Abstract
Objective
Both the incidence and the prevalence of end-stage renal disease (ESRD) in elderly patients are increasing worldwide. Elderly ESRD patients have been found to be more prone to depression than the general population. There are many studies that have addressed the relationship between sleep quality (SQ), depression, and health related quality of life (HRQoL) in ESRD patients, but previous studies have not confirmed the association in elderly hemodialysis (HD) patients. Therefore, the aim of the present study was to demonstrate this relationship in elderly HD patients.
Patients and methods
Sixty-three elderly HD patients (32 females and 31 males aged between 65 and 89 years) were included in this cross-sectional study. A modified Post-Sleep Inventory (PSI), the Medical Outcomes Study 36-item short form health survey, and the Beck Depression Inventory (BDI) were applied.
Results
The prevalence of poor sleepers (those with a PSI total sleep score [PSI-4 score] of 4 or higher) was 71% (45/63), and the prevalence of depression was 25% (16/63). Of the 45 poor sleepers, 15 had depression, defined as a BDI score of 17 or higher. Poor sleepers had a significantly higher rate of diabetes mellitus (P = 0.03), significantly higher total BDI scores, and lower Physical Component Scale scores (ie, lower HRQoL) than good sleepers. The PSI-4 score correlated negatively with Physical Component Scale (r = −0.500, P < 0.001) and Mental Component Scale scores (r = −0.527, P < 0.001) and it correlated positively with the BDI score (r = 0.606, P < 0.001). In multivariate analysis, independent variables of PSI-4 score were BDI score (beta value [β] = 0.350, P < 0.001), Mental Component Scale score (β = −0.291, P < 0.001), and age (β = 0.114, P = 0.035).
Conclusion
Poor SQ is a very common issue and is associated with both depression and lower HRQoL in elderly HD patients.
Introduction
The prevalence of depression in elderly patients (those aged 65 years or older) may be as high as 40% in hospital and nursing home settings and 8%–15% in community settings.Citation1 Depression is a major contributor to health care costs associated with older populations, and it is projected to be the leading cause of disease burden in older populations by the year 2020.Citation2,Citation3 Both the incidence and the prevalence of end-stage renal disease (ESRD) in elderly patients are also increasing worldwide.Citation4,Citation5 Elderly ESRD patients, especially those with vascular risk factors, have been found to be more prone to depression than the general population.Citation6 In a meta-analysis, both the presence of chronic disease and poor self-reported health status were found to be risk factors for increased depression among the elderly, with poor self-reported health appearing to be more closely associated with depression than the presence of chronic disease.Citation7 The prognosis of these depressive states is poor. Clinical depression is a common psychiatric disorder and is associated with increased morbidity and mortality in ESRD patients.Citation8
Poor sleep quality (SQ) is not uncommon in hemodialysis (HD) patients; the prevalence of poor SQ in this population has been shown to range from 41% to 83%.Citation9,Citation10 Previous studies have shown that poor SQ in HD patients is associated with female sex, advanced age, depression, cardiovascular disease, dialysis vintage, poor dialysis quality, and poor health-related quality of life (HRQoL).Citation11,Citation12,Citation13 It is widely accepted that HRQoL is an important outcome of health care, both in the general population and in ESRD patients.Citation14 Also, as stated earlier, depressive mood has been found to be associated with morbidity and mortality in ESRD patients.Citation15,Citation16 There are many studies that have addressed the relationship between SQ, depression, and HRQoL in the general population;Citation17–Citation20 however, the data about SQ, depression, and HRQoL in elderly HD patients are limited. Kutner et alCitation21 reported that older dialysis patients are significantly prone to restless sleep. Because SQ is a modifiable risk factor and there are implications that improving SQ can also cure depression and improve HRQoL, the exact relationship between these issues should be examined in elderly HD patients. Therefore, the aim of this study was to investigate the association between SQ, depression, HRQoL, and independent variables of SQ in elderly HD patients.
