each well and the samples were incubated at 37°C for 4 hours to form formazen. Afterwards, formazen was dissolved in dimethyl sulfoxide (DMSO; 1 mL/well). Two hundred microliters of the mixed solution was transferred to a new 96-well dish and the optical density value of each well was monitored at 490 nm using a spectrophotometer (Bio-tek, US).Citation12,Citation18
Morphological observation of HGFs
A 1 mL cell suspension at a density of 2 × 104 cells/mL was seeded on each sample and cultured in DMEM with 10% bovine calf serum. After 3 days, the samples were fixed in a 2.5% glutaraldehyde solution. After a series of dehydration (in graded acetone and isoamyl acetate) and desiccation (lyophilization), the samples were gold-coated and the cell morphology was observed by FE-SEM (JSM-6460, JEOL).
ECM-related gene expression
Expressions of the ECM-related genes were analyzed using quantitative real-time polymerase chain reaction (RT-PCR). The HGFs were cultured in the same manner as described in the proliferation assay. The total RNA of each sample was extracted with TRIzol reagent (Invitrogen). One microgram total of RNA from each sample was reverse transcribed into complementary DNA (cDNA, 50 μL system) using the PrimeScript™ RT reagent kit (TaKaRa, Japan). Quantitative PCR was conducted on the ABI7500 RT-PCR system to determine the mRNA relative expression of the ECM-related genes including vascular endothelial growth factor A (VEGFA), β-integrin (ITGB), intercellular adhesion molecule 1 (ICAM1), and laminin-1 (LAMA1) using SYBR® Premix Ex™ TaqII (TaKaRa). The forward/reverse primers for the selected genes are listed in . The PCR efficiency was compared. The relative expression levels for each gene of interest were normalized to the expression of the housekeeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH) by calculating the change (Δ) in cycle threshold (Ct): ΔCt = (Ctgene of interest − CtGAPDH), and the expression of the different genes was expressed as 2−(ΔCt). The gene expression of PT as the control was normalized to 1.Citation31 The specificity of every pair of PCR primers was confirmed by analyzing the melting curves, and the data were analyzed using the Applied Biosystem Software in the Excel® format.
Table 1 Target cDNA primer sequences used in quantitative polymerase chain reaction
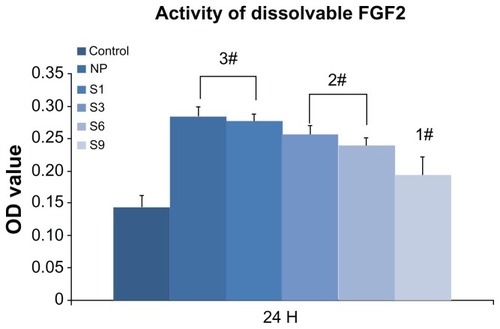
Bioactivity changes of immobilized FGF2
To evaluate the bioactivity changes of FGF2 after repeated lyophilization, 1000 ng of FGF2 was pretreated with three cycles of lyophilization dissolution and diluted to 10 ng/mL in 100 mL of DMEM (serum-free). The FGF2-loaded DMEM was divided into five groups and stored at 37°C to be used at five different time intervals: newly prepared (NP) and S1, S3, S6, S9 (stored for 1 day, 3 days, 6 days, and 9 days, respectively). The PT samples were placed in 24-well dishes (three samples per group), and 4 × 104 HGF cells were seeded on each well. The samples were cultured in FGF2-free DMEM or one of the five types of FGF2-loaded DMEM. After 24 hours, the samples were placed in a new 24-well dish, and the proliferation activity was monitored using the MTT assay as described previously.
Statistical analyses
The data were analyzed using SPSS 18.0 software (SPSS, Inc, Chicago, IL). The statistical results were presented as means ± standard deviation and analyzed by one-way analysis of variance followed by a Student-Newman-Keuls post hoc test to identify significant differences among the groups (multiple comparisons).Citation12 When the probability value (P) was less than 0.01, the difference was regarded as significant.
