Abstract
End-stage renal disease (ESRD) patients are at much higher risk of cardiac arrest as compared to the general population. In the event of a cardiac arrest, cardiopulmonary resuscitation (CPR) is a lifesaving procedure. In fact, the need for CPR among hospitalized ESRD patients is almost 20 times higher than the general population. Complications of CPR include thoracic injuries such as flail chest, rib fractures, pneumothorax, and rarely intra-abdominal complications. Hemoperitoneum is a well-recognized complication among peritoneal dialysis patients but as a complication of CPR is rarely described. Inappropriate CPR technique, hepatic ischemia and venous congestion, platelet dysfunction, and the use of anti-platelet agents can increase the risk of such injury and bleeding. Hemoperitoneum in this setting can be serious with significant complications and may require transition from peritoneal dialysis (PD) to hemodialysis. We report two such PD patients who developed hemoperitoneum as a complication after CPR and their course.
Introduction
Hemoperitoneum is a known complication among peritoneal dialysis (PD) patients with an incidence of 6%, often due to any trauma from PD catheter, bleeding tendencies due to hematological disorders, obstetric and gynecologic disorders, rupture of hepatic or splenic or renal cysts, and abdominal trauma.Citation1,Citation2 Women of childbearing age can experience such episodes as a result of reflux menstruation, endometriosis, ovulation, and follicular cysts bleeding.Citation1,Citation2 Hemoperitoneum as a result of cardiopulmonary resuscitation (CPR) among PD patients is extremely rare.Citation3 We report two PD patients who developed such complication after CPR ().
Table 1 Baseline Demographics and Outcomes of Hemoperitoneum Because of CPR Among PD Patients
Case 1
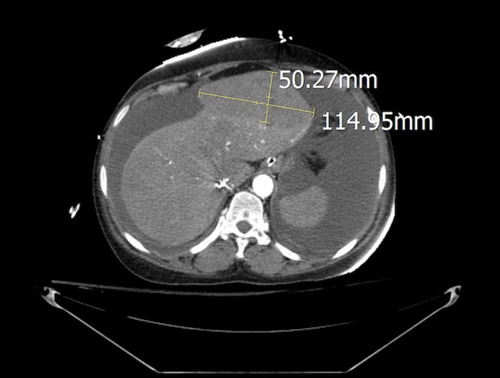
A 48-year-old African-American female with a history of hypertension, cardiovascular disease, and end-stage renal disease (ESRD) treated with automated PD (APD) since August 2019 was admitted to the hospital with worsening shortness of breath which was attributed to community-acquired pneumonia. Her home medications included dual anti-platelet therapy– aspirin 81 mg once daily and ticagrelor 90 mg twice a day. Continuous ambulatory peritoneal dialysis (CAPD) using 2.5% dextrose solution (Dianeal) with a fill volume of 2000 mL and dwell time of 4 h targeting five exchanges per 24 h was initiated. On day one, the patient went into cardiac arrest and received CPR for 12 min before return of spontaneous circulation (ROSC). Peritoneal dialysis was held during this time and resumed on day two. At that time, effluent was noted to be grossly hemorrhagic and hematocrit abruptly decreased from 41% to 28%. Analysis of PD fluid revealed 664,149 red blood cells (RBC)/mm3. A total of four-unit packed RBCs were transfused on that day to manage the anemia secondary to acute blood loss. Contrast-enhanced computed tomographic (CECT) imaging showed a large left hepatic subcapsular hematoma (11 x 5 x 8 cm) without active extravasation which was managed conservatively as per the surgery team recommendations (). Her anti-platelet agents were discontinued. She was switched to intermittent hemodialysis on day two due to the severity of hemoperitoneum. Once the patient was clinically stable and anemia stabilized, CAPD was resumed on day 8 which she tolerated well with adequate ultrafiltration. The patient was discharged on day 19 and continued to be managed successfully with APD in the ambulatory setting.
