Abstract
Although surgical techniques, post-transplant care medicine, and immunosuppressants have been greatly improved, permanent acceptance of renal allograft remains a clinical challenge owing to the appearance of various influencing factors. To predict graft dysfunction, development of noninvasive biomarkers is becoming a highlighted research topic in the field of renal transplantation, which provides a possibility for physicians to give preemptive rescue treatment. From the viewpoint of diagnostic techniques, repetitive sampling is prerequisite to identify applicable biomarkers in the clinic. Early biomarkers can be used to dynamically monitor renal graft status and accurately predict transplant outcome independent of various confounders. This review highlights recent studies on the predictive value of biomarkers and methods to quantify biomarkers for monitoring kidney transplant. It is important to analyze and compare different biomarkers for living, and nonliving donors. Analysis of identified clinically relevant biomarkers will advance our understanding of distinct molecular and cellular mechanisms of transplantation and provide insight into developing novel potential approaches to induce transplant tolerance.
Introduction
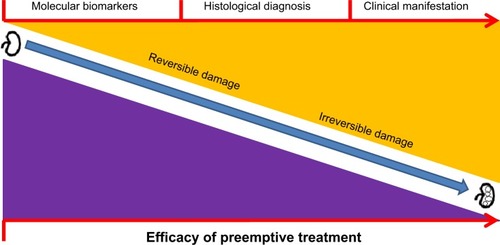
Currently, kidney transplantation remains an efficient and major therapeutic strategy for end-stage renal disease. Although surgical techniques and postoperative care have greatly advanced, achievement of long-term allograft survival remains a clinical challenge owing to various confounders, such as viral infection and nephrotoxicity.Citation1 Therefore, earlier detection and identification of renal graft status may guide clinicians in minimizing the risk of graft rejection events and provide decisive advice regarding withdrawal of immunosuppression.Citation1 Subsequent preemptive treatment can be adopted to prevent irreversible damage of graft and rescue allograft (). To this end, efficient implementation of biomarker identification can realize personalized therapy for renal transplant patients.Citation2
Figure 1 Schematic illustration of progress of renal graft damage, diagnostic techniques, and efficacy of preemptive treatment.
Indeed, biomarkers for monitoring graft function have been studied for decades.Citation1,Citation3 As molecular biological techniques are developing, various types of biomarkers have been successfully identified ();Citation1 however, no suitable biomarkers are widely used for renal transplant patients since clinical cases are normally complicated. Much of the data from experimental findings failed to connect bedside clinical applications. Therefore, standardization of identified biomarkers is required on a large scale in prospective multicenter trials.Citation2
Table 1 Biomarkers for specific conditions of donor kidney grafts
In practice, the ideal biomarkers for renal transplantation should be independently validated and standardized by multiple international centers,Citation4,Citation5 which can prove their reliability and reproducibility in parallel with corresponding histological analysis. It is encouraging that the European Union Reprogramming the Immune System for the Establishment of Tolerance Consortium undertook such collaborative studies in different European laboratories.Citation2 Bestard et al presented their very recent data in which a cross-validation of the interferon gamma enzyme-linked immunosorbent spot assay was used to assess the circulating alloreactive memory/effector T-cells for renal transplant patients.Citation5 Similarly, 12 US pediatric transplant programs cross-validated and analyzed a five gene-set (NKTR, PBEF1, MAPK9, DUSP1, PSEN1) with high accuracy for acute rejection in clinical renal transplantation.Citation4 Ideal biomarkers should also be capable of sensitively and specifically monitoring allograft function, independent of various confounding factors such as the influence of cytomegalovirus infection or donors from brain death (DBD).Citation1 Early identification and prognosis of graft dysfunction are also required so that a preemptive regimen can be promptly administered to prevent irreversible damage to the allograft. In addition, optimal biomarkers are expected to precisely reflect alteration of allograft function at an early stage.Citation1
Herein, our present review analyzes laboratory techniques for identifying biomarkers to better understand the development of diagnostic tools. Current studies on biomarkers for living and nonliving donors are discussed to acknowledge their predictive values and practical considerations.