Results
Surface characterization
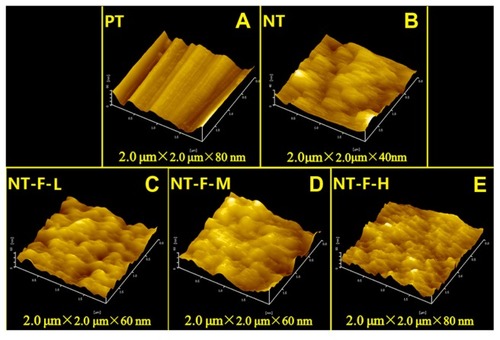
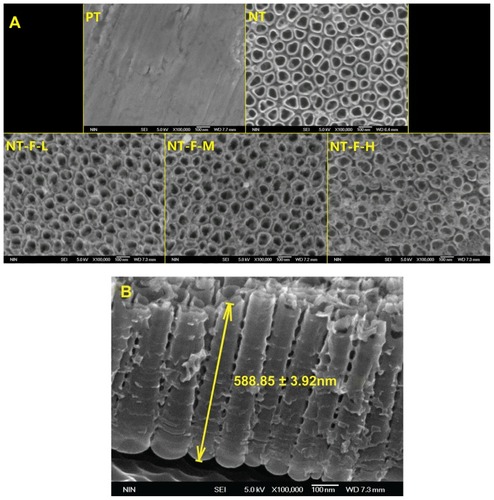
The FGF2-immobilized surfaces (NT-F-L/M/H) generated fluorescence both initially and after 9 days, but no fluorescence was observed from the PT or NTs (). FGF2 was found to be immobilized on the TiO2 nanotubular surface and remained so for a certain period of time. The surface morphology of the samples is displayed in (FE-SEM) and (AFM). On the nanoscale, the TiO2 NTs are organized in a vertical array with a diameter of ~100 nm () and tube length 588.8 ± 31.92 nm (). On the FGF2-immobilized nanotubular surfaces, FGF2 adsorbs on to the TiO2 NT walls homogeneously on NT-F-L and NT-F-M. The morphology is evidently different from that of NT-F-H. The FGF2 on NT-F-H manifested as clumps or cord-like aggregates with a nonuniform distribution. On the microscale, PT demonstrated a microgroove-like surface structure that was a lot rougher than the other four types of NT-based surfaces that have similar nanoporous structures. Anodization produced a smooth Ti surface, whereas the surface roughness barely changed after FGF2 immobilization ( and ).
Table 2 Measurement of surface roughness by atomic force microscopy
Figure 1 Immobilized FGF2 compared with FGF2-free samples initially and after 9 days.
Abbreviations: FGF2, fibroblast growth factor 2; NT, nanotube; PT, polished titanium.
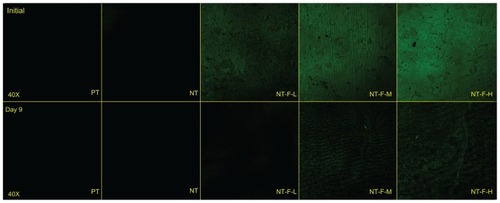
Figure 2 Field emission scanning electron microscopy results. (A) NT surface showed an NT array structure; NT-F-H surface showed clumps of fibroblast growth factor 2 and that the typical NT surface was changed. (B) Profile of titania NT.
Note: The length of NT was 588.85 ± 31.92 nm (mean value ± standard deviation).
Abbreviations: NT, nanotube; PT, polished titanium.
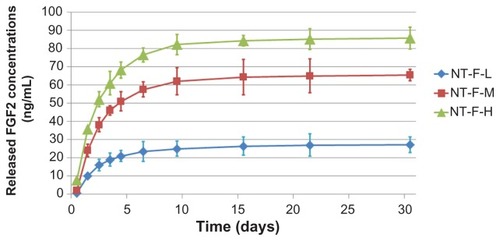
Elution kinetics of immobilized FGF2
Results of the elution kinetics are shown in and . The immobilized FGF2 was released from all the samples rapidly within the first 3 days, followed by a gradual reduction in the elution rate. On Day 9, over 90% of the dissolvable immobilized FGF2 had been eluted (with the total amount of dissolvable FGF2 in 30 days considered 100% likely elution). Almost all the dissolvable FGF2 was eluted in 21 days, after which (up to 30 days) the amount of additional elution was negligible.
