Abstract
Chemotherapy offers a systemic cancer treatment; however, it is limited in clinical administration due to its serious side effects. In cancer medicine, the use of nanoparticles (NPs) drug delivery system (DDS) can sustainedly release anticancer drug at the specific site and reduce the incidence of toxicity in normal tissues. In the present study, we aimed to evaluate the benefit of a novel chemotherapeutic DDS and its underlying mechanisms. Daunorubicin (DNR) was loaded into poly (lactic-co-glycolic acid) (PLGA)-poly-l-lysine (PLL)-polyethylene glycol (PEG)-transferrin (Tf) NPs to construct DNR-PLGA-PLL-PEG-Tf-NPs (DNR-loaded NPs) as a DDS. After incubating with PLGA-PLL-PEG-Tf-NPs, DNR, and DNR-loaded NPs, the leukemia K562 cells were collected and the intracellular concentration of DNR was detected by flow cytometry, respectively. Furthermore, the effect of drugs on the growth of tumors in K562 xenografts was observed and the relevant toxicity of therapeutic drugs on organs was investigated in vivo. Meanwhile, cell apoptosis in the excised xenografts was measured by transferase-mediated dUTP nick-end labeling assay, and the expression of apoptosis-related proteins, including Bcl-2, Bax, Caspase-9, Caspase-3, and cleaved-PARP, was determined by Western blotting analysis. Results showed that DNR-loaded NPs increased intracellular concentration of DNR in K562 cells in vitro and induced a remarkable improvement in anticancer activity in the xenografts in vivo. The expression of Bcl-2 protein was downregulated and that of Bax, Caspase-9, Caspase-3, and cleaved-PARP proteins were obviously upregulated in the DNR-loaded NPs group than that in other ones. Interestingly, pathological assessment showed no apparent damage to the main organs. In summary, the results obtained from this study showed that the novel NPs DDS could improve the efficacy of DNR in the treatment of leukemia and induce apoptosis via intrinsic pathway. Thus, it can be inferred that the new drug delivery may be a useful clinical tool.
Introduction
Cancer is a major public health problem in the world. Frequent challenges encountered by current cancer therapies include nonspecific systemic distribution of chemotherapeutic agents, inadequate drug concentrations reaching the tumor, relatively short circulating half-lives, poor solubility, and limited ability to monitor therapeutic responses.Citation1 Current advances in biotechnology and related areas are aiding the discovery and rational design of many new classes of drugs, in which it is crucial to improve specific drug delivery methods.Citation2
As we know, nanoparticles (NPs) have been widely evaluated as carriers for the delivery of drugs and genes because of their small size, sustained-release characteristics,Citation3 ability to offer physical protection against ribonuclease (RNase) activity,Citation4 and ability of specifically targeting tumors for either drugs or genes.Citation5,Citation6 Owing to both active and passive targeting, NPs are a promising carrier system for the targeted delivery of chemotherapeutic agents, and serious systemic toxicity or adverse effects can be avoided.Citation7 Poly (lactic-co-glycolic acid) (PLGA) is one of the most effective biodegradable polymeric NPs, and it has been approved by the Food and Drug Administration for drug delivery and has been frequently used.Citation8 Poly-l-lysine (PLL) has an advantage of being water soluble, hydrodegradable, biodegradable, and biocompatible,Citation9 and so it is suitable for the backbone as a drug delivery carrier. Recently, it has been reported that PLL-modified PLGA NPs showed significantly higher amounts than unmodified PLGA NPs.Citation10 PLGA has a relatively rapid rate of hydrolysis,Citation11 and it could reduce systemic clearance rates and prolong circulation half-life in vivo when being coated with biocompatible polymers such as polyethylene glycol (PEG).Citation12
It is well known that the transferrin receptor (TfR) was highly expressed in metastatic and drug-resistant tumors, while it was lowly expressed in normal cells.Citation13 Given the differential expression of TfR between the normal cells and tumor tissue, targeted chemotherapeutic agents can efficiently differentiate them and deliver antineoplastic drugs to the tumor cells.Citation14,Citation15 Nano-based drug delivery, modified with targeted moieties, including transferrins (Tfs), can enhance selective cellular uptake through Tf-mediated processes, and increase therapeutic benefit through the ability to encapsulate high concentrations of drug to the tumor site.Citation16
Daunorubicin (DNR) is widely used in the treatment of leukemia. However, the undesirable properties including cumulative cardiotoxicity, which is one of the most serious side effects, lead to a very narrow therapeutic index;Citation17 there is a need to explore alternate formulations. In this study, we aimed to test a novel PLGA-PLL-PEG-Tf-based targeted NPs drug delivery system (DDS) in enhancing antitumor of a classical chemotherapeutic agent, DNR, on K562 cells in vitro and in vivo.
