Abstract
Background
Despite the increasing magnitude and impact, there are limited data available on the clinical management and in-hospital outcomes of patients who have diabetes mellitus (DM) and chronic kidney disease (CKD) at the time of hospitalization for acute myocardial infarction (AMI). The objectives of our population-based observational study in residents of central Massachusetts were to describe decade-long trends (1999–2009) in the characteristics, in-hospital management, and hospital outcomes of AMI patients with and without these comorbidities.
Methods
We reviewed the medical records of 6,018 persons who were hospitalized for AMI on a biennial basis between 1999 and 2009 at all eleven medical centers in central Massachusetts. Our sample consisted of the following four groups: DM with CKD (n=587), CKD without DM (n=524), DM without CKD (n=1,442), and non-DM/non-CKD (n=3,465).
Results
Diabetic patients with CKD were more likely to have a higher prevalence of previously diagnosed comorbidities, to have developed heart failure acutely, and to have a longer hospital stay compared with non-DM/non-CKD patients. Between 1999 and 2009, there were marked increases in the prescribing of beta-blockers, statins, and aspirin for patients with CKD and DM as compared to those without these comorbidities. In-hospital death rates remained unchanged in patients with DM and CKD, while they declined markedly in patients with CKD without DM (20.2% dying in 1999; 11.3% dying in 2009).
Conclusion
Despite increases in the prescribing of effective cardiac medications, AMI patients with DM and CKD continue to experience high in-hospital death rates.
Introduction
Diabetes mellitus (DM) is a major public health concern. The prevalence of DM in the US has more than doubled over the past decade, and DM is a major risk factor for cardiovascular disease.Citation1 In addition to being at increased risk of developing coronary heart disease, patients with diabetes experience higher hospital mortality rates after acute myocardial infarction (AMI) than patients without diabetes.Citation2–Citation5 Chronic kidney disease (CKD) is also a relatively common condition in the general population with more than 26 million American adults estimated to have CKD;Citation6,Citation7 this condition is also associated with considerable morbidity and mortality. A recent European report using data from a large cardiac registry found that more than one third of patients with CKD have concomitant DM,Citation8 increasing the difficulty of managing patients with these serious comorbidities. Diagnostic and treatment challenges in these high-risk patients presenting with an AMI are further complicated by their more advanced presentation, treatment delays, and medication side effects.Citation9 Although several studies have described trends in the medical management and clinical outcomes of patients hospitalized with AMI who have either preexisting DM or CKD,Citation2,Citation3,Citation5,Citation9,Citation10 there are extremely limited contemporary data available about the characteristics, clinical management, and in-hospital outcomes of patients who present with either or both of these chronic conditions at the time of hospitalization for AMI, especially from the more generalizable perspective of a population-based investigation.
The objectives of this population-based study were to describe overall differences, and decade-long trends (1999–2009), in the characteristics, in-hospital management, clinical complications, and in-hospital death rates of patients with preexisting DM and CKD, as compared with nondiabetic/non-CKD patients, hospitalized with AMI in all medical centers throughout central Massachusetts.
Methods
Data from the Worcester Heart Attack Study were used for this investigation.Citation11–Citation13 This is an ongoing population-based investigation describing long-term trends in the epidemiology of AMI among residents of the Worcester, MA, metropolitan area (2000 census =478,000) hospitalized with AMI at all medical centers in central Massachusetts.Citation11–Citation13 In brief, the medical records of residents of this metropolitan area admitted to all eleven hospitals in central Massachusetts with a discharge diagnosis of AMI and related coronary disease rubrics during the years under study were individually reviewed and validated according to preestablished criteria.Citation11 In brief, the diagnosis of AMI was made on the basis of criteria developed by the World Health Organization and that have been consistently utilized in the Worcester Heart Attack Study since its inception. This well-accepted schema uses a supportive clinical history, serum enzyme/biomarker elevations, and serial electrocardiogram changes.Citation11–Citation13 All doubtful or “probable” cases of AMI, CKD, DM, or other comorbidities were reviewed by the principal investigator in conjunction with the project director and then by the study’s senior cardiologists for final case classification.Citation11–Citation13 Doubtful or questionable diagnoses were defined as those in which there is uncertainty or lack of adequate information available to classify the patient as having had an AMI.Citation11–Citation13 The present study sample consisted of greater Worcester residents hospitalized with AMI on a biennial basis between 1999 and 2009.