Table 3 Elution of dissolvable FGF2 at different time intervalsTable Footnote*
Behavior of HGFs
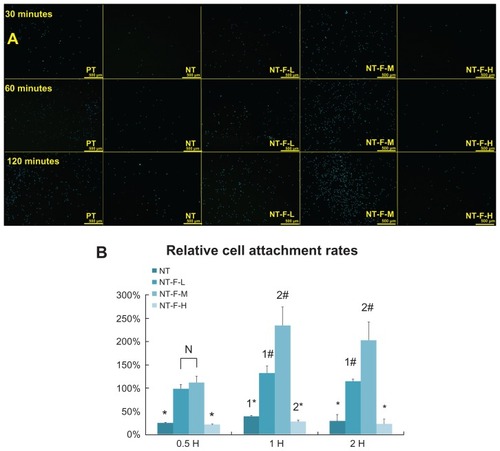
The HGF adhesion assay results are displayed in , and the RCAR results are shown in . The number of adhered cells on the NT-F-L and -M are significantly larger than those on the PT, NT, or NT-F-H at 30 minutes, 60 minutes, and 120 minutes (P < 0.01). NT-F-M shows the highest cell adhesion among the tested samples. Cell adhesion on NT and NT-F-H samples is significantly suppressed (<50%) compared with PT. The TiO2 NT array without FGF2 or with over FGF2 immobilization appears to impair HGF adhesion.
Figure 5 HGF adhesion. (A) HGFs attached to the substrates with 4′,6′-diamidino-2-phenylindole stain and (B) relative cell adhesion rate of attached HGFs. The NT and NT-F-H surfaces inhibited cell adhesion, whereas the NT-F-L and NT-F-M improved cell attachment.
Notes: #Higher than PT (P < 0.01), *lower than PT (P < 0.01), difference also exists between 1*, 2*, 1#, and 2# (P < 0.01).
Abbreviations: HGF, human gingival fibroblast; NT, nanotube; PT, polished titanium.
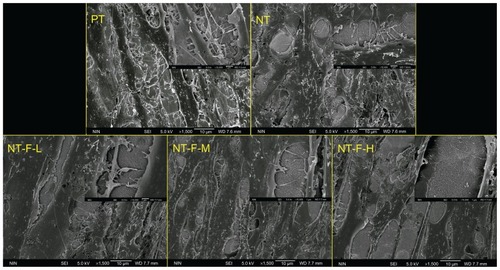
The results of the cell proliferation study are depicted in . Compared with PT, NT-F-L and NT-F-M have enhanced HGF proliferation at all time points, whereas NT shows enhanced proliferation on Day 3 only (P < 0.01). NT-F-H exhibited extremely low cell proliferation on Days 1 and 3, but improved HGF proliferation was noted on Days 6 and 9. Nevertheless, the enhanced effect of NT-F-H was not as substantial as that observed from NT-F-L and NT-F-M. The morphology of HGFs on the samples is displayed in . The observed morphological differences of HGFs among the PT, NT, NT-F-L, and NT-F-M samples are slight. The HGFs on the NT-F-H surface were narrow, with fewer prominences or pseudopods under normal conditions. Furthermore, HGFs on the NT-F-H surface did not fuse together or demonstrate any trend to form tissue-like structures during the time.
Figure 6 Cell proliferation measured by the methyl-thiazolyl-tetrazolium assay. NT-F-L and NT-F-M showed the higher cell proliferation at each interval, whereas NT-F-H with overimmobilized FGF2 showed the lowest at the early stage (Days 1 and 3).
Notes: #Higher than PT (P < 0.01), *lower than PT (P < 0.01), significant difference exists between 1# and 2# (P < 0.01).
Abbreviations: FGF2, fibroblast growth factor 2; NT, nanotube; OD, optical density; PT, polished titanium.
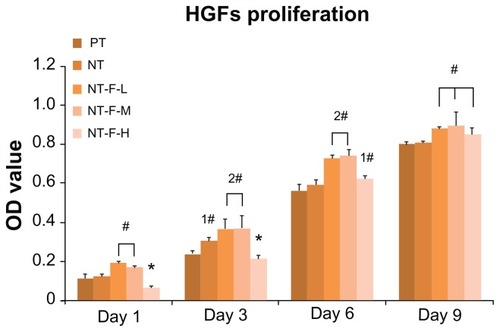
Figure 7 Morphology of HGFs: (A) PT, (B) NT, (C) NT-F-L, (D) NT-F-M, and (E) NT-F-H lacking sufficient prominences/pseudopods and not fusing together.
Abbreviations: HGF, human gingival fibroblast; NT, nanotube; PT, polished titanium.