Materials and methods
Main materials
DNR was pursed from Main Luck Pharmaceuticals Inc (Shenzhen, People’s Republic of China), RPMI-1640 from Gibco Chemical Co. (Carlsbad, CA, USA), 10% heat-inactivated fetal bovine serum from Sigma-Aldrich Co (St Louis, MO, USA), Hematoxylin–Eosin Staining Kit from Beyotime Institute of Biotechnology (Shanghai, People’s Republic of China), In Situ Cell Death Detection Kit from Nanjing KeyGen Biotech Co Ltd (Nanjing, People’s Republic of China), and monoclonal for Western blotting from Santa Cruz Biotechnology Inc. (Dallas, TX, USA). All other reagents were of analytical grade.
Preparation and characterization of DNR-loaded NPs
PLGA-PLL-PEG-NPsCitation18 were provided by College of Pharmacy, Nanjing University of Technology. The conjugation was analyzed with 1H NMR, and then the PLGA-PLL-PEG-NPs-loaded DNR was prepared using a modified double-emulsion solvent evaporation/diffusion methodCitation19 and separated using ultracentrifuge (GL-20G-H; Shanghai Anting Scientific Instrument Factory, Shanghai, People’s Republic of China) for 30 minutes (4°C, 1,500 rpm). Then, PLGA-PLL-PEG-NPs-loaded DNR was well dissolved in phosphate buffered saline (PBS) using ultrasound treatment for 30 seconds and then Tf was added (Tf/PLGA-PLL-PEG molar ratio 8:1) with stirring at room temperature for 3 hours to conjugate with the surface of DNR-PLGA-PLL-PEG via CDI (N,N-carbonyldiimidazole) of PEG. Thereafter, DNR-PLGA-PLL-PEG-Tf-NPs (DNR-loaded NPs) were extracted using ultracentrifuge for 20 minutes (4°C, 1,500 rpm).
Mean particle size and ZP value of DNR-loaded NPs were determined by a Zetasizer 3000HS system (Malvern Instruments, Malvern, UK), the diameters and width of particle distribution were calculated using a volume distribution from the Gaussian distribution, and morphological evaluation was observed under transmission electron microscope (Hitachi Ltd, Tokyo, Japan). Meanwhile, drug loading efficiency was calculated as the percent ratio of actual amount of DNR encapsulated into PLGA-PLL-PEG-Tf-NPs to total amounts of DNR-PLGA-PLL-PEG-Tf-NPs. The drug entrapping efficiency of DNR was calculated as the actual amount of DNR encapsulated into PLGA-PLL-PEG-Tf-NPs vs the theoretical of DNR in DNR-PLGA-PLL-PEG-Tf-NPs, respectively.Citation19
Cell line and cell culture
Leukemia K562 cells were obtained from Institute of Hematology, Chinese Academy of Medical Sciences (Beijing, People’s Republic of China). The cells were cultured in RPMI-1640 media supplemented with 10% (v/v) fetal bovine serum, 100 U/mL penicillin, and 100 μg/mL streptomycin at 37°C in a humidified atmosphere containing 5% carbon dioxide. The cells used in experiments were in logarithmic growth phase.
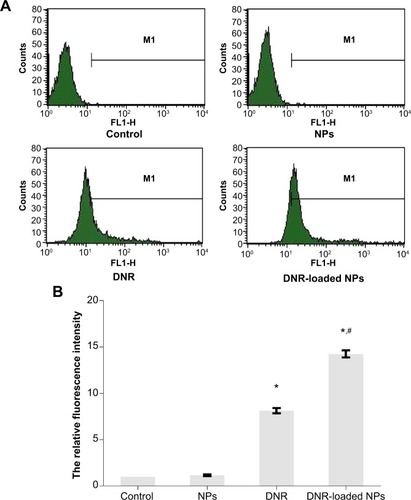
Cellular accumulation of DNR
Briefly, K562 cells were incubated with PLGA-PLL-PEG-Tf-NPs, DNR, and DNR-loaded NPs with equivalent concentration of DNR for 48 hours. Meanwhile, those were exposed to RPMI-1640 medium as control. Then cells were harvested and washed three times with phosphate buffered saline (PBS). Thereafter, cells were suspended in 500 μL PBS, and the cellular accumulation of DNR in each sample was directly detected by FACSCalibur flow cytometry (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) at excitation/emission wavelengths of 488/575 nm. The relative fluorescence intensity (RFI) of DNR was calculated as FItreated group/FIcontrol group.
