Abstract
Background
Combined uterine and urinary bladder rupture following prolonged obstructed labor is indeed a momentous uro-obstetric emergency. The urinary bladder involvement is distinctly rare in the absence of factors that predispose the bladder to be adherent to the lower uterine segment and is quite unusual in a primigravida.
Objective
To report a rare case of uterine rupture involving urinary bladder secondary to a prolonged obstructed labor in a primigravida from a low resource setting.
Case
A 17-year-old married unbooked primigravida who presented with a 3-day history of spontaneous onset of labor at term that was initially managed at home and later in a primary health care center where she had fundal pressure and oxytocin augmentation, respectively. The labor was complicated by combined uterine and urinary bladder rupture with sepsis. She was resuscitated and had exploratory laparotomy with uterine and urinary bladder repair. The postoperative period was uneventful and she was followed-up at the gynecology and family planning clinics.
Conclusion
There is a need for community reawakening on the inherent risks of teenage pregnancy, bad obstetric practices, and unsupervised pregnancy, labor, and delivery, particularly in the rural settings as in the index patient. A high index of suspicion and prompt appropriate intervention will reduce the sequel of morbidity and occasional mortality from this predicament.
Introduction
Uterine rupture involving the urinary bladder in labor and delivery is a momentous uro-obstetric emergency that results in stillbirth, maternal morbidity, and occasional maternal fatality.Citation1 Uterine rupture is unusual in the primigravida. In the few isolated recorded cases of uterine rupture from prolonged obstructed labor in the primigravida, bladder rupture is distinctly rare.Citation2,Citation3 We obtained a written informed consent from the patient to report this unusual intricacy of labor and delivery.
Case report
The patient was a 17-year-old unbooked primigravida who was uncertain of her date but was said to be 9 months pregnant at the time of her presentation to the Médecins Sans Frontières France (MSF-F) Emergency Obstetrics, Neonatal, and Vesico-Vaginal Fistula (VVF) Care Center in Jahun, Jigawa State, Northern Nigeria. She presented as a referral from a primary health care center (PHCC) approximately 100 km from Jahun town. We obtained approval from the Jigawa State Ministry of Health Ethics Committee to report these unusual complications of labor in a primigravida.
She was apparently well when she went into spontaneous labor 3 days prior to the presentation. The labor was under the supervision of a traditional birth attendant at home for 2 days. She had oral traditional medicaments, fundal pressure, and later a “gishiri cut” (traditional genital mutilation) while at home. On the second day, the labor pain became relentless with the involvement of the whole abdomen that necessitated her presentation to a close-by PHCC. She had oxytocin augmentation with 10 IU given as intramuscular injection and 20 IU via an intravenous fluid at the PHCC; nonetheless, her condition deteriorated with associated high-grade fever, inability to void urine, vomiting, vaginal bleeding, chest pain, and difficulty in breathing before her referral to MSF-F a day after her presentation to the PHCC.
She attained menarche at the age of 15 and had a regular menstrual pattern. She had no known comorbidity, no antecedent abdominopelvic surgery, no abdominal trauma, no history signifying previous pelvic inflammatory disease, and no history suggestive of urinary tract pathology. She was married to a 22-year-old petty trader, had no formal education, nor was she gainfully employed.
At presentation, she was acutely ill-looking, febrile (axillary temperature 39°C), dehydrated, pale but anicteric. She had a height of 1.51m. Her pulse rate was 130 per minute, regular with moderate volume; her blood pressure was 100/70 mmHg, and the heart sounds were I and II only. Her respiratory rate was 36 cycles per minute but lung fields were clinically clear. The abdomen was grossly distended with Bandl’s ring and symphysio-fundal height of 41 cm. There was generalized tenderness with crepitus and guarding over the anterior abdominal wall. Fetal parts were freely felt; singleton fetus, longitudinal lie, and cephalic presentation with a descent of 3/5th. Fetal heart sounds were absent. Pelvic examination revealed a foul smelling, blood stained vulva, and vagina. There was a glaring gishiri cut. The cervix was edematous but fully dilated with offensive watery discharge. There was marked carput formation and pelvic assessment affirmed an inadequate pelvis. An indwelling urethral catheter we passed drained scanty bloody urine. A diagnosis of a ruptured uterus with urinary bladder involvement secondary to prolonged obstructed labor and sepsis in a primigravida was made.