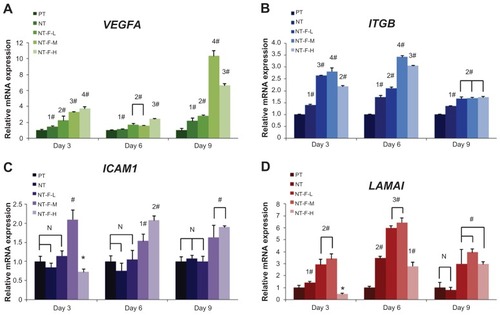
Adequate ECM-related gene expression is expected to realize wound healing and tissue regeneration. The results of ECM-related gene expression on different surfaces are shown in . The HGFs on NT-F-L and NT-F-M show beneficial ECM-related gene expression, and the details of the ECM-related gene expressions are summarized in .
Table 4 Summary of extracellular matrix-related gene expressions on Days 3, 6, and 9
Figure 8 Extracellular matrix-related gene expressions by HGFs cultured on four different titanium surfaces at Days 3, 6, and 9: (A) VEGFA, (B) ITGB, (C) ICAM1, and (D) LAMA1. Inverse concentration-dependent effects of NT-F-H were observed at Day 3 on (C) and (D).
Notes: #Upregulated compared with PT (P < 0.01), *downregulated (P < 0.01), significant difference exists between 1*, 2*, 1#, and 2# (P < 0.01).
Abbreviations: HGF, human gingival fibroblast; ICAM1, intercellular adhesion molecule 1; ITGB, β-integrin; LAMA1, laminin-1; NT, nanotube; PT, polished titanium; VEGFA, vascular endothelial growth factor A.
Bioactivity changes of immobilized FGF2
The changes in bioactivity of immobilized FGF2 are shown in . The activity of FGF2 was not significantly affected by repeated lyophilization-dissolving cycles but reduced gradually over time (NP ≈ S1 > S3 ≈ S6 > S9) at 37°C. After storing for 9 days (S9), the activity of FGF2 was reduced to less than 50% compared with NP. Proteolytic degradation may be the main reason for the loss of activity due to the absence of the protective ECM componentCitation32 in DMEM.
Figure 9 Activity changes of dissolvable FGF2 (10 ng/mL): control (FGF2-free); newly prepared Dulbecco’s modified Eagle’s medium; and S1, S3, S6, and S9 (FGF2 in Dulbecco’s modified Eagle’s medium stored for 1 day, 3 days, 6 days, or 9 days, respectively). The activity of FGF2 reduced gradually in culture medium with time and dropped to less than 50% after 9 days (S9) compared with NP.
Note: #Higher than PT (P < 0.01), significant difference exists between 1#, 2#, and 3# (P < 0.01).
Abbreviations: FGF2, fibroblast growth factor 2; NT, nanotube; OD, optical density; PT, polished titanium.
Discussion and conclusion
Unlike previous methods used to prepare microscale porous TiO2 films,Citation33,Citation34 in the present study, F+-based electrolyte anodization was used to obtain the TiO2 nanotubular surface on dental implants. However, in the transgingival part of a Ti dental implant, a smooth surface helps to maintain cleanliness. It has been shown that various types of cells have dissimilar reactions to different nanotubular surfaces of disparate tube sizes.Citation14–Citation16,Citation18,Citation35 Sterilization also affects the cytocompatibility of the TiO2 surface, and ultraviolet irradiation is one of the methods to improve the bioactivity of TiO2 without unexpected biological contamination.Citation35
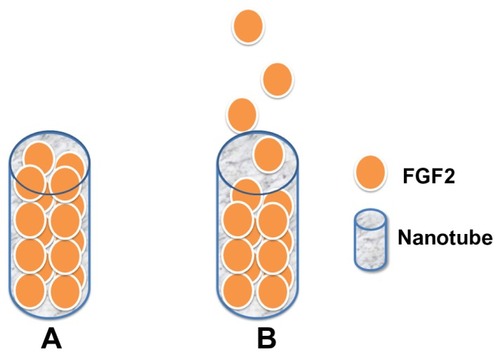
Application of FGF2 to periodontal tissue regeneration has been previously reported.Citation36,Citation37 FGF2 can be immobilized on to Ti surfaceCitation24 and hydroxyapatite-chitosan scaffolds.Citation38 The immobilization procedure used in this study as well as the chemical inertness and stability of TiO2 ensure that there is very little possibility for the FGF2 to react with the TiO2 NT array. Besides, using a TiO2 nanotubular surface for long-term drug elution is feasible due to its multitubular-like structure and ability to trap relatively small amounts of drug.Citation25 FGF2 (17 kDa) is approximately 1.45 nmCitation39 in hydrodynamic radius, and a biomolecule with such a small size is more likely to enter the inner space of the TiO2 NTs (). Intratube FGF2 storage may provide the possibility for an NT-based control release system. Although the total amount of immobilized FGF2 is difficult to quantify accurately, the elution kinetics of dissolvable immobilized FGF2 can be monitored with an enzyme-linked immunosorbent assay. The elution curves in this study are similar to those reported previously by Peng et al,Citation25 indicating that the length of the NT mainly affects the controlled release of immobilized FGF2.