Animals
Six-week age BALB/c nude mice, weighing 18–22 g, from the Shanghai National Center for Laboratory Animals were housed in cages under specific pathogen-free conditions where temperature was maintained at 22°C and humidity was in the range of 40%–50%, and sterile water and food were fed. All experiments involving the mice were carried out following the Guidelines for the Care and Use of Laboratory Animals of the National Institutes of Health.
Experimental design and animal treatments
Mice were subcutaneously inoculated into the left thigh with an injection of 1×107 K562 cells suspended in 0.2 mL of RPMI-1640 medium. Tumor sizes were measured with a digital caliper, and the tumor volumes were calculated according to the following formula: tumor volume V (mm3) =(1/2)×a×b2, where a is the largest diameter (length) and b is the smallest diameter (width) of the tumor. When tumors reached an average volume of approximately 50 mm3, animals were divided into four groups with six animals each for treatment as follows: Group 1, saline water (control); Group 2, PLGA-PLL-PEG-Tf-NPs; Group 3, free DNR (1 mg/kg for the single injection); and Group 4, DNR-loaded NPs (containing 1 mg/kg DNR for the single injection).
The intravenous treatments were done once every other day for 9 times for 18 days, and antitumor activity was determined by calculating the tumor volume as described earlier twice a week before sacrifice. After intravenous treatment for 18 days, mice were sacrificed and their xenograft tumors were harvested and processed for histopathologic analysis and determination of protein expression. During the whole experiment, the trial animals were monitored for signs of toxicity.
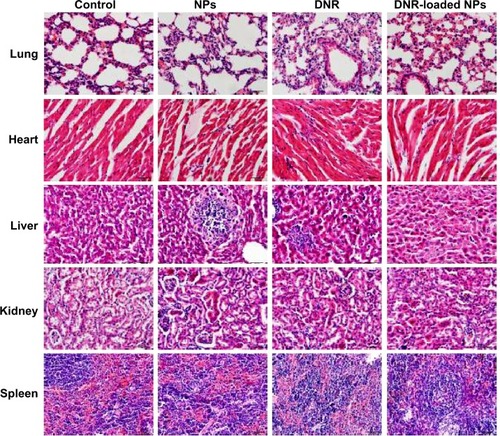
Histopathologic examination
After the mice were sacrificed, the lung, heart, liver, kidney, and spleen were quickly removed and immediately fixed in 4% paraformaldehyde, dehydrated in a graded series of alcohol, and then embedded in paraffin. Tissue sections (4 μm) were prepared and stained with hematoxylin and eosin. Thereafter, the sections were examined and micro-photographed by using Olympus IX51 microscope (400×; Olympus Corporation, Tokyo, Japan).
Transferase-mediated dUTP nick-end labeling
Based on the detection of single- and double-stranded DNA breaks by the terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) assay, analysis of apoptosis was performed using an In Situ Cell Death Detection Kit according to the manufacturer’s instructions. Tissue sections were analyzed to detect the localized green fluorescence of apoptotic cells and blue fluorescence of cell nuclei by fluorescence microscope; fluorescent images were acquired and photographed under the Olympus IX51 microscope (400×).
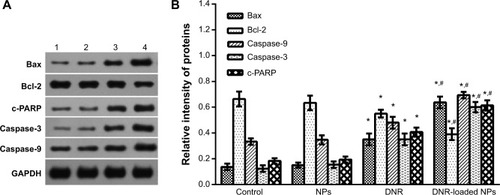
Western blot assays
In brief, the tissues were extracted with Triton X-100, and then the proteins were subjected to 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a polyvinylidene difluoride membrane. The membrane was blocked with buffer containing 5% skim milk. Thereafter, Western blotting was performed with the primary antibodies for Bcl-2, Bax, c-PARP, Caspase-3, Caspase-9, and GAPDH overnight at 4°C; and then with horseradish peroxidase-conjugated secondary antibody for 2 hours at room temperature. The protein bands were detected by enhanced chemiluminescence (ECL system; Amersham, UK) and analyzed by Gel-Pro32 software.
Statistical analysis
All experiments were performed three times. The results were presented as mean ± standard deviation, and data were analyzed with SPSS software (version 13.0; SPSS Inc, Chicago, IL, USA). The statistical significance of differences was determined by one-way analysis of variance among multiple groups, and differences with P<0.05 were considered statistically significant.