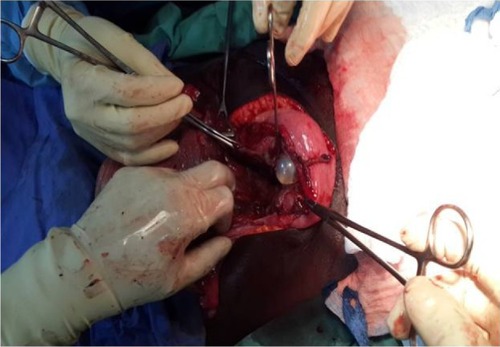
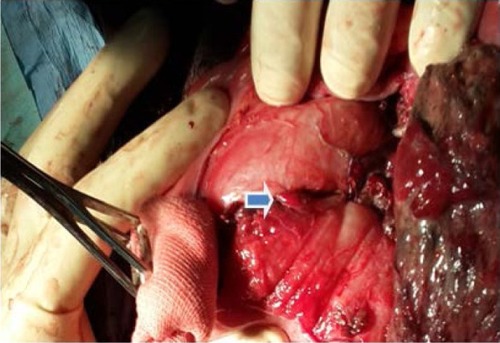
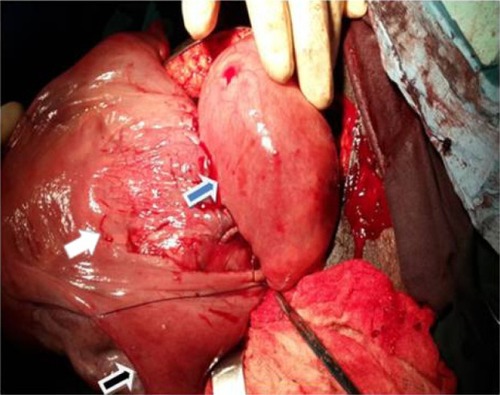
She was resuscitated with intravenous normal saline, intravenous antibiotic, and analgesics. Her full blood count result showed leukocytosis with a packed cell volume of 26%. She had normal electrolyte but elevated urea and creatinine levels that normalized following her resuscitation. The HIV and hepatitis B surface antigen tests were negative and the random blood glucose with liver function test were normal. She was prepared for exploratory laparotomy. The findings at the surgery included thick foul smelling liquor and a fresh stillborn male baby weighing 3.85 kg. There was a ragged lower uterine segment rupture that extended down to the uterine cervix with posterior urinary bladder rupture measuring 8 cm and the urethral catheter balloon visible outside the bladder (). Other pelvic and abdominal organs were normal. She had uterine and urinary bladder repair in double layers ( and ). Abdomen was lavaged with normal saline, cleaned, and wall sutured in layers. The estimated blood loss was 450 mL and she had two units of whole blood transfused. A nasogastric tube was passed and left in situ for 24 hours. She had sitz bath for the genital mutilation and was discharged home on the 12th day postoperation on hematinics after the removal of the urinary catheter. Her overall postoperative recovery period was uneventful. At her consecutive follow-up, the wound had healed completely; she was continent of urine, had no lower urinary tract symptoms, and was thereupon commenced on family planning.
Discussion
In spite of the notable global gains in health care delivery, maternal and child health has prevailed as a great health challenge in the developing countries.Citation4 Many national and international bodies, including governmental, intergovernmental, and nongovernmental bodies,Citation5 have devoted resources aimed at curbing the high maternal morbidity and mortality. MSF-F has been in Nigeria since 1996. In collaboration with Jigawa State Ministry of Health and indigenous specialist health caregivers, MSF-F offers free health care services in Jahun General Hospital at the maternity/VVF section since 2008.Citation6 Their main objectives include bettering the access to obstetric and neonatal care, hence, lowering the maternal and neonatal mortality rates in addition to improving the care for patients with obstetric fistula. Principally, patients from the Northwest region of Nigeria and a part of Niger Republic receive care from the center. The analysis of the services offered by the center in 2013 showed that greater than 70% of the admissions were from complications of pregnancy, labor, and delivery.Citation7
The index patient, a primigravida, presented as a referral from a PHCC approximately 100 km away which might have contributed to the delay in her presentation.Citation8 The patient’s prolonged obstructed labor of 3 days was further complicated by the uterine rupture involving the urinary bladder. Our literature search revealed that the Nigerian former minister of health (1961 to 1966), MA Majekodounmi, was the first known Nigerian author who reported a case of the unscarred uterine rupture with urinary bladder involvement he managed in 1954; but that patient was a multigravida.Citation9
This is the first primigravida with combine uterine and urinary bladder rupture who presented to the MSF-F center in Jahun and among the very few reported. Our quest of PubMed divulged a single case managed in a tertiary maternity hospital, Kathmandu, Nepal, in their 20-year review of 251 patients with a ruptured uterus.Citation2 The urinary bladder involvement in uterine rupture is distinctly rare in the absence of adhesions of the urinary bladder to the lower uterine segment; hence, rare in the unscarred uterusCitation9 and distinctly unusual in a primigravida. Supplementary to her delay in presentation, the index case displayed much of the harmful time-honored practices still a tradition in some of the rural settings in Nigeria. The harmful traditions included concoctions ingested during labor and delivery under the supervision of the traditional birth attendantsCitation10–Citation12; this contributed to the index patient presenting clinical state. Pan et al reported uterine rupture in an unscarred uterus after application of fundal pressure;Citation13 the index patient had fundal pressure while at home. Urine retention during labor is not unusual; trivial trauma or significant pressure could lead to rupture of the distended bladder in an unsupervised labor and delivery in addition to it hindering the progression of labor, as may probably be the case in our patient. Abdominal massage-related urinary bladder rupture and spontaneous rupture though rare have been reported in a distended bladder.Citation14,Citation15 Hence, the fundal pressure in a distended bladder could have contributed to the urinary bladder involvement as these traditional birth attendants do not have the expertise of draining the distended urinary bladder. The patient had oxytocin at the primary health care facility; these centers often have little or no experience of safe augmentation using oxytocin. Oxytocin-associated rupture of an unscarred uterus in a primigravida was recognized in the literature.Citation16 Our patient had a total of 30 IU of oxytocin both by intramuscular injection (an erroneous dose and route of administration) and intravenous infusion at the PHCC. The teenage pregnancy that was unbooked, the formal education she lacked, and her poor economic status are established factors that contributed to poor health-seeking behavior and a bad obstetric history along with an unfavorable outcome in our patient.