Patients and methods
The present study is a subgroup analysis of a previous study by the authors.Citation11 A total of 233 ESRD patients receiving HD three times weekly over a period of more than 3 months at five centers in Konya, Turkey, between February and June 2006 were evaluated in this cross-sectional study. Patients aged 65 years or older were accepted as “elderly” patients. A review of medical records, including information on age, sex, weight, height, duration of renal replacement therapy, medications, and primary cause of ESRD, was undertaken. Exclusion criteria included (1) severe cognitive impairment, (2) inability to answer the questionnaire, (3) treatment with a sleep medication, (4) presence of chronic pain, (5) presence of chronic obstructive pulmonary disease, (6) presence of psychosis, (7) a past history of sleep disorders including dyssomnias (frequent awakening, hypervigilance, etc) and parasomnias (sleepwalking, bruxism, etc), (8) a past history of sleep apnea syndrome, and (9) patients younger than 65 years of age. Of the 233 ESRD patients evaluated, 63 elderly patients (aged between 65 and 89 years) who were willing to participate and who met the inclusion criteria were included in the study.
HD patients received dialysis three times a week for 4 hours each time. Patients were dialyzed with a standard bicarbonate-containing dialysate bath, using a biocompatible HD membrane (Fresenius Polysulfone®, FX-80 series; Fresenius Medical Care, Bad Homburg, Germany). Dialysate flow rates were set at 500 mL per minute and blood flow rates were kept between 250 and 300 mL per minute. Both the systolic and the diastolic blood pressures of patients were measured in the upright sitting position after 5 minutes or more of rest, using an Erka sphygmomanometer [PMS (Instruments) Ltd, Berkshire, UK] with an appropriate cuff size. Two readings were recorded for each individual, and the mean value of these two readings was defined as the blood pressure. Patients with a systolic blood pressure greater than 140 mmHg and a diastolic blood pressure of 90 mmHg or those who were already on antihypertensive treatment were assumed to be hypertensive.
In patients receiving HD, venous blood samples for biochemical analyses were drawn after an overnight fast before the midweek HD session. All biochemical analyses – including glucose, creatinine, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and plasma triglyceride concentrations – were performed using an oxidase-based technique and were measured by a Roche/Hitachi Modular System (Roche Diagnostics GmbH, Mannheim, Germany) in the Central Biochemistry Laboratory of Selcuk University, Konya, Turkey.
The institutional medical ethics committee of Selçuk University, Konya, Turkey, approved the study protocol, and written informed consent was obtained from all subjects included in the study.
Evaluation of SQ
To evaluate SQ, a modified Post-Sleep Inventory (PSI) was applied to all patients. The PSI was developed by Webb et alCitation22 to permit an adequate description of subjective responses to a preceding period of sleep. The PSI involves a questionnaire with three groups of opposing statements separated by an analog rating scale from 0 to 1. A score of 0 reflects a positive opinion about the patient’s SQ, while a score of 1 reflects a negative opinion. The aim is to classify the patient’s understanding about his or her SQ in terms of feelings at bedtime (PSI-1 score), quality of nocturnal sleep (PSI-2 score), and feelings at awakening (PSI-3 score). For this study, a total sleep score (PSI-4 score) was calculated by adding the PSI-1, PSI-2, and PSI-3 scores for each patient. The PSI-4 score could indicate no sleep problems at all (0), or mild (1–3), moderate (4–6), severe (7–9), or very severe (10–12) sleep problems.
