Abstract
Background:
Active renin mass concentration (ARC) is independent of the endogenous level of angiotensinogen, and less variable and more reproducible than plasma renin activity. Reference values for the aldosterone-to-renin ratio (ARR) using ARC are still undefined. The objective of the present study was to determine the threshold of ARR using ARC measurement to screen for primary aldosteronism.
Methods:
A total of 211 subjects were included in the study, comprising 78 healthy normotensive controls, 95 patients with essential hypertension, and 38 patients with confirmed primary aldosteronism (20 with surgery-confirmed aldosterone-producing adenoma and 18 with idiopathic adrenal hyperplasia). Blood samples were drawn from ambulatory patients and volunteers in the mid-morning without specific dietary restriction for measuring plasma aldosterone concentration, ARC, and serum potassium.
Results:
Most normotensive controls and essential hypertension patients had ARR results below 100 pmol/ng, a value which corresponded to 3.3 times the median of these two groups.
Conclusion:
Patients with ARR values above this level should be considered for further investigation (confirmatory tests) or for repeat testing should ARR values be borderline. This study indicates that ARC can be used reliably in determining ARR for primary aldosteronism screening.
Introduction
Primary aldosteronism, as initially described by Conn,Citation1 is defined as an inappropriate and autonomous production of aldosterone by the adrenal glands. With improved screening approaches, such as the ratio of plasma aldosterone to renin levels (ARR), the average number of screened patients with primary aldosteronism has increased considerably.Citation2–Citation6 Plasma renin activity has been usually measured to define ARR.Citation7–Citation9 More recently, the use of active renin mass concentration (ARC), instead of the plasma renin activity assay, has gained broader acceptance.Citation10 Indeed, ARC does not require ice cooling of the specimen, is independent of the endogenous level of angiotensinogen, is easier to standardize, and is more reproducible than plasma renin activity. In addition, studies have demonstrated a significant correlation between plasma renin activity and ARC measurements,Citation11–Citation14 although this correlation is weaker at low renin levelsCitation7 but improved under captopril stimulation.Citation14 So far, only a few small studies have reported an ARR threshold using ARC measurements in screening for primary aldosteronism.Citation15–Citation18 The objective of the present study was to assess the value of ARC in determining ARR for primary aldosteronism screening.
Methods and materials
Blood samples for measuring plasma aldosterone concentration, ARC, and serum potassium were drawn according to the Endocrine Society Clinical Practice GuidelineCitation19 from ambulatory patients and volunteers in the mid-morning at the outpatient clinic of the L’Hôtel-Dieu de Québec Hospital, a tertiary care center. Informed consent was obtained for all subjects, as required by the local ethics committee. Preliminary data for the current study has been reported previously.Citation20 The control group was recruited from normotensive subjects (blood pressure below 140/90 mmHg) coming for routine blood samples. Patients with a history of hypertension, diabetes, or with cardiac, hepatic, or renal diseases were excluded. Hypertensive patients had the same blood samples drawn while being investigated for hypertension. Patients were diagnosed with essential hypertension when clinical and laboratory investigation excluded any secondary forms of hypertension. Among patients referred to us for sustained hypertension and hypokalemia, those with primary aldosteronism were included retrospectively in the analysis. The ARR using plasma renin activity or ARC was not measured prior to referral. Our initial investigation of these patients showed that they had low ARC, high plasma aldosterone concentrations, and increased ARR values. A definite diagnosis of primary aldosteronism was confirmed in all patients by demonstrating an inappropriate autonomous hypersecretion of aldosterone with captopril suppression and salt loading procedures as described previously.Citation21 Subtyping investigations included computed tomography imaging with fine cuts (2.5–3.0 mm) and a postural stimulation test in all patients.Citation22 Adrenal venous sampling (10 patients) and/or adrenal scintigraphy using 6 beta 131-iodomethyl-19-norcholesterol after dexamethasone suppression (six patients) were performed in patients with conflicting results. Beta-blockers, clonidine, renin-angiotensin blockers, and thiazide diuretics were withdrawn progressively one week prior to the investigation. Spironolactone was discontinued six weeks prior to blood sampling. Postsynaptic α1 blockers and calcium channel blockers were maintained or added when necessary to control hypertension. No subject in any of the three groups was taking oral contraceptive pills.