We classified patients as having a history of either DM or CKD, or the absence thereof, based on the review of data available in hospital medical records.Citation3,Citation14 Due to the data collection efforts of this observational study, and missing data on several laboratory values, we classified patients as having DM and/or CKD based only on information collected and routinely recorded in hospital medical records and not on either serum glucose or creatinine findings during their index hospitalization. This study was approved by the institutional review board at the University of Massachusetts Medical School.
Data collection
Trained nurses and physicians abstracted demographic and clinical data from the medical records of greater Worcester residents hospitalized with confirmed AMI. Abstracted information included patient’s age, sex, medical history, AMI order (initial vs prior), physiologic factors, laboratory test results, length of hospital stay, time interval between patient-reported acute symptom onset and emergency department arrival, and hospital discharge status.Citation11,Citation15 Information about the use of important cardiac medications, coronary angiography, percutaneous coronary intervention (PCI), and coronary artery bypass (CABG) surgery during the patient’s index hospitalization was collected. Development of several significant clinical complications (eg, atrial fibrillation, cardiogenic shock, stroke, heart failure) during the patient’s hospitalization was defined according to standard criteria.Citation11,Citation13,Citation16,Citation17
Data analysis
Differences in the characteristics of patients with DM and/or CKD, as compared with nondiabetic and/or non-CKD patients, were examined through the use of chi-square tests for discrete variables and analysis of variance for continuous variables; these analytic tests were also used to examine potentially changing trends in various patient demographic and clinical factors during the years under study. In-hospital case-fatality rates, and proportion of patients developing various in-hospital clinical complications, in our four comparison groups, as well as decade-long trends in these endpoints, were calculated by the number of deaths, or clinical complications, that occurred during the index hospitalization divided by the number of patients admitted to a hospital with confirmed AMI during the specific period examined. Decade-long trends in the prescribing of several cardiac medications and coronary reperfusion/revascularization interventions were also calculated for the various DM/CKD groups under study through the use of chi-square tests for trend.
We carried out a series of unadjusted and multivariable-adjusted logistic regression analyses for purposes of assessing the overall impact of DM and CKD with regard to the odds of developing atrial fibrillation, heart failure, and cardiogenic shock and dying during the patient’s acute hospitalization while controlling for several potentially confounding demographic, medical history, and clinical factors that have been shown to affect these outcomes. Control variables included indicators for the following: age, sex, history of various coexisting disorders (angina, heart failure, hypertension, or stroke), AMI order (initial vs prior), and study year.
Results
Characteristics of study patients
A total of 6,018 greater Worcester residents were hospitalized with independently confirmed AMI during the years under study (). The average age of these patients was 72.4 years, 55.4% were men, 33.7% were diabetic, and 18.5% had previously diagnosed CKD based on the review of information obtained from hospital medical records. There were marked increases between 1999 and 2009 in the prevalence of CKD (from 11.8% to 23.3%, P<0.001) and DM (from 30.8% to 36.1%, P=0.06); the proportion of patients with both conditions approximately doubled from 6.0% in 1999 to 11.8% in 2009. Our comparative study samples consisted of the following: DM with CKD (n=587), CKD without DM (n=524), DM without CKD (n=1,442), and non-DM/non-CKD (n=3,465).
Table 1 Characteristics of patients hospitalized with AMI by group
Overall, the mean age of diabetic patients with CKD was 73 years; patients with CKD without DM were the oldest, with a mean age of 78 years (). Patients with both comorbidities had a higher average body mass index than nondiabetics and were much more likely to be overweight. Diabetic patients with CKD had a higher prevalence of several important cardiovascular comorbidities and chronic obstructive pulmonary disease as compared with the other three groups ().