Figure 10 Pattern of nanotube-based FGF2 control release system: (A) initial stage, (B) in culture medium, FGF2 is gradually released from the nanotubes.
Abbreviation: FGF2, fibroblast growth factor 2.
Compared with PT, NT and NT-F-H exhibit significantly suppressed cell adhesion probably because of the surface physicochemical properties and nanotopography. The TiO2 NT array has a multiringed shape with small initial cell- substrate contact areas. The hollow structure of the TiO2 NT array may also inhibit the formation of focal adhesion. Integrin clustering and focal adhesion reinforcement are not influenced by the nanoscale pits with a diameter of <70 nm irrespective of pit depth. However, increasing the size of the central lumen to >70 nm in these vertically aligned NTs significantly reduces cellular adhesion.Citation15,Citation40 In this study, the attachment of HGFs is better on NT-F-L and NT-F-M than on NT, probably due to FGF2 immobilization. This offers functional regions to accelerate cell attachment and increases the contact area between the cells and substrate. The main reason for the suppressed HGF attachment on NT-F-H may be the direct contact with the clumps of FGF2 on NT-F-H with over FGF2 immobilization. According to FE-SEM results and FGF2 elution kinetics, when the samples are immersed in the culture medium, the clumps of FGF2 dissolve rapidly, leaving the HGFs with a relatively unstable environment and making HGFs hard to attach.
Inverse concentration-dependent effect has been observed in the proliferation of HGFs on NT-F-H, which was much less than that on PT on Days 1 and 3, but gradually increased by Days 6 and 9. On the contrary, both NT-F-L and NT-F-M demonstrated excellent performance in terms of proliferation at all time points. Our results illustrate the enhanced behavior of fibroblasts in a medium with the appropriate concentration of eluted FGF2. Referring to the results in and , the activity and concentrations of eluted FGF2 from NT-F-L, -M, and -H are all suitable for cell proliferation within 3 days (10–100 ng/mL),Citation22 whereas NT-F-H shows extremely low proliferation. An unstable microenvironment is probably the main reason for this suppressive effect. On the NT-F-H surface, FGF2 dissolves within the first day and impedes the attachment of HGFs, therefore delaying their proliferation when compared with those on NT-F-L and NT-F-M. In all organ systems, the normal mammalian response to injury occurs in three overlapping but distinctive stages: (1) inflammation, (2) new tissue formation, and (3) remodeling. Stage 1 lasts for about 2 days after injury, whereas Stage 2 occurs 2–10 days after injury and is characterized by cellular proliferation.Citation41 Therefore, early proliferation of HGFs after implantation is crucial to healthy soft tissue sealing, and concentration-related impeded proliferation should be avoided.
In the morphogenesis of virtually all tissues, the ECM is essential and forms a structural framework possessing signal-transducing receptors that interact with cells. VEGFA enhances blood vessel growth and permeability and is a powerful mitogen for endothelial cells, fulfilling an important role in angiogenesis.Citation42,Citation43 Hence, an FGF2-immobilized TiO2 nanotubular surface may promote vascularization and further accelerate soft tissue regeneration around dental implants. In this work, the VEGFA expressions of NT, NT-F-L, -M, and -H are all upregulated, and NT-F-H shows the highest expression on Days 3 and 6. Overexpression of VEGFA may produce tissue inflammation or edema, thereby delaying tissue regeneration.
