Abstract
Background
The impact of bacteriuria on mortality and cardiovascular risk has not been previously reported for patients with chronic kidney disease (CKD).
Objective
To assess the relationship between outpatient episodes of bacteriuria and mortality and cardiovascular risk among women with CKD.
Design
Retrospective cohort study using an electronic health database from an integrated healthcare system in central Pennsylvania.
Subjects
Adult women with CKD receiving primary care at Geisinger Health System between January 1, 2004 and December 31, 2009 were eligible, and were followed through December 31, 2010 for study outcomes.
Main measures
The study exposure was bacteriuria, defined as an outpatient urine culture with bacterial growth of 104 cfu/mL. Treatment history (antibiotic prescription within 90 days) was identified. Study outcomes were death and the composite of hospitalization for myocardial infarction, congestive heart failure, or stroke. Multivariate-adjusted Cox models incorporated all bacteriuria episodes and antibiotic prescriptions in time-dependent fashion (in addition to other covariates) to account for the cumulative impact of infections, treatment, and hospitalization during follow-up.
Key results
6807 women were followed for a median (interquartile range) of 5.2 (3.4, 5.9) years. In adjusted models, each untreated bacteriuria episode was associated with an increased risk of death (hazard ratio [HR] 1.56, 95% CI 1.35–1.81) and the composite cardiovascular outcome (HR 1.32, 95% CI 1.05–1.65); treated episodes were not associated with an increased risk of death or cardiovascular events.
Conclusion
Among female patients with CKD, untreated bacteriuria occurring in the outpatient setting is associated with an increased risk of death and cardiovascular morbidity.
Background
Patients with chronic kidney disease (CKD) suffer disproportionately from premature death and cardiovascular morbidity relative to those without CKD.Citation1–Citation3 Both traditional and nontraditional factors may contribute to this burden.
The period prevalence of bacteriuria among women over age 65 in the general population may be as high as 30%.Citation4 Patients with CKD are three times more likely to develop infections than those without CKD, and the urinary tract is the most common source in this population.Citation5 Unlike sepsis and pneumonia, urinary tract infections occur more commonly among those with non-dialysis requiring CKD than among those on dialysis.Citation5 Higher infection rates among patients with CKD may contribute to the burden of atherosclerotic cardiovascular disease due to systemic inflammation and free-radical derived endothelial dysfunction.Citation6–Citation9
Given the increased infection risk and cardiovascular disease burden among those with CKD, we sought to investigate the relationship between bacteriuria, treatment status, cardiovascular events, and death among a retrospective cohort of adult females with CKD who were not receiving dialysis. We were particularly interested in accounting for the impact of recurrent episodes as well as changing bacteriuria status over time, given that among older adults, transitions between states is common.Citation10 We hypothesized that untreated bacteriuria would increase the risk of death and cardiovascular events in this population.
Methods
This study was approved under “exempt” status by the Geisinger Medical Center Institutional Review Board on February 24, 2011.
Study setting and population
We retrospectively assembled a cohort of adult female patients receiving primary care within the Geisinger Health System. The data source was EpicCare®, Geisinger Medical Center’s (Danville, PA) electronic health record, which contains detailed demographic, lifestyle, pharmaceutical, procedural, laboratory, radiographic, vital, and other clinical data for more than 3.5 million patients receiving care at any of more than 40 outpatient clinics and three inpatient facilities in central Pennsylvania.