In terms of acute presenting symptoms, diabetic patients with and without CKD were less likely to have presented with classic anginal symptoms including chest pain, left arm pain, shoulder pain, or diaphoresis, and were more likely to have complained of dyspnea, than patients without DM. Interestingly, almost 40% of patients with previously diagnosed CKD, with or without DM, failed to report the presence of pain, in the chest or otherwise, at the time of hospital admission for AMI. Overall, persons with DM and CKD experienced similar delays in seeking acute medical care as compared to those without these comorbidities (). Diabetic patients with CKD had a longer average hospital stay than non-DM/non-CKD patients (5.0 days vs 4.0 days). Serum glucose levels at the time of hospital admission were significantly higher in diabetic patients with and without CKD as compared to those without DM and CKD ().
Hospital treatment practices
Overall, the prescribing of in-hospital cardiac medications was relatively similar in all four patient groups (). However, patients with DM and CKD were more likely to have been prescribed calcium channel blockers, diuretics, and statins during their acute hospitalization as compared with other patient groups (). Comparing medication-prescribing practices between 1999 and 2009, there were important increases over time in the use of recommended cardiac medications including angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, beta-blockers, aspirin, and statins in our four study groups (). In patients with CKD and without DM, particularly, marked increases were noted in the prescribing of beta-blockers, statins, and aspirin during the years under study.
Figure 1 Trends in-hospital medical treatments in patients with myocardial infarction and comorbidities.
Abbreviations: ACEi, angiotensin-converting enzyme inhibitors; ARBs, angiotensin receptor blockers; DM, diabetes mellitus; CKD, chronic kidney disease.
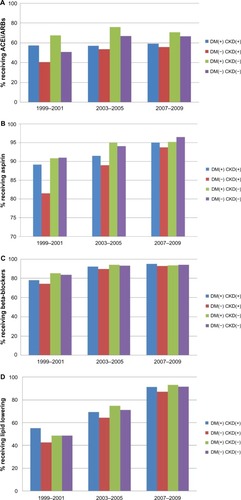
Table 2 Hospital management practices by group
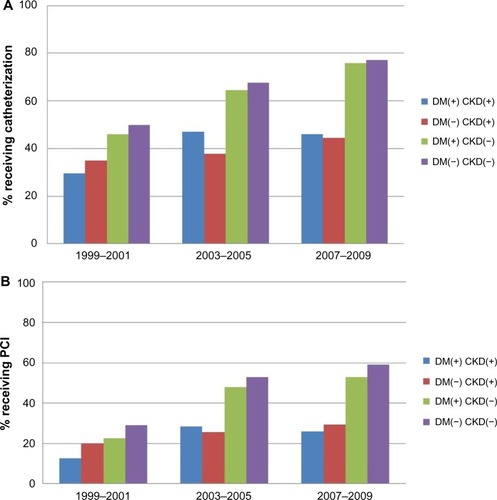
Diabetic patients with CKD were less likely to have undergone a PCI and CABG surgery in comparison to patients without both comorbidities (). While there were marked increases over time in the proportion of hospitalized patients undergoing cardiac catheterization and PCI in each of our four comparison groups, patients without these previously diagnosed comorbidities had a greater increase in the receipt of cardiac catheterization and PCI during the years under study ().
Figure 2 Use of coronary interventions in patients with acute myocardial infarction according to comorbidities.
Abbreviations: PCI, percutaneous coronary intervention; DM, diabetes mellitus; CKD, chronic kidney disease.
In-hospital clinical complications and hospital death rates
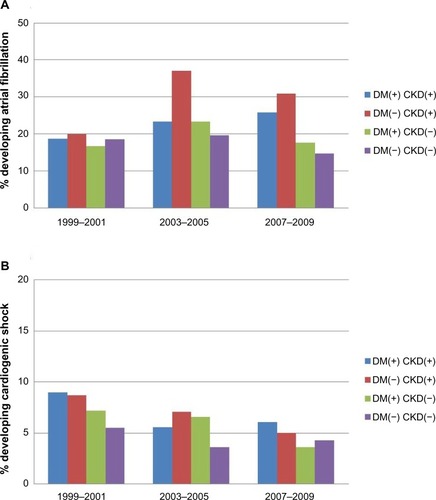
Overall, diabetic patients with CKD were more likely to have developed heart failure during their acute hospitalization as compared to the other diseased groups. Nondiabetic patients with CKD were more likely to have developed other important in-hospital complications, including atrial fibrillation, and to have died during hospitalization for AMI ().