Blood was collected in EDTA tubes for ARC and plasma aldosterone measurement, maintained at room temperature during delivery to the laboratory, and rapidly frozen at −20°C after centrifugation. Plasma ARC was determined using a two-site immunometric assay (Renin III Generation, Cisbio Bioassays, Bedford, MA). Typical imprecision in the normal range for this assay shows coefficients of variation below 4% within-run and below 7.5% between-run. Reference values ranged from 7 ng/L to 25 ng/L in the recumbent position and from 12 ng/L to 43 ng/L after ambulation. Plasma aldosterone concentration was measured by radioimmunoassay according to the manufacturer’s recommendations (DSL-8600 kit, Beckman Coulter, Fullerton, CA). Typical imprecision in the normal range for this assay shows coefficients of variation below 7% within-run and below 10% between-run. Reference values with patients in the recumbent position ranged from 90 pmol/L to 290 pmol/L and after normal ambulation from 290 pmol/L to 871 pmol/L. Serum potassium was determined using an autoanalyzer system (Ilab 1800 or Beckman LX-20).
Statistical analysis
Results are expressed as mean ± standard error of the mean. The unpaired Student’s t-test was used to establish statistically significant differences between groups. Two approaches were tested to establish cutoff values and to assess sensitivity and specificity; the first one was based on laboratory reference values (upper limit for aldosterone and lower limit for renin) and the second one corresponded to the optimal discriminator from receiver-operating characteristic (ROC) curves (point closest to the upper left corner). For ARR, we used the 95th percentile for the controls and essential hypertension patients. ROC curves were generated and their surfaces evaluated using the Mann–Whitney U test. For the ROC curves, controls and essential hypertension results were pooled to assess specificity. Statistical assessments of proportions were done using the χ2 test and Cohen’s kappa test.
Results
A total of 211 subjects were included in the study, comprising 78 healthy normotensive controls, 95 patients with essential hypertension, and 38 patients with confirmed primary aldosteronism (20 had surgery-confirmed unique aldosterone-producing adenoma and 18 were presumed to have idiopathic adrenal hyperplasia). presents the patient characteristics and basal biochemical determinations. The mean age of control subjects was lower but not significantly different from the other two patient groups. Plasma aldosterone and ARR values were significantly higher (P < 0.01), and ARC and serum potassium values were significantly lower (P < 0.01) in primary aldosteronism patients. Mean ARR values were not significantly different in patients with unique adenoma and with idiopathic adrenal hyperplasia (614 ± 169 pmol/ng versus 414 ± 91 pmol/ng, P > 0.05). depicts individual values for plasma aldosterone, ARC, and ARR from the subjects in all three groups. ARR values (bottom graph) discriminate better between the primary aldosteronism patients, essential hypertension patients, and control subjects. shows comparisons between the two approaches used to establish cutoff values in screening for primary aldosteronism (upper and lower limits of laboratory references or 95th percentile values and ROC curve analysis). The results show that the ROC curve analysis has the best sensitivity and specificity in establishing cutoff values for ARR. shows ROC curves for plasma aldosterone concentration, ARC, and ARR. ARR values above 130 pmol/ng detected primary aldosteronism with a sensitivity and specificity of 100%. provides the area under the ROC curves ±standard error of the mean and 95% confidence intervals.
Figure 1 Individual values of plasma aldosterone, active renin mass concentration (ARC) and aldosterone to renin ratio (ARR) in the three groups.
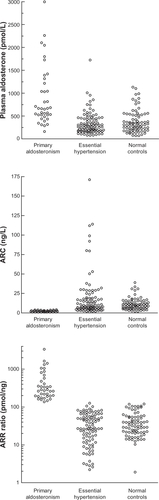
Figure 2 Analysis of receiver-operating characteristic curves. Circle, plasma aldosterone; triangle, active renin mass concentration; square, aldosterone to renin ratio.
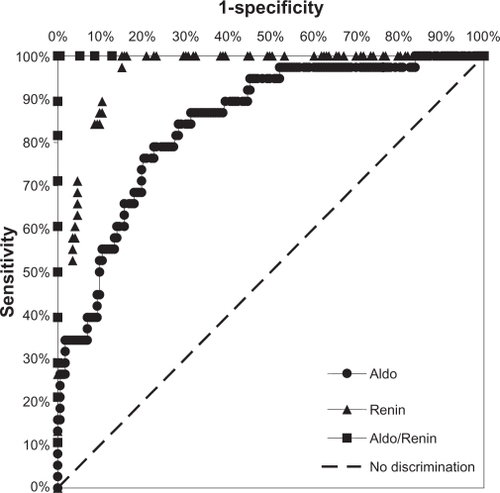
Table 1 Clinical and biochemical data
Table 2 Comparison of cutoff values derived from the upper limits of laboratory references or 95th percentile values and those from the receiver-operator characteristic curve
Table 3 Area under the receiver-operator characteristic curve ± standard error of the mean and confidence intervals
There were significant correlations between serum potassium and ARR (r = −333, P < 0.001), and ARC (r = +0.304, P < 0.001) and aldosterone (r = −0.274, P = 0.007). All but three patients with essential hypertension had an ARR below 100 pmol/ng (106, 102, 126 pmol/ng; range 2–126 pmol/ng). When repeated, the ratio value of 126 pmol/ng decreased to 56 pmol/ng. All primary aldosteronism patients had ARR values above 130 pmol/ng (range 137–3349 pmol/ng). The mean ARR in normotensive subjects was 42.4 ± 3.3 pmol/ng (range 2–118); five subjects were above 100 pmol/ng (104, 103, 104, 105, and 118 pmol/ng). shows suggested screening thresholds for ARR.
