Abstract
As a major cause of low back pain, intervertebral disc degeneration is an increasingly prevalent chronic disease worldwide that leads to huge annual financial losses. The intervertebral disc consists of the inner nucleus pulposus, outer annulus fibrosus, and sandwiched cartilage endplates. All these factors collectively participate in maintaining the structure and physiological functions of the disc. During the unavoidable degeneration stage, the degenerated discs are surrounded by a harsh microenvironment characterized by acidic, oxidative, inflammatory, and chaotic cytokine expression. Loss of stem cell markers, imbalance of the extracellular matrix, increase in inflammation, sensory hyperinnervation, and vascularization have been considered as the reasons for the progression of intervertebral disc degeneration. The current treatment approaches include conservative therapy and surgery, both of which have drawbacks. Novel stimuli-responsive delivery systems are more promising future therapeutic options than traditional treatments. By combining bioactive agents with specially designed hydrogels, scaffolds, microspheres, and nanoparticles, novel stimuli-responsive delivery systems can realize the targeted and sustained release of drugs, which can both reduce systematic adverse effects and maximize therapeutic efficacy. Trigger factors are categorized into internal (pH, reactive oxygen species, enzymes, etc.) and external stimuli (photo, ultrasound, magnetic, etc.) based on their intrinsic properties. This review systematically summarizes novel stimuli-responsive delivery systems for intervertebral disc degeneration, shedding new light on intervertebral disc therapy.
Introduction
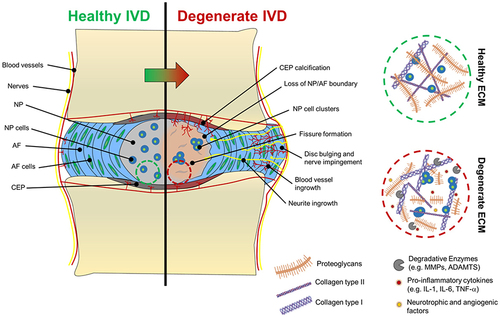
Intervertebral disc (IVD) degeneration (IVDD) is a major cause (40%) of low back pain (LBP), with a prevalence of over 11.9% in the population worldwide (over 568 million), which leads to huge economic losses estimated at 70 billion euros annually.Citation1–4 Epidemiological research in 195 countries found that LBP is the primary cause of years lived with disability in 126 countries.Citation5 As an essential structure in the human body, the intervertebral disc allows correct spatial alignment of vertebrae and facet joints, provides spinal mechanical stability, and enables segment movement.Citation6 The intervertebral disc comprises the nucleus pulposus (NP), annulus fibrosus (AF), and cartilage endplates (CEP). All these factors collectively participate in maintaining the structure and physiological functions of the disc.
The pathology of IVDD mainly includes dysfunction of intervertebral disc cells and an imbalance between anabolism and catabolism of the extracellular matrix (ECM).Citation7–10 Current IVDD treatments can be classified into conservative therapy (physical exercise and therapy, oral medication, and pain-relieving injections) and surgery.Citation11 Surgical treatments include intervertebral disc fusion (regarded as the standard method) and total disc replacement.Citation11 However, these IVDD treatment categories have unavoidable disadvantages. It is often difficult to achieve effective therapeutic outcomes with conservative physical treatments.Citation12 Moreover, owing to the avascular nature of the IVDs, it is difficult to achieve therapeutic concentrations of bioactive agents by systemic administration. The high doses of drugs required may cause multiple systemic side effects. Although local injections and interventional treatment can avoid this dilemma, repeated injections can cause adverse effects.Citation13 Simultaneously, the degenerated intervertebral disc features a harsh microenvironment, including acidic, oxidative, inflammatory, and chaotic cytokines, which is not conducive to medication.Citation14 However, surgical treatment is expensive, risky, and relapsable. IVD fusion eliminates the movement of the adjacent vertebral body, while total disc replacement induces a series of complications, including facet dislocation, pedicle fracture, device dislocation, and vertebral split fracture.Citation15–17
Biomaterial-based treatments have been widely researched to effectively alleviate the symptoms of IVDD and restore the disc structure. Various scaffolds, hydrogels, nanoparticles, and microspheres have been designed to relieve pain and restrain disc degeneration.Citation18,Citation19 Biomaterial-assisted interventions offer a significant advancement over traditional methods for treating IVDD, as they eliminate the need for multiple injections and circumvent the risk of widespread adverse effects, thereby providing a more efficient and safer therapeutic strategy. Moreover, biomaterials, such as hydrogels, have excellent biocompatibility and hypotoxicity.Citation20 Typically, biomaterials are effective for tissue regeneration and repair, which conventional treatments lack.Citation21 However, few biomaterials have shown significant effects in clinical trials, failing to address discogenic pain and maintain sustained therapeutic effects.Citation21 Therefore, novel smart therapeutic methods are needed to treat IVDD.
Conventional drug delivery systems include systemic administration (oral and intravenous) and local injections. Recently, researchers have focused on novel stimuli-responsive drug delivery systems that exhibit targeted and sustained drug release, with fewer invasive features.Citation22 By specially modifying functional polymers and wrapping them into various stimuli-responsive “shells”, these synthetics can effectively relieve pain and restore the metabolism of degenerated discs. Stimuli-responsive drug delivery systems are categorized based on internal stimuli, including pH, enzymes, and oxidative agents, and external stimuli, including temperature, photo, ultrasound, and magnetic field. In conclusion, special stimuli-responsive system presents a superior alternative to conventional IVDD treatment options, offering a more effective, safer, and personalized approach to managing IVDD. This review systematically summarizes novel stimuli-responsive drug delivery systems based on different stimulating factors, shedding new light on the intervertebral disc therapy field. This review encompasses a systematic search of Web of Science, Scopus, and PubMed from utilizing keywords including stimuli responsive, stimulus response, stimulation, disc, intervertebral disc degeneration, pH, enzyme, oxidative agents, photo, light, temperature, ultrasound, and magnetic. The search strategy was designed to be as inclusive as possible, ensuring a broad spectrum of available research is represented.
Anatomical and Molecular Structure of the Intervertebral Discs
The IVD is a major component of the spine. IVDs account for approximately 15–20% of the length of the spinal column, and their percentage depends on age, time of day, occupation, and disease state.Citation23 From the cervical region to the sacrum, at least 23 IVDs exist between the adjacent surfaces of the vertebrae to unite them, which is important for movement and load distribution.Citation24 Each IVD is structurally characterized by three integrated tissues: NP, AF, and CEP.Citation25 The AF surrounds the NP, and both are sandwiched between the CEP of the adjacent vertebrae.Citation23
AF
AF consists of highly organized collagen fibers arranged in 10–20 lamellae.Citation26 The thickness of each lamella ranges from 100 to 500 µm, in which the inner lamellae are thinner than the outer lamellae.Citation27,Citation28 Each lamella is inclined at approximately 30° from one vertebra to the other.Citation27 The fibers of the adjacent lamellae cross diagonally at angles >60°. Such arrangement enables limited rotation and bending between adjacent vertebrae and allows the IVD to withstand circumferential loads.Citation27,Citation29 Water represents 60–70% of AFCitation30 and the dry weight contains approximately 20% proteoglycan, 50–70% collagen, and 2% elastin.Citation23 AF can be further divided into an inner fibrocartilaginous region and an outer or peripheral fibrous zone.Citation31 The inner zone contains mainly type II collagen fibers generated by round chondrocyte-like cells, whereas the outer zone primarily contains type I collagen fibers produced by elongated, fusiform, fibroblast-like cells of mesenchymal origin.Citation29,Citation32,Citation33 Other differences between the inner and outer regions include the distribution of decorin and biglycan, which are mainly found in the outer annulus.Citation23
NP
As the core of the IVD, the NP is derived from the notochord and cartilaginous cells, with a few irregular collagen fibers disseminated in a semiliquid medium.Citation34 The fluidic nature of NP enables their deformation under pressure without volume changes. Regarding chemical composition, 70–90% of NP is water, and the dry weight consists of approximately 35–65% proteoglycan, 5–20% type II collagen, and a small amount of non-collagenous proteins and elastin.Citation24 Proteoglycan can store water and reduce the stress of IVD by distributing the hydraulic pressure to the ECM.Citation35,Citation36 NP cells are a hybrid group of cells in different phases of maturation that sustain tissue homeostasis.Citation37 In newborn and premature tissues, NP cells are large and highly vacuolated (often referred to as “notochordal cells”), occurring in clusters with tight intercellular junctions and a compact cytoskeletal network.Citation38–40 In adults, the cell density of NP is low, and large notochordal cells morphologically transform into small fibrochondrocyte-like cells.Citation41 Tang et al confirmed a new set of NP markers (brain abundant membrane attached signal protein 1 (BASP1), neurochondrin (NCDN), neuropilin 1 (NRP1), cluster of differentiation (CD)24, CD155, CD221, and Brachyury T) and one non-NP marker (CD90), which have the potential to reveal shifts in NP cell phenotype and function during degeneration.Citation42 With respect to the ECM, the NPCitation23 features abundant collagen types I and II and scarce types IX and XI. Collagen type X is present during degeneration.Citation23 Based on the physiological characteristics of the blood supply, the disc exhibits low oxygen tension. In this case, the NP cells rely almost completely on the glycolytic pathway to generate energy.Citation43
End Plates
End plates form the boundaries of adjacent intervertebral discs and are composed of bony endplates (BEP) and CEP. The actual width of the CEP is approximately 0.6–1 mm. Moreover, CEP have a water content of about 60%, and the main dry-weight components are type II collagen and proteoglycans.Citation24 The predominant cell type within the CEP is chondrocytes.Citation23 CEP form a functional structure that connects the IVD and adjacent vertebrae via the adjacent BEP.Citation25 Moreover, CEP serve as a mechanical barrier between the NP and vertebrae, which prevents direct pressure on the bone.Citation23 CEP also serve as a gateway for nutrient transport into the disc.Citation44 In addition, hyaline cartilage is present in neonates and children, whereas adult CEP are fibrocartilage.Citation34 Collagen fibers in the CEP and vertebrae are originally separated and can be dislocated by excessive horizontal stresses.Citation45,Citation46
Blood Supply and Innervation
In general, vessels and nerves are concomitant within the IVD. IVD is an avascular tissue with a limited blood supply to the peripheral fibers of the AF.Citation47 The CEP have branched blood vessels from the spinal artery in the fetus that disappear with aging.Citation48 Nutrients and metabolic waste products are delivered by diffusion from outer annulus blood vessels.Citation49 Regarding innervation in the IVDs, the NP has no nerve supply,Citation50 while the AF has limited nerves that are mainly restricted to the outer lamellae, with some terminating in the proprioceptor.Citation51 The nerves are branches of the sinus vertebral nerve, which consists of a combination of somatic nerve roots from the ventral ramus and autonomic nerve roots from the gray ramus.Citation47 Some nerves in the IVD contain glial support cells or Schwann cells. Clinically, many pathological changes, such as osteosclerosis, altered blood flow, and CEP calcification, can affect vascular transportation, which, in turn, may lead to cell death. The NP has the poorest blood supply in the IVD and is consequently susceptible to injury.Citation49
Pathological Alterations and Microenvironments in IVDD
AF Degeneration
The major pathological alteration of the AF in IVDD is a change in the distribution of collagen fibers. The mechanism theory is the “wear and tear”, which means that the ECM remolding can be accelerated by high mechanical stress.Citation52 In IVDD, the level of outer tension-resisting type I collagen increases, while that of inner compression force-combating type II collagen decreases.Citation53,Citation54 Consequently, with the changes in the types of collagen, the ability of AF to resist shear stress decreases, which leads to morphological changes in IVDs and the progression of IVDD.Citation55 Moreover, the drastic microenvironment in IVDD restrains AF regeneration. Early AF repair may be an ideal therapeutic strategy for IVDD.Citation56 Mechanistically, overexpression of cytokines, including cyclooxygenase-2, interleukin (IL)-6, and IL-8, leads to the formation of an inflammatory microenvironment and changes in collagen types.Citation57,Citation58
NP Degeneration
IVD can lead to long-term spinal dysfunction and instability. Generally, compared to a healthy NP, a degenerated NP features unorganized fibrous tissue, which makes it difficult to bind water under compression.Citation59 Consequently, both the pressure in the NP and the disc height decrease.Citation60,Citation61 Degenerative factors include biological and biomechanical factors that play crucial roles in the pain signaling pathway and cause clinical symptoms.Citation62 IVDD can develop as early as the first decade of life. The notochordal cells in the NP gradually disappear as the body grows, and this reduction is considered the initiation process of disc degeneration.Citation6,Citation63 Apoptosis and autophagy cause these cellular alterations. The cells in the NP change from notochordal cells to nuclear chondrocytes.Citation3 Mature nuclear chondrocytes mainly produce collagen type I and reduce the amount of water-attracting proteoglycans and collagen type II, resulting in the transition to fibrillated NP tissue.Citation64 Such cell type changes cause a decrease in proteoglycan synthesis; thus, tissue hydration is lost, which further affects the ability of the NP to maintain its structure and composition.Citation65,Citation66
Furthermore, in IVDD, the balance between ECM synthesis and catabolism is disrupted due to a decrease in cell number.Citation67 Inflammation also mediates ECM degradation. As demonstrated, the proinflammatory factors, such as IL-1β and tumor necrosis factor (TNF)-α,Citation68,Citation69 could accelerate the matrix remodeling in IVDD. IL-1β and TNF-α can stimulate the matrix-degrading enzymes, including matrix metalloproteinase (MMP)-2, MMP-1, MMP-13, MMP-3, MMP-14, a disintegrin and metalloproteinases with thrombospondin motifs (ADAMTS)-4, and ADAMTS-5.Citation70,Citation71 In comparison, the levels of ECM enzyme inhibitors of MMPs tissue inhibitor of metalloproteinase (TIMP)-1, and TIMP-2 are reduced.Citation72 Long-lasting proteoglycan loss and collagen type alterations contribute to the degeneration of the NP.