Table 3 In-hospital clinical complications by group
To more systematically examine the odds of developing selected in-hospital complications, we carried out a series of multivariable-adjusted regression analyses controlling for several potentially confounding factors of prognostic importance (). The results of these analyses were consistent with our univariate findings showing that diabetic patients with CKD were more likely to have developed heart failure as compared to those without these comorbidities. Patients with DM and without a history of CKD were at greatest odds for developing cardiogenic shock, whereas patients with CKD and without DM had a markedly higher risk of developing atrial fibrillation and dying during hospitalization.
There were important trends in the likelihood of developing each of these clinical complications during the years under study (). Patients with CKD with or without DM experienced a significant increase in the odds of developing atrial fibrillation between 1999 and 2009 (from 18.8% to 25.8% for those with DM and from 20.0% to 30.9% for those without DM). Diabetic patients without CKD had a slight increase in the odds of developing heart failure over time, whereas patients with CKD without DM had a significant decline in the likelihood of developing heart failure during the years under study ().
Figure 3 In-hospital clinical complications according to comorbidities.
Abbreviations: DM, diabetes mellitus; CKD, chronic kidney disease.
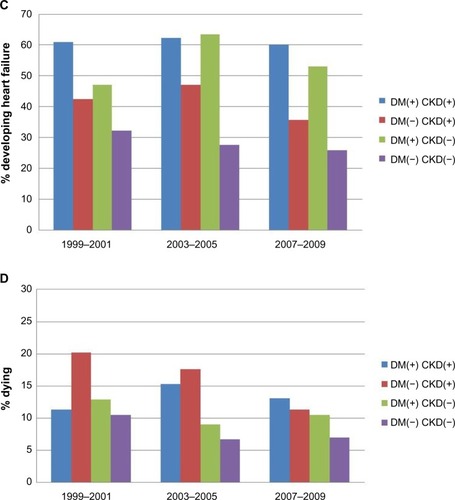
Overall, diabetic patients with CKD experienced significantly lower in-hospital death rates as compared to those with CKD without previously diagnosed DM, who had the highest in-hospital death rates (). The risk of dying during hospitalization decreased in each of our study groups during the decade-long period under study with the exception of those who had both comorbidities previously diagnosed (11.3% dying in 1999; 13.1% in 2009). Nondiabetic patients with CKD experienced the greatest decline in the risk of dying between 1999 (20.2%) and 2009 (11.3%) ().
We calculated the overall multivariable-adjusted odds of dying for the different groups of patients as compared to those without DM and CKD, first calculating unadjusted odds ratios (ORs) and then adjusting for several confounding factors of prognostic importance and year of the index hospitalization (). After multivariable adjustment, only the ORs for patients with CKD without DM were statistically significant (OR =1.31; 9 5% confidence interval 1.01, 1.70) as compared to those without these comorbidities. Patients with CKD and DM had a slightly higher multivariable-adjusted risk of dying as compared to those without these comorbidities.
Discussion
The principal finding of this large population-based study of residents of central Massachusetts who were hospitalized at all area medical centers with AMI was that, despite marked increases in the use of medical and invasive treatments during the years under study, and general declines in hospital mortality over time, patients with CKD with or without DM remained at increased risk of developing important inhospital complications and dying as compared to patients without either of these important comorbidities.