Development of laboratory techniques for identifying novel biomarkers
Since creatinine cannot be used as an early marker for predicting or monitoring renal graft function, great efforts have been made to explore suitable biomarkers or parameters to prevent the occurrence of graft impairment.Citation1,Citation6 Indeed, the development of laboratory techniques has facilitated the production of novel biomarkers. Firstly, the real-time polymerase chain reaction (RT-PCR) is a sensitive and accurate technique, well-accepted to identify and validate potential biomarkers at the gene level for decades.Citation1 However, the data from RT-PCR is insufficient for high throughput screening and cannot meet researchers’ needs. As a replacement, microarray profiling arose to generate a large amount of potential biomarkers for comprehensive analysis on various renal transplant patients in different transplant scenarios.Citation4,Citation7,Citation8 During the past years, mass spectrometry analysis was employed to identify potential biomarkers at the protein level in patients’ serum samples.Citation9 Apart from specimens from peripheral blood, urine was utilized to identify qualified biomarkers for early detection of glomerular injury.Citation6 Research findings exhibited that urinary cystatin C, clusterin, and beta-2 microglobulin could significantly monitor kidney injury better than serum creatinine or blood urea nitrogen, as supported by in situ hybridization, gene and protein expression analysis, and immunohistochemistry.Citation6 Other multiple platforms are also used in empirical studies, such as enzyme-linked immunosorbent assay, flow cytometry, and immune cell functional assays, although their efficiency is unsatisfactory ().Citation10,Citation11 In addition, perfusate was utilized to detect applicable noninvasive biomarkers for renal transplant patients ().
Different types of biomarkers for renal allograft monitoring in kidney transplantation
Diverse confounding factors such as viral infection, malignancy, surgical complication, and nephrotoxicity from immunosuppressive drugs can affect graft function, and even survival.Citation1 Therefore, specific biomarkers were investigated for such varying clinical scenarios of kidney transplantation.Citation7–Citation9
First, transplant organs can be categorized into those received from living donors, and those from deceased donors. To some extent, the quality of donor organs determines transplant outcome.Citation12 It is well known that living donor organs function better than those from deceased donors. Accordingly, the biomarkers for kidney transplantation can be divided into two types: biomarkers for living donors, and biomarkers for deceased donors.Citation8
Biomarkers for living donor kidneys
Although living donors benefit patients in regard to long-term graft survival, no protocols for perfect tolerance induction exist in empirical transplantation. Graft dysfunction is always observed from a living donor. A study on 72 living-donor kidney transplant recipients who received total lymphoid irradiation or bortezomib was performed to identify sensitive biomarkers for preventing graft failure.Citation13 The findings exhibited that the level of donor-specific antibodies (DSA) steadily increased post-transplantation. Administration of prednisone could reduce DSA production, and an inverse association between prednisone dose and peripheral DSA level was observed (risk ratio =0.92). The study indicated that monitoring DSA level might predict alteration of immune reactivity and may help determine the weaning process from immunosuppressive drugs.Citation13 Another interesting study revealed that the level of neutrophil gelatinase-associated lipocalin (NGAL) in the urine might be a sensitive biomarker reflecting acute renal allograft dysfunction. This biomarker was validated by immunohistochemical analysis.Citation14 NGAL is mainly released by activated neutrophils and can accumulate in the proximal tubule after acute tubular injury.Citation15 As an acute rejection event occurred, NGAL protein expression was significantly increased in the proximal tubules of the living-donor kidney graft. Furthermore, it was observed that the peripheral NGAL level was sensitively augmented.Citation14 Data from porcine renal transplantation support these findings, in that NGAL concentration in perfusate could be utilized to reflect machine-perfused kidney injury and indicated renal graft function after transplantation.Citation15
Since the first micro-ribonucleic acid (microRNA), a small noncoding molecule, was discovered in 1993,Citation16 microRNAs have been widely studied, particularly in the regulation of immune cells including innate and adaptive immune responses.Citation17 An important study by Anglicheau et al on the role of microRNA biomarkers in transplantation exhibited that high expression of microRNA (miR)-142-5p, miR-155, and miR-223 in the peripheral blood mononuclear cells and renal allograft biopsy of living donor transplant recipients were predictive of an acute rejection event.Citation18 Danger et al validated the biomarker miR-142-5p in the peripheral blood mononuclear cells, which can reflect chronic antibody-mediated rejection of renal transplant patients.Citation19
Biomarkers for nonliving donor kidneys
Outcome of nonliving donor transplants is worse than that of living donor transplants.Citation12 Nonliving donor kidneys can cause various postoperative complications, such as delayed graft function (DGF).Citation20 Early graft function is a crucial determinant of long-term kidney transplant outcome;Citation21 therefore, it is of great interest to summarize the various biomarkers after nonliving donor kidney transplantation.
DGF and primary nonfunction (PNF) frequently occur in the first week of graft life, which has a deleterious effect on long-term allograft survival.Citation7,Citation22 They may be caused by multiple factors, such as utilization of DBD,Citation22 donors from cardiac death (DCD),Citation7 or there may be a weight difference between the donor and recipient, resulting in acute tubular necrosis, post-transplantation oliguria, and even an increased risk of acute rejection episodes.Citation23 Indeed, post-transplantation renal allograft function of DCD recipients is comparable to that of DBD patients, although their influential mechanisms are different.Citation22,Citation24 Therefore, early identification of DGF and PNF is of great value and interest for clinicians and researchers, which will benefit prognostic stratification of renal transplant patients and eventually improve transplant outcome.Citation9 An intriguing question is whether the same biomarkers can be identified and used to monitor allograft function.