Endplate Degeneration
Moore et al pointed out that blood vessels in the CEP become narrowed, constricted, or even disappear as they mature, a change that is likely to affect the nutrient supply to the cartilage and discs.Citation73 With aging, the endplate gradually undergoes calcification, which also affects the nutrient supply to the IVD. Moreover, the endplate becomes thinner with age, increasing the risk of endplate fracture.Citation74 Furthermore, the displacement of the damaged CEP leads to a decreased NP pressure (estimated at 30–50%) and an uneven load distribution.Citation75 The magnetic resonance imaging (MRI) signal of the vertebral endplate and subchondral bone changes in patients with IVDD, providing complementary diagnostic evidence.Citation76 Such MRI changes are named “Modic” changes. Type 1 Modic changes refer to hypointensity on T1-weighted imaging (T1WI) and hyperintensity on T2-weighted imaging (T2WI); Type 2 changes refer to hyperintensity on T1WI and isointensity or slight hyperintensity on T2WI; Type 3 changes refer to hypointensity on both T1WI and T2WI.Citation77
Overall, compared to a non-degenerated IVD, a degenerated IVD features a loss of disc height, a fibrous dehydrated nucleus, inward and outward buckling of annulus fibers, extensive endplate damage, and sclerosis of the subchondral bone ().
Figure 1 Macroscopic and microscopic changes of the IVDD during degeneration. Characteristic changes of the NP’s ECM after degeneration are illustrated in the dashed circles. ECM of degenerated discs (dashed red circle) shows shorter aggrecan macromolecules and more collagen type I fibres (thicker fibre bundles) than collagen type II (thinner collagen bundles), which are largely abundant in the ECM of healthy discs (dashed green circle). Reprinted from Costăchescu B, Niculescu AG, Teleanu RI, et al. Recent advances in managing spinal intervertebral discs degeneration. Int J Mol Sci. 2022;23(12):6460. Creative Commons.Citation78
Harsh Microenvironment in IVDD
As is widely acknowledged, degenerated IVDs exhibit harsh microenvironments, such as inflammatory, oxidative, and acidic environments. The production of other bioactive agents, such as enzymes and cytokines is also abnormal. Meanwhile, both NP and AF cells secrete high levels of proinflammatory cytokines, such as TNF-α, interferon-γ (IFN-γ), IL-1β, IL-10, IL-4, IL-6, IL-17, IL-2, IL-8, and C-C chemokine ligand 20 (CCL20).Citation79,Citation80 Such harsh microenvironments are detrimental to disc cell metabolism and tissue regeneration. The inflammatory microenvironment exacerbates the dysfunction and abnormal apoptosis of disc cells, leading to further ECM degradation and disruption. Based on these features, a novel and promising stimuli-responsive drug delivery system can be specially constructed, which produces precise and sustained IVDD treatment while reducing adverse impact factors.
Internal Stimuli-Responsive Delivery Systems for IVDD
Redox-Responsive System
The IVDD microenvironment features an increased expression of reactive oxygen species (ROS), which induces the progression and deterioration of IVDD. ROS includes oxygen-derived molecules and high-reactivity free radicals, including hydrogen peroxide (H2O2), hydroxyl radicals (•OH), and superoxide anion radicals (O2−•).Citation81,Citation82 The excessive level of ROS leads to the overexpression of catabolic factors, such as TNF-α, MMPs, and aggrecanases, causing dramatic histological changes. Moreover, decreased levels of antioxidant substances aggravate the oxidative microenvironment in IVDD.Citation83 Thus, therapeutic strategies for reducing ROS and ROS-induced inflammation are considered promising options for attenuating disc catabolism and restoring disc anabolism. High levels of ROS can be a suitable stimulus for drug delivery systems.
Zhang et al constructed ROS-responsive magnesium-containing microspheres (Mg@PLPE MSs) as a new ROS-responsive drug delivery system that could realize the controlled release of hydrogen gas (H2).Citation84 Constructed in a core-shell format, the core component is magnesium microparticles, and the exposed shell is developed using the ROS-responsive polymers poly(polybutylene terephthalate [PBT]-co-ethylene glycol dimethacrylate (EGDM) and poly(lactic-co-glycolic acid) (PLGA). The specific design and combination of PBT-co-EGDM and PLGA can achieve ROS-targeted migration and a hydrophobic-to-hydrophilic transition through a reaction with the overproduced H2O2 in the degenerated disc. Then, the Mg-water reaction starts, and H2 is produced continuously, which further reduces the ROS level of the degenerated discs by reacting with oxidative substances. The efficiency of this ROS-responsive drug delivery system was verified in vivo using a puncture-induced rat IVDD model, and the results showed biocompatibility, negligible toxicity, and excellent treatment outcomes.Citation84
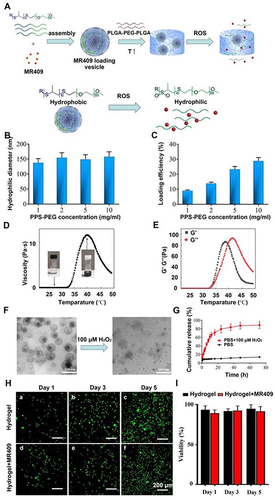
Moreover, Wang et al constructed a special ROS-responsive vesicle hydrogel to alleviate disc degeneration in a rat model, which featured a peptide core component named mineralocorticoid receptor (MR)409.Citation85 The underlying mechanism is that MR409 modulates the secretory autophagy of NP cells by regulating disease-associated inflammation, immune infiltration, and IL-1β synthesis.Citation85–88 MR409 was loaded onto a special ROS-responsive poly(propylene sulfide) (PPS)-poly(ethylene glycol) (PEG) (PPS-PEG) amphiphilic polymer. Eventually, the MR409-loading vesicles were embedded in a thermosensitive PLGA-PEG-PLGA hydrogel (). This special hydrogel is thermosensitive and protects the internal materials from harsh microenvironments. The MR409-vesicle-hydrogel was tested in a rat model and demonstrated to be valid for disc degeneration treatment.Citation85
Figure 2 A new injectable thermosensitive hydrogel with ROS-sensitive MR409-loaded vesicles demonstrates sustained controlled release and biocompatibility. (A) Schematic illustration of the thermosensitive hydrogel loaded with ROS-responsive PPS-PEG vesicles for controlled release of MR409. (B) Hydrodynamic diameters and (C) MR409-loading efficiencies of PPS-PEG vesicles. (D) Viscosity of the PLGA-PEG-PLGA solution containing MR409-loaded vesicles as a function of temperature. (E) G’ and G” of the PLGA-PEG-PLGA solution containing MR409-loaded vesicles as a function of temperature. (F) Change in the morphology of MR409-loaded vesicles in the presence of external H2O2 (100 µM). (G) Cumulative release of MR409 from PPS-PEG vesicles or hydrogel containing vesicles in the presence of 100 µM H2O2. (H and I) Images of live/dead cell staining (H) and quantitation (I) of rat NP cells cultured with hydrogel confirming good biocompatibility. Reprinted from Zheng Q, Shen H, Tong Z, et al. A thermosensitive, reactive oxygen species-responsive, MR409-encapsulated hydrogel ameliorates disc degeneration in rats by inhibiting the secretory autophagy pathway. Theranostics. 2021;11(1):147–163. Creative Commons.Citation85
Isoginkgetin (IGK), a natural flavonoid extracted from Ginkgo biloba leaves, can enhance autophagy and scavenge ROS. Yu et al constructed a ROS-responsive IGK-loaded nanodelivery system (IGK@SeNP) and achieved its smart release under the stimulation of excessive ROS.Citation89 The IGK@SeNP system contained Se-Se bonds and exhibited excellent biocompatibility. Se-Se bonds and IGK play a joint role in clearing ROS. Simultaneously, the targeted and controlled release of IGK increases autophagy in NPCs, which maintains the balance between the anabolism and catabolism of the ECM. Further testing in a rat needle puncture IVDD model showed that this intelligent system has superior efficacy for treating IVDD in vivo.Citation89
Bai et al designed an in situ-formed rapamycin-loaded ROS-scavenging scaffold and offered a new strategy for promoting IVDD tissue regeneration.Citation90 In an oxidative environment, the scaffold consumed ROS and gradually released rapamycin. Rapamycin reduces the inflammatory response and promotes the regeneration of disc cells by promoting macrophage polarization toward an anti-inflammatory M2-like phenotype. In a rat IVDD model, this ROS-scavenging scaffold showed significant effects in in vivo experiments.Citation90
Enzyme-Responsive System
Enzyme-responsive features have excellent biocompatibility and high catalytic efficacy, which enable the targeted migration of therapeutic substances to injury sites.Citation88 In the pathological state of IVDD, enzymes with elevated levels include MMP, hyaluronidase (HA), and ADAMTS.Citation91–93 Possessing the ability to catalyze chemical reactions, enzymes overexpressed in IVDD are ideal stimuli for enzyme-responsive delivery systems.
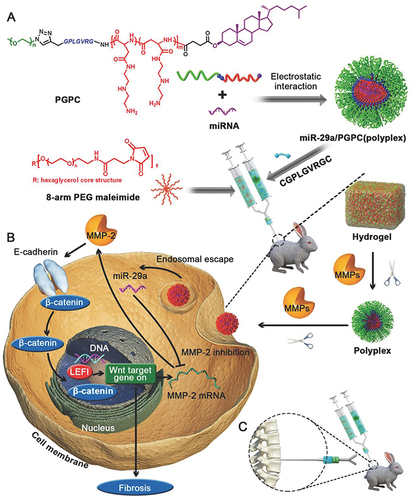
The micro-ribonucleic acid (RNA) (miRNA)-29 (miR-29) family (miR-29a, miR-29b, and miR-29c) is involved in tissue fibrosis and is crucial for inhibiting abnormal fibrosis and collagen transition.Citation94–98 Ge et al designed a valuable complex named MMP-responsive miR-29a polyplex micelles to achieve precise and efficient delivery while maintaining the integrity of miRNAs.Citation99 This MMP-responsive shell is composed of MMP-responsive PEG/ CGPLGVRGC peptide hydrogels and PEG-GPLGVRG-poly{N′-[N-(2-aminoethyl)-2-aminoehtyl]aspartamide}-cholesteryl (PEG-GPLGVRG-PAsp(DET)-Chole) (PGPC). The peptide linkage (GPLGVRG) of the shell can be decomposed by the overproduction of MMPs. This special delivery system includes two MMP-responsive processes and enables a more accurate and efficient miRNA delivery for IVDD treatmentCitation99 ().
