Abstract
Autonomy is considered essential for decision-making in a range of health care situations, from health care seeking and utilization to choosing among treatment options. Evidence suggests that women in developing or low-income countries often have limited autonomy and control over their health decisions. A review of the published empirical literature to identify definitions and methods used to measure women’s autonomy in developing countries describe the relationship between women’s autonomy and their health care decision-making, and identify sociodemographic factors that influence women’s autonomy and decision-making regarding health care was carried out. An integrated literature review using two databases (PubMed and Scopus) was performed. Inclusion criteria were 1) publication in English; 2) original articles; 3) investigations on women’s decision-making autonomy for health and health care utilization; and 4) developing country context. Seventeen articles met inclusion criteria, including eleven from South Asia, five from Africa, and one from Central Asia. Most studies used a definition of autonomy that included independence for women to make their own choices and decisions. Study methods differed in that many used study-specific measures, while others used a set of standardized questions from their countries’ national health surveys. Most studies examined women’s autonomy in the context of reproductive health, while neglecting other types of health care utilized by women. Several studies found that factors, including age, education, and income, affect women’s health care decision-making autonomy. Gaps in existing literature regarding women’s autonomy and health care utilization include gaps in the areas of health care that have been measured, the influence of sex roles and social support, and the use of qualitative studies to provide context and nuance.
Introduction
Women’s ability to attend to their health and utilize health care facilities appropriately may depend in part on their decision-making autonomy. In many societies, especially in developing or low-income countries, the status of women often limits their autonomy and ability to make decisions about many aspects of their own lives. Many such societies still have strong social structures that rigidly define the roles of men and women, usually encoded in religious, tribal, and social traditions. These constraints often define the circumstances under which women have or do not have autonomy to make decisions regarding their own health. In the literature on maternal health, women’s decision-making ability regarding use of health services is often discussed using the concept of autonomy.Citation1 Despite significant philosophical literature devoted to the concept of autonomy, no univocal meaning of the concept exits.Citation2 Similarly, although women’s autonomy is widely referred to in many studies, especially about reproductive issues, there is no single widely accepted definition that represents the multiple dimensions of autonomy.Citation1 Dyson and Moore,Citation3 for example, define autonomy as the technical, social, and psychological ability to obtain information and to use it as the basis for making decisions about one’s private concerns and those of one’s intimates. BasuCitation4 defined women’s autonomy as the capacity and freedom to act independently, for example, the ability to go places, such as health facilities or the market, or to make decisions regarding contraceptive use or household purchases alone and without asking anyone’s permission. MasonCitation5 also defined autonomy as women’s ability to make and execute independent decisions pertaining to personal matters of importance to their lives and their families. Some studies show that women with greater autonomy are more likely to seek health care for themselvesCitation6 and use different forms of health care services available to them.Citation7,Citation8
Studies have also shown that increased female autonomy confers benefits such as long-term reduction in fertility, higher child survival rates, and allocation of resources in favor of children in the household.Citation9 To further examine the relationship between women’s autonomy in developing countries and their ability to make health care decisions, as well as the influence of sociocultural and other characteristics on women’s autonomy, we reviewed published empirical literature about health care decision-making among women in developing countries, with special interest in the description and measurement of autonomy. Specifically, the aim of this review was to describe 1) definitions and methods that studies have used to measure women’s autonomy in developing countries, 2) the relationship between women’s autonomy and their health care decision-making and utilization across a range of health care, and 3) factors that influence women’s autonomy and decision-making regarding health care.
Materials and methods
Sources of information
All studies were found by searching through the electronic database (PubMed and Scopus). Additional searches were conducted of the gray literature using Google Scholar, and relevant articles were included in the review. Following the identification of relevant articles, the reference lists of articles identified were searched to locate relevant publications not indexed in the database.
Search strategy
The following search terms were used to search all databases to identify research studies from developing countries: “autonomy”, “decision-making”, “decision-making autonomy”, “women’s autonomy”, “women’s health”, “female”, “health”, “clinical”, “hospital”, “disease”, “developing countries”, “low and middle income countries”, “underdeveloped”, “Africa”, “sub-Sahara”, “reproductive health”, “third world”, and “maternal health services”. The exact search strategy using MeSH terms for PubMed and Scopus is described in detail in the Supplementary materials.
Study selection and data extraction
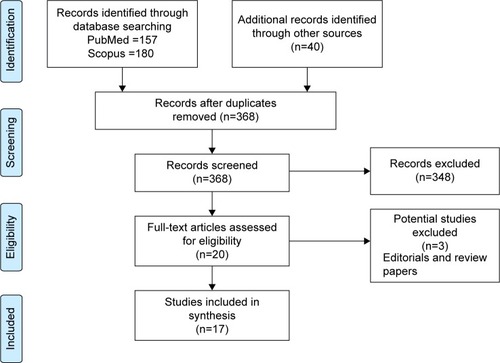
The process of study selection and extraction is presented in a PRISMA flow chart in . The search returned 377 publications from PubMed (157), Scopus (180), Google Scholar (28), and the reference list of identified articles (12). After removing duplicates, 368 studies remained. After screening titles and abstracts for relevance, ie, studies presenting data (including primary and secondary data) were included if they evaluated and reported women’s autonomy in health care decision-making or decision-making as a function of autonomy, 348 studies were excluded. Therefore, 20 full texts were assessed, and then three additional studies were excluded because they were reviews or commentaries. A final set of 17 articles were included in the review. A quality assessment of the included studies was not done because our aim was to synthesize the literature rather than summarize the estimates of an effect size derived from a systematic review.