The clinical features in the patient were classical of uterine rupture with urinary bladder involvement.Citation1,Citation2,Citation9 She was therefore appropriately managed as a uro-obstetric emergency by prompt resuscitation, evaluation, and laparotomy.Citation1 At the laparotomy, the diagnosis was confirmed; cystoscopy was not done because the center does not have the facility and time was a big issue for her survival and the outcome. The stillborn is a common aftermath in uterine rupture. The patient, fortunately, had uneventful recovery before her discharge and at consecutive follow-ups. The follow-up in the patient will be all through her reproductive age. She was additionally counseled that her ensuing pregnancy and labor must be medically supervised and delivery should only be in a center with facility and expertise to handle high-risk deliveries.
Conclusion
Uterine rupture is not common among primigravidas and urinary bladder involvement is particularly unusual; hence, a high index of suspicion helps in the management. Prompt and appropriate intervention reduces the sequel of morbidities and occasional mortality. There is a need for continuous community reawakening on the inherent imperils of teenage pregnancy, harmful traditional obstetric practices, and those of unsupervised pregnancy, labor and delivery. Stiff legislation may enhance compliance.
Disclosure
The authors report no conflicts of interest in this work.
References
- ChamberlainGSteerPABC of labour care: obstetric emergenciesBMJ199931871941342134510323825
- PadhyeSMRupture uterus in primigravida: morbidity and mortalityKathmandu Univ Med J (KUMJ)2007549249618604081
- HofmeyrGJSayLGulmezogluAMWHO systematic review of maternal mortality and morbidity: the prevalence of uterine ruptureBJOG20051121221122816101600
- World Health OrganizationMaternal mortality in 1990–2015WHO, UNICEF, UNFPA, World Bank Group, and United Nations Population Division Maternal Mortality Estimation Inter-Agency Group Available from: www.who.int/gho/maternal_health/countries/nga.pdf?ua=1Accessed December 27, 2015
- United Nations International Children’s Emergency FundMaternal and child health Available from: http://www.unicef.org/nigeria/children_1926.htmlAccessed December 27, 2015
- Médecins Sans Frontières (MSF)International Activity Report 2014 Available from: http://www.msf.org/sites/msf.org/files/msf_international_activity_report_2014_en.pdfAccessed December 27, 2015
- GuerrierGOluyideBKeramarouMGraisRFFactors associated with severe preeclampsia and eclampsia in Jahun, NigeriaInt J Womens Health2013550951323983493
- National Statistics DirectorateTimor-Leste Demographic and Health Survey 2009–2010CalvertonICF Macro2010
- MajekodunmiMARupture of the uterus involving the bladderBr Med J19571501327027113383247
- FakeyeTOAdisaRMusaIEAttitude and use of herbal medicines among pregnant women in NigeriaBMC Complement Altern Med200995320043858
- OlogeMOAboyejiAPIjaiyaMAAdesinaKTAdewaraAAOlarinoyeJKHerbal use among pregnant mothers in Ilorin, Kwara State, NigeriaJ Obstet Gynaecol200828772072119065368
- GharoroEPIgbafeAAPattern of drug use amongst antenatal patients in Benin City, NigeriaMed Sci Monit200061848711208289
- PanHSHuangLWHwangJLLeeCYTsaiYLChengWCUterine rupture in an unscarred uterus after application of fundal pressure. A case reportJ Reprod Med200247121044104612516327
- PalaniappanKAbuAPBladder rupture following normal vaginal delivery: A report of two cases over 11 yearsSingapore J Obstet Gynaecol20013237879
- FarajRO’DonovanPJonesAHillSSpontaneous rupture of urinary bladder in second trimester of pregnancy: A case reportAust N Z J Obstet Gynaecol200810;485520
- CatanzariteVCousinsLDowlingDDaneshmandSOxytocin-associated rupture of an unscarred uterus in a primigravidaObstet Gynecol20061083 Pt 272372517018478