Results
Characterization of DNR-loaded NPs
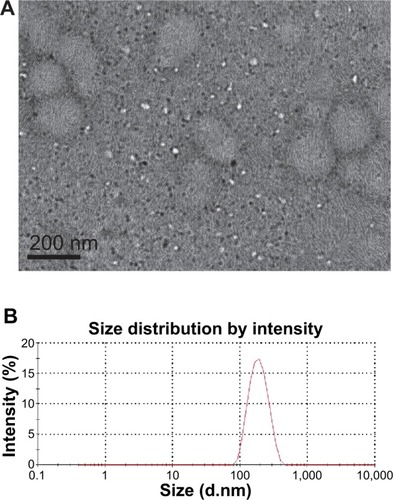
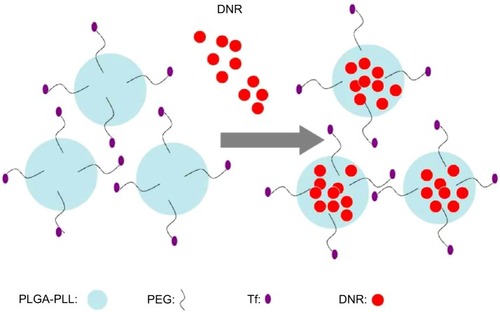
DNR-loaded NPs had a spherical shape and dispersed uniformly under transmission electron microscope (); the mean size and ZP of DNR-loaded NPs were 176.4±11.0 nm ( Size distribution by intensity) and −19.24±0.12 mV, respectively. shows the schematic representation of DNR loading into NPs. The drug entrapping efficiency was 75.12%±1.68%, and the loading efficiency was 5.32%±0.15%. All these results demonstrated that DNR-loaded NPs were relatively homogenous in size and stably stored.
Intracellular DNR
The relative fluorescence intensity of intracellular DNR (FItreated group/FIcontrol group) in K562 cells was lower in DNR group than that in DNR-loaded NPs (equivalent DNR concentration) group (8.14±0.29 vs 14.26±0.39) (), and there was a significant difference between them (P<0.05, ). Otherwise, there was no significant difference between the PLGA-PLL-PEG-Tf-NPs group and the control groups (P>0.05, ). These results suggested that DNR modified by PLGA-PLL-PEG-Tf-NPs could be targeted successfully to leukemia cells.
Figure 3 Intracellular accumulation of DNR in K562 cells incubated for 48 hours by FCM assay (A). Intracellular relative fluorescence intensity associated with DNR (B).
Notes: *P<0.05 when compared with the control group and #P<0.05 when compared with the DNR group.
Abbreviations: DNR, daunorubicin; FCM, flow cytometry; NPs, nanoparticles.
Drug inhibits the growth of tumor tissue
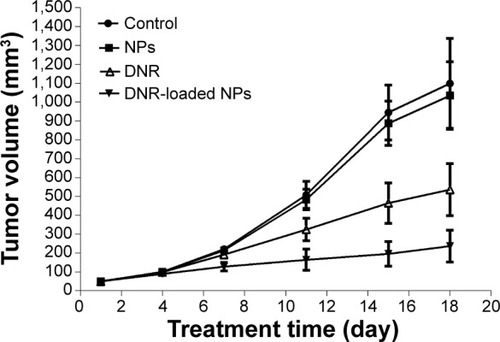
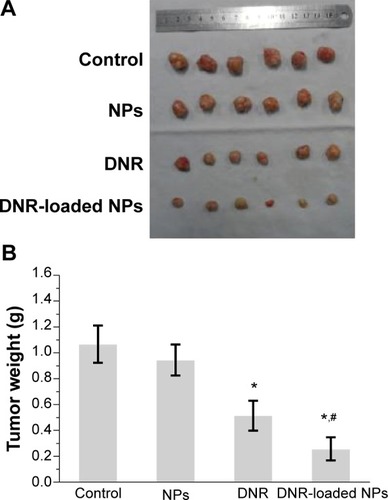
After intravenous treatment for 18 days, the mean tumor volume was 1,099±238 mm3 for the saline water group, 1,034±178 mm3 for the PLGA-PLL-PEG-Tf-NPs group, 536±137 mm3 for the DNR group, and 237±85 mm3 for the DNR-loaded NPs group (); and the inhibition of tumor growth in the DNR or DNR-loaded NPs groups was significantly higher than that in the PLGA-PLL-PEG-Tf-NPs group and the control group (P<0.05). Interestingly, the mean tumor volume in the DNR-loaded NPs group was smaller than that in the DNR group (P<0.05), while there was no significant difference between the PLGA-PLL-PEG-Tf-NPs group and control group (P>0.05). These results were further demonstrated by gross-observation (). Moreover, the weight of the tumors from the animals treated with either DNR or DNR-loaded NPs decreased significantly when compared with the PLGA-PLL-PEG-Tf-NPs group and control groups (P<0.05; ). Thus, we inferred that the DNR-loaded NPs had a greater antitumor efficacy than DNR (P<0.05).