Integrins constitute the primary family of cell-surface receptors that mediate attachment to the ECM and substratesCitation44 and play a key role in early signal transduction.Citation45 In the integrin family, β-integrin is important in cellular binding on coated or textured Ti implants.Citation46 The total ITGB expression levels are concentration-dependent and increased by FGF2.Citation47 In this study, NT-stimulated ITGB is overexpressed at all time points, because the nanotubular surface hinders cellular attachment in the early stage but improves ITGB expression due to reverse compensation. NT-F-L, -M, and -H significantly enhance ITGB expression at all time intervals, and NT-F-M shows the highest gene expression among them on Days 3 and 6. However, this trend is not observed at Day 9. The probable reason may be that ITGB is richly expressed during the early stages. After cell-material integration has occurred, the expression of ITGB is less sensitive to the various concentrations of FGF2. Unlike VEGFA expression, excessive FGF2 does not give rise to a reverse effect but cannot fully exert its bioactivity. The TiO2 nanotubular surface is probably the main factor regulating ITGB expression after Day 9.
ICAM1, which is a widely expressed cell adhesion moleculeCitation48–Citation50 and belongs to the immunoglobulin super family, plays an important physiological role in routing polymorphonuclear neutrophils to the gingival sulcus efficiently and initiating a host response toward the implant. The expression of endothelial cell adhesion molecules (CAMs) for leukocytes, P-selectin, E-selectin, and ICAM1 is significantly upregulated in inflamed tissues by FGF2.Citation51 Our results reveal that the TiO2 nanotubular surface does not affect ICAM1 expression, and even the NT-F-L’s efficacy is nil. It is only when the concentration of FGF2 reaches a certain threshold that the effect is observed, thereby impairing (NT-F-H, , Day 3) or enhancing (NT-F-M , Days 3, 6, and 9; NT-F-H, , Days 6 and 9) ICAM1 expression. This effect may result in the increase of intercellular adhesion in the early stage as well as recruitment of polymorphonuclear neutrophils to produce anti-infective activity in the long term,Citation50 thereby improving the microecological environment around the dental implant.
Laminins are CAMs found predominantly in basement membranesCitation52 and may help to form a base for cell-substrate adhesion and improve the interface between cells (even epithelium) and dental implants. The mRNA levels of laminin in periodontal ligament cells are specifically upregulated by FGF2 stimulation.Citation36 In this study, both the TiO2 nano-tubular surface and FGF2 exhibit stimulated the LAMA1 expression. The inverse concentration-dependent effect was significantly observed on NT-F-H on Days 3 and 6 but diminished on Day 9.
From the perspective of cell adhesion, proliferation, and ECM-related gene expression, our results reveal that the functions of FGF2 immobilized on TiO2 nanotubular surface are definitely bidirectional as well as concentration- and time-dependent. The FGF2 solution with a concentration of 500 ng/mL is optimal for repeated lyophilization in spite of some loss of bioactivity with time. The TiO2 nanotubular surface might be ideal because its microstructure facilitates FGF2 immobilization, storage, and controlled release within 9 days. However, overimmobilization of FGF2 could lead to unwanted impairment of tissue healing and must therefore be avoided. Although the NT-based drug control release system needs further research for optimization, this FGF2/TiO2 nanotubular surface (NT-F-M) modification may lead to excellent gingival tissue-implant integration in vivo and has promising applications in dentistry and other biomedical devices.
Ethical approval
The Medical Ethics Committee of the School of Stomatology of the Fourth Military Medical University approved this study. The study adhered to the tenets of the Declaration of Helsinki. All three patients gave written informed consent.
Acknowledgments
This work was supported financially by the National Natural Science Fund No 81070862 and 31170915, City University of Hong Kong Applied Research Grants (ARG) No 9667038, and Hong Kong Research Grants Council (RGC) General Research Funds (GRF) No CityU 112510.
Disclosure
The authors report no conflict of interest relevant to this research.