Patients eligible for the study were female, aged 18–88 at entry, with stage 1–5 CKD (non-dialysis dependent). We limited the cohort to female patients given that prostatism may confound the relationship between bacteriuria and outcomes among men.Citation11 Stage 1 CKD criteria included two or more outpatient episodes of proteinuria separated by at least 90 days, as well as one or more estimated glomerular filtration rate (eGFR) value(s) (derived using the CKD-EPI formula)Citation12 greater than 90 mL/minute/1.73 m2. Proteinuria was defined as a random urine protein-to-creatinine ratio of 0.2 g/g or greater, a 24-hour urine protein of 300 mg or greater, a urine dipstick reading of “1+” or greater, or random urine albumin-to-urine creatinine more than 30 μg/mg (“microalbuminuria”). Stage 2 CKD was defined using similar criteria for proteinuria, along with two outpatient eGFR readings between 60 and 89 mL/minute/1.73 m2, separated by at least 90 days. Stages 3–5 CKD were defined using eGFR criteria alone, with a requirement for at least two readings between 10 and 59 mL/minute/1.73 m2 separated by at least 90 days.
We excluded patients with a history of myocardial infarction, stroke, transient ischemic attack, or congestive heart failure; a history of solid-organ or bone marrow transplant; end-stage renal disease; structural kidney abnormality; neurogenic bladder or obstructive uropathy; chronic indwelling foley catheter, or history of nephrostomy tubes (collectively “kidney or urologic disorders”). Patients entered the cohort between January 1, 2004 and December 31, 2009, and were followed for study outcomes through December 31, 2010. Follow-up for outcomes began at the time an individual met all study entry criteria.
Exposure
The exposure of interest was bacteriuria, defined as growth from a urine specimen obtained in the outpatient setting of at least 104 cfu/mL. The date of the physician’s order for the culture was defined as the exposure date for those with a positive culture result. For the purposes of baseline comparison, patients were grouped by exposure and antibiotic treatment status, incorporating information from the entirety of the study period:
Group 1: no urine culture order, or all urine culture orders resulted in “no growth.”
Group 2: one or more positive urine cultures resulted, with an antibiotic prescription ordered within 90 days of each positive urine culture order date.
Group 3: one or more positive urine cultures resulted, without an antibiotic prescription ordered within 90 days of each positive urine culture order date.
Group 4: two or more positive urine cultures, with at least one treated and one not treated (with antibiotics) within 90 days of the urine culture order date.
Survival models incorporated exposure status (both infection and treatment status) as time-dependent variables by updating exposure history at each occurrence after study entry.Citation13 No distinction was made among various cultured organisms or antibiotic classes prescribed.
Outcomes
Study outcomes were (1) death and (2) a composite of hospitalization (primary discharge diagnosis) for one of the following cardiovascular events (International Classification of Diseases [ICD]-9-CM codes are in parentheses): myocardial infarction (411.1), congestive heart failure (425.4, 425.5, 425.7, 425.8, 428.*, 428.**), transient ischemic attack (435.8, 435.9), or cerebrovascular accident (433.01, 433.11, 433.21, 433.31, 433.91, 434.01, 434.11, 434.91, 431, 432.1, 432.0, 432.9). These diagnoses were obtained from hospital billing records. Information on vital status for Geisinger primary care recipients is updated monthly by institutional query of the Social Security Administration’s dataset through the National Technical Information Service.Citation14 Analysis of mortality was censored on December 31, 2010; analysis of the composite cardiovascular endpoint was censored at death or December 31, 2010, whichever occurred first.
Other variables
Variables included for baseline comparison and as potential covariates in survival models included age at cohort entry, race (self-reported by Geisinger primary care patients using the following, institution-specified categories: White or Caucasian, Black or African American, American Indian or Alaskan Native, Asian, or Native Hawaiian or Pacific Islander; race was included in this study due to known differences in cardiovascular risk among patients with CKD), smoking status (ever vs never), hospitalization during the 6 months prior to cohort entry, Charlson Co-Morbidity Index score, diabetes, hypertension, hyperlipidemia, peripheral arterial disease, dementia, chronic obstructive pulmonary disease, connective tissue disease (rheumatoid arthritis, systemic lupus erythematosis, polymyalgia rheumatica, dermatomyositis, or systemic sclerosis), coronary artery disease, history of malignancy, CKD stage at entry, and entry lab values (proteinuria, serum albumin, and eGFR). Hospitalization during follow-up was also included in survival models as a time-dependent covariate. Lab values closest and proximal (within 6 months) to the index date were used. Comorbid conditions were required to be coded on at least two separate outpatient physician encounters or listed as an active problem on the patient’s medical problem list within the prior 12 months.