Case 2
A 39-year-old Hispanic female with a past medical history of diabetes mellitus, hypertension, cerebrovascular disease, and ESRD on APD since 2018 was admitted to the hospital in July of 2020 with COVID-19 pneumonia. Her home medications included aspirin 81 mg once daily. She was managed with CAPD using 2.5% dextrose solution (Dianeal) with a fill volume of 2000 mL and dwell time of 4 h targeting 5 exchanges per 24 h. The patient was transferred to the intensive care unit on day three due to severe hypoxemia and acute respiratory failure. Peritoneal dialysis was continued during this time which she tolerated with adequate ultrafiltration and clearance. Dialysate effluent remained clear until she suffered cardiac arrest on day five. CPR was performed for 11 min with ROSC. PD was reinitiated on next day with the first exchange showing frank bloody output. The patient was noted to be hemodynamically unstable and required vasopressor support. Her hematocrit decreased from 30% to 19.7% which required transfusion of three units of packed RBCs. She was diagnosed with hemoperitoneum and temporarily switched to intermittent hemodialysis considering the severity of bleeding. Her aspirin was discontinued at that time. Her CECT imaging on day six did not show any evidence of active bleeding. Analysis of PD fluid revealed 705,556 RBC/mm3 (). Later, hematocrit stabilized at ~29%. She was transitioned back to CAPD, on day nine of hospital admission, which was tolerated well with an adequate ultrafiltration volume of 100–500 mL per exchange. The patient’s course was complicated by anoxic encephalopathy and she expired on day 16.
Discussion
The need for CPR among hospitalized ESRD patients (6.3%) is almost 20 times higher than the general population (0.3%).Citation4 CPR is an emergent lifesaving procedure which can greatly improve the chances of survival after cardiac arrest. During CPR, hands should be positioned in the center of the chest and provide compression to a depth of at-least 2 inches but not more than 2.6 inches due to the risk of injury.Citation5 In a report of 10 PD patients who received CPR, thoracic injuries such as flail chest (5 patients) and multiple rib fractures (4 patients) were common.Citation6 In a nationwide sample of hospitalized ESRD patients who received CPR (N=56,069), incidences of rib fracture, pneumothorax, and cardiac tamponade were 0.5%, 1.4%, and 0.4%, respectively. In this review, data on intra-abdominal injuries were not reported.Citation7
Intra-abdominal complications of CPR are rare. When they occur, they usually include injury to liver, spleen, and intestines.Citation8,Citation9 Both of our patients developed hemoperitoneum soon after CPR. Koutserimpas et al reported two cases of hemoperitoneum following CPR.Citation10 The first included a 29-year-old female who had a massive pulmonary embolism and developed left hepatic lobe laceration (5 cm) because of CPR. The second patient was a 62-year-old female that developed cardiac arrest after drowning. CPR was complicated by hemoperitoneum and gastric vessel injury was noted to be the source of bleeding. In a retrospective review of 2558 cardiac arrest patients, authors found only 15 cases (0.6%) of major liver injury. Left lobe of liver was the site of injury in most of the (N=11) patients.Citation11 The left lobe of liver is in close proximity to the xiphoid process which may predispose it to injury especially if the technique of CPR is not appropriate.Citation9 In an autopsy series of 203 patients who underwent CPR, 87 patients (42.8%) had an evidence of CPR-related injury. Of these, most had thoracic injuries and only two patients had intra-abdominal injuries.Citation12 Myocardial infarction and lung cancer were reported as the causes of death in these two patients with intra-abdominal injury. On the autopsy, the first case had a right hepatic lobe laceration (3 x 3 cm) with 600 mL of blood in the peritoneum. The second case also had a right hepatic lobe laceration (2 x 1 cm) with 500 mL of blood in the peritoneum. These findings suggest that intra-abdominal injury is uncommon among patients who receives CPR but can lead to significant blood loss when it happens.