Evaluation of HRQoL
The Medical Outcomes Study 36-item short form health survey was used to evaluate HRQoL.Citation23 The test comprises 36 items, which are assigned to eight dimensions – namely, (1) physical functioning (ten items), (2) physical role functioning (four items), (3) bodily pain (two items), (4) general health status (five items), (5) vitality (four items), (6) social functioning (two items), (7) emotional role functioning (three items), and (8) mental health (five items). Each scale is scored within a range of 0–100 – the higher the score, the better the HRQoL indicated. While the first four items constitute the Physical Component Scale (PCS), the remaining four items constitute the Mental Component Scale (MCS). These two summary scales have been shown to adequately represent values of their individual scale components with 80% and 85% variability, respectively.Citation24 This scale has been validated and is commonly used in patients with ESRD.Citation25,Citation26
Evaluation of depression
Depression was assessed using the Beck Depression Inventory (BDI), which had been validated and is commonly used in patients with ESRD.Citation15,Citation16 It has been reported that 85% of Western dialysis patients with BDI scores of 11 or higher meet the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, criteria for diagnosis of major depression.Citation15 In Hisli’sCitation27 validation and reliability study in a Turkish population, a BDI score of 17 or higher was determined as the cutoff value for the diagnosis of depression. Depression was also defined as a BDI score of 17 or higher in the present study.Citation28
Statistical analysis
All calculations were performed using a standard statistical software package (SPSS v 13.0 for Windows; SPSS Inc, Chicago, IL). The data are presented as the mean plus or minus the standard deviation, unless otherwise specified. The proportion of subjects with a PSI-4 score of 4 or higher determined the prevalence of poor sleepers. Student’s t-test was used to compare the means of normally distributed variables and the Mann-Whitney U test was used for variables that were not normally distributed. Differences among categorical variables were analyzed using the chi-square test or the two-tailed Fisher’s exact test as appropriate. Spearman correlation coefficients were used to examine associations between continuous variables. Multiple linear regression analysis with forward stepwise selection (P = 0.05) was performed to identify factors independently associated with the PSI-4 score. The level of significance (P-value) was 0.05 for all comparisons.
Results
The sociodemographic and clinical features of the patients in this study are shown in . The mean age of the patients was 70.5 ± 4.7 years and the mean dialysis vintage was 48.3 ± 35 months. The patients had a range of conditions: diabetic nephropathy (n = 19), chronic glomerulonephritis (n = 2), hypertensive nephropathy (n = 15), polycystic kidney disease (n = 2), chronic pyelonephritis (n = 5), and unknown (n = 20).
Table 1 Sociodemographic and clinical characteristics of elderly hemodialysis patients (n = 63)
The mean and median PSI-4 scores were 6.4 ± 3.6 and 6.0 (range, 0–12), respectively. The prevalence of poor sleepers (defined as those having a PSI-4 score of 4 or higher) was 71% (45/63), and the prevalence of depression in elderly HD patients was 25% (16/63) in this study.
The sociodemographic characteristics of the good sleepers compared with the poor sleepers are shown in . Of the 45 poor sleepers in this study, 15 had depression (ie, a BDI score of 17 or higher); however, of the 18 good sleepers in this study, only one had depression. The presence of diabetes was significantly higher in poor sleepers than in good sleepers (38% and 11%, respectively; P = 0.03). The mean BDI, PCS, and MCS scores of good sleepers were 10.4 ± 5.3, 56.9 ± 21.8, and 66.7 ± 20.5, respectively. Poor sleepers had significantly higher total BDI scores and lower PCS scores than good sleepers (). A comparison of the mean MCS scores of poor sleepers and good sleepers shows 56 ± 23 and 66.7 ± 20.5, respectively (P = 0.06).
Table 2 Sociodemographic and clinical characteristics of good versus poor sleepers
The correlations between the PSI-4 score and other continuous variables were studied. There was a significant negative correlation between PSI-4 score and PCS score (r = −0.500, P < 0.001) () and between PSI-4 score and MCS score (r = −0.527, P < 0.001) (). Additionally, there was a positive correlation of PSI-4 score with BDI score (r = 0.606, P < 0.001) (). In multivariate analysis, the independent variables of PSI-4 score were BDI score (beta value [β] = 0.350, P < 0.001), MCS score (β = −0.291, P < 0.001), and age (β = 0.114, P = 0.035) (). All of the dimensions of HRQoL were significantly higher in good sleepers than in poor sleepers ().
Figure 1 The correlation between Physical Component Scale (PCS) score and Post-Sleep Inventory total sleep score (PSI-4 score).