Table 4 Suggested screening thresholds for aldosterone-to-renin ratio using active renin mass concentration (pmol/ng)
Discussion
In the present study, which included control subjects and patients with essential hypertension and primary aldosteronism, we used ARC to define ARR in screening for primary aldosteronism. Patients with essential hypertension and control subjects had similar mean ARR values (mostly below 100 pmol/ng). ARR results above 130 pmol/ng indicated primary aldosteronism with a sensitivity and specificity of 100%. ARR results that fall between 100 pmol/ng and 130 pmol/ng (gray zone) suggest a need for repeat testing.
So far, few laboratories have attempted to establish reference values for ARR by using ARC expressed as pmol/ng. In a group of 36 hypertensive patients (nine with adrenal adenoma), Ferrari et alCitation12 reported that an ARR ≥ 150 pmol/ng can indicate primary aldosteronism. Perschel et alCitation16 measured ARR in 76 healthy normotensive volunteers and 28 primary aldosteronism patients. No patients with essential hypertension were included in that study. Their proposed cutoff value for ARR in normotensive volunteers versus primary aldosteronism patients was 118 pmol/ng. The cutoff value adopted by Westerdahl et alCitation18 to separate essential hypertension was 100 pmol/ng.
To our knowledge, the current report is the largest study in this area, and included control subjects, essential hypertensives, and primary aldosteronism patients. We compared two approaches to establish the cutoff values for plasma aldosterone, ARC and ARR (). The ROC curve analysis was clearly the best performing test, and ARR showed the highest sensitivity and specificity in detecting primary aldosteronism.
The combination of an ARR cutoff value with a plasma aldosterone threshold (>416 pmol/L or >15 ng/dL) has been suggested by some investigators.Citation8 This approach limits the number of false positive ARR, namely in patients with low renin essential hypertension, which represents around 25% of essential hypertension. However, to this end, it is important to use ambulatory plasma aldosterone values. Indeed, many patients with idiopathic adrenal hyperplasia exhibit normal early-morning plasma aldosterone values in the recumbent position, but their plasma aldosterone concentrations increase markedly with ambulation.Citation22
As for many screening tests performed without rigorous conditions throughout daily routine blood samplings, we observed borderline ARR results overlapping the proposed cutoff values. For this reason, we introduced the notion of a “gray zone” to help clinicians sort out patients in whom ARR should be repeated. In such cases, more attention should be paid to sampling conditions, ie, dietary sodium intake and serum potassium concentration, with careful revision and adjustment of medication. In addition, it is important to point out that the thresholds reported in the current paper cannot be applied universally, and should be adapted to each laboratory depending on the assays utilized. To this end, the median values (see ) can be used as comparison points; for instance, the proposed ARR threshold for control subjects and essential hypertension (100 pmol/ng) corresponds to 3.3 times the median value of these two groups.
The use of the ARR appears to be the preferred screening approach for distinguishing between patients with essential hypertension and those with primary aldosteronism.Citation10,Citation23 In past years, the ARR was based almost exclusively on plasma renin activity measurements. More recently, the utilization of ARC, instead of plasma renin activity, has gained acceptance. Indeed, studies have revealed a significant correlation between ARC and plasma renin activity assays.Citation11–Citation14 Moreover, the immunometric method to measure ARC offers many advantages over the plasma renin activity procedure. These advantages include this method being easier to standardize than the enzymatic assay, which can be altered by variation in the concentration of the endogenous angiotensinogen, having a better interlaboratory and intralaboratory coefficient of variation and reproducibility that allows comparisons between different laboratories,Citation24 and angiotensin II being more closely correlated with immunoreactive renin than with plasma renin activity.Citation25,Citation26 Recent methods have improved the sensitivity of the assay, which can now be used to assess suppressed renin levels.Citation27 Because of these advantages, ARC is progressively becoming the preferred method for measuring renin in humans. A recent study by Wu et alCitation17 showed that ARC is as accurate as plasma renin activity when using the captopril suppression confirmatory test. In conclusion, this study indicates that ARC can be used reliably to determine ARR when screening for primary aldosteronism. Patients with essential hypertension usually have ARR values ≤ 100 pmol/ng, while ARR in patients with primary aldosteronism is ≥130 pmol/ng. Results that fall between 100 and 130 pmol/ng (gray zone) suggest a need for repeat testing.