Statistical analysis
Some patients did not have laboratory assessment of proteinuria or serum albumin during the baseline exposure window, therefore the values were coded using a variable to indicate whether or not this test was ordered.Citation15 Baseline comparisons between groups were made using the Kruskal–Wallis nonparametric and Pearson’s Chi-square tests, as appropriate. Rates of death and cardiovascular events were determined for each group and expressed as the number of events per 1000 person-years. A Poisson regression model was used to estimate the mortality rate across groups and expressed as incident rate ratios.
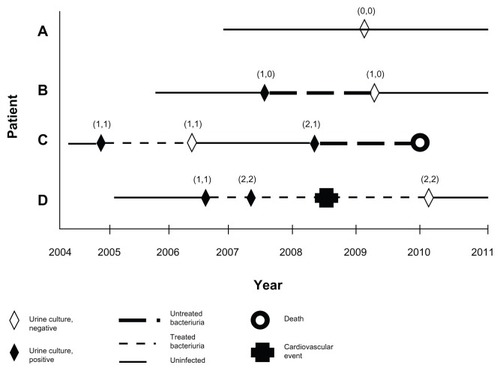
Time until death and the composite cardiovascular endpoint were analyzed using multivariate Cox proportional hazard regression models. Variables significant at P < 0.10 in the univariate analysis, or previously associated with death or cardiovascular events among patients with CKD, were included in the models. These multiple-determinant survival models incorporated information about each urine culture result and antibiotic treatment course (if any) during follow-up; in this manner, exposure status was continuously updated throughout the follow-up period to reflect changes in infection and treatment status ().Citation13 Multivariate adjusted subgroup analyses (stratified by age, smoking status, diabetic status, and CKD stage) were performed to examine the stability of the observed associations. Interaction testing across the specified subgroups was performed. P < 0.05 was considered significant.
Figure 1 Survival analysis incorporating time-dependent and cumulative characteristics of the exposure (bacteriuria) and treatment among females with chronic kidney disease. The figure shows four hypothetical cohort members (A–D) with various cohort entry dates and variable numbers of infections and antibiotic treatment courses during the study period.
Sensitivity analysis
Because other studies have treated a single (first) positive urine culture as the exposure without considering additional infections during follow-up,Citation16 we repeated the analyses limiting the exposure assessment to the first bacteriuria episode among those who were not treated, with comparison to those without a positive culture. In this manner, bacteriuria episodes occurring during follow-up were not accounted for, after the first positive culture, in order to mirror the methodologic approach of prior studies. All analyses were performed using SAS 9.2 (SAS Institute, Cary, NC).
Results
A total of 7471 patients were eligible for the study. Of these, 600 were excluded for a prior cardiovascular event (myocardial infarction, stroke or transient ischemic attack, or congestive heart failure), four for solid-organ or bone marrow transplant, 42 for end-stage renal disease, and 18 for kidney or urologic disorders.
Among the 6807 patients in the final cohort, 5796 (85.2%) were never infected (Group 1), 451 (6.6%) had only treated infections (Group 2), 428 (6.3%) had only untreated infections (Group 3), and the remaining 132 (1.9%) comprised the “mixed” treatment/no treatment group after a positive urine culture (Group 4). Baseline characteristics of the study cohort are shown in . Relative to those not infected, patients with bacteriuria were more likely to have diabetes, peripheral arterial disease, and proteinuria. Those in Group 3 were more likely to have been hospitalized in the 6 months prior to cohort entry than those in Group 2.