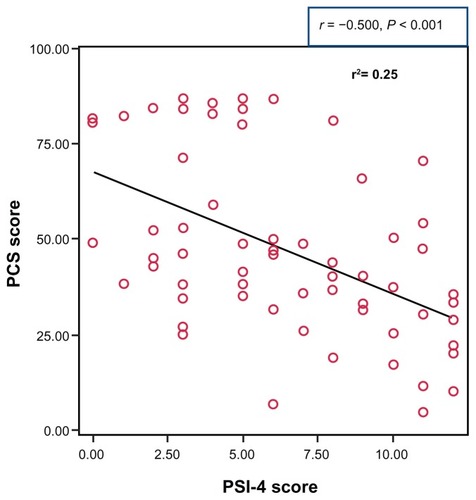
Figure 2 The correlation between Mental Component Scale (MCS) score and Post-Sleep Inventory total sleep score (PSI-4 score).
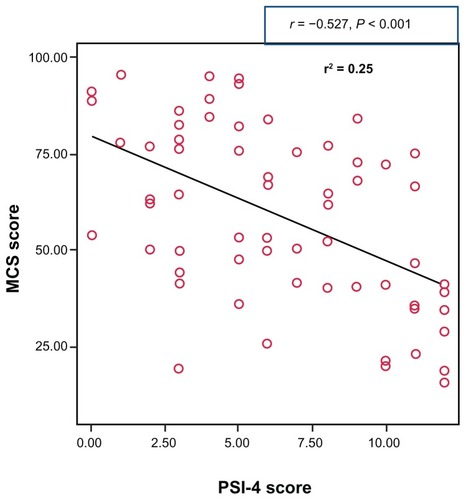
Figure 3 The correlation between Beck Depression Inventory (BDI) score and Post-Sleep Inventory total sleep score (PSI-4 score).
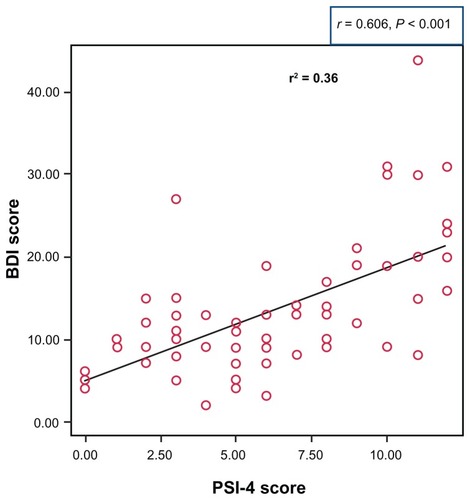
Table 3 Multiple linear regression models of independent variables of Post-Sleep Inventory total sleep score
Table 4 Dimensions of health-related quality of life (HRQoL) among good and poor sleepers
The authors also analyzed whether any correlation could be found between BDI score and smoking status, hypertension, and biochemical parameters (including parathormon, hemoglobin, and albumin levels). No relationship was found between PSI-4 score and smoking status, hypertension, and biochemical parameters. Also, none of the dimensions of HRQoL were correlated with these parameters (data not shown).
Discussion
There were four main findings of this study. First, the authors found the prevalence of poor sleepers (those with a PSI-4 score of 4 or higher) to be 71% in the elderly HD patients. Second, poor sleepers had significantly higher total BDI scores and lower PCS scores than good sleepers. Third, there was a significant inverse relationship between the PSI-4 score and the PCS and MCS scores; however, a positive correlation was found between the PSI-4 score and the BDI score. Fourth, in the multivariate analysis, the independent variables of the PSI-4 score were found to be BDI score, MCS score, and age.
To the best of the authors’ knowledge, this is the first study evaluating the relationship between SQ, depression, and HRQoL in elderly HD patients. In previous studies, the prevalence of poor SQ in HD patients has been reported as 41%–83%.Citation9–Citation11 In the present study, the prevalence of poor SQ in elderly HD patients was found to be 71% (45/63). This result shows that the prevalence of poor SQ in elderly HD patients is high, as also seen in the general HD population.