Figure 3 (A) Schematic illustration for formation of miRNA/PGPC polyplex micelles. (B) Encapsulation of miRNA/PGPC polyplexes in PEG hydrogels in an injectable manner and molecular mechanism of MMP-2 silence in nucleus pulposus cells for fibrosis inhibition. (C) Injection sites in the IVDs of rabbits. Reprinted from Feng G, Zha Z, Huang Y, et al. Sustained and Bioresponsive Two-Stage Delivery of Therapeutic miRNA via Polyplex Micelle-Loaded Injectable Hydrogels for Inhibition of Intervertebral Disc Fibrosis. Adv Healthc Mater. 2018 Nov;7(21):e1800623. VCH Verlag GmbH & Co. KGaA, Weinheim.Citation99
In addition, stem cell therapy using mesenchymal stem cells (MSCs) and pluripotent stem cells is a crucial IVDD treatment approach that features fewer autoimmune reactions and fewer side effects.Citation100,Citation101 NP progenitor cells (NPPCs) are ideal tissue-specific stem cells for IVDD regeneration. However, because of the harsh microenvironment (hypoxia, acidity, and inflammation) of the degenerated disc, stem cell therapy often results in poor outcomes.Citation101 To overcome this obstacle, Tang et al designed an esterase-responsive ibuprofen copolymer nanomicelle (PEG- polyisobutene) that modified embryo-derived NPPCs for IVDD treatment. As an effective inflammatory inhibitor, ibuprofen is suitable for protecting NPPCs. To resolve the fast degradation speed of direct ibuprofen injection, researchers constructed esterase-responsive nanomicelle-premodified NPPCs, which achieved a sustained release of ibuprofen and protected NPPCs during IVDD regeneration.Citation102 The production process of this special delivery system is illustrated in .
Figure 4 General schematic of synthesis of esterase-responsive ibuprofen nano-micelles (PEG-PIB) to pre-modify embryo-derived long-term expandable nucleus pulposus progenitor cells (NPPCs) for synergistic transplantation in intervertebral disc degeneration. Reprinted from Xia KS, Li DD, Wang CG, et al. An esterase-responsive ibuprofen nano-micelle pre-modified embryo derived nucleus pulposus progenitor cells promote the regeneration of intervertebral disc degeneration. Bioact Mater. 2023;21:69–85. Creative Commons.Citation102

Hydrogen sulfide (H2S) has been used to treat many diseases, including cardiac diseases, skin injury, and neuronal degeneration.Citation103–105 H2S participates in signal transduction and protects the cells from apoptosis. Some studies have shown that it can upregulate antioxidant expression and reduce inflammation through macrophage polarization.Citation103 However, although H2S has been demonstrated to be effective in suppressing the degeneration process of NP cells, there is a huge obstacle to the production and accumulation of H2S, and the quick volatilization of H2S gas limits its clinical usage. Considering these difficulties, Xiao et al developed a pH and enzyme dual-responsive H2S release system, named collagen-JK1 hydrogel (Col-JK1), for IVDD treatment.Citation106 This specially designed H2S release system included the core component of a pH-responsive H2S donor, named JK1, and a carrier of the MMP-responsive collagen hydrogel. This unique combination resulted in sustained H2S release and retention in situ. The in vivo results showed that the Col-JK1 significantly reduced the apoptosis of NP cells. H2S participated in and regulated the nuclear factor (NF)-κB signaling pathway.Citation106
pH-Responsive System
The normal human tissues possess an extracellular pH of 7.4.Citation107 The pH of the normal IVD is estimated to be 7.1; however, the pH in mildly, moderately, and severely degenerated IVDs is reported as 6.8, 6.5, and 6.2, respectively.Citation108,Citation109 The acidic microenvironment of NP tissues is also a detrimental factor in IVDD. Accordingly, acidic microenvironments can lead to abnormal cell damage and apoptosis.Citation110 Other studies have demonstrated that lower pH results in increased expression of acid-sensing ion channel-3 (ASIC-3), which is considered novel therapeutic targets.Citation109
Zeolite imidazolate framework-8 is a metal–organic framework (MOF) with a large surface area and good degradability in acidic microenvironments. Protocatechuic acid (PCA) is a phenolic compound extracted from traditional Chinese herbs that promotes chondrocyte regeneration. Recently, Ding et al designed an intelligent drug delivery system named MOF@PH that could release PCA under the stimulation of an acidic environment at the degenerated disc. MOF@PH satisfactorily inhibited IVDD progression in a rat model.Citation111
Wang et al associated H2 therapy with hollow polydopamine (HPDA) to achieve sustained H2 release from a degenerated disc. They used HPDA as a pH-responsive carrier and developed ammonia borane (AB) as a source of H2. This specially designed complex, called AB@HPDA, is characterized by a large surface area, high biocompatibility, and permeability.Citation112 The complex is incorporated into the nanoparticles and can be injected at degenerated positions. In vivo experiments showed that this injectable nanoparticle significantly reduced tissue oxidative damage by the pH-responsive delivery of H2 and restored normal physiological functions.Citation112
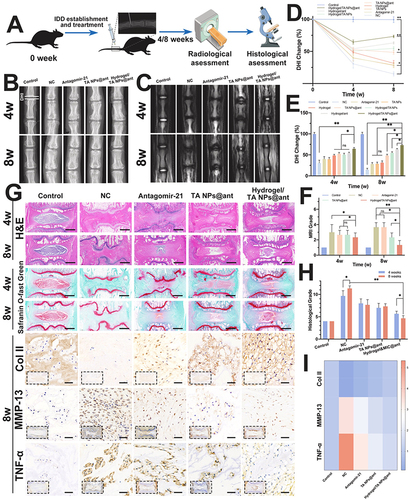
Wang et al designed another novel injectable and pH-responsive miRNA delivery system, Ta nanoparticles@antagomir-21, which has great potential for regulating ECM metabolism in NP tissues. The surrounding hydrogel is formed by glycidyl methacrylate (GMA)-modified carboxy-methyl chitosan (CMC-GMA), which can achieve a two-stage inflammation-triggered on-demand delivery of antagomir-21.Citation113 In vivo experiments confirmed the efficacy of the multifunctional delivery system (). Researchers have also explored the mechanism of antagomir-21 in degenerated NP cells, demonstrating that antagomir-21 is a mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK) signaling pathway regulator.Citation113
Figure 5 In vivo therapeutic effects in a rat IVDD model. (A) Schematic illustration showing the overall processes of animal experiments. (B) X-ray and (C) MRI images of rat coccygeal vertebral discs at different time points indicated that the height and water content of the degenerative intervertebral disc were significantly improved after treatment with the Hydrogel/TA NPs@ant. (D and E) The changes in DHI and (F) MRI grade at 4 and 8 w quantitatively confirmed the repair effect of IVDD implanted with Hydrogel/TA NPs@ant. (G) Representative images of H&E, safranin-O/fast green, Col II, MMP-13 and TNF-α immunohistochemical staining of different treatments at 4 and 8 w (scale bars, 1 mm (for H&E, safranin-O/fast green), 50 μm (for immunohistochemical staining)). The histological results further confirmed the role of the Hydrogel/TA NPs@ant in improving the metabolic balance of the ECM in degenerative nucleus pulposus and inhibiting the infiltration of inflammatory factors. (H) The histological grades in different groups further proved the synergistic effect of antagomir-21, TA NPs and the hydrogel on nucleus pulposus regeneration. (I) Heatmap represents the total intensity of Col II, MMP-13 and TNF-α immunohistochemical staining in nucleus pulposus of different treatments at 8 w. Reprinted from Biomaterials, volume: 298, Wang Y, Wu Y, Zhang B, et al. Repair of degenerative nucleus pulposus by polyphenol nanosphere-encapsulated hydrogel gene delivery system. 122132. Copyright 2023, with permission from Elsevier.Citation113
Temperature-Responsive System
In general, the properties of a temperature-responsive delivery system can shift to another morphology as the surrounding temperature changes, and the embedded cargo can then be released. Temperature-sensitive hydrogels are ideal matrices for engineered cartilage and spine construction.Citation114 Temperature-sensitive materials are critical components of the temperature-responsive delivery system, which mainly include poly(N-isopropylacrylamide),Citation115 poly(amidoamine),Citation116 poly(2-oxazoline),Citation117 and poly[2-(2-methoxyethoxy) ethyl methacrylate].Citation118 Based on previous studies, the currently promising temperature-responsive delivery systems for IVDD treatment can be classified into three categories.
Cell-Encapsulated Temperature-Responsive Delivery System
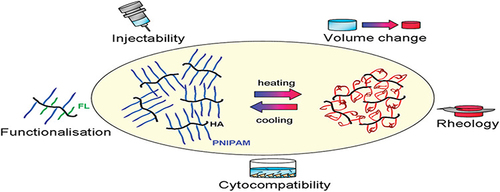
Based on modified polysaccharides with temperature-sensitive polyamides, poly(N-isopropylacrylamide) (pNIPAM), the temperature-sensitive hydrogel (TR-HG) is liquid at room temperature and hardens over 32 °C (). Malonzo et al used a papain-induced disc degeneration model to assess a temperature-sensitive hydrogel cell therapeutic approach. The results showed no significant changes in the activity of NP cells after TR-HG+NP cells were injected into the discs, illustrating the cytocompatibility and practicability of TR-HG. By further examining gene expression in AF tissues from TR-HG and TR-HG+NP cell-treated discs, researchers found that the IVD tissues responded differently to the gel+cell mixtures than to the pure gel. This phenomenon indicates that the potential of TR-HG partly depends on the cell signaling (IL-6β and IL-1β) of the NP cells.Citation119
Figure 6 Various properties of the temperature-sensitive material hyaluronan-poly(N-isopropylacrylamide) HA-pNIPAM. Reprinted with permission from Mortisen D, Peroglio M, Alini M, Eglin D. Tailoring thermoreversible hyaluronan hydrogels by “click” chemistry and RAFT polymerization for cell and drug therapy. Biomacromolecules. 2010;11(5):1261–1272. Copyright {2010} American Chemical Society.Citation114
HA is the preferred cellular delivery platform because it is a major component of the ECM in connective, epithelial, and neural tissues. However, the unmodified hyaluronic acid solutions exhibited rapid degradation and clearance after implantation.Citation120 Based on the above backgrounds, Guo et al introduced an HA-based hybrid interpenetrating polymer network (IPN), which could be used to deliver NP cells and repair nucleotomized IVDs. The components of HA–IPN include pNIPAM and 1.4-butanediol diglycidyl ether (BDDE). Both pNIPAM and BDDE supported the survival and differentiation of embedded NP cells. The characteristics of HA-IPN, such as its swelling properties, cytocompatibility, and support for ECM deposition, were excellent in vitro.Citation121
Nucleic Acid-Encapsulated Temperature-Responsive Delivery System
miRNAs are a class of small, non-coding, endogenous RNA molecules that direct the function of corresponding messenger RNAs.Citation122 Previous studies have demonstrated that miRNAs are crucial for IVDD progression.Citation123,Citation124 The miRNA-25-3p could precisely silence the targeted metal regulatory transcription factor 1 (MTF1) protein expression and inhibit IL-1β-induced effects.Citation125 However, miRNAs and negatively charged mimics cannot cross cell membranes, and the “naked” miRNAs are highly susceptible to degradation in serum.Citation126
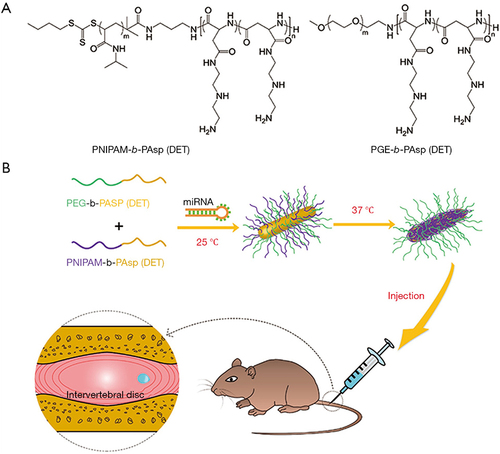
Based on this background, Huang et al constructed a novel temperature-responsive carrier formed by mixed cationic block copolymers (MCBCs), PEG-b-poly [Poly(L-Aspartic acid) (PAsp)(DET)], and PNIPAM-b-PAsp(DET).Citation125 As the temperature increased from room temperature (25 °C) to physiological temperature (37 °C), the PNIPAM-b-PAsp(DET) formed a hydrophobic PNIPAM core in the micellar structure, which facilitated gene transfection and stability.Citation127,Citation128 High efficiency of the temperature-responsive vector MCBC was observed, and miRNA-25-3p was effectively delivered in rat modelsCitation125 ().