Table 1 Baseline characteristics of adult females with CKD, by outpatient bacteriuria and treatment status (2004–2009)
Among the overall cohort, during a median (interquartile range) follow-up of 5.2 (3.4–5.9) years, 784 (11.5%) patients died and 547 (8%) suffered a first cardiovascular event. Crude death and cardiovascular event rates were highest in Groups 3 and 4 (). Incidence rate ratios (95% CIs) for death (each of Groups 2, 3 and 4 vs Group 1) were 0.9 (0.7–1.2), 1.6 (1.3–2.0), and 1.1 (0.7–1.7), respectively, while those for the composite cardiovascular outcome were 2.5 (1.9–3.2), 3.0 (2.4–3.8), and 2.9 (1.9–4.3), respectively.
Table 2 Crude rates (death and cardiovascular events) among adult females with CKD, by bacteriuria and treatment status
In univariate analysis, factors associated with death (P < 0.10) included both treated and untreated infection, age, race, smoking status (ever vs never), hospitalization during 6 months prior to cohort entry as well as during follow-up, CKD stage at cohort entry, Charlson score, hyperlipidemia, peripheral arterial disease, chronic obstructive pulmonary disease, connective tissue disease, a history of cancer, coronary artery disease, and proteinuria. Factors associated with the composite cardiovascular outcome included both treated and untreated infection, age, race, hospitalization during 6 months prior to cohort entry as well as during follow-up, CKD stage at cohort entry, Charlson score, hyperlipidemia, diabetes, peripheral arterial disease, chronic obstructive pulmonary disease, connective tissue disease a history of cancer, coronary artery disease, and proteinuria.
Results of the Cox survival models are shown in . In unadjusted analyses, both treated (hazard ratio [HR] per cumulative episode 1.26, 95% CI 1.08–1.47) and untreated (HR per cumulative episode 1.86, 95% CI 1.62–2.13) events were associated with an increased risk of death; these risks persisted (HR per cumulative treated episode 1.32, 95% CI 1.13–1.54; HR per cumulative untreated episode 1.78, 95% CI 1.55–2.05) after adjustment for all covariates except hospitalization during follow up. When follow-up hospitalization was added to the survival models, risk associations were attenuated: HR for death per cumulative treated episode 0.96, 95% CI 0.81–1.14; HR for death per cumulative untreated episode 1.56, 95% CI 1.35–1.81. Similar results were observed for the composite cardiovascular outcome. In adjusted models, treated (HR per cumulative episode 1.34, 95% CI 1.10–1.62) and untreated (HR per cumulative episode 1.73, 95% CI 1.43–2.08) bacteriuria episodes each significantly increased the risk of a cardiovascular event, but the addition of follow-up hospitalizations attenuated this risk: treated (HR per cumulative episode 0.85, 95% CI 0.67–1.09) episodes were not associated with an increased risk, whereas the association with untreated episodes remained significant (HR per cumulative untreated episode 1.32, 95% CI 1.05–1.65).
Table 3 Cox proportional hazard model for mortality and cardiovascular events among adult females with CKD, by treatment status after bacteriuria
Among all positive culture results (n = 1487 episodes), 72.4% never resulted in a hospital admission after the culture result, while 5.2% were followed by an admission within 30 days and 14.9% were followed by an admission more than 180 days after the culture result.
Results were consistent across specified subgroups (age ≥ 65 vs <65, smoking status, diabetic status, and CKD stages 1 and 2 vs 3–5 [data not shown]). Tests for interaction among these subgroups were not significant (P > 0.15).
Sensitivity analysis
When limiting the exposure assessment to the first bacteriuria episode among those who were not treated, as opposed to accounting for all bacteriuria episodes, the results were consistent with the primary analysis: the multivariate-adjusted HR (95% CI) for death was 1.34 (1.07–1.68) for each untreated episode relative to those uninfected, whereas the composite cardiovascular endpoint was 2.55 (2.02–3.22) for untreated episodes.
Discussion
The results of this study suggest that older female patients with CKD who experience bacteriuria without treatment in the outpatient setting are at increased risk for both death and cardiovascular events.