In the present study, the prevalence of depression in elderly HD patients was found to be 25% (16/63), which is similar to that found in previous studies.Citation28,Citation29 Several previous studies have reported a remarkable relationship between sleep alterations and depression in the general population. Elder et alCitation9 showed that depression was the only predictor of poor SQ. Along the same lines, Pai et alCitation10 also reported that poor sleepers had a higher BDI score than good sleepers and that this factor was one of the predictors of poor SQ in patients. Furthermore, Güney et alCitation30 concluded that poor SQ is a significant problem in peritoneal dialysis patients and suggested that regular assessment and management of SQ may be important for improvement of depression therapy in this population. Recently, Araujo et alCitation31 demonstrated that depressive symptoms are also independently associated with poor SQ in 400 patients on chronic HD. However, this relationship has been demonstrated less in elderly HD patients. In the present study, the authors observed that the elderly poor sleepers had a higher BDI score than the elderly good sleepers, which indicates that poor SQ is also associated with depression in the elderly HD population.
ESRD affects SQ at least by increasing the incidence of some specific sleep diseases.Citation32–Citation34 Previous studies have found SQ to be associated with HRQoL in ESRD patients, and patients with good SQ have been found more likely to have high MCS and PCS scores (ie, good HRQoL).Citation9,Citation11,Citation35 Recently, Li et alCitation36 demonstrated that SQ is also affected by malnutrition and calcium-phosphorus product in continuous ambulatory peritoneal dialysis patients. In the present study, the poor sleepers had lower PCS scores (ie, lower HRQoL) than the good sleepers, and there was a significant negative correlation between PSI-4 score and both MCS and PCS scores. In multiple linear regression analysis, BDI score, MCS score, and age were found to be independent variables of the PSI-4 score. These results were consistent with results from the authors’ previous study evaluating HD patients.Citation11
There are conflicting results in the literature regarding the role of gender, smoking status, and comorbidity in sleep diseases in patients with ESRD. Some studies have reported that female sex has a negative impact on SQ,Citation9,Citation10,Citation12 while other studies have reported that SQ is not affected by gender.Citation30,Citation35,Citation37–Citation39 Smoking cigarettes was also found to be associated with sleep diseases in someCitation9,Citation38 but not all studies.Citation12,Citation37 In the present study, only 8% of the patients were smokers and there was no relationship found between smoking and sleep diseases. This result could be attributed to the small sample size of elderly HD patients who smoked cigarettes, compared with the number of elderly HD patients who did not smoke.
Restless legs syndrome (RLS) has been found to be associated with diabetes in the general population.Citation40,Citation41 Although some of the increased risk of RLS in diabetes appears to be mediated through the presence of peripheral neuropathy, the association between RLS and diabetes remains significant, even in patients without neuropathy.Citation42 Epidemiologic data are increasingly attesting to the negative impact of RLS upon health. RLS is significantly associated with diminished quality of lifeCitation43 and depression.Citation44 RLS was not explored in the patients in the present study; however, the rate of diabetes was higher in poor sleepers than in good sleepers (38% and 11%, respectively) – this might explain the poor quality of sleep noted in the patients in the present study.
Cognitive behavioral therapy (CBT) is a psychotherapeutic approach that addresses dysfunctional emotions, behaviors, and cognitions through a goal-oriented, systematic process. CBT has six phases: (1) assessment, (2) reconceptualization, (3) skills acquisition, (4) skills consolidation and application training, (5) generalization and maintenance, and (6) post-treatment assessment follow-up.Citation45 CBT has been shown to have a role in the treatment plans for anxiety disordersCitation46 and depression.Citation47 CBT has been found to be an effective treatment for sleep disturbance and has been found to reduce inflammation in HD patients.Citation48 Recently, Chen et alCitation48 demonstrated that CBT is effective for correcting disorganized sleep patterns and that it reduced inflammation and oxidative stress in 72 sleep – disturbed HD patients. Therefore, CBT should be encouraged in HD patients.
This study had three main limitations. First, this was a cross-sectional analysis; this was not a prospective controlled study, so cause-and-effect relationships cannot be drawn from the findings. Second, the sample size was relatively small. Third, the diagnosis of sleep apnea syndrome depended on each patient’s past history; therefore, the authors could not ensure the diagnosis of sleep apnea syndrome was correct for each patient.
Conclusion
In conclusion, poor SQ is a very common issue and is found to be associated with depression and poor HRQoL in elderly HD patients. Social and economic environment, family status, life events, personality, and biological consequences of aging may be additional determinants of depression, poor SQ, and poor HRQoL in this population. Assessment of SQ and bystander factors such as depression and HRQoL and treatment of these factors should become a part of treatment for elderly dialysis patients.