Brain death remains a clinical challenge to be overcome in the field of transplantation, causing hormonal alteration, neuroimmunologic effects, and hemodynamic instability. Consequently, a cascade of inflammatory events is unleashed, leading to exacerbation of ischemia/reperfusion injury and an impaired graft survival.Citation25 To identify biomarkers for DBD transplant recipients, a study was performed by Welberry Smith et al.Citation9 Their findings revealed that serum aminoacylase-1 (ACY-1) levels at day 1 or 3 post-transplant were significantly associated with delayed, slow, and immediate graft function, particularly dialysis-free survival, by using proteomic analysis of long-term follow-up of 54 renal transplant patients.Citation9 Furthermore, an independent confirmative cohort study was employed among 194 patients to validate the association between serum ACY-1 level and incidence of DGF.Citation9 Indeed, ACY-1 can be expressed in the pan-tubule and predominantly proximal tubule of pig and human kidneys.Citation9 It is reasonable to explain that DGF causes tubular damage and a significant increase of serum ACY-1 level.Citation9
Donor from cardiac death can also result in DGF and even PNF. A very recent attempt was made to identify accurate early biomarkers from perfusate to predict the occurrence of DGF and PNF.Citation7 The establishment of a biomarker prior to implantation would provide a possibility to prevent the process of graft injury. It was found that lactate dehydrogenase and interleukin-18 concentrations in the preservation solution of machine-perfused kidneys were associated with PNF and DGF, but there was no significant association with 1-year graft survival.Citation7 Therefore, more studies are required to investigate biomarkers for DCD-related graft dysfunction.
With respect to a single factor of deceased-donor graft, three critical genes (CXCR4, CCL5, and ITGB2) were identified from 112 specimens by using microarray profiling examination. Based on a random forest analysis, these were suggested to be suitable biomarkers to assess organ quality and predict kidney graft function.Citation8 Nevertheless, further prospective studies are absent.
Combined use of biomarkers
Indeed, implementation of more biomarkers can significantly improve predictive value. Based on our own studies, Foxp3 gene expression in the peripheral blood might be dramatically increased at early stage post-transplantation, after an acute rejection episode has occurred. However, this increased level was insufficiently differentiated from that of chronically rejecting recipients, which hampered its application as a suitable biomarker. Interestingly, the ratio of Foxp3/alpha-1,2-manosidase might monitor allograft function and predict long-term transplant outcomeCitation26,Citation27 but alpha-1,2-manosidase alone does not (Weihua Gong, unpublished data, 2008). Therefore, combined use of biomarkers is necessary and will enable identification of patients suitable for preemptive treatment, particularly for those at risk of rejection, overdose of immunosuppression, and nephrotoxicity.
Future directions
As experimental transplant models are improving, a considerable number of potential biomarkers are being identified,Citation15,Citation28 including more biomarkers for living or nonliving donors. Suitable biomarkers available for both patient populations are required. It is well-accepted that the great advances in translational medicine can potentiate validation of these identified biomarkers from bench to bed in a transplant center. Nevertheless, international standardization of biomarkers is still required to test their predictive power through prospective multicenter studies,Citation29,Citation30 and their reliability and reproducibility will be accordingly validated.Citation2
The sensitivity and specificity of these biomarkers for monitoring allograft function is an important issue, particularly in the settings of various confounders.Citation1 Combined use of biomarker patterns might provide reliable and significant indication on allograft function, which might shed light on the appropriate preemptive therapeutic strategies.Citation1 Furthermore, systematic analysis using bioinformatics tools can be utilized to avoid repetitive scientific research. Taken together, our goal is to achieve long-term allograft survival using personalized biomarkers.
Acknowledgments
This work was supported by the Department of Education of Zhejiang Province (Grant No Y201226017), the National Natural Science Foundation of China (No 81270323), the Qianjiang Talents Project of Zhejiang Province (Grant No 2012R10022), the Young Eagles Program of the First Affiliated Hospital of Zhejiang Chinese Medicine University, and Zhejiang Provincial Outstanding Youth Foundation (Grant No LR13H020001).
Disclosure
The authors report no conflicts of interest in this work.