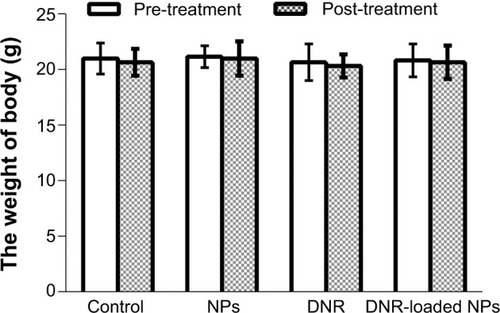
Toxicity in vivo
All the mice were alive, and they were weighed during the experiment period of 18 days. It is noteworthy that no significant differences in body weight (P>0.05; ) and no abnormal findings in any group were observed.
Figure 6 The body weight of mice pre- and post-treatment for various times.
Abbreviations: DNR, daunorubicin; NPs, nanoparticles.
Next, we carried out histological bioanalysis of organs to evaluate the potential side effects of NPs on the main organs of mice in vivo. There were no apparent histopathologic changes in the tissues, including lung, heart, liver, kidney, and spleen (). These results indicate that DNR-loaded NPs are safe and have no obvious toxic effects on the main organs of mice.
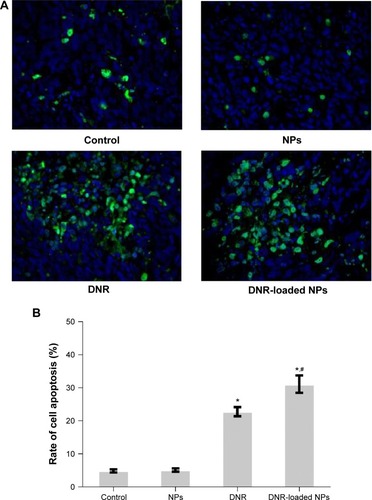
Analysis of cell apoptosis in K562 xenograft tumors
Samples were analyzed to detect the localized green fluorescence of apoptotic cells and blue fluorescence of cell nuclei using fluorescence microscope (). The percentage of apoptotic cells compared to the average number of cells per field was determined and graphically represented (). The apoptotic rate in DNR-loaded NPs group increased significantly compared with that in DNR group (P<0.05). However, there was no significant difference between the PLGA-PLL-PEG-Tf-NPs group and the control group (P>0.05), indicating that DNR-loaded NPs are a more effective drug treatment to achieve apoptosis than DNR (P<0.05).
Figure 8 Apoptotic cells in K562 xenograft tumors.
Notes: (A) Representative images of the TUNEL assay (green fluorescence of apoptotic cells and blue fluorescence of cell nuclei were detected using fluorescence microscope ×400); (B) rate apoptosis of each group. *P<0.05 when compared with control group, #P<0.05 when compared with DNR group.
Abbreviations: DNR, daunorubicin; NPs, nanoparticles.
Expression of Bcl-2, Bax, cleaved-PARP, Caspase-3, and Caspase-9
To explore the possible signaling pathways through which DNR-loaded NPs induced more anticancer activity, we examined the changes in the expression levels of apoptosis-related proteins by Western blotting. In our study, the levels of apoptosis regulating proteins Bcl-2 in both DNR group and DNR-loaded NPs group were downregulated while that of Bax was upregulated compared with the control group (P<0.05). In addition, the expression of Bcl-2 and Bax proteins in DNR-loaded NPs group was more obviously regulated than that in DNR group (P<0.05). The expression of Caspase-9 was upregulated in the DNR or DNR-loaded NPs group compared with the control group (P<0.05), and the increase was much more dramatic in the DNR-loaded NPs group than that in the DNR group (P<0.05; ). Similar results for Caspase-3 and cleaved-PARP were detected. Notably, the protein expression in the PLGA-PLL-PEG-Tf-NPs group was not obviously changed when compared with the control group (P>0.05).