Disclosure
The authors report no conflicts of interest in this work.
References
- LeonFGAshtonAKD’MelloDADepression and comorbid medical illness: therapeutic and diagnostic challengesJ Fam Pract2003SupplS19S3314693075
- GoodwinRDAssociation between physical activity and mental disorders among adults in the United StatesPrev Med200336669870312744913
- KatonWJLinERussoJUnutzerJIncreased medical costs of a population-based sample of depressed elderly patientsArch Gen Psychiatry200360989790312963671
- KurellaMCovinskyKECollinsAJChertowGMOctogenarians and nonagenarians starting dialysis in the United StatesAnn Intern Med2007146317718317283348
- CollinsAJFoleyRHerzogCExcerpts from the United States Renal Data System 2007 annual data reportAm J Kidney Dis2008511 Suppl 1S1S320
- PrinceMJBeekmanATDeegDJDepression symptoms in late life assessed using the EURO-D scale: effect of age, gender and marital status in 14 European centresBr J Psychiatry199917433934510533553
- Chang-QuanHXue-MeiZBi-RongDZhen-ChanLJi-RongYQing-XiuLHealth status and risk for depression among the elderly: a meta-analysis of published literatureAge Ageing2010391233019903775
- LopesAABraggJYoungEfor Dialysis Outcomes and Practice Patterns StudyDepression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and EuropeKidney Int200262119920712081579
- ElderSJPisoniRLAkizawaTSleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS)Nephrol Dial Transplant2008233998100417911092
- PaiMFHsuSPYangSYHoTILaiCFPengYSSleep disturbance in chronic hemodialysis patients: the impact of depression and anemiaRen Fail200729667367717763161
- GüneyIAtalayHSolakYPredictors of sleep quality in hemodialysis patientsInt J Artif Organs201033315416020383859
- SabbatiniMMinaleBCrispoAInsomnia in maintenance haemodialysis patientsNephrol Dial Transplant200217585285611981073
- TurkmenKYaziciRSolakYHealth-related quality of life, sleep quality, and depression in peritoneal dialysis and hemodialysis patientsHemodial Int201216219820622136456
- WuAWFinkNEMarsh-ManziJVChanges in quality of life during hemodialysis and peritoneal dialysis treatment: generic and disease specific measuresJ Am Soc Nephrol200415374375314978177
- KimmelPLPetersonRAWeihsKLMultiple measurements of depression predict mortality in a longitudinal study of chronic hemodialysis outpatientsKidney Int20005752093209810792629
- WatnickSKirwinPMahnensmithRConcatoJThe prevalence and treatment of depression among patients starting dialysisAm J Kidney Dis200341110511012500227
- MotivalaSJLevinMJOxmanMNIrwinMRImpairments in health functioning and sleep quality in older adults with a history of depressionJ Am Geriatr Soc20065481184119116913983
- MorganKClarkeDLongitudinal trends in late-life insomnia: implications for prescribingAge Ageing19972631791849223712
- Habte-GabrEWallaceRBColsherPLHulbertJRWhiteLRSmithIMSleep patterns in rural elders: demographic, health, and psychobehavioral correlatesJ Clin Epidemiol19914415131986057
- SchechtmanKBKutnerNGWallaceRBBuchnerDMOryMGGender, self-reported depressive symptoms, and sleep disturbance among older community-dwelling persons. FICSIT group. Frailty and Injuries: Cooperative Studies of Intervention TechniquesJ Psychosom Res19974355135279394268
- KutnerNGBliwiseDLBroganDZhangRRace and restless sleep complaint in older chronic dialysis patients and nondialysis community controlsJ Gerontol B Psychol Sci Soc Sci2001563P170P17511316835
- WebbWBBonnetMHWhiteRMState and trait correlates of sleep stagesPsychol Rep1976383 Pt 211811182935309
- WareJEJrSherbourneCDThe MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selectionMed Care19923064734831593914
- WareJEJrKosinskiMBaylissMSMcHorneyCARogersWHRaczekAComparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes StudyMed Care199533Suppl 4AS264AS2797723455