Figure 7 Schematic illustration of miRNA-based gene therapy delivered by a thermo-responsive vector for intervertebral disc degeneration (IVDD). (A) The chemical structure of cationic block copolymers: PNIPAM-b-PAsp (DET) and PEG-b-PAsp (DET). (B) The mixed cationic block copolymers (MCBC) PNIPAM-b-PAsp (DET) and PEG-b-PAsp (DET) as vectors for miRNA to form mixed polyplex micelles. With a temperature increase from room temperature (25 °C) to physiological temperature (37 °C), thermo-sensitivity of PNIPAM segments become hydrophobic and form more compact mixed polyplex micelles with hydrophobic and hydrophilic heterogeneous surfaces. The mixed cationic block copolymers delivered miRNA-25-3p for IVDD gene therapy. Reprinted from Huang Y, Huang L, Li L, et al. MicroRNA-25-3p therapy for intervertebral disc degeneration by targeting the IL-1β/ZIP8/MTF1 signaling pathway with a novel thermo-responsive vector. Ann Transl Med. 2020;8(22):1500. Creative Commons.Citation125
Bioactive Agent-Encapsulated Temperature-Responsive Delivery System
Previous studies have demonstrated that bioactive agents, such as simvastatin, alleviate IVDD deterioration by stimulating endogenous bone morphogenetic protein (BMP)-2 expression.Citation129 To further test and promote therapeutic efficacy, researchers have combined simvastatin with novel delivery systems. Zhang et al constructed a special simvastatin-loaded PEG-PLGA-PEG gel, which showed significant effects on disc regeneration.Citation130 By incorporating simvastatin into the temperature-sensitive liquid PEG-PLGA-PEG gel, the exposure of IVD cells to simvastatin was confined to the disc core, as the compound is converted to the gel phase after reaching body temperature.Citation130 Moreover, the use of the PEG-PLGA-PEG hydrogel reduced the instantaneous drug concentration and enabled sustained therapy. Such triblock polymers are widely used as drug-controlled vehicles for gene delivery.Citation131–133
External Stimuli-Responsive Delivery Systems for IVDD
Photo-Responsive System
Photo, as a stimulus for biomaterials, provides non-invasive precision and physiological benignity, essential for advanced biomedical applications.Citation134 The cargo delivered by the photoresponsive system includes cells and bioactive substances. Photosensitive biomaterial-embedded agents are activated by photoisomerization, photolysis, photo-crosslinking, photo-oxidative reduction (which can be applied to photodynamic therapy), and photothermal triggering (which is related to photothermal therapy).Citation135
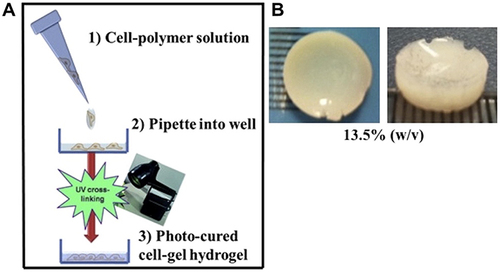
Chen et al combined a photo-crosslinked gelatin (Gel)-HA methacrylate (MA) (HAMA) (GelHA) hydrogel with adipose stromal cells (ASCs),Citation136 which possess the potential for NP-like cell differentiation.Citation137,Citation138 The addition of HAMA increases the mechanical properties of photocrosslinked GelMA hydrogels, and the whole complex promotes the expression of articular cartilage ECM while avoiding the formation of osteophytes caused by direct injection of stem cells. The efficacy of the GelHA hydrogel and ASCs was evaluated in an IVDD rat model.Citation136 Kumar et al embedded human bone marrow-derived MSC (hMSC) in a novel three-dimensional photo-curable, biodegradable synthetic polymer hydrogel, in which polyhydroxyethyl MA-co-N-(3-aminopropyl)methacrylamide was grafted with polyamidoamine.Citation139 Their results showed that a special photocurable hydrogel enhanced the differentiation ability of hMSC toward the NP cell type. ()
Figure 8 Schematic showing the process of photo-curing of hMSC encapsulated within p(HEMA-co-APMA) g PAA hydrogels: (A) procedure of Three-dimensional hMSC encapsulation in polymer to produce hydrogel; (B) representative image of a 13.5% (w/v) photo-cured hydrogel with dimensions 1 cm Ø and 3 mm thick). Reprinted from Kumar D, Gerges I, Tamplenizza M, Lenardi C, Forsyth NR, Liu Y. Three-dimensional hypoxic culture of human mesenchymal stem cells encapsulated in a photocurable, biodegradable polymer hydrogel: a potential injectable cellular product for nucleus pulposus regeneration. Acta Biomater. 2014;10(8):3463–3474. Creative Commons.Citation139
Ultrasound-Responsive System
Ultrasound is considered a prospective external stimulus for delivery systems that exhibits effective energy focus, deep penetration, ease of handling, security, low cost, and portability of ultrasound instruments.Citation140,Citation141 Ultrasonication improves the delivery efficiency of bioactive substances and genes through thermal and non-thermal effects.Citation140,Citation142 Tissues with higher ultrasound absorption coefficients, such as bones, expand in temperature more rapidly than muscles with lower absorption coefficients.Citation143 Moreover, non-thermal effects include ultrasound pressure, shockwaves, acoustic streaming, liquid microjets, and ultrasound-induced oscillations or cavitation.Citation144–146
Previous studies have shown that ultrasound enhances the penetration of agents into living cells.Citation147 Based on this characteristic, microbubbles have been widely applied as cavitation nuclei in ultrasound-mediated delivery systems.Citation148,Citation149 Common microbubbles have a gas core and phospholipid, polymer, and protein shells.Citation150 Microbubbles commonly circulate with red blood cells and have a short circulation time in the bloodstream because of their size, which limits their transportation between blood vessels and target tissues. Recently, nanoscale bubbles, droplets, micelles, and nanoliposomes have been developed as novel nanomaterials in ultrasound-responsive delivery systems.Citation151–153
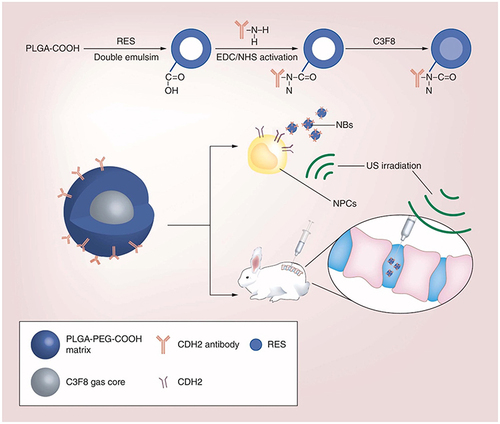
Guo et al constructed special resveratrol (RES) 3,5,4′-trihydroxystilbene-loaded anti-cadherin 2 (CDH2) antibody-decorated PLGA nanobubbles, which are effectively imploded by external ultrasound.Citation154 The released microjets led to the propulsion of the delivered drugs, which was applied in rat models. Relevant synthetic process is illustrated in . Additionally, Kobayashi et al demonstrated that low-intensity pulsed ultrasound (LIPUS) stimulation upregulated proteoglycan production in human NP cells, which showed potential in IVDD treatment.Citation155 Relevant studies have found that the mechanisms underlying the therapeutic effects of LIPUS include activation of the focal adhesion kinase (FAK)/phosphoinositide 3-kinase (PI3K)/AKT pathway and upregulation of aggrecan, collagen II, and SRY-box transcription factor 9 (SOX9) expression.Citation156 Furthermore, Horne et al and Chen et al found that LIPUS downregulated the expression of TNF-α gene in NP cells and upregulated the metabolic rate of AF cells.Citation157,Citation158
Figure 9 A schematic illustration for the experiment design and the fabrication process of RES-loaded, CDH2-decorated nanobubbles. Reprinted from Shen J, Zhuo N, Xu S et al. Resveratrol delivery by ultrasound-mediated nanobubbles targeting nucleus pulposus cells. Nanomedicine (Lond). 2018 Jun;13(12):1433–1446.Citation154 Copyright 2018 Future Medicine Ltd; permission conveyed through Copyright Clearance Center, Inc.
Magnetic-Responsive System
Magnetically responsive materials respond to changes in the magnetic fields by switching their properties. Owing to its changeable nature, magnetically responsive drug delivery can be achieved under the guidance of a magnetic field. Magnetic materials generate heat when exposed to alternating magnetic fields (AMFs), and magnetic NP cells generate heat through two methods: hysteresis loss (ferromagnetic particles) and the oscillation of their magnetic moment owing to Néel and Brownian relaxation (superparamagnetic particles).
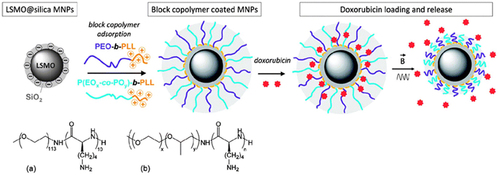
“Small” magnets have larger magnetic moments and are more sensitive to weak stimuli (static or alternating magnetic fields) than molecular magnets.Citation159 Composites have a variety of merging properties, including deformability, magnetically guided action, and magnetothermal effectsCitation159 (). Activation approaches for magnetically responsive polymer composites (MRPCs) involve the application of static magnetic fields or AMFs. The magnetothermal effect of the MRPCs can be used for controlled drug release. The underlying mechanism is attributed to the heat generated by the oscillating AMF, which causes structural changes in the nanocarrier structure, such as an increase in shell or double-layer pores,Citation160,Citation161 disintegration of the Fe3O4 core,Citation162 and deformation of the single-crystal nanoshell lattice.Citation163
Figure 10 Schemes depicting the different types of magnetic responsive materials obtained from the doping of various polymers with magnetic particles and illustration of their response when exposed to a static magnetic field (H dc) or to an alternating magnetic field (H ac). From left to right: composites made from elastomeric polymers can be deformed in homogeneous fields or gradients in a controlled fashion (A-C); MRPC particles made of polymers designed for biomedical applications can be used for magnetic guidance for drug delivery or separation purpose (D–F); MRPC from thermo-responsive polymers can be activated by magnetic induction using alternating fields (G and H). Reprinted from Thévenot J, Oliveira H, Sandre O, Lecommandoux S. Magnetic responsive polymer composite materials. Chem Soc Rev. 2013 Sep 7;42(17):7099–116.Citation159 Copyright 2013 Royal Society of Chemistry; permission conveyed through Copyright Clearance Center, Inc.
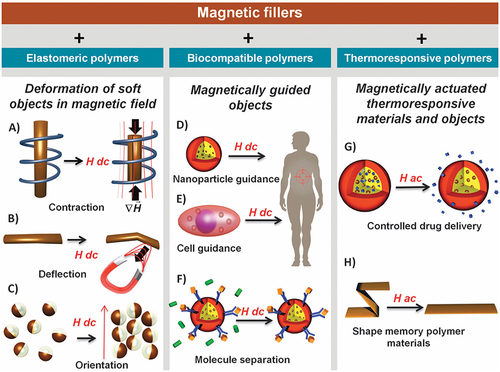
shows the release of the drug in relation to the contraction of the polymer brushes when the temperature exceeds the lower critical solution temperature. Moreover, Okada et al found that a pulsed electromagnetic field enhances the function of BMP-2 in IVD-cell matrix regeneration,Citation164 which explored the usage of the magnetic field. Although relevant studies have been limited to IVDD treatment, magnetically responsive drug delivery systems are a new research direction.