Figure 1 Summary of search strategy.(/P)(P)Note: Based on the PRISMA statement template from Moher D et al.Citation47
Inclusion criteria
Studies were included in the review if they met the following criteria:
Publication in English
Original articles
Investigations on women’s decision-making autonomy about health and health care utilization
Developing or low-income country context.
Results
Characteristics of reviewed articles
Most (eleven) of the studies were conducted in South Asia, five in Africa, and one in Central Asia. Only one study utilized a combination of quantitative and qualitative methods of data collection, while the remaining 16 used quantitative methods. Regarding data source, the majority (12) used secondary data from their countries’ national demographic and health surveys, and five collected primary data. Most studies (14 of 17) focused on women’s decision-making autonomy in respect to maternal/reproductive health care utilization, and three investigated women’s decision-making about health care more broadly ().
Table 1 Characteristics of reviewed articles
Definition and assessment of autonomy and decision-making
Twelve of the 17 articles defined women’s autonomy using definitions from prior authors and literature, two had study-specific definitions, and another three did not report a definition of autonomy (). The majority adopted definitions proposed by Dyson and MooreCitation3 or Basu.Citation4 For example, five studiesCitation10–Citation14 used Dyson and Moore’sCitation3 definition alone, which defined autonomy as the “ability – technical, social, and psychological – to obtain information and to use it as the basis for making decisions about one’s private concerns and those of one’s intimates.” Two studiesCitation7,Citation15 used a combination of the definition of Dyson and MooreCitation3 and Basu,Citation4 defining female autonomy as “the capacity to manipulate one’s environment through control over resources and information for personal interest.” Five studiesCitation1,Citation6,Citation16–Citation18 combined aspects of Dyson and MooreCitation3 and Basu’sCitation4 definitions with other previously published definitions.Citation9,Citation19–Citation24 Senarath and GunawardenaCitation25 used a study-specific definition of women’s autonomy specifically related to health care and household decisions as “the proportion of women who make the decision either alone or jointly with husband or someone else,” while AllendorfCitation26 defined autonomy as “women’s opportunity to make choices that affect their lives.”
Table 2 Definition and measures of women’s autonomy
Nine of the papers had study-specific measures of female autonomy. Most of these included the following as common components of women’s autonomy: decision-making over household matters or health care, control over some finances, and freedom of movement. For instance, Thapa and NiehofCitation13 in their study measured autonomy in four dimensions, including economic autonomy, domestic autonomy, movement autonomy, and intraspousal communication; Mistry et alCitation15 measured women’s autonomy across three dimensions, including decision-making autonomy, permission to go out, and financial autonomy; Bloom et alCitation6 assessed the degree of women’s autonomy in three related areas: control over finances, decision-making, and extent of freedom of movement. Dharmalingam and PhilipCitation12 used similar measures in South India where the study focused on perceived economic independence, freedom to move within and between villages, and spousal interaction as measures of autonomy. Women’s participation in household decisions was often considered an indicator of women’s autonomy in decision-making.Citation25 Nigatu et alCitation18 specifically measured autonomy by the composite index of three constructs of women’s autonomy: control over finances, decision-making power, and extent of freedom of movement. Fotso et alCitation16 used a principal component analysis (PCA) method to generate measures of autonomy, and used responses to nine questions as a “decision-making autonomy” variable, from six additional questions to create a “freedom of movement autonomy” variable, and then used all the questions to generate an “overall autonomy” variable. Each measure of autonomy (ie, the principal component) was then recoded as tertiles with categories labeled low autonomy, middle autonomy, and high autonomy. In one study,Citation17 women’s decision-making power within the household was used as a proxy indicator to measure female autonomy.