References
- GongWWhitcherGHTownamchaiNXiaoXGeFBiomarkers for monitoring therapeutic side effects or various supratherapeutic confounders after kidney transplantationTransplant Proc20124451265126922663998
- SawitzkiBPascherABabelNReinkePVolkHDCan we use biomarkers and functional assays to implement personalized therapies in transplantation?Transplantation200987111595160119502949
- Pantschewa-Haschen R, Schulze R, Schneider G, Schabel J. [Urinary enzymes in monitoring kidney transplant patients.]Z Urol Nephrol19807310719724 German [with English abstract]6109413
- LiLKhatriPSigdelTKA peripheral blood diagnostic test for acute rejection in renal transplantationAm J Transplant201212102710271823009139
- BestardOCrespoESteinMCross-validation of IFN-γ Elispot assay for measuring alloreactive memory/effector T cell responses in renal transplant recipientsAm J Transplant20131371880189023763435
- DieterleFPerentesECordierAUrinary clusterin, cystatin C, beta2-microglobulin and total protein as markers to detect drug-induced kidney injuryNat Biotechnol201028546346920458316
- HooglandERde VriesEEChristiaansMHWinkensBSnoeijsMGvan HeurnLWThe value of machine perfusion biomarker concentration in DCD kidney transplantationsTransplantation201395460361023296150
- ScianMJMalufDGArcherKJIdentification of biomarkers to assess organ quality and predict posttransplantation outcomesTransplantation201294885185822992769
- Welberry SmithMPZougmanACairnsDASerum aminoacylase-1 is a novel biomarker with potential prognostic utility for long-term outcome in patients with delayed graft function following renal transplantationKidney Int Epub201365
- WenRWuVDmitrienkoSYuABalshawRKeownPAGenome Canada Biomarkers in Transplantation GroupBiomarkers in transplantation: prospective, blinded measurement of predictive value for the flow cytometry crossmatch after negative antiglobulin crossmatch in kidney transplantationKidney Int20067081474148116941026
- VyasSRobertiILymphocyte ATP immune cell function assay in pediatric renal transplants: is it useful?Transplantation Proc2011431036753678
- MatasAJPayneWDSutherlandDE2,500 living donor kidney transplants: a single-center experienceAnn Surg2001234214916411505060
- HoshinoJKanekuHEverlyMJGreenlandSTerasakiPIUsing donor-specific antibodies to monitor the need for immunosuppressionTransplantation201293111173117822592887
- KoheiJIshidaHKazunariTTsuchiyaKNittaKNeutrophil gelatinase-associated lipocalin is a sensitive biomarker for the early diagnosis of acute rejection after living-donor kidney transplantationInt Urol Nephrol20134541159116723161375
- JochmansIMonbaliuDPirenneJNeutrophil gelatinase-associated lipocalin, a new biomarker candidate in perfusate of machine-perfused kidneys: a porcine pilot experimentTransplant Proc20114393486348922099824
- LeeRCFeinbaumRLAmbrosVThe C elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14Cell19937558438548252621
- LodishHFZhouBLiuGChenCZMicromanagement of the immune system by microRNAsNat Rev Immunol20088212013018204468
- AnglicheauDSharmaVKDingRMicroRNA expression profiles predictive of human renal allograft statusProc Natl Acad Sci U S A2009106135330533519289845
- DangerRPaulCGiralMExpression of miR-142-5p in peripheral blood mononuclear cells from renal transplant patients with chronic antibody-mediated rejectionPloS One201384e6070223577151
- PremasathianNAvihingsanonYIngsathitAPongskulCJittiganontSSumethkulVRisk factors and outcome of delayed graft function after cadaveric kidney transplantation: a report from the Thai Transplant RegistryTransplant Proc201042104017402021168615
- ParekhJBostromAFengSDiabetes mellitus: a risk factor for delayed graft function after deceased donor kidney transplantationAm J Transplant201010229830320055796
- SiedleckiAIrishWBrennanDCDelayed graft function in the kidney transplantAm J Transplant201111112279229621929642
- GongWKlöpfelMReutzel-SelkeAHigh weight differences between donor and recipient affect early kidney graft function – a role for enhanced IL-6 signalingAm J Transplant2009981742175119563340
- WadeiHMHeckmanMGRawalBComparison of kidney function between donation after cardiac death and donation after brain death kidney transplantationTransplantation201396327428123778649
- FloerchingerBOberhuberRTulliusSGEffects of brain death on organ quality and transplant outcomeTransplant Rev (Orlando)2012262545922459036
- SawitzkiBReinkePVolkHDWoodKTurkaLAAutoimmunity and transplantation: a meeting at the crossroads in BerlinNat Immunol20089544744918425094
- SawitzkiBBushellAStegerUIdentification of gene markers for the prediction of allograft rejection or permanent acceptanceAm J Transplant2007751091110217456197
- ThuillierRCodasRMarchandEChronic renoprotective effect of pulsatile perfusion machine RM3 and IGL-1 solution in a preclinical kidney transplantation modelJ Transl Med20121023323171422
- BrouardSAshton-ChessJSoulillouJPSurrogate markers for the prediction of long-term outcome in transplantation: Nantes Actualité Transplantation (NAT) 2007 meeting reportHum Immunol20086912818295669
- ParikhCREdelsteinCLDevarajanPCantleyLBiomarkers of acute kidney injury: early diagnosis, pathogenesis, and recoveryJ Investig Med2007557333340