No previous study has reported on these outcomes among those with CKD and bacteriuria. Abrutyn et al found that among a prospective cohort of ambulatory, elderly women, the crude risk of death associated with bacteriuria was increased.Citation16 However, this risk association disappeared when baseline comorbidities were accounted for in adjusted models. Survival analyses in their study utilized scheduled 6-month culture results in assigning exposure status, but accounted for unidirectional change in exposure status only (ie, from “non-infected” to “infected,” but not the reverse – those infected were presumed to be persistently infected regardless of subsequent culture results). The effects of cumulative bacteriuria events were not accounted for.
Other studies have also identified a risk associated with bacteriuria, but may have important limitations, to include a lack of adjustment for key confounding factors, and/or by misclassification bias due to limited information about infection recurrence, resolution, or persistence. Dontas et al identified a crude association between bacteriuria and increased mortality among a cohort of older nursing home subjects in Greece.Citation17 In this analysis, only the initial culture result was considered in assigning exposure status, and nearly 20% of the “unexposed” group at baseline subsequently developed bacteriuria during follow-up. Evans et al likewise found that a single positive urine culture was associated with a long-term increased risk (adjusted only for age and weight) of death among community-dwelling women living in Jamaica and Wales.Citation18 Others have not confirmed this association in studies which account for a number of important confounders more prevalent among those with urinary tract infections.Citation19
The explanation for the observations we report, and differences with previously reported analyses, may be related to any one of several factors. First, we studied by design a different population. Although speculative, the impact of bacteriuria may be different in a population with a greater burden of cardiovascular risk factors (such as those with CKD) than it is among general adult populations. Other studies have not generally included information about baseline kidney function, thus it is difficult to accurately assess differences in that regard between and among studies, but none have sought to explore these relationships in CKD populations specifically. Our study design does not permit analyses incorporating measures of inflammation or endothelial dysfunction, thus our findings are hypothesis-generating with respect to any relationship between bacteriuria and morbidity and mortality among those with CKD.
Second, the methods used in this analysis differ from those used in prior observational studies, and this in turn might account for the different results. Using an electronic health record from an integrated health care system we were able to incorporate the cumulative impact of both recurrent episodes of bacteriuria, the treatment associated with these episodes (if any), and a broad array of potential confounders known to be associated with the outcomes of interest. The importance of fully accounting for changes in exposure status when investigating bacteriuria should not be discounted, given the likelihood of both spontaneous resolution and recurrence in this population.Citation10 Misclassification bias is introduced when information about exposure status is limited to the first occurrence of bacteriuria.Citation13 Notably, our findings were generally consistent in sensitivity analysis, an approach modeled after the designs of previous studies in which exposure status was limited to the first infectious event. This would suggest that the risk associated with bacteriuria within the female CKD population itself may be distinctly different than in the adult, female, non-CKD population. Whether this is due to the interplay of bacteriuria with underlying comorbid diseases like diabetes among those with CKD, or differences in immunologic and nonspecific inflammatory responses in this population, remains speculative.
This study has both strengths and weaknesses. We used a detailed electronic health record to account for both exposure and treatment status throughout the study period, and thus limited misclassification of subjects. Loss to follow-up is not accounted for, though the outmigration rate for primary care patients at Geisinger was 1.1%–1.7% annually between 2006 and 2011 (Brenda L Eckrote, Senior Director, Finance, Geisinger Clinic Community Practice, email communication, February 6, 2012). Additional limitations of this study include its retrospective nature, and the potential for confounding by unmeasured covariates. We did not have information on markers of inflammation which might have informed the major study findings. Due to limitations imposed by electronic data capture, we did not distinguish between various infectious organisms, some of which would be more toxic than others. The study population mirrored the predominantly Caucasian population of central Pennsylvania, and extrapolation of study findings to more diverse populations would be inappropriate. Finally, the possibility that the relatively better outcomes associated with treated infections, relative to untreated, are due to differences in care patterns and quality among physicians within the Geisinger system should be considered.