- JohansenKLPainterPKent-BraunJAValidation of questionnaires to estimate physical activity and functioning in end-stage renal diseaseKidney Int20015931121112711231369
- KuğleikaitėNBumblytėIAKuzminskisVVaičiūnienėRThe association between health-related quality of life and mortality among hemodialysis patientsMedicina (Kaunas)201046853153720966629
- HisliNA study about the validation of Beck Depression Inventory. Beck Depresyon Envanterinin geçerliliği üzerine bir çalışmaPsikoloji Dergisi19986118122 Turkish
- BalogunRATurgutFBalogunSAHolroydSAbdel-RahmanEMScreening for depression in elderly hemodialysis patientsNephron Clin Pract20111182c72c7721150214
- BrownEAJohanssonLFarringtonKBroadening options for long-term dialysis in the elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patientsNephrol Dial Transplant201025113755376320400451
- GüneyIBiyikMYeksanMSleep quality and depression in peritoneal dialysis patientsRen Fail200830101017102219016155
- AraujoSMde BruinVMDaher EdeDAlmeidaGHMedeirosCAde BruinPFRisk factors for depressive symptoms in a large population on chronic hemodialysisInt Urol Nephrol20124441229123521779919
- HanlyPJPierratosAImprovement of sleep apnea in patients with chronic renal failure who undergo nocturnal hemodialysisN Engl J Med2001344210210711150360
- CengićBResićHSpasovskiGAvdićEAlajbegovićAQuality of sleep in patients undergoing hemodialysisInt Urol Nephrol201244255756721152979
- MolnarMZNovakMMucsiISleep disorders and quality of life in renal transplant recipientsInt Urol Nephrol200941237338219184510
- UnruhMLBuysseDJDewMAfor Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) StudySleep quality and its correlates in the first year of dialysisClin J Am Soc Nephrol20061480281017699290
- LiJGuoQYeXPrevalence and risk factors of sleep disturbance in continuous ambulatory peritoneal dialysis patients in Guangzhou, southern ChinaInt Urol Nephrol201244392993621960370
- De VecchiAFinazziSPadalinoRSleep disorders in peritoneal and haemodialysis patients as assessed by a self-administered questionnaireInt J Artif Organs200023423724210832657
- MerlinoGPianiADolsoPSleep disorders in patients with end-stage renal disease undergoing dialysis therapyNephrol Dial Transplant200621118419016144846
- ChenWCLimPSWuWCSleep behavior disorders in a large cohort of Chinese (Taiwanese) patients maintained by long-term hemodialysisAm J Kidney Dis200648227728416860194
- PhillipsBYoungTFinnLAsherKHeningWAPurvisCEpidemiology of restless legs symptoms in adultsArch Intern Med2000160142137214110904456
- BergerKLuedemannJTrenkwalderCJohnUKesslerCSex and the risk of restless legs syndrome in the general populationArch Intern Med2004164219620214744844
- BenediktsdottirBJansonCLindbergEPrevalence of restless legs syndrome among adults in Iceland and Sweden: lung function, comorbidity, ferritin, biomarkers and quality of lifeSleep Med201011101043104820961808
- UlfbergJNyströmBCarterNEdlingCRestless legs syndrome among working-aged womenEur Neurol2001461171911455178
- AllenRPWaltersASMontplaisirJRestless legs syndrome prevalence and impact: REST general population studyArch Intern Med2005165111286129215956009
- GatchelRJRollingsKHEvidence-informed management of chronic low back pain with cognitive behavioral therapySpine J200881404418164452
- OtteCCognitive behavioral therapy in anxiety disorders: current state of the evidenceDialogues Clin Neurosci201113441342122275847
- DriessenEHollonSDCognitive behavioral therapy for mood disorders: efficacy, moderators and mediatorsPsychiatr Clin North Am201033353755520599132
- ChenHYChengICPanYJCognitive-behavioral therapy for sleep disturbance decreases inflammatory cytokines and oxidative stress in hemodialysis patientsKidney Int201180441542221654719