Figure 11 Preparation of magnetic responsive drug delivery systems (DDS) based on lanthanum strontium manganese oxide (LSMO) MNPs and polymer brush with a tunable LCST (top left). Chemical structures of the block copolymers used: (a) poly (ethylene glycol)-b-poly(lysine), and (b) poly (ethylene glycol-co-propylene glycol)-b-poly(lysine), with x = 6 and y = 29. Principle of drug loading and alternating magnetic field (AMF) triggered drug release (right). Reprinted from Louguet S, Rousseau B, Epherre R, et al. Thermoresponsive polymer brush-functionalized magnetic manganite nanoparticles for remotely triggered drug release. 10.1039/C2PY20089A. Polym Chem. 2012;3(6):1408–1417.Citation165 Copyright 2013 Royal Society of Chemistry; permission conveyed through Copyright Clearance Center, Inc.
Summary and Prospects
Compared to traditional systemic and local administration methods, newly developed stimuli-responsive delivery systems hold promise for treating a variety of diseases. These systems, such as hydrogels, scaffolds, nanoparticles, and microspheres, when combined with therapeutic molecules and specially modified, enable the precise release of therapeutic agents into degenerated intervertebral discs. This novel approach to stimuli-responsive delivery provides a more precise and sustained treatment for intervertebral disc degeneration (IVDD), aiming to reduce adverse effects. As research continues to advance and our understanding of biomaterials deepens, it is expected that the conception of stimuli-responsive will play an increasingly vital role in the future of IVDD therapy, ultimately leading to improved patient outcomes and quality of life.
However, emerging problems still need to be addressed. Low biocompatibility and high toxicity are the prime limitations of molecular delivery vectors. Thus, with their great biocompatibility and far lower toxicity, hydrogels are better applied as delivery systems than NPs and MSs. One novel approach to address the limitations of molecular delivery vectors is the integration of biomimicry principles. By mimicking the body’s natural mechanisms of healing and drug transport, we can design delivery systems that not only enhance biocompatibility but also reduce toxicity. For instance, the use of biologically derived materials, such as natural polymers and proteins, can create a more hospitable environment for the encapsulated bioactive agents, thereby preserving their therapeutic efficacy and reducing the risk of adverse reactions.
The diffusion ability of bioactive agents in a combined complex is another limiting factor for stimuli-responsive delivery systems. Current delivery systems usually use shell-core structures that feature special stimuli-responsive surface shells and curable core components. Following the reaction between the shell and stimulatory factors, the diffusive ability determines the therapeutic functions of the core bioactive agents. As the synthetic process may suppress the migration capability of the core component, it is vital to avoid additional restrictions on the main bioactive agents. More importantly, the intrinsic properties of core components should remain intact under all circumstances. Chemical synthesis can easily change the natural properties of the core components, which are crucial for their therapeutic ability. The synthesis process should be carefully optimized to ensure that the natural properties and therapeutic potential of the core components are not compromised. Employing gentle synthesis techniques and carefully selecting the appropriate materials can help maintain the integrity of the bioactive agents.
In conclusion, the future of stimuli-responsive drug delivery systems lies in the integration of biomimetic designs, smart materials, multifunctional capabilities, gentle synthesis techniques, and personalized medicine approaches. By pursuing these innovative strategies, we can overcome existing limitations and enter a new era of effective, safe, and patient-centered treatments for IVDD, ultimately improving patient outcomes and quality of life.
Abbreviations
IVD, intervertebral disc; IVDD, intervertebral disc degeneration; LBP, low back pain; NP, nucleus pulposus; AF, annulus fibrosus; CEP, cartilage endplates; ECM, extracellular matrix; BASP1, brain abundant membrane attached signal protein 1; NCDN, neurochondrin; NRP1, neuropilin 1; CD, cluster of differentiation; BEP, bony endplate; IL, interleukin; TNF, tumor necrosis factor; MMP, matrix metalloproteinase; ADAMTS, a disintegrin and metalloproteinase with thrombospondin motifs; TIMP, tissue inhibitors of metalloproteinase; MRI, magnetic resonance imaging; T1WI, T1-weighted imaging; T2WI, T2-weighted imaging; IFN-γ, interferon-γ; CCL20, C-C chemokine ligand 20; ROS, reactive oxygen species; H2O2, hydrogen peroxide; •OH, hydroxyl radicals; O2−•, superoxide anion radicals; H2, hydrogen gas; PLGA, poly(lactic-co-glycolic acid); EGDM, ethylene glycol dimethacrylate; PBT, polybutylene terephthalate; MR, mineralocorticoid receptor; PPS, poly(propylene sulfide); PEG, poly(ethylene glycol); IGK, Isoginkgetin; HA, hyaluronidase; miRNA, micro-ribonucleic acid; RNA, ribonucleic acid; PGPC, PEG-GPLGVRG-poly{N′-[N-(2-aminoethyl)-2-aminoehtyl]aspartamide}-cholesteryl; MSCs, mesenchymal stem cells; NPPCs, NP progenitor cells; H2S, Hydrogen sulfide; Col-JK1, collagen-JK1 hydrogel; NF, nuclear factor; ASIC-3, acid-sensing ion channel-3; MOF, metal–organic framework; PCA, Protocatechuic acid; HPDA, hollow polydopamine; AB, ammonia borane; GMA, glycidyl methacrylate; CMC, carboxy-methyl chitosan; MAPK, mitogen-activated protein kinase; ERK, extracellular signal-regulated kinase; pNIPAM, poly(N-isopropylacrylamide); TR-HG, temperature-sensitive hydrogel; IPN, interpenetrating polymer network; BDDE, 1.4-butanediol diglycidyl ether; MTF1, metal regulatory transcription factor 1; MCBCs, mixed cationic block copolymers; MA, methacrylate; Gel, gelatin; ASCs, adipose stromal cells; hMSC, human bone marrow-derived MSC; RES, resveratrol; CDH2, 3,5,4′-trihydroxystilbene-loaded anti-cadherin 2; FAK, focal adhesion kinase; LIPUS, low-intensity pulsed ultrasound; PI3K, phosphoinositide 3-kinase; SOX9, SRY-box transcription factor 9; AMFs, alternating magnetic fields; MRPCs, magnetically responsive polymer composites.
Author Contributions
All authors have contributed significantly to the work presented, spanning from its conception and study design to involvement in drafting, revising, and critically reviewing the article. All authors gave final approval of the version to be published, and have agreed on the journal to which the article has been submitted. All authors agree to take responsibility and be accountable for the contents of the article.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by the National Key R&D Program of China (2021YFA1102600), the National Natural Science Foundation of China (82372407,82002315), the Basic Research Support Program of Huazhong University of Science and Technology (2024BRB021), and Wuhan Knowledge Innovation Project (2023020201020228).
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–747. doi:10.1016/s0140-6736(16)30970-9
- Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP. Low back pain. Lancet. 2021;398(10294):78–92. doi:10.1016/s0140-6736(21)00733-9
- Vergroesen PP, Kingma I, Emanuel KS, et al. Mechanics and biology in intervertebral disc degeneration: a vicious circle. Osteoarthritis Cartilage. 2015;23(7):1057–1070. doi:10.1016/j.joca.2015.03.028
- van Uden S, Silva-Correia J, Oliveira JM, Reis RL. Current strategies for treatment of intervertebral disc degeneration: substitution and regeneration possibilities. Biomater Res. 2017;21:22. doi:10.1186/s40824-017-0106-6
- Global, regional. and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi:10.1016/s0140-6736(18)32279-7
- Mohd Isa IL, Teoh SL, Mohd Nor NH, Mokhtar SA. Discogenic low back pain: anatomy, pathophysiology and treatments of intervertebral disc degeneration. Int J Mol Sci. 2022;24(1):208. doi:10.3390/ijms24010208
- Risbud MV, Shapiro IM. Role of cytokines in intervertebral disc degeneration: pain and disc content. Nat Rev Rheumatol. 2014;10(1):44–56. doi:10.1038/nrrheum.2013.160
- Kos N, Gradisnik L, Velnar T. A brief review of the degenerative intervertebral disc disease. Med Arch. 2019;73(6):421–424. doi:10.5455/medarh.2019.73.421-424
- Zhao CQ, Wang LM, Jiang LS, Dai LY. The cell biology of intervertebral disc aging and degeneration. Ageing Res Rev. 2007;6(3):247–261. doi:10.1016/j.arr.2007.08.001
- Smith LJ, Nerurkar NL, Choi KS, Harfe BD, Elliott DM. Degeneration and regeneration of the intervertebral disc: lessons from development. Dis Model Mech. 2011;4(1):31–41. doi:10.1242/dmm.006403
- Xin J, Wang Y, Zheng Z, Wang S, Na S, Zhang S. Treatment of Intervertebral Disc Degeneration. Orthop Surg. 2022;14(7):1271–1280.
- Wu PH, Kim HS, Jang IT. Intervertebral disc diseases PART 2: a review of the current diagnostic and treatment strategies for intervertebral disc disease. Int J Mol Sci. 2020;21(6):1.
- Kamali A, Ziadlou R, Lang G, et al. Small molecule-based treatment approaches for intervertebral disc degeneration: current options and future directions. Theranostics. 2021;11(1):27–47. doi:10.7150/thno.48987
- Esquijarosa Hechavarria M, Richard SA. Edifying the focal factors influencing mesenchymal stem cells by the microenvironment of intervertebral disc degeneration in low back pain. Pain Res Manag. 2022;2022:6235400. doi:10.1155/2022/6235400
- Aunoble S, Donkersloot P, Le Huec JC. Dislocations with intervertebral disc prosthesis: two case reports. Eur Spine J. 2004;13(5):464–467. doi:10.1007/s00586-004-0687-3
- van Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: a report of 27 patients with the SB Charité disc. J Spinal Disord Tech. 2003;16(4):369–383. doi:10.1097/00024720-200308000-00009
- Shim CS, Lee S, Maeng DH, Lee SH. Vertical split fracture of the vertebral body following total disc replacement using ProDisc: report of two cases. J Spinal Disord Tech. 2005;18(5):465–469. doi:10.1097/01.bsd.0000159035.35365.df
- Huang Y, Feng G. Editorial: biomaterial advances in intervertebral disc degeneration. Front Bioeng Biotechnol. 2023;11:1153019. doi:10.3389/fbioe.2023.1153019
- Liu Z, Bian Y, Wu G, Fu C. Application of stem cells combined with biomaterial in the treatment of intervertebral disc degeneration. Front Bioeng Biotechnol. 2022;10:1077028. doi:10.3389/fbioe.2022.1077028
- Ligorio C, Hoyland JA, Saiani A. Self-assembling peptide hydrogels as functional tools to tackle intervertebral disc degeneration. Gels. 2022;8(4):211. doi:10.3390/gels8040211
- Mohd Isa IL, Mokhtar SA, Abbah SA, Fauzi MB, Devitt A, Pandit A. Intervertebral disc degeneration: biomaterials and tissue engineering strategies toward precision medicine. Adv Healthc Mater. 2022;11(13):e2102530. doi:10.1002/adhm.202102530
- Le Moal B, Lepeltier É, Rouleau D, et al. Lipid nanocapsules for intracellular delivery of microRNA: a first step towards intervertebral disc degeneration therapy. Int J Pharm. 2022;624:121941. doi:10.1016/j.ijpharm.2022.121941
- Shapiro IM, Risbud MV. Introduction to the Structure, Function, and Comparative Anatomy of the Vertebrae and the Intervertebral Disc. In: Shapiro IM, Risbud MV, editors. The Intervertebral Disc: Molecular and Structural Studies of the Disc in Health and Disease. Springer Vienna; 2014:3–15.