Disclosure
The authors report no financial or other relationships that might lead to a conflict of interest in this work.
References
- ConnJPrimary aldosteronism, a new clinical syndromeJ Lab Clin Med19554531713233623
- YoungWFJrPrimary aldosteronism: a common and curable form of hypertensionCardiol Rev1999720721410423672
- GordonRDStowasserMTunnyTJHigh incidence of primary aldosteronism in 199 patients referred with hypertensionClin Exp Pharmacol Physiol1994213153187923898
- FardellaCEMossoLGomez-SanchezCPrimary hyperaldosteronism in essential hypertensives: prevalence, biochemical profile, and molecular biologyJ Clin Endocrinol Metab2000851863186710843166
- LimPODowEBrennanGHigh prevalence of primary aldosteronism in the Tayside hypertension clinic populationJ Hum Hypertens20001431131510822317
- LohKCKoayESKhawMCPrevalence of primary aldosteronism among Asian hypertensive patients in SingaporeJ Clin Endocrinol Metab2000852854285910946893
- SealeyJEGordonRDManteroFPlasma renin and aldosterone measurements in low renin hypertensive statesTrends Endocrinol Metab200516869115808804
- YoungWFPrimary aldosteronism: renaissance of a syndromeClin Endocrinol (Oxf)20076660761817492946
- RossiGPSecciaTMPalumboGWithin-patient reproducibility of the aldosterone: renin ratio in primary aldosteronismHypertension201055838919933925
- RossiGPSecciaTMPessinaACClinical use of laboratory tests for the identification of secondary forms of arterial hypertensionCrit Rev Clin Lab Sci20074418517175520
- UngerNLopez SchmidtIPittCComparison of active renin concentration and plasma renin activity for the diagnosis of primary hyperaldosteronism in patients with an adrenal massEur J Endocrinol200415051752315080782
- FerrariPShawSGNicodJActive renin versus plasma renin activity to define aldosterone-to-renin ratio for primary aldosteronismJ Hypertens20042237738115076197
- de BruinRABouhuizenADiederichSValidation of a new automated renin assayClin Chem2004502111211615502082
- RossiGPBarisaMBelfioreAThe aldosterone-renin ratio based on the plasma renin activity and direct renin assay for diagnosing aldosterone-producing adenomaJ Hypertens2010281892189920683340
- TrenkelSSeifarthCSchobelHRatio of serum aldosterone to plasma renin concentration in essential hypertension and primary aldosteronismExp Clin Endocrinol Diabetes2002110808511928071
- PerschelFHSchemerRSeilerLRapid screening test for primary hyperaldosteronism: ratio of plasma aldosterone to renin concentration determined by fully automated chemiluminescence immunoassaysClin Chem2004501650165515247156
- WuVCKuoCCChangHWDiagnosis of primary aldosteronism: comparison of post-captopril active renin concentration and plasma renin activityClin Chim Acta201041165766320117105
- WesterdahlCBergenfelzAIsakssonAHigh frequency of primary hyperaldosteronism among hypertensive patients from a primary care area in SwedenScand J Prim Health Care20062415415916923624
- FunderJWCareyRMFardellaCCase detection, diagnosis, and treatment of patients with primary aldosteronism: an Endocrine Society clinical practice guidelineJ Clin Endocrinol Metab2008933266328118552288
- RacineMCDouvillePLebelMFunctional tests for primary aldosteronism: value of captopril suppressionCurr Hypertens Rep2002424524912003708
- AgharaziiMDouvillePGroseJHCaptopril suppression versus salt loading in confirming primary aldosteronismHypertension2001371440144311408392
- PlamondonIAgharaziiMDouvillePMorning plasma aldosterone predicts the subtype of primary aldosteronism independant of sodium intakeClin Exp Hypertens20072912713417364612
- MulateroPStowasserMLohKCIncreased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continentsJ Clin Endocrinol Metab2004891045105015001583
- MorgantiAA comparative study on inter and intralaboratory reproducibility of renin measurement with a conventional enzymatic method and a new chemiluminescent assay of immunoreactive reninJ Hypertens2010281307131220224432
- MenardJGuyenneTTCorvolPDirect immunometric assay of active renin in human plasmaJ Hypertens19853Suppl 3S275S278
- JuilleratLNussbergerJMenardJDeterminants of angiotensin II generation during converting enzyme inhibitionHypertension1990165645722172161
- DeinumJDerkxFHSchalekampMAImproved immunoradiometric assay for plasma reninClin Chem19994584785410351994