Our findings are consistent with those of prior studies that have shown that diabetic patients with CKD hospitalized with AMI are older, more likely to present with a prior myocardial infarction, and overweight, and have a variety of additional cardiovascular comorbidities present than patients without DM and CKD. Similarly, in a large study that analyzed data from more than one million Medicare beneficiaries between 1998 and 2001, CKD patients with and without DM were older than diabetic patients and those without these comorbidities. This study also found that patients with DM and CKD presented with the highest prevalence of other important comorbidities.Citation7,Citation18
Our results support previous studies that have shown that diabetic patients with CKD hospitalized with AMI were less likely to report classic angina symptoms but were more likely to complain of dyspnea and palpitations, and experienced longer stays in the hospital than patients without these comorbidities.Citation19,Citation20 Differences in acute symptom presentation, and possible reasons that could explain the different symptom patterns in diabetic patients with CKD compared to those without these comorbidities, need to be explored further to enhance the more rapid diagnosis and treatment of these high-risk patients.
We found that diabetic patients with CKD were more likely to have been prescribed beta-blockers, calcium channel blockers, digoxin, diuretics, and statins during their acute hospitalization for AMI than the other comparison groups. Somewhat different prescribing patterns were observed in the SYMPHONY (Sibrafiban versus aspirin to Yield Maximum Protection from ischemic Heart events post-acute cOroNary sYndromes) study, a large international investigation that collected data from more than 16,000 patients hospitalized with AMI in 37 countries between 1997 and 1999. In this study, aspirin, beta-blockers, and statins were less frequently prescribed to patients with CKD during hospitalization and over a 9 0-day follow-up period compared to patients without CKD.Citation21 Unfortunately, information on the diabetic status of study participants was not reported. Similarly, 1,683 patients with AMI who were hospitalized at a single large hospital in Israel were classified into three categories of CKD: normal, moderate, and severe. Compared to patients with normal renal function, standard therapy for AMI was underutilized in patients with moderate and severe CKD; these individuals were also more likely to have developed several in-hospital clinical complications including heart failure and atrial fibrillation.Citation22 Information about patients with diabetes was not reported for participants in this study, and we were unable to find other published articles to compare our findings with.
The prescribing of recommended in-hospital cardiac medications increased significantly during the years under study in all four patient groups. Notably, diabetic patients with CKD experienced a greater increase in the prescribing of beta-blockers, statins, and aspirin than all other patient groups. Unfortunately, there is very little literature to compare our findings to. Much of the current literature has focused on AMI patients with either DM or CKD but not on patients with both comorbidities. The majority of the studies that have, however, evaluated the use of beneficial cardiac medications in AMI patients with either DM or CKD have reported an underuse of effective cardiac medications in patients with either of these comorbidities compared to patients without either CKD or DM.Citation22,Citation23
In the present study, the utilization of PCI and cardiac catheterization increased to a greater extent during the decade-long period under investigation in diabetic patients with CKD than in patients without either of these comorbidities; on the other hand, less than half of these patients received these cardiac interventions. One potential explanation for this relatively low percentage is likely due to the high prevalence of additional comorbidities in patients with CKD with and without DM, which may make clinicians more reluctant to treat these complex, high-risk patients. In a recent study using data from several national Danish registries, more than 3,100 patients with and without CKD, and with and without DM, were hospitalized with an initial AMI between 2000 and 2009.Citation24 There was an increase over time in the use of coronary angiography in patients with and without CKD and a relatively similar increase in the use of PCI in patients with and without CKD during the period under study. Unfortunately, information from patients with various combinations of these comorbidities was not presented.