Discussion
Current cancer treatments are restricted to chemotherapy, radiation, and surgery. Radiotherapy and surgery are largely localized in nature and fail to remove occult metastatic disease that can lead to eventual recurrence and poor patient survival. Nowadays, chemotherapy, particularly with respect to drug delivery, has evolved from traditional methodology.Citation20 DDS is an intriguing field of research that has captured the interest of researchers. Many studies focus on the safe and effective chemotherapeutic DDS, which can directly target tumor cells while sparing normal cells.Citation1 Targeted DDS can convey drugs more effectively and conveniently than chemotherapy in the past.Citation21
As we know, nanotechnology has provided a wide field of research among chemistry, biology, medicine, material science, engineering, and mathematics. These innovations are referred to as nanomedicines by the National Institutes of Health and have a significant impact on drug delivery. NPs as carrier can reduce the cytotoxic side effects and achieve targeting chemotherapy.Citation22,Citation23 We had previously evaluated the application of NPs and found that it would provide a promising strategy for chemotherapy.Citation24
Tfs are a family of homologous iron-binding glycoproteins. A growing number of studies have demonstrated that use of the Tf uptake pathway is highly effective in cancer therapy.Citation25 The TfR is a cell membrane-associated glycoprotein involved in the cellular uptake of iron and in the regulation of cell growth.Citation26 Many studies have shown that the level of TfR expressed in malignant cells is many times higher than their normal counterparts. Its expression can be correlated with tumor stage or cancer progression.Citation26,Citation27 Because of the elevated levels of TfR in malignancies, it can be targeted by directly conjugating with its ligand Tf or by monoclonal antibodies specific for the extracellular domain. Compared with free drugs, the combination of Tf targeting was highly effective in increasing levels of DNA double-stranded breaks and apoptosis in leukemia cells without accumulation of conjugate in normal cells, retaining the conjugate for longer periods of time, and declining the rate of chemotherapeutic agent efflux.Citation28 In an in vivo experiment, artemisinin-Tf conjugate demonstrated its ability to significantly retard the growth of breast cancer tumors in a rat model.Citation29 Tf-based DDS for cancer therapy has been tested to produce tumor responses without systemic toxicity in patients.Citation15 On the other hand, a possible limitation of Tf-based therapeutics is the short period that Tf remains within the cells to deliver its payload. Recently, nano-based drug delivery has been demonstrated to enhance the circulation time of targeted therapeutic drug.Citation15 In accordance with these findings, we aim to explore whether the targeted delivery of a therapeutic drug DNR-loaded NPs can improve therapeutic benefit in leukemia. Currently, 100–200 nm is accepted as the optimal size for DDS because nanocarriers take advantage of the EPR effect in tumors and avoid filtration in the spleen.Citation3 In the present study, spherical DNR-loaded NPs with diameters of 176.4±11.0 nm could be produced with a remarkably high DNR entrapping efficiency (75.12%±1.68%) and loading efficiency (5.32%±0.15%), which is suitable for drug delivery.
Drug targeting can be classified into two types: passive and active targeting. PEG-modification of NPs is useful to passively deliver the NPs to cancer tissues via an enhanced permeability and retention, avoiding the reticuloendothelial system.Citation30,Citation31 Active targeting allows the increased accumulation of drug in cancer tissue through specific interactions, such as antigen–antibody and ligand–receptor binding. Endocytosis plays a major role in active targeting.Citation15 The formulation of DNR-PEG-PLGA-PLL-Tf-NPs in our study was based on either passive or active processes. In vitro, we found that DNR-loaded NPs showed higher DNR accumulation than the DNR alone (). In vivo, the tumor volume of the mice injected with DNR-loaded NPs was smaller than that of the mice treated with DNR, and PLGA-PLL-PEG-Tf-NPs without DNR did not obviously affect the tumor volume in mice ( and ). These results indicated that DNR-loaded NPs showed more significant antitumor activity, and the intravenous delivery of DNR using NPs amplified the DNR antitumor that possibly elicited systemic targeting in leukemia. We infer that DNR-loaded NPs can be directly delivered into tumor cells by receptor-mediated endocytosis and drug-sustained release from NPs surface with the NPs skeleton degradation. Thereby, DNR-loaded NPs may render longer half-life of DNR in blood, and DNR concentration must be increased in the tumor tissue. Besides, there were no apparent histopathologic damages to the main organs of mice due to the size of the NPs.Citation32 Based on mice body weights, the tolerability of the NPs formulation was acceptable. These results may advocate the feasibility of reducing the dose and intensifying the tumor-tissue targeting ability of DNR.