- Newell N, Little JP, Christou A, Adams MA, Adam CJ, Masouros SD. Biomechanics of the human intervertebral disc: a review of testing techniques and results. J Mech Behav Biomed Mater. 2017;69:420–434. doi:10.1016/j.jmbbm.2017.01.037
- Humzah MD, Soames RW. 1 Human intervertebral disc: structure and function. Anat Rec. 1988;220(4):337–356. doi:10.1002/ar.1092200402
- Kessel L. Backache. Ian McNab. 230 × 150 mm. Pp. 235 + xii. Illustrated. 1977. Baltimore: Williams & Wilkins. $17.00. Br J Surg. 2005;65(1):67. doi:10.1002/bjs.1800650126
- D’Antoni AV. Clinically Oriented Anatomy, 7th Edition, by Keith L. Moore, Arthur F. Dalley II, and Anne M. R. Agur, Baltimore, MD: Lippincott Williams & Wilkins, 2014, 1134 pages, Paperback, ISBN 978-1-4511-1945-9. Price: $92.99. Clin Anat. 2014;27(2):274. doi:10.1002/ca.22316
- Stein D, Assaf Y, Dar G, et al. 3D virtual reconstruction and quantitative assessment of the human intervertebral disc’s annulus fibrosus: a DTI tractography study. Sci Rep. 2021;11(1):6815. doi:10.1038/s41598-021-86334-8
- Molladavoodi S, McMorran J, Gregory D. Mechanobiology of annulus fibrosus and nucleus pulposus cells in intervertebral discs. Cell Tissue Res. 2020;379(3):429–444. doi:10.1007/s00441-019-03136-1
- Maroudas A, Stockwell RA, Nachemson A, Urban J. Factors involved in the nutrition of the human lumbar intervertebral disc: cellularity and diffusion of glucose in vitro. J Anat. 1975;120:1.
- Souter WA, Taylor TK. Sulphated acid mucopolysaccharide metabolism in the rabbit intervertebral disc. J Bone Joint Surg Br. 1970;52(2):371–384. doi:10.1302/0301-620X.52B2.371
- Torre OM, Mroz V, Bartelstein MK, Huang AH, Iatridis JC. Annulus fibrosus cell phenotypes in homeostasis and injury: implications for regenerative strategies. Ann N Y Acad Sci. 2019;1442(1):61–78. doi:10.1111/nyas.13964
- van den Akker GG, Surtel DA, Cremers A, et al. Novel immortal cell lines support cellular heterogeneity in the human annulus fibrosus. PLoS One. 2016;11(1):e0144497. doi:10.1371/journal.pone.0144497
- Lavignolle B. The Intervertebral Disc. In: Vital JM, Cawley DT, editors. Spinal Anatomy: Modern Concepts. Springer International Publishing; 2020:207–216.
- Lv F, Leung VY, Huang S, Huang Y, Sun Y, Cheung KM. In search of nucleus pulposus-specific molecular markers. Rheumatology. 2014;53(4):600–610. doi:10.1093/rheumatology/ket303
- Maarof M, Sulaiman S, Saim A, Idrus R. Cultivation of intervertebral disc cells in medium fortified with growth factors improved in vitro chondrogenesis. Biomed Res. 2011;22:435–441.
- Morris H, Gonçalves CF, Dudek M, Hoyland J, Meng Q-J. Tissue physiology revolving around the clock: circadian rhythms as exemplified by the intervertebral disc. Ann Rheumatic Dis. 2021;80(7):828–839. doi:10.1136/annrheumdis-2020-219515
- Chen J, Yan W, Setton LA. Molecular phenotypes of notochordal cells purified from immature nucleus pulposus. Eur Spine J. 2006;15(3):303–311. doi:10.1007/s00586-006-0088-x
- Guilak F, Ting-Beall HP, Baer AE, Trickey WR, Erickson GR, Setton LA. Viscoelastic properties of intervertebral disc cells. Identification of two biomechanically distinct cell populations. Spine (Phila Pa 1976). 1999;24(23):2475–2483. doi:10.1097/00007632-199912010-00009
- Hunter CJ, Matyas JR, Duncan NA. Cytomorphology of notochordal and chondrocytic cells from the nucleus pulposus: a species comparison. J Anat. 2004;205(5):357–362. doi:10.1111/j.0021-8782.2004.00352.x
- Taylor JR, Twomey LT. The Development of the Human Intervertebral Disc. Biology Intervertebral Disc. 2019;2019:1.
- Tang X, Jing L, Chen J. Changes in the molecular phenotype of nucleus pulposus cells with intervertebral disc aging. PLoS One. 2012;7(12):e52020. doi:10.1371/journal.pone.0052020
- Agrawal A, Guttapalli A, Narayan S, Albert TJ, Shapiro IM, Risbud MV. Normoxic stabilization of HIF-1alpha drives glycolytic metabolism and regulates aggrecan gene expression in nucleus pulposus cells of the rat intervertebral disk. Am J Physiol Cell Physiol. 2007;293(2):C621–31. doi:10.1152/ajpcell.00538.2006
- Moon SM, Yoder JH, Wright AC, Smith LJ, Vresilovic EJ, Elliott DM. Evaluation of intervertebral disc cartilaginous endplate structure using magnetic resonance imaging. Eur Spine J. 2013;22(8):1820–1828. doi:10.1007/s00586-013-2798-1
- Moore RJ. The vertebral endplate: disc degeneration, disc regeneration. Eur Spine J. 2006;15(3):333–337. doi:10.1007/s00586-006-0170-4
- Inoue H. Three-dimensional architecture of lumbar intervertebral discs. Spine. 1981;6(2):139–146. doi:10.1097/00007632-198103000-00006
- Standring S. Gray’s anatomy: the anatomical basis of clinical practice; 2015.
- Crock HV, Goldwasser M, Yoshizawa H. Vascular anatomy related to the intervertebral disc. The Biology of the Intervertebral Disc. 2019;2019:1.
- Shirazi-Adl A, Taheri M, Urban JP. Analysis of cell viability in intervertebral disc: effect of endplate permeability on cell population. J Biomech. 2010;43(7):1330–1336. doi:10.1016/j.jbiomech.2010.01.023
- Groh AMR, Fournier DE, Battié MC, Séguin CA. Innervation of the human intervertebral disc: a scoping review. Pain Med. 2021;22(6):1281–1304. doi:10.1093/pm/pnab070
- Roberts S, Eisenstein SM, Menage J, Evans EH, Ashton IK. Mechanoreceptors in intervertebral discs. Morphology, distribution, and neuropeptides. Spine (Phila Pa 1976). 1995;20(24):2645–2651. doi:10.1097/00007632-199512150-00005
- Chu G, Shi C, Wang H, Zhang W, Yang H, Li B. Strategies for annulus fibrosus regeneration: from biological therapies to tissue engineering. Front Bioeng Biotechnol. 2018;6:90. doi:10.3389/fbioe.2018.00090
- Hayes AJ, Benjamin M, Ralphs JR. Extracellular matrix in development of the intervertebral disc. Matrix Biol. 2001;20(2):107–121. doi:10.1016/s0945-053x(01)00125-1
- Rutges JP, Nikkels PG, Oner FC, et al. The presence of extracellular matrix degrading metalloproteinases during fetal development of the intervertebral disc. Eur Spine J. 2010;19(8):1340–1346. doi:10.1007/s00586-010-1378-x
- Chuah YJ, Peck Y, Lau JE, Hee HT, Wang DA. Hydrogel based cartilaginous tissue regeneration: recent insights and technologies. Biomater Sci. 2017;5(4):613–631. doi:10.1039/c6bm00863a
- Yu Q, Han F, Yuan Z, et al. Fucoidan-loaded nanofibrous scaffolds promote annulus fibrosus repair by ameliorating the inflammatory and oxidative microenvironments in degenerative intervertebral discs. Acta Biomater. 2022;148:73–89. doi:10.1016/j.actbio.2022.05.054
- Miyamoto H, Doita M, Nishida K, Yamamoto T, Sumi M, Kurosaka M. Effects of cyclic mechanical stress on the production of inflammatory agents by nucleus pulposus and anulus fibrosus derived cells in vitro. Spine (Phila Pa 1976). 2006;31(1):4–9. doi:10.1097/01.brs.0000192682.87267.2a
- Pratsinis H, Papadopoulou A, Neidlinger-Wilke C, Brayda-Bruno M, Wilke HJ, Kletsas D. Cyclic tensile stress of human annulus fibrosus cells induces MAPK activation: involvement in proinflammatory gene expression. Osteoarthritis Cartilage. 2016;24(4):679–687. doi:10.1016/j.joca.2015.11.022
- Roughley PJ, Melching LI, Heathfield TF, Pearce RH, Mort JS. The structure and degradation of aggrecan in human intervertebral disc. Eur Spine J. 2006;15:S326–32. doi:10.1007/s00586-006-0127-7
- Brinckmann P, Grootenboer H. Change of disc height, radial disc bulge, and intradiscal pressure from discectomy. An in vitro investigation on human lumbar discs. Spine (Phila Pa 1976). 1991;16(6):641–646. doi:10.1097/00007632-199106000-00008
- Vergroesen PP, van der Veen AJ, van Royen BJ, Kingma I, Smit TH. Intradiscal pressure depends on recent loading and correlates with disc height and compressive stiffness. Eur Spine J. 2014;23(11):2359–2368. doi:10.1007/s00586-014-3450-4
- Singh K, Phillips FM. The biomechanics and biology of the spinal degenerative cascade. Sem Spine Surg. 2005;17(3):128–136. doi:10.1053/j.semss.2005.06.001
- Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976). 2002;27(23):2631–2644. doi:10.1097/00007632-200212010-00002
- Antoniou J, Goudsouzian NM, Heathfield TF, et al. The human lumbar endplate. Evidence of changes in biosynthesis and denaturation of the extracellular matrix with growth, maturation, aging, and degeneration. Spine (Phila Pa 1976). 1996;21(10):1153–1161. doi:10.1097/00007632-199605150-00006
- Urban JP, Roberts S, Ralphs JR. The nucleus of the intervertebral disc from development to degeneration. Am Zool. 2000;2000:1.