References
- AdellRErikssonBLekholmUBranemarkPIJemtTLong-term follow-up study of osseointegrated implants in the treatment of totally edentulous jawsInt J Oral Maxillofac Implants1990543473592094653
- ArvidsonKBystedtHFrykholmAvon KonowLLothigiusEFive-year prospective follow-up report of the Astra Tech Dental Implant System in the treatment of edentulous mandiblesClin Oral Implants Res1998942252349760897
- OlssonMGunneJAstrandPBorgKBridges supported by free-standing implants versus bridges supported by tooth and implant. A five-year prospective studyClin Oral Implants Res1995621141217578781
- AbrahamssonIBerglundhTLindheJThe mucosal barrier following abutment dis/reconnection. An experimental study in dogsJ Clin Periodontol19972485685729266344
- LindheJBerglundhTThe interface between the mucosa and the implantPeriodontology 20001998171475410337312
- SchwarzFFerrariDHertenMEffects of surface hydrophilicity and microtopography on early stages of soft and hard tissue integration at non-submerged titanium implants: an immunohistochemical study in dogsJ Clin Periodontol2007781121712184
- AbrahamssonIBerglundhTLindheJSoft tissue response to plaque formation at different implant systems. A comparative study in the dogClin Oral Implants Res19989273799663034
- AbrahamssonICardaropoliGPeri-implant hard and soft tissue integration to dental implants made of titanium and goldClin Oral Implants Res200718326927417298489
- FaveriMGoncalvesLFFeresMPrevalence and microbiological diversity of Archaea in peri-implantitis subjects by 16S ribosomal RNA clonal analysisJ Periodontal Res201146333834421338359
- ShibliJAMeloLFerrariDSFigueiredoLCFaveriMFeresMComposition of supra- and subgingival biofilm of subjects with healthy and diseased implantsClin Oral Implants Res2008191097598218828812
- BrunetteDEffects of surface topography of implant materials on cell behavior in vitro and in vivoNanofabrication and Biosystems: Integrating Materials Science, Engineering, and Biology1996335355
- ZhaoLMeiSWangWChuPKWuZZhangYThe role of sterilization in the cytocompatibility of titania nanotubesBiomaterials20103182055206320022370
- GongDGrimesCVargheseOKTitanium oxide nanotube arrays prepared by anodic oxidationJ Mater Res2001161233313334
- BalasundaramGYaoCWebsterTJTiO2 nanotubes functionalized with regions of bone morphogenetic protein-2 increases osteoblast adhesionJ Biomed Mater Res A200884244745317618492
- ParkJBauerSvon der MarkKSchmukiPNanosize and vitality: TiO2 nanotube diameter directs cell fateNano Lett2007761686169117503870
- BrammerKSOhSCobbCJBjurstenLMHeydeHJinSImproved bone-forming functionality on diameter-controlled TiO2 nanotube surfaceActa Biomaterialia2009583215322319447210
- von WilmowskyCBauerSLutzRIn vivo evaluation of anodic TiO2 nanotubes: an experimental study in the pigJ Biomed Mater Res B Appl Biomater200989116517118780361
- DemetrescuIPirvuCMitranVEffect of nano-topographical features of Ti/TiO2 electrode surface on cell response and electrochemical stability in artificial salivaBioelectrochemistry201079112212920189888
- OrnitzDMItohNFibroblast growth factorsGenome Biol2001233005
- GerritsenMESorianoRYangSBranching out: a molecular fingerprint of endothelial differentiation into tube-like structures generated by affymetrix oligonucleotide arraysMicrocirculation2003101638112610664
- PalmonARoosHEdelJInverse dose- and time-dependent effect of basic fibroblast growth factor on the gene expression of collagen type I and matrix metalloproteinase-1 by periodontal ligament cells in cultureJ Periodontol200071697498010914801
- TakayamaSMurakamiSMikiYEffects of basic fibroblast growth factor on human periodontal ligament cellsJ Periodontal Res19973286676759409462
- PitaruSKotev-EmethSNoffDKaffulerSSavionNEffect of basic fibroblast growth factor on the growth and differentiation of adult stromal bone marrow cells: enhanced development of mineralized bone-like tissue in cultureJ Bone Miner Res1993889199298213254
- KokubuEYoshinariMMatsuzakaKInoueTBehavior of rat periodontal ligament cells on fibroblast growth factor-2-immobilized titanium surfaces treated by plasma modificationJ Biomed Mater Res A2009911697518767059
- PengLMendelsohnADLaTempaTJYoriyaSGrimesCADesaiTALong-term small molecule and protein elution from TiO2 nanotubesNano Lett2009951932193619323554
- HankemeierSKeusMZeichenJModulation of proliferation and differentiation of human bone marrow stromal cells by fibroblast growth factor 2: potential implications for tissue engineering of tendons and ligamentsTissue Eng2005111–2414915738660