Our first patient had left hepatic lobe subcapsular hematoma and an obvious source of hemoperitoneum. We suspect our second patient had some type of visceral injury that was likely no longer actively bleeding when the CT scan was performed on the following day. Alternative sources of bleeding could have been an omental injury from the PD catheter. However, this was not considered to be as likely considering the extent of blood loss. Hepatic ischemia and liver distension due to venous congestion secondary to cardiac arrest increase the risk of injury and subsequent bleeding as a result of CPR.Citation9 Moreover, ESRD patients are already at an increased risk of bleeding due to platelet dysfunction.Citation13 Both reported PD patients were on anti-platelet agents which likely enhanced their susceptibility to bleeding ().
Focused assessment with sonography in trauma (FAST) is a rapid screening test often utilized to diagnose hemoperitoneum as a result of trauma.Citation8 In a prospective study of 50 blunt trauma patients, authors compared findings of FAST with CECT, laparotomy, and autopsy. Overall, sensitivity, specificity, and accuracy of FAST were reported to be 80%, 75%, and 80%, respectively.Citation14 CT scan is the gold standard test for diagnosing intra-abdominal injuries. In a review of 113 adult patients with trauma, sensitivity and specificity of CT scan and angiogram in diagnosing active ongoing bleeding was similar as 75% and 100%, respectively. Importantly, bleeding among 25% of patients would have been missed with the use of CT scan alone without the use of angiogram.Citation15 Diagnosis of hemoperitoneum is relatively easy among PD patients due to frequent visualization of effluent. The Eastern Association for the Surgery of Trauma Practice Management Guidelines recommends conservative non-operative among hemodynamically stable patients with blunt liver injuries.Citation16 Angiography with embolization can be a treatment option among patients with evidence of active extravasation, which can be seen on CT scan as contrast blush.Citation16 Both of our patients were managed conservatively, as they did not show any active extravasation on the imaging tests.
Hemoperitoneum can have serious implications for PD patients depending upon the etiology. The management of hemoperitoneum in PD depends on the severity and cause of the bleeding. Several rapid exchanges can help distinguish between persistent versus acute events. Coagulopathy among patients with hemoperitoneum should be corrected. An addition of 500 U/L of heparin to the PD fluid is recommended to prevent catheter malfunction.Citation17 Hemoperitoneum was associated with severe anemia of acute blood loss requiring multiple transfusion among both patients. In addition, they both required transition from PD to intermittent hemodialysis. Despite the hemoperitoneum, peritoneal membrane function appeared to be preserved in both patients as they both tolerated PD with adequate ultrafiltration and solute control. In fact, in a retrospective review of CAPD patients (N=21) with recurrent hemoperitoneum (number of episodes=91), authors observed it as a benign complication without any lasting impact on PD technique or patient survival.Citation18
Conclusions
The need for CPR among ESRD patients can be quite high. It is a lifesaving procedure however it can be associated with thoracic and visceral injuries. Hemoperitoneum among PD patients after CPR is rare but can be a serious complication. It can lead to significant blood loss and may require transition from PD to hemodialysis. These transitions can expect to be temporary. Hence, appropriate technique of CPR is crucial to minimize the complications among ESRD patients.
Consent for Publication
Written informed consent was obtained from the patient or next of kin where patient was deceased, to have their data published.