In summary, this study suggests that older female patients with CKD and untreated bacteriuria occurring in the outpatient setting are at increased risk for death and major cardiovascular events, independent of factors previously shown to impact the risk of these outcomes. Additional analyses targeting an improved understanding of the link between bacteriuria and cardiovascular risk are warranted, as are confirmatory studies in other CKD populations.
Acknowledgment
The authors wish to thank Ms Amanda Bengier and Mr Joseph Leader for their assistance with data extraction and programming.
Disclosure
This study was presented at the annual meeting of The American Society of Nephrology, Philadelphia, PA, November 12, 2011. Dr Kirchner and Dr Perkins have received research funding unrelated to this work within the past 5 years from Amgen, Inc, and American Regent. Dr Perkins is an unpaid consultant for Mitsubishi-Tanabe, and has received reimbursement from them for travel expenses. The authors report no other conflicts of interest in this work.
References
- GoASChertowGMFanDMcCullochCEHsuCYChronic kidney disease and the risks of death, cardiovascular events, and hospitalizationN Engl J Med2004351131296130515385656
- MuntnerPHeJHammLLoriaCWheltonPKRenal insufficiency and subsequent death resulting from cardiovascular disease in the United StatesJ Am Soc Nephrol200213374575311856780
- United States Renal Data SystemUSRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End Stage Renal Disease in the United StatesMinneapolisUnited States Renal Data System20121 Available from: http://www.usrds.org/2010/slides/indiv/v1index.htmlAccessed February 8, 2012
- SouranderLBKasanenAA 5-year follow-up of bacteriuria in the agedGerontol Clin (Basel)19721452742814571598
- NaqviSBCollinsAJInfectious complications in chronic kidney diseaseAdv Chronic Kidney Dis200613319920416815225
- FoleyRNGuoHSnyderJJGilbertsonDTCollinsAJSepticemia in the United States dialysis population, 1991 to 1999J Am Soc Nephrol20041541038104515034107
- RidkerPMCushmanMStampferMJTracyRPHennekensCHInflammation, aspirin, and the risk of cardiovascular disease in apparently healthy menN Engl J Med1997336149739799077376
- RossRAtherosclerosis – an inflammatory diseaseN Engl J Med199934021151269887164
- RidkerPMHennekensCHBuringJERifaiNC-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in womenN Engl J Med20003421283684310733371
- BosciaJAKobasaWDKnightRAAbrutynELevisonMEKayeDEpidemiology of bacteriuria in an elderly ambulatory populationAm J Med19868022082143946436
- RuleADJacobsonDJRobertsROThe association between benign prostatic hyperplasia and chronic kidney disease in community-dwelling menKidney Int20056762376238215882282
- LeveyASStevensLASchmidCHCKD-EPI (Chronic Kidney Disease Epidemiology Collaboration)A new equation to estimate glomerular filtration rateAnn Intern Med2009150960461219414839
- StrickerBHStijnenTAnalysis of individual drug use as a time-varying determinant of exposure in prospective population-based cohort studiesEur J Epidemiol201025424525120358262
- National Technical Information Service[homepage on the Internet]AlexandriaNational Technical Information Service2012 Available from: http://www.ntis.gov/Accessed February 8, 2012
- CohenJCohenPMissing dataApplied Multiple Regression; Correlation Analysis for the Behavioral Sciences2nd edHillsdaleErlbaum1983275300
- AbrutynEMosseyJBerlinJADoes asymptomatic bacteriuria predict mortality and does antimicrobial treatment reduce mortality in elderly ambulatory women?Ann Intern Med1994120108278337818631
- DontasASKasviki-CharvatiPPapanayiotouPCMarketosSGBacteriuria and survival in old ageN Engl J Med1981304169399437207542
- EvansDAKassEHHennekensCHBacteriuria and subsequent mortality in womenLancet1982182641561586119524
- NordenstamGRBrandbergCAOdénASSvanborg EdénCMSvanborgABacteriuria and mortality in an elderly populationN Engl J Med198631418115211563960089