- MustafaKSilva LopezBHultenbyKWennerbergAArvidsonKAttachment and proliferation of human oral fibroblasts to titanium surfaces blasted with TiO2 particles. A scanning electron microscopic and histomorphometric analysisClin Oral Implants Res19989319520710530134
- YoshinariMMatsuzakaKInoueTOdaYShimonoMEffects of multigrooved surfaces on fibroblast behaviorJ Biomed Mater Res A200365335936812746883
- KimS-YOhNLeeM-HKimS-ELeesungbokRLeeSWSurface microgrooves and acid etching on titanium substrata alter various cell behaviors of cultured human gingival fibroblastsClin Oral Implants Res200920326227219397638
- GeloverSGomezLAReyesKTeresa LealMA practical demonstration of water disinfection using TiO2 films and sunlightWater Research200640173274328016949121
- LivakKJSchmittgenTDAnalysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) methodMethods200125440240811846609
- SchultzGSWysockiAInteractions between extracellular matrix and growth factors in wound healingWound Repair Regen200917215316219320882
- SulYTJohanssonCBPetronisSCharacteristics of the surface oxides on turned and electrochemically oxidized pure titanium implants up to dielectric breakdown: the oxide thickness, micropore configurations, surface roughness, crystal structure and chemical compositionBiomaterials200223249150111761170
- ShibliJAGrassiSde FigueiredoLCInfluence of implant surface topography on early osseointegration: a histological study in human jawsJ Biomed Mater Res B Appl Biomater200780237738516850464
- ZhaoLMeiSChuPKZhangYWuZThe influence of hierarchical hybrid micro/nano-textured titanium surface with titania nanotubes on osteoblast functionsBiomaterials201031195072508220362328
- MurakamiSTakayamaSIkezawaKRegeneration of periodontal tissues by basic fibroblast growth factorJ Periodontal Res199934742543010685372
- NakaharaTNakamuraTKobayashiENovel approach to regeneration of periodontal tissues based on in situ tissue engineering: effects of controlled release of basic fibroblast growth factor from a sandwich membraneTissue Eng20039115316212625964
- AkmanACTigliRSGumusdereliogluMNohutcuRMbFGF-loaded HA-chitosan: a promising scaffold for periodontal tissue engineeringJ Biomed Mater Res A201092395396219291690
- FilionRJPopelASIntracoronary administration of FGF-2: a computational model of myocardial deposition and retentionAm J Physiol Heart Circ Physio20052881H263279
- BiggsMJRichardsRGDalbyMJNanotopographical modification: a regulator of cellular function through focal adhesionsNanomedicine20106561963320138244
- GurtnerGCWernerSBarrandonYLongakerMTWound repair and regenerationNature2008453719331432118480812
- JohnsonRBSerioFGDaiXVascular endothelial growth factors and progression of periodontal diseasesJ Periodontol199970884885210476891
- ConnollyDTVascular permeability factor: a unique regulator of blood vessel functionJ Cell Biochem19914732192231791186
- DiamondMSSpringerTAThe dynamic regulation of integrin adhesivenessCurr Biol1994465065177922371
- ClarkEABruggeJSIntegrins and signal transduction pathways: the road takenScience199526852082332397716514
- KramerPRJanikkeithACaiZMaSWatanabeIIntegrin mediated attachment of periodontal ligament to titanium surfacesDent Mater200925787788319217655
- SuzukiYYanagisawaMYagiHNakataniYYuRKInvolvement of beta1-integrin up-regulation in basic fibroblast growth factor- and epidermal growth factor-induced proliferation of mouse neuroepithelial cellsJ Biol Chem201028524184431845120371608
- CrawfordJMHoppBJunctional epithelium expresses the intercellular adhesion molecule ICAM-1J Periodontal Res19902542542561973732
- NorrisPPostonRNThomasDSThornhillMHawkJHaskardDOThe expression of endothelial leukocyte adhesion molecule-1 (ELAM-1), intercellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1) in experimental cutaneous inflammation: a comparison of ultraviolet B erythema and delayed hypersensitivityJ Invest Dermatol19919657637701708800
- MoughalNAAdonogianakiEThornhillMHKinaneDFEndothelial cell leukocyte adhesion molecule-1 (ELAM-1) and intercellular adhesion molecule-1 (ICAM-1) expression in gingival tissue during health and experimentally-induced gingivitisJ Periodontal Res19922766236301281230
- ZittermannSIIssekutzACBasic fibroblast growth factor (bFGF, FGF-2) potentiates leukocyte recruitment to inflammation by enhancing endothelial adhesion molecule expressionAm J Pathol2006168383584616507899
- DurbeejMLamininsCell Tissue Res2010339125926819693542