Our findings suggest that diabetic patients with CKD were more likely to have developed heart failure, whereas patients presenting with CKD and without DM experienced the highest rates of atrial fibrillation, cardiogenic shock, and stroke. Our findings are consistent with those of a large study based on a sample of Medicare beneficiaries with different cardiovascular diseases who were enrolled and followed between 1998 and 2001. Diabetic patients with CKD had the highest risk of experiencing heart failure and reinfarction during the 2-year follow-up period in comparison to those without CKD.Citation7
Similarly, as reported in several studies,Citation25–Citation29 patients presenting with CKD and without DM at the time of hospitalization for AMI experienced higher in-hospital death rates than other comparison groups in the present study. In a recent meta-analysis, data from more than one million patients with CKD (120,000 had DM) from the Chronic Kidney Disease Prognosis Consortium between 2011 and 2012 were analyzed. Cardiovascular and all-cause mortality were significantly higher in patients with CKD, irrespective of whether or not they had DM, underscoring the importance of identifying and treating risk factors for cardiovascular disease in patients with CKD.Citation10 In the Cooperative Cardiovascular Project, the 1-month death rate after AMI was 44% among elderly patients who had moderate renal insufficiency compared with 13% in elderly patients who had normal kidney function. Unfortunately, this study did not provide information on the diabetes status of this population.Citation25
Patients with DM and CKD in the present study were at the highest risk of dying during hospitalization during the most recent years under study. Similarly, in a large population-based cohort study in Alberta, Canada, more than 10,000 patients with and without CKD and DM were admitted to the hospital with AMI between 2 002 and 2 009. Overall short-term mortality (within 30 days from admission to the hospital) was markedly higher in patients with CKD and DM as compared to those without each of these comorbidities.Citation30 These data reinforce the significant impact of CKD on short-term prognosis after AMI and the need for heightened surveillance and targeted use of effective treatment regimens in these high-risk patients.
The strengths of the present study include our population-based design that included all patients hospitalized with AMI from a large central New England metropolitan area, multiple years under study, and the independent validation of each possible case of AMI. Study limitations include the inability to more systematically measure, and thereby control for, other clinical factors (eg, severity of disease, CKD stage, other physiological variables, or comorbidities) that may have affected or mediated the observed relationships between CKD and DM in patients hospitalized with AMI. Neither the etiology nor the duration of DM and/or CKD, and its relationship with other outcomes after hospitalization for AMI, could be evaluated from the available data. We also did not collect more detailed data on the therapeutic management of hospitalized patients, including dosage and frequency of selected medications.
Conclusion
The results of this large community-wide study suggest that although CKD and DM continue to negatively impact short-term prognosis after AMI, increased adoption of effective medical treatment regimens and coronary reperfusion/revascularization approaches in these high-risk patients has occurred over time with positive results. That being said, there remains room for improvement in the medical management of these high-risk patients. Furthermore, it remains important to heighten awareness among health care providers about the magnitude of, associations between, and impact of these two important and comorbid conditions in relation to prognosis after AMI.
Authors’ contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (grant number R01 HL35434). Partial salary support for Drs Goldberg and McManus was provided by the National Institutes of Health grant 1U01HL105268-01. Dr Tisminetzky was funded by Diversity Supplement National Institutes of Health grant R01 HL35434-29. Partial salary support was additionally provided to Dr McManus by National Institutes of Health grant KL2RR031981.
Disclosure
There are no conflicts of interest to report for any of the authors.
References
- GoreMOPatelMJKosiborodMNational Registry of Myocardial Infarction InvestigatorsDiabetes mellitus and trends in hospital survival after myocardial infarction, 1994 to 2006: data from the national registry of myocardial infarctionCirc Cardiovasc Qual Outcomes2012579179723132330
- BergerAKBreallJAGershBJEffect of diabetes mellitus and insulin use on survival after acute myocardial infarction in the elderly (The Cooperative Cardiovascular Project)Am J Cardiol20018727227711165959
- CrowleyAMenonVLessardDSex differences in survival after acute myocardial infarction in patients with diabetes mellitus (Worcester Heart Attack Study)Am Heart J200314682483114597931