Eight of the 17 articles adopted measures of women’s autonomy from questions in their country’s Demographic Health Surveys (DHS). For example, among Bangladeshi women, decision-making autonomy was measured based on responses to individual questions regarding who makes decisions in the household about 1) obtaining health care, 2) large household purchases, 3) household purchases for daily needs, 4) visits to family or relatives, and 5) child health care.Citation7 Similarly, using items in the Ethiopian Demographic Health Survey, Woldemicael and TenkorangCitation1 considered four behavioral indicators that measured the degree of a woman’s autonomy: who has the final say on 1) making large household purchases, 2) making household purchases for daily needs, 3) obtaining the woman’s own health care, and 4) freedom of movement. In Ghana, autonomy was measured by a novel five-point scale created from existing DHS items: women’s freedom of movement, discretion over earned income, decision-making related to economic matters, freedom from violence or intimidation by husbands, and decision-making related to health care.Citation27
Decision-making autonomy and women’s health care
The reviewed studies found varying levels of health care decision-making autonomy in different countries and among different regions of the same country. Among Nepalese women, a low level of women’s autonomy was found to be a contributory factor to poor maternal health service utilization.Citation13 A study using nationally representative household surveys found that 13.4% of ever-married women in the reproductive age group in Nepal, 17.6% in Bangladesh, and 28.1% in India made decisions alone regarding care for their own health, including 11.5% of current users of contraceptives who reported that they alone made decisions to use contraception.Citation25 At the same time, however, health care decisions were made without women’s participation in the majority of Nepalese households (72.7%) and approximately half of Bangladesh (54.3%) and Indian (48.5%) households.Citation25
This was consistent with the study findings among Bangladeshi women that more than one-third (37.3%) were not involved in decision-making about their own health care,Citation7 and among women in rural India, more than half (55.6%) were not involved in decision-making about their own health care.Citation15 Nigatu et alCitation18 reported that about half of the women in their Ethiopian study had the autonomy to take their child to a health facility, while 43.9% of women were free to go to a health facility for their own health care service needs. They also reported that of the 65.2% women who had access to money, 38.1% of them were autonomous to use the money for health services utilizations without consulting others.
Decision-making with respect to different types of health care
Most of the reviewed papers examined autonomy in the context of decisions about reproductive health. Mistry et alCitation15 reported that greater autonomy in decision-making increased the likelihood of women receiving prenatal, delivery, and postnatal care in rural India and stressed that low levels of autonomy adversely affect women’s likelihood of using pregnancy care services, especially prenatal and postnatal checkups. Rahman et alCitation7 reaffirmed the association between women’s autonomy and contraceptive use in Bangladesh. Nigatu et alCitation18 reported that a higher degree of women’s autonomy in household decision-making greatly increased the use of contraception. Similar findings were reported by Al Riyami et alCitation11 for women in Oman and by Saleem and BobackCitation28 in Pakistan.
KamiyaCitation17 reported that in households in which female members make decisions on financial matters, women have a greater chance of receiving antenatal and delivery care. Mistry et alCitation15 also showed that financial autonomy of women was associated with the use of delivery care and postnatal checkups. Similarly, Saleem and BobakCitation28 reported a significant association between decision-making autonomy and contraceptive use, even after controlling for sociodemographic variables. In contrast, Fotso et alCitation16 did not find any relationship between utilization of maternal health services for delivery and high levels of women’s overall autonomy, freedom of movement, or decision-making in Kenya. Three studies found that the level of autonomy affects women’s health care seeking generally, not limited to reproductive health.Citation10,Citation25,Citation26 No study, however, examined other specific domains of health care such as immunization, surgical procedures, invasive clinical procedures (such as biopsies), hospital admission, or blood transfusion.
Determinants of women’s decision-making autonomy
Some of the reviewed studies examined factors such as age, education, and other socioeconomic and cultural factors to describe their influence on women’s decision-making autonomy. One of the studies from South AsiaCitation25 reported that women’s autonomy and decision to seek health care were determined by social and cultural factors and, in some cases, legal constructs and practices and perceived beliefs about the severity of the illness. Haque et alCitation29 found that mothers with greater autonomy are more likely to be older, have more education, live in urban areas, and be among the richest bands of wealth. Similarly, Acharya et alCitation10 found that increased age, paid employment, more education, and having a greater number of living children were all positively associated with women’s autonomy in decision-making.
Nigatu et alCitation18 reported that women in Ethiopia who have primary, secondary, and postsecondary education are about two and four times more likely to have higher autonomy compared to women with no formal education. KamiyaCitation17 reported no statistically significant relationship in Tajikistan between women’s autonomy and their educational attainment, but a favorable association with the husbands’ education, implying that educated husbands are more likely to include female family members in decision-making processes. The latter finding was corroborated by Nigatu et alCitation18 where along with household income, women’s age, and husbands’ employment, husbands’ secondary educational status was significantly associated with women’s autonomy in seeking health care services for themselves. In Bangladesh, Haque et alCitation29 expressed the notion that because women are governed by social norms of female seclusion, even in instances where women wish to make decisions regarding their health care, they may need help and agreement from other family members, particularly their husbands or mothers-in-law.
Discussion
Female autonomy has been widely acknowledged as a multidimensional entity that refers to different aspects of women’s lives. In addition to its significant intrinsic value, autonomy is considered instrumentally essential for decision-making in a range of health care situations, from health care seeking and utilization to choosing among treatment options. This review synthesized the published empirical research on women’s autonomy in health care decision-making in developing countries and included studies using diverse methodologies, from different geographical and cultural settings, and within different health care systems. Several themes emerged: 1) despite the observation that there is no one widely accepted operational definition for autonomy, there are common elements to most definitions utilized in these studies and these elements lend themselves to measuring the level of women’s autonomy; 2) autonomy that supports health care decision-making is associated with better health outcomes, although these studies predominantly examined reproductive health, and very few other areas of women’s health care; and 3) several sociocultural factors, such as education, age, and income, positively affect women’s autonomy, independent of the country or culture