Apoptosis is a physiological process of programmed cell death that is essential for normal tissue development, and resistance to apoptosis is a hallmark feature of cancer; therefore, apoptosis induction of cancer cells is one of the most important and direct ways to control the development of cancer and eliminate tumors. In our present study, extensive cell apoptosis by TUNEL assay was observed in tumor tissues of xenografts treated with DNR-loaded NPs compared to the control one. Studies have shown that apoptosis can be triggered via two distinct pathways: the extrinsic and the intrinsic or mitochondria pathway.Citation33 Once cellular stress signals arise, the intrinsic pathway is activated and then causes permeabilization of mitochondrial outer membrane, which allows Caspase-9-mediated mitochondrial damage, thereby activating the downstream member Caspase-3.Citation34 To further explore the possible apoptosis pathways through which DNR-loaded NPs induced targeted chemotherapy, we assayed the expressions of some key apoptosis-associated proteins, including Caspase-3, Caspase-9, and c-PARP. In our study, the level of Caspase-9, Caspase-3, and c-PARP proteins was remarkably elevated in DNR-loaded NPs group compared to other groups. As we know, one of the most important functions of PARP is to help repair single-stranded DNA nicks, and the cleaved-PARP is critically involved in the intrinsic apoptosis pathway and considered to be a marker of apoptosis.Citation35,Citation36 In the present study, we observed the expression of proapoptotic and antiapoptotic members of the Bcl-2 family, which is the mitochondrial-related death switch. The members of Bcl-2 homology are divided into three main groups based on function and regions of the domains: multi-domain anti-apoptotic proteins (Bcl-2, Bcl-xL, Bcl-w, Mcl-1, and A1), multi-domain proapoptotic proteins (Bax and Bak), and BH3-only proapoptotic proteins (Bid, PUMA, Bim, and NOXA), trigger the activation of Bak and Bax.Citation37 Our present results showed that the level of Bcl-2 protein was downregulated by the treatment of DNR-loaded NPs, compared to DNR group, whereas that of Bax was upregulated, and the ratio of Bax to Bcl-2 was increased. Taken together, these data indicate that DNR-loaded NPs can activate the intrinsic signaling pathway to trigger leukemia cells apoptosis.
Conclusion
In summary, the results obtained from the current study demonstrate that the novel NPs DDS enhances the activity of traditional anticancer drug DNR against leukemia cells through activation of the intrinsic apoptosis by both active and passive targeting pathways. This would ensure improved efficacy and minimize toxicity. Thus, novel NPs DDS may be a useful clinical tool.
Acknowledgments
This work was supported by the Jiangsu Province Health Department Medical Science and Technology Development Fund Project (No H201229), the National Natural Science Foundation of China (Nos 81170492, 81370673), the National High-Tech Research and Development Program 863 (No 2012AA022703), the National Key Basic Research Program 973 (No 2010CB732404), the National Innovative Research Program for College Students (No 1210286098), and Key Department of Jiangsu Medicine (No 2011-12).
Disclosure
The authors report no conflicts of interest in this work.
References
- SakhraniNMPadhHOrganelle targeting: third level of drug targetingDrug Des Devel Ther20137585599
- ParveenSMisraRSahooSKNanoparticles: a boon to drug delivery, therapeutics, diagnostics and imagingNanomedicine2012814716621703993
- PetrosRADeSimoneJMStrategies in the design of nanoparticles for therapeutic applicationsNat Rev Drug Discov2010961562720616808
- DavisMEZuckermanJEChoiCHEvidence of RNAi in humans from systemically administered siRNA via targeted nanoparticlesNature20104641067107020305636
- WoodrowKACuYBoothCJSaucier-SawyerJKWoodMJSaltzmanWMIntravaginal gene silencing using biodegradable polymer nanoparticles densely loaded with small-interfering RNANat Mater2009852653319404239
- ZhangJSunHMaPXHost-guest interaction mediated polymeric assemblies: multifunctional nanoparticles for drug and gene deliveryACS Nano201041049105920112968
- GeelsPEisenhauerEBezjakAPalliative effect of chemotherapy: objective tumor response is associated with symptom improvement in patients with metastatic breast cancerJ Clin Oncol2000182395240510856099
- AcharyaSSahooSKPLGA nanoparticles containing various anticancer agents and tumour delivery by EPR effectAdv Drug Deliv Rev20116317018320965219