- MurciaAMHennekensCHLamasGAImpact of diabetes on mortality in patients with myocardial infarction and left ventricular dysfunctionArch Intern Med20041642273227915534166
- AbbudZAShindlerDMWilsonACKostisJBEffect of diabetes mellitus on short- and long-term mortality rates of patients with acute myocardial infarction: a statewide study. Myocardial Infarction Data Acquisition System Study GroupAm Heart J199513051587611123
- LeveyASCoreshJBalkENational Kidney FoundationNational Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratificationAnn Intern Med200313913714712859163
- FoleyRNMurrayAMLiSChronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999J Am Soc Nephrol20051648949515590763
- VöllerHGittAJannowitzCTreatment patterns, risk factor control and functional capacity in patients with cardiovascular and chronic kidney disease in the cardiac rehabilitation settingEur J Prev Cardiol2014211125113323508927
- BaberUAugusteUPatients with chronic kidney disease/diabetes mellitus: the high-risk profile in acute coronary syndromeCurr Cardiol Rep20131538639523843182
- FoxCSMatsushitaKWoodwardMChronic Kidney Disease Prognosis ConsortiumAssociations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysisLancet20123801662167323013602
- FloydKCYarzebskiJSpencerFAA 30 year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack StudyCirc Cardiovasc Qual Outcomes20092889520031820
- GoldbergRJSpencerFAYarzebskiJA 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study)Am J Cardiol2004941373137815566906
- GoldbergRJGoreJMAlpertJSDalenJERecent changes in attack and survival rates of acute myocardial infarction (1975 through 1981)The Worcester Heart Attack StudyJAMA1986255277427793701991
- GoldbergRJKramerDGLessardDYarzebskiJGoreJMSerum glucose levels and hospital outcomes in patients with acute myocardial infarction without prior diabetes: a community-wide perspectiveCoron Artery Dis20071812513117301604
- GoldbergRJYarzebskiJLessardDGoreJMDecade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack studyArch Intern Med20001603217322311088081
- SaczynskiJSMcManusDZhouZTrends in atrial fibrillation complicating acute myocardial infarctionAm J Cardiol200910416917419576341
- McManusDDChinaliMSaczynskiJSThirty-year trends in heart failure in patients hospitalized with acute myocardial infarctionAm J Cardiol201110735335921256998
- StefanMSBannuruRRLessardDGoreJMLindenauerPKGoldbergRJThe impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction: a 10-year retrospective observational studyChest20121411441144822207679
- SosnovJLessardDGoldbergRJYarzebskiJGoreJMDifferential symptoms of acute myocardial infarction in patients with kidney disease: a community-wide perspectiveAm J Kidney Dis20064737838416490615
- KentschMRodemerkUGittAKAngina intensity is not different in diabetic and non-diabetic patients with acute myocardial infarctionZ Kardiol20039281782414579045
- ReddanDNSzczechLBhapkarMVRenal function, concomitant medication use and outcomes following acute coronary syndromesNephrol Dial Transplant2005202105211216030030
- TessoneAGottliebSBarbashIMUnderuse of standard care and outcome of patients with acute myocardial infarction and chronic renal insufficiencyCardiology200710819319917095865
- SantolucitoPATigheDAMcManusDDManagement and outcomes of renal disease and acute myocardial infarctionAm J Med201012384785520800154
- BlicherTMHommelKOlesenJBTorp-PedersenCMadsenMKamperALLess use of standard guideline-based treatment of myocardial infarction in patients with chronic kidney disease: a Danish nation-wide cohort studyEur Heart J2013342916292323798578
- ShlipakMGHeidenreichPANoguchiHChertowGMBrownerWSMcClellanMBAssociation of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patientsAnn Intern Med200213755556212353942
- BeattieJNSomanSSSandbergKRDeterminants of mortality after myocardial infarction in patients with advanced renal dysfunctionAm J Kidney Dis2001371191120011382688
- NautaSTvan DomburgRTNuisRJAkkerhuisMDeckersJWDecline in 2 0-year mortality after myocardial infarction in patients with chronic kidney disease: evolution from the prethrombolysis to the percutaneous coronary intervention eraKidney Int20138435335823486524
- FoxCSMuntnerPChenAYAcute Coronary Treatment and Intervention Outcomes Network registryUse of evidence-based therapies in short-term outcomes of ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction in patients with chronic kidney disease: a report from the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network registryCirculation201012135736520065168
- SzummerKLundmanPJacobsonSHSWEDEHEARTInfluence of renal function on the effects of early revascularization in non-ST-elevation myocardial infarction: data from the Swedish web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART)Circulation200912085185819704097
- TonelliMMuntnerPLloydAAlberta Kidney Disease NetworkRisk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort studyLancet201238080781422717317