Disclosure
NG and DBH have served on Nephrology Advisory Board meeting for Horizon Therapeutics. Danny B Haddad reports personal fees from Amgen, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- Dozio B, Scanziani R, Rovere G, Sangalli L, Sacerdoti S, Surian M. Hemoperitoneum in a continuous ambulatory peritoneal dialysis patient caused by a hepatocarcinoma treated with percutaneous embolization. Am J Kidney Dis. 2001;38(3):E11. doi:10.1053/ajkd.2001.2691511532713
- Balsera C, Guest S. Hemoperitoneum in a peritoneal dialysis patient from a retroperitoneal source. Adv Perit Dial. 2013;29:69–72.24344496
- Shah AD, Hu SL, Kerns ES. Hemoperitoneum after CPR in a peritoneal dialysis patient. Perit Dial Int. 2020;40(2):237–238. doi:10.1177/089686081988980332063203
- Wong SP, Kreuter W, Curtis JR, Hall YN, O’Hare AM. Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA Intern Med. 2015;175(6):1028–1035. doi:10.1001/jamainternmed.2015.040625915762
- Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417–435. doi:10.1161/CIR.0b013e31829d865423801105
- Tzamaloukas AH, Zager PG, Quintana BJ, Nevarez M, Rogers K, Murata GH. Mechanical cardiopulmonary resuscitation choice of patients on chronic peritoneal dialysis. Perit Dial Int. 1990;10(4):299–302.2096933
- Saeed F, Adil MM, Malik AA, Schold JD, Holley JL. Outcomes of in-hospital cardiopulmonary resuscitation in maintenance dialysis patients. J Am Soc Nephrol. 2015;26(12):3093–3101. doi:10.1681/ASN.201408076625908784
- Biswas S, Alpert A, Lyon M, Kaufmann C. Cardiopulmonary resuscitation complicated by traumatic hepatic laceration: a case report and review of literature. J Med Cases. 2017;8(3):93–97. doi:10.14740/jmc2775w
- Kapłon-Cieślicka A, Kosior DA, Grabowski M, Rdzanek A, Huczek Z, Opolski G. Coronary artery dissection, traumatic liver and spleen injury after cardiopulmonary resuscitation - a case report and review of the literature. Arch Med Sci. 2013;9(6):1158–1161. doi:10.5114/aoms.2013.3923524482665
- Koutserimpas C, Ioannidis A, Siaperas P, et al. Intra-abdominal hemorrhage following cardiopulmonary resuscitation: a report of two cases. Case Rep Emerg Med. 2018;4(2018):5243105.
- Meron G, Kurkciyan I, Sterz F, et al. Cardiopulmonary resuscitation-associated major liver injury. Resuscitation. 2007;75(3):445–453. doi:10.1016/j.resuscitation.2007.05.02317640792
- Kaldırım U, Toygar M, Karbeyaz K, et al. Complications of cardiopulmonary resuscitation in non-traumatic cases and factors affecting complications. Egypt J Forensic Sci. 2016;6:270–274. doi:10.1016/j.ejfs.2015.07.005
- Goel N, Jain D, Haddad DB, Shanbhogue D. Anticoagulation in patients with end-stage renal disease and atrial fibrillation: confusion, concerns and consequences. J Stroke. 2020;22(3):306–316. doi:10.5853/jos.2020.0188633053946
- Kumar S, Bansal VK, Muduly DK, et al. Accuracy of focused assessment with sonography for trauma (FAST) in blunt trauma abdomen-a prospective study. Indian J Surg. 2015;77(Suppl 2):393–397. doi:10.1007/s12262-013-0851-2
- Ahmed N, Kassavin D, Kuo YH, Biswal R. Sensitivity and specificity of CT scan and angiogram for ongoing internal bleeding following torso trauma. Emerg Med J. 2013;30(3):e14. doi:10.1136/emermed-2011-20037622505301
- Stassen NA, Bhullar I, Cheng JD, et al. Nonoperative management of blunt hepatic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S288–S293. doi:10.1097/TA.0b013e318270160d23114483
- Lew SQ. Hemoperitoneum: bloody peritoneal dialysate in ESRD patients receiving peritoneal. Perit Dial Int. 2007;27(3):226–233. doi:10.1177/08968608070270030317468466
- Tse KC, Yip PS, Lam MF, et al. Recurrent hemoperitoneum complicating continuous ambulatory peritoneal dialysis. Perit Dial Int. 2002;22(4):488–491. doi:10.1177/08968608020220040712322820