- UmanoMUechiKUriudaTTumor accumulation of epsilon-poly-lysines-based polyamines conjugated with boron clustersAppl Radiat Isot2011691765176721439838
- TaharaKFurukawaSYamamotoHKawashimaYHybrid-modified poly(D,L-lactide-co-glycolide) nanospheres for a novel cellular drug delivery systemInt J Pharm201039231131320347023
- DuncansonWJFigaMAHallockKZalipskySHamiltonJAWongJYTargeted binding of PLA microparticles with lipid-PEG-tethered ligandsBiomaterials2007284991499917707503
- GrefRMinamitakeYPeracchiaMTBiodegradable long-circulating polymeric nanospheresScience1994263160016038128245
- RyschichEHusztyGKnaebelHPHartelMBüchlerMWSchmidtJTransferrin receptor is a marker of malignant phenotype in human pancreatic cancer and in neuroendocrine carcinoma of the pancreasEur J Cancer2004401418142215177502
- SinhaRKimGJNieSShinDMNanotechnology in cancer therapeutics: bioconjugated nanoparticles for drug deliveryMol Cancer Ther200651909191716928810
- TortorellaSKaragiannisTCTransferrin receptor-mediated endocytosis: a useful target for cancer therapyJ Membr Biol201424729130724573305
- TortorellaSKaragiannisTCThe significance of transferrin receptors in oncology: the development of functional nano-based drug delivery systemsCurr Drug Deliv20141142744324387131
- PetreCEDittmerDPLiposomal daunorubicin as treatment for Kaposi’s sarcomaInt J Nanomedicine2007227728818019828
- GuoLTChenBALiuRBiocompatibility assessment of polyethylene glycol-poly L-lysine-poly lactic-co-glycolic acid (PEG-PLL-PLGA) nano-particles in vitro and in vivoJ Nanosci Nanotechnol20141411024730249
- LiuJQiuZWangSZhouLZhangSA modified double-emulsion method for the preparation of daunorubicin-loaded polymeric nanoparticle with enhanced in vitro anti-tumor activityBiomed Mater2010506500220924138
- HaleyBFrenkelENanoparticles for drug delivery in cancer treatmentUrol Oncol200826576418190833
- SannaVPalaNSechiMTargeted therapy using nanotechnology: focus on cancerInt J Nanomedicine2014946748324531078
- SharmaAJainNSareenRNanocarriers for diagnosis and targeting of breast cancerBiomed Res Int2013201396082123865076
- KimBYRutkaJTChanWCNanomedicineN Engl J Med20103632434244321158659
- ZhangHWangCChenBWangXDaunorubicin-TiO2 nanocomposites as a “smart” pH-responsive drug delivery systemInt J Nanomedicine2012723524222275838
- BrandsmaMEJevnikarAMMaSRecombinant human transferrin: beyond iron binding and transportBiotechnol Adv20112923023821147210
- DanielsTRDelgadoTRodriguezJAHelgueraGPenichetMLThe transferrin receptor part I: biology and targeting with cytotoxic antibodies for the treatment of cancerClin Immunol200612114415816904380
- SinghMMuglerKHailooDWDifferential expression of transferrin receptor (TfR) in a spectrum of normal to malignant breast tissues: implications for in situ and invasive carcinomaAppl Immunohistochem Mol Morphol20111941742321297444
- SzwedMMatusiakALaroche-ClaryARobertJMarszalekIJozwiakZTransferrin as a drug carrier: cytotoxicity, cellular uptake and transport kinetics of doxorubicin transferrin conjugate in the human leukemia cellsToxicol In Vitro20142818719724055890
- LaiHNakaseILacosteESinghNPSasakiTArtemisinin-transferrin conjugate retards growth of breast tumors in the ratAnticancer Res2009293807381019846912
- FangJNakamuraHMaedaHThe EPR effect: unique features of tumor blood vessels for drug delivery, factors involved, and limitations and augmentation of the effectAdv Drug Deliv Rev20116313615120441782
- FumotoSKawakamiSCombination of nanoparticles with physical stimuli toward cancer therapyBiol Pharm Bull20143721221624492718
- KettigerHSchipanskiAWickPHuwylerJEngineered nanomaterial uptake and tissue distribution: from cell to organismInt J Nanomedicine201383255326924023514
- PackhamGStevensonFKBodyguards and assassins: Bcl-2 family proteins and apoptosis control in chronic lymphocytic leukaemiaImmunology200511444144915804279
- ElkholiRFlorosKVChipukJEThe role of BH3-only proteins in tumor cell development, signaling, and treatmentGenes Cancer2011252353721901166
- AgarwalAMahfouzRZSharmaRKSarkarOMangrolaDMathurPPPotential biological role of poly (ADP-ribose) polymerase (PARP) in male gametesReprod Biol Endocrinol2009714319961617
- DanialNNBCL-2 family proteins: critical checkpoints of apoptotic cell deathClin Cancer Res2007137254726318094405
- OltersdorfTElmoreSWShoemakerARAn inhibitor of Bcl-2 family proteins induces regression of solid tumoursNature200543567768115902208