- Sakai D, Nakamura Y, Nakai T, et al. Exhaustion of nucleus pulposus progenitor cells with ageing and degeneration of the intervertebral disc. Nat Commun. 2012;3:1264. doi:10.1038/ncomms2226
- Quero L, Klawitter M, Schmaus A, et al. Hyaluronic acid fragments enhance the inflammatory and catabolic response in human intervertebral disc cells through modulation of toll-like receptor 2 signalling pathways. Arthritis Res Ther. 2013;15(4):R94. doi:10.1186/ar4274
- Richardson SM, Doyle P, Minogue BM, Gnanalingham K, Hoyland JA. Increased expression of matrix metalloproteinase-10, nerve growth factor and substance P in the painful degenerate intervertebral disc. Arthritis Res Ther. 2009;11(4):R126. doi:10.1186/ar2793
- Purmessur D, Walter BA, Roughley PJ, Laudier DM, Hecht AC, Iatridis J. A role for TNFα in intervertebral disc degeneration: a non-recoverable catabolic shift. Biochem Biophys Res Commun. 2013;433(1):151–156. doi:10.1016/j.bbrc.2013.02.034
- Vo NV, Hartman RA, Yurube T, Jacobs LJ, Sowa GA, Kang JD. Expression and regulation of metalloproteinases and their inhibitors in intervertebral disc aging and degeneration. Spine J. 2013;13(3):331–341. doi:10.1016/j.spinee.2012.02.027
- Hadjipavlou AG, Tzermiadianos MN, Bogduk N, Zindrick MR. The pathophysiology of disc degeneration: a critical review. J Bone Joint Surg Br. 2008;90(10):1261–1270. doi:10.1302/0301-620x.90b10.20910
- Wang J, Markova D, Anderson DG, Zheng Z, Shapiro IM, Risbud MV. TNF-α and IL-1β promote a disintegrin-like and metalloprotease with thrombospondin type I motif-5-mediated aggrecan degradation through syndecan-4 in intervertebral disc. J Biol Chem. 2011;286(46):39738–39749. doi:10.1074/jbc.M111.264549
- Moore RJ. The vertebral end-plate: what do we know? Eur Spine J Apr. 2000;9(2):92–96. doi:10.1007/s005860050217
- Che-Nordin N, Deng M, Griffith JF, et al. Prevalent osteoporotic vertebral fractures more likely involve the upper endplate than the lower endplate and even more so in males. Ann Transl Med. 2018;6(22):442. doi:10.21037/atm.2018.10.61
- Adams MA, Dolan P. Intervertebral disc degeneration: evidence for two distinct phenotypes. J Anat. 2012;221(6):497–506. doi:10.1111/j.1469-7580.2012.01551.x
- Kuisma M, Karppinen J, Niinimäki J, et al. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine (Phila Pa 1976). 2007;32(10):1116–1122. doi:10.1097/01.brs.0000261561.12944.ff
- Rahme R, Moussa R. The modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. AJNR Am J Neuroradiol. 2008;29(5):838–842. doi:10.3174/ajnr.A0925
- Costăchescu B, Niculescu AG, Teleanu RI, et al. Recent advances in managing spinal intervertebral discs degeneration. Int J Mol Sci. 2022;23(12):6460. doi:10.3390/ijms23126460
- Khalil M, Ray A, Dittel BN. Characterization of the cell surface phenotype and regulatory activity of B-Cell IgD Low (BD(L)) Regulatory B Cells. Methods Mol Biol. 2021;2270:217–231. doi:10.1007/978-1-0716-1237-8_12
- Hiyama A, Suyama K, Sakai D, Tanaka M, Watanabe M. Correlational analysis of chemokine and inflammatory cytokine expression in the intervertebral disc and blood in patients with lumbar disc disease. J Orthop Res. 2022;40(5):1213–1222. doi:10.1002/jor.25136
- Feng C, Yang M, Lan M, et al. ROS: crucial intermediators in the pathogenesis of intervertebral disc degeneration. Oxid Med Cell Longev. 2017;2017:5601593. doi:10.1155/2017/5601593
- Suzuki S, Fujita N, Hosogane N, et al. Excessive reactive oxygen species are therapeutic targets for intervertebral disc degeneration. Arthritis Res Ther. 2015;17:316. doi:10.1186/s13075-015-0834-8
- Wang Y, Cheng H, Wang T, Zhang K, Zhang Y, Kang X. Oxidative stress in intervertebral disc degeneration: molecular mechanisms, pathogenesis and treatment. Cell Prolif. 2023;56:e13448. doi:10.1111/cpr.13448
- Zhang T, Wang Y, Li R, et al. ROS-responsive magnesium-containing microspheres for antioxidative treatment of intervertebral disc degeneration. Acta Biomater. 2023;158:475–492. doi:10.1016/j.actbio.2023.01.020
- Zheng Q, Shen H, Tong Z, et al. A thermosensitive, reactive oxygen species-responsive, MR409-encapsulated hydrogel ameliorates disc degeneration in rats by inhibiting the secretory autophagy pathway. Theranostics. 2021;11(1):147–163. doi:10.7150/thno.47723
- Zhang X, Cui T, He J, et al. Beneficial effects of growth hormone-releasing hormone agonists on rat INS-1 cells and on streptozotocin-induced NOD/SCID mice. Proc Natl Acad Sci U S A. 2015;112(44):13651–13656. doi:10.1073/pnas.1518540112
- Bagno LL, Kanashiro-Takeuchi RM, Suncion VY, et al. Growth hormone-releasing hormone agonists reduce myocardial infarct scar in swine with subacute ischemic cardiomyopathy. J Am Heart Assoc. 2015;4(4). doi:10.1161/JAHA.114.001464
- Czikora I, Sridhar S, Gorshkov B, et al. Protective effect of growth hormone-releasing hormone agonist in bacterial toxin-induced pulmonary barrier dysfunction. Front Physiol. 2014;5:259. doi:10.3389/fphys.2014.00259
- Yu H, Teng Y, Ge J, et al. Isoginkgetin-loaded reactive oxygen species scavenging nanoparticles ameliorate intervertebral disc degeneration via enhancing autophagy in nucleus pulposus cells. J Nanobiotechnology. 2023;21(1):99. doi:10.1186/s12951-023-01856-9
- Bai J, Zhang Y, Fan Q, et al. Reactive oxygen species-scavenging scaffold with rapamycin for treatment of intervertebral disk degeneration. Adv Healthc Mater. 2020;9(3):e1901186. doi:10.1002/adhm.201901186
- Zhang GZ, Deng YJ, Xie QQ, et al. Sirtuins and intervertebral disc degeneration: roles in inflammation, oxidative stress, and mitochondrial function. Clin Chim Acta. 2020;508:33–42. doi:10.1016/j.cca.2020.04.016
- Zhang C, Gullbrand SE, Schaer TP, et al. Inflammatory cytokine and catabolic enzyme expression in a goat model of intervertebral disc degeneration. J Orthop Res. 2020;38(11):2521–2531. doi:10.1002/jor.24639
- Peng Y, Qing X, Shu H, et al. Proper animal experimental designs for preclinical research of biomaterials for intervertebral disc regeneration. Biomater Transl. 2021;2(2):91–142. doi:10.12336/biomatertransl.2021.02.003
- Maurer B, Stanczyk J, Jüngel A, et al. MicroRNA-29, a key regulator of collagen expression in systemic sclerosis. Arthritis Rheum. 2010;62(6):1733–1743. doi:10.1002/art.27443
- Qin W, Chung AC, Huang XR, et al. TGF-β/Smad3 signaling promotes renal fibrosis by inhibiting miR-29. J Am Soc Nephrol. 2011;22(8):1462–1474. doi:10.1681/asn.2010121308
- Wang B, Komers R, Carew R, et al. Suppression of microRNA-29 expression by TGF-β1 promotes collagen expression and renal fibrosis. J Am Soc Nephrol. 2012;23(2):252–265. doi:10.1681/asn.2011010055
- He Y, Huang C, Lin X, Li J. MicroRNA-29 family, a crucial therapeutic target for fibrosis diseases. Biochimie. 2013;95(7):1355–1359. doi:10.1016/j.biochi.2013.03.010
- Ramdas V, McBride M, Denby L, Baker AH. Canonical transforming growth factor-β signaling regulates disintegrin metalloprotease expression in experimental renal fibrosis via miR-29. Am J Pathol. 2013;183(6):1885–1896. doi:10.1016/j.ajpath.2013.08.027
- Feng G, Zha Z, Huang Y, et al. Sustained and bioresponsive two-stage delivery of therapeutic miRNA via polyplex micelle-loaded injectable hydrogels for inhibition of intervertebral disc fibrosis. Adv Healthc Mater. 2018;7(21):e1800623. doi:10.1002/adhm.201800623
- Bhujel B, Shin HE, Choi DJ, Han I. Mesenchymal stem cell-derived exosomes and intervertebral disc regeneration: review. Int J Mol Sci. 2022;23(13):7306. doi:10.3390/ijms23137306
- Sakai D, Andersson GB. Stem cell therapy for intervertebral disc regeneration: obstacles and solutions. Nat Rev Rheumatol. 2015;11(4):243–256. doi:10.1038/nrrheum.2015.13
- Xia KS, Li DD, Wang CG, et al. An esterase-responsive ibuprofen nano-micelle pre-modified embryo derived nucleus pulposus progenitor cells promote the regeneration of intervertebral disc degeneration. Bioact Mater. 2023;21:69–85. doi:10.1016/j.bioactmat.2022.07.024
- Szabó C. Hydrogen sulphide and its therapeutic potential. Nat Rev Drug Discov. 2007;6(11):917–935. doi:10.1038/nrd2425
- Wu J, Li Y, He C, et al. Novel H(2)S releasing nanofibrous coating for in vivo dermal wound regeneration. ACS Appl Mater Interfaces. 2016;8(41):27474–27481. doi:10.1021/acsami.6b06466
- Wallace JL, Wang R. Hydrogen sulfide-based therapeutics: exploiting a unique but ubiquitous gasotransmitter. Nat Rev Drug Discov. 2015;14(5):329–345. doi:10.1038/nrd4433
- Zheng Z, Chen A, He H, et al. pH and enzyme dual-responsive release of hydrogen sulfide for disc degeneration therapy. J Mater Chem B. 2019;7(4):611–618. doi:10.1039/c8tb02566e
- Razaq S, Wilkins RJ, Urban JP. The effect of extracellular pH on matrix turnover by cells of the bovine nucleus pulposus. Eur Spine J. 2003;12(4):341–349. doi:10.1007/s00586-003-0582-3
- Kitano T, Zerwekh JE, Usui Y, Edwards ML, Flicker PL, Mooney V. Biochemical changes associated with the symptomatic human intervertebral disk. Clin Orthop Relat Res. 1993;293:372–377. doi:10.1097/00003086-199308000-00050
- Gilbert HTJ, Hodson N, Baird P, Richardson SM, Hoyland JA. Acidic pH promotes intervertebral disc degeneration: acid-sensing ion channel −3 as a potential therapeutic target. Sci Rep. 2016;6:37360. doi:10.1038/srep37360
- Hodson NW, Patel S, Richardson SM, Hoyland JA, Gilbert HTJ. Degenerate intervertebral disc-like pH induces a catabolic mechanoresponse in human nucleus pulposus cells. JOR Spine. 2018;1(1):e1004. doi:10.1002/jsp2.1004
- Ding H, Zhang X, Liu Z, et al. Construction of MOFs nanoplatform with pH-triggered release of protocatechuic acid for intervertebral disc degeneration therapy. Mater Des. 2023;225:111493. doi:10.1016/j.matdes.2022.111493
- Wang W, Xiao B, Qiu Y, et al. pH-Responsive Delivery of H2 through ammonia borane-loaded hollow polydopamine for intervertebral disc degeneration therapy. Oxid Med Cell Longev. 2023;2023:7773609. doi:10.1155/2023/7773609
- Wang Y, Wu Y, Zhang B, et al. Repair of degenerative nucleus pulposus by polyphenol nanosphere-encapsulated hydrogel gene delivery system. Biomaterials. 2023;298:122132. doi:10.1016/j.biomaterials.2023.122132
- Mortisen D, Peroglio M, Alini M, Eglin D. Tailoring thermoreversible hyaluronan hydrogels by ”click” chemistry and RAFT polymerization for cell and drug therapy. Biomacromolecules. 2010;11(5):1261–1272. doi:10.1021/bm100046n
- Barhoumi A, Wang W, Zurakowski D, Langer RS, Kohane DS. Photothermally targeted thermosensitive polymer-masked nanoparticles. Nano Lett. 2014;14(7):3697–3701. doi:10.1021/nl403733z
- Kono K, Murakami E, Hiranaka Y, et al. Thermosensitive molecular assemblies from poly(amidoamine) dendron-based lipids. Angew Chem Int Ed Engl. 2011;50(28):6332–6336. doi:10.1002/anie.201101007
- Osawa S, Ishii T, Takemoto H, Osada K, Kataoka K. A facile amino-functionalization of poly(2-oxazoline)s’ distal end through sequential azido end-capping and Staudinger reactions. Eur Polym J. 2017;88:553–561. doi:10.1016/j.eurpolymj.2016.11.029
- Yang J, Zhang P, Tang L, et al. Temperature-tuned DNA condensation and gene transfection by PEI-g-(PMEO(2)MA-b-PHEMA) copolymer-based nonviral vectors. Biomaterials. 2010;31(1):144–155. doi:10.1016/j.biomaterials.2009.09.027
- Malonzo C, Chan SC, Kabiri A, et al. A papain-induced disc degeneration model for the assessment of thermo-reversible hydrogel-cells therapeutic approach. J Tissue Eng Regen Med. 2015;9(12):E167–76. doi:10.1002/term.1667
- Sahoo S, Chung C, Khetan S, Burdick JA. Hydrolytically degradable hyaluronic acid hydrogels with controlled temporal structures. Biomacromolecules. 2008;9(4):1088–1092. doi:10.1021/bm800051m
- Guo W, Douma L, Hu MH, et al. Hyaluronic acid-based interpenetrating network hydrogel as a cell carrier for nucleus pulposus repair. Carbohydr Polym. 2022;277:118828. doi:10.1016/j.carbpol.2021.118828
- Amin NP, Mohindra P, Jabbour SK. Serum microRNA guiding personalized radiation therapy in non-small cell lung cancer. J Thorac Dis. 2018;10(Suppl 33):S4108–s4112. doi:10.21037/jtd.2018.09.143
- Wang C, Wang WJ, Yan YG, et al. MicroRNAs: new players in intervertebral disc degeneration. Clin Chim Acta. 2015;450:333–341. doi:10.1016/j.cca.2015.09.011
- Lin X, Lin Q. MiRNA-495-3p Attenuates TNF-α Induced Apoptosis and Inflammation in Human Nucleus Pulposus Cells by Targeting IL5RA. Inflammation. 2020;43(5):1797–1805. doi:10.1007/s10753-020-01254-5
- Huang Y, Huang L, Li L, et al. MicroRNA-25-3p therapy for intervertebral disc degeneration by targeting the IL-1β/ZIP8/MTF1 signaling pathway with a novel thermo-responsive vector. Ann Transl Med. 2020;8(22):1500. doi:10.21037/atm-20-6595
- Yin H, Kanasty RL, Eltoukhy AA, Vegas AJ, Dorkin JR, Anderson DG. Non-viral vectors for gene-based therapy. Nat Rev Genet. 2014;15(8):541–555. doi:10.1038/nrg3763
- Calejo MT, Cardoso AM, Kjøniksen AL, et al. Temperature-responsive cationic block copolymers as nanocarriers for gene delivery. Int J Pharm. 2013;448(1):105–114. doi:10.1016/j.ijpharm.2013.03.028
- Wong SY, Han L, Timachova K, et al. Drastically lowered protein adsorption on microbicidal hydrophobic/hydrophilic polyelectrolyte multilayers. Biomacromolecules. 2012;13(3):719–726. doi:10.1021/bm201637e
- Zhang H, Lin CY. Simvastatin stimulates chondrogenic phenotype of intervertebral disc cells partially through BMP-2 pathway. Spine (Phila Pa 1976). 2008;33(16):E525–31. doi:10.1097/BRS.0b013e31817c561b
- Zhang H, Wang L, Park JB, et al. Intradiscal injection of simvastatin retards progression of intervertebral disc degeneration induced by stab injury. Arthritis Res Ther. 2009;11(6):R172. doi:10.1186/ar2861
- Tyagi P, Li Z, Chancellor M, De Groat WC, Yoshimura N, Huang L. Sustained intravesical drug delivery using thermosensitive hydrogel. Pharm Res. 2004;21(5):832–837. doi:10.1023/b:pham.0000026436.62869.9c
- Jeong B, Bae YH, Kim SW. Drug release from biodegradable injectable thermosensitive hydrogel of PEG-PLGA-PEG triblock copolymers. J Control Release. 2000;63(1–2):155–163. doi:10.1016/s0168-3659(99)00194-7
- Li Z, Ning W, Wang J, et al. Controlled gene delivery system based on thermosensitive biodegradable hydrogel. Pharm Res. 2003;20(6):884–888. doi:10.1023/a:1023887203111
- Lee HP, Gaharwar AK. Light-responsive inorganic biomaterials for biomedical applications. Adv Sci (Weinh). 2020;7(17):2000863. doi:10.1002/advs.202000863
- Karimi M, Sahandi Zangabad P, Baghaee-Ravari S, Ghazadeh M, Mirshekari H, Hamblin MR. Smart nanostructures for cargo delivery: uncaging and activating by light. J Am Chem Soc. 2017;139(13):4584–4610. doi:10.1021/jacs.6b08313
- Chen P, Ning L, Qiu P, et al. Photo-crosslinked gelatin-hyaluronic acid methacrylate hydrogel-committed nucleus pulposus-like differentiation of adipose stromal cells for intervertebral disc repair. J Tissue Eng Regen Med. 2019;13(4):682–693. doi:10.1002/term.2841
- Clarke LE, McConnell JC, Sherratt MJ, Derby B, Richardson SM, Hoyland JA. Growth differentiation factor 6 and transforming growth factor-beta differentially mediate mesenchymal stem cell differentiation, composition, and micromechanical properties of nucleus pulposus constructs. Arthritis Res Ther. 2014;16(2):R67. doi:10.1186/ar4505
- Minogue BM, Richardson SM, Zeef LA, Freemont AJ, Hoyland JA. Characterization of the human nucleus pulposus cell phenotype and evaluation of novel marker gene expression to define adult stem cell differentiation. Arthritis Rheum. 2010;62(12):3695–3705. doi:10.1002/art.27710
- Kumar D, Gerges I, Tamplenizza M, Lenardi C, Forsyth NR, Liu Y. Three-dimensional hypoxic culture of human mesenchymal stem cells encapsulated in a photocurable, biodegradable polymer hydrogel: a potential injectable cellular product for nucleus pulposus regeneration. Acta Biomater. 2014;10(8):3463–3474. doi:10.1016/j.actbio.2014.04.027
- Endo-Takahashi Y, Negishi Y, Suzuki R, Maruyama K, Aramaki Y. MicroRNA imaging in combination with diagnostic ultrasound and bubble liposomes for MicroRNA delivery. Methods Mol Biol. 2016;1372:209–213. doi:10.1007/978-1-4939-3148-4_16
- Sirsi SR, Borden MA. State-of-The-art materials for ultrasound-triggered drug delivery. Adv Drug Deliv Rev. 2014;72:3–14. doi:10.1016/j.addr.2013.12.010
- Liao WH, Hsiao MY, Lo CW, et al. Intracellular triggered release of DNA-quaternary ammonium polyplex by ultrasound. Ultrason Sonochem. 2017;36:70–77. doi:10.1016/j.ultsonch.2016.11.002
- Ultrasound LK. Its Chemical, Physical, and Biological Effects. Kenneth S. Suslick, Ed. VCH, New York, 1988 xiv, 336 pp. illus. $65. Science. 1989;243(4897):1499. doi:10.1126/science.243.4897.1499-a
- Marin A, Sun H, Husseini GA, Pitt WG, Christensen DA, Rapoport NY. Drug delivery in pluronic micelles: effect of high-frequency ultrasound on drug release from micelles and intracellular uptake. J Control Release. 2002;84(1–2):39–47. doi:10.1016/s0168-3659(02)00262-6
- Mannaris C, Yang C, Carugo D, et al. Acoustically responsive polydopamine nanodroplets: a novel theranostic agent. Ultrason Sonochem. 2020;60:104782. doi:10.1016/j.ultsonch.2019.104782
- Husseini GA, Christensen DA, Rapoport NY, Pitt WG. Ultrasonic release of doxorubicin from Pluronic P105 micelles stabilized with an interpenetrating network of N,N-diethylacrylamide. J Control Release. 2002;83(2):303–305. doi:10.1016/s0168-3659(02)00203-1
- Lentacker I, De Cock I, Deckers R, De Smedt SC, Moonen CT. Understanding ultrasound induced sonoporation: definitions and underlying mechanisms. Adv Drug Deliv Rev. 2014;72:49–64. doi:10.1016/j.addr.2013.11.008
- Zullino S, Argenziano M, Stura I, Guiot C, Cavalli R. From micro- to nano-multifunctional theranostic platform: effective ultrasound imaging is not just a matter of scale. Mol Imaging. 2018;17:1536012118778216. doi:10.1177/1536012118778216
- Wang P, Yin T, Li J, et al. Ultrasound-responsive microbubbles for sonography-guided siRNA delivery. Nanomedicine. 2016;12(4):1139–1149. doi:10.1016/j.nano.2015.12.361
- Mulvana H, Browning RJ, Luan Y, et al. Characterization of contrast agent microbubbles for ultrasound imaging and therapy research. IEEE Trans Ultrason Ferroelectr Freq Control. 2017;64(1):232–251. doi:10.1109/tuffc.2016.2613991
- Ahmed SE, Martins AM, Husseini GA. The use of ultrasound to release chemotherapeutic drugs from micelles and liposomes. J Drug Target. 2015;23(1):16–42. doi:10.3109/1061186x.2014.954119
- Ulrich AS. Biophysical aspects of using liposomes as delivery vehicles. Biosci Rep. 2002;22(2):129–150. doi:10.1023/a:1020178304031
- Zhuang F, Ma Q, Dong C, et al. Sequential ultrasound-triggered and hypoxia-sensitive nanoprodrug for cascade amplification of sonochemotherapy. ACS Nano. 2022;16(4):5439–5453. doi:10.1021/acsnano.1c09505
- Shen J, Zhuo N, Xu S, et al. Resveratrol delivery by ultrasound-mediated nanobubbles targeting nucleus pulposus cells. Nanomedicine. 2018;13(12):1433–1446. doi:10.2217/nnm-2018-0019
- Kobayashi Y, Sakai D, Iwashina T, Iwabuchi S, Mochida J. Low-intensity pulsed ultrasound stimulates cell proliferation, proteoglycan synthesis and expression of growth factor-related genes in human nucleus pulposus cell line. Eur Cell Mater. 2009;17:15–22. doi:10.22203/eCM.v017a02
- Zhang X, Hu Z, Hao J, Shen J. Low intensity pulsed ultrasound promotes the extracellular matrix synthesis of degenerative human nucleus pulposus cells through FAK/PI3K/Akt pathway. Spine (Phila Pa 1976). 2016;41(5):E248–54. doi:10.1097/brs.0000000000001220
- Horne D, Jones P, Salgaonkar V, et al. Low intensity pulsed ultrasound (LIPUS) for the treatment of intervertebral disc degeneration. Proc SPIE Int Soc Opt Eng. 2017;10066. doi:10.1117/12.2255761
- Chen MH, Sun JS, Liao SY, Tai PA, Li TC, Chen MH. Low-intensity pulsed ultrasound stimulates matrix metabolism of human annulus fibrosus cells mediated by transforming growth factor β1 and extracellular signal-regulated kinase pathway. Connect Tissue Res. 2015;56(3):219–227. doi:10.3109/03008207.2015.1016609
- Thévenot J, Oliveira H, Sandre O, Lecommandoux S. Magnetic responsive polymer composite materials. Chem Soc Rev. 2013;42(17):7099–7116. doi:10.1039/c3cs60058k
- Bringas E, Köysüren Ö, Quach DV, et al. Triggered release in lipid bilayer-capped mesoporous silica nanoparticles containing SPION using an alternating magnetic field. Chem Commun. 2012;48(45):5647–5649. doi:10.1039/c2cc31563g
- Hu SH, Chen SY, Gao X. Multifunctional nanocapsules for simultaneous encapsulation of hydrophilic and hydrophobic compounds and on-demand release. ACS Nano. 2012;6(3):2558–2565. doi:10.1021/nn205023w
- Hu SH, Liu DM, Tung WL, Liao C-F, Chen S-Y. Surfactant‐free, self‐assembled PVA‐iron oxide/silica core–shell nanocarriers for highly sensitive, magnetically controlled drug release and ultrahigh cancer cell uptake efficiency. Adv Funct Mater. 2008;1186:18. doi:10.1002/adfm.200701210
- Hu SH, Chen SY, Liu DM, Hsiao CS. Core/single-crystal-shell nanospheres for controlled drug release via a magnetically triggered rupturing mechanism. Adv Mater. 2008;20(14):2690–2695. doi:10.1002/adma.200800193
- Okada M, Kim JH, Yoon ST, Hutton WC. Pulsed Electromagnetic Field (PEMF) plus BMP-2 upregulates intervertebral disc-cell matrix synthesis more than either BMP-2 alone or PEMF alone. J Spinal Disord Tech. 2013;26(6):E221–6. doi:10.1097/BSD.0b013e31827caeb7
- Louguet S, Rousseau B, Epherre R, et al. Thermoresponsive polymer brush-functionalized magnetic manganite nanoparticles for remotely triggered drug release. Polym Chem. 2012;3(6):1408–1417. doi:10.1039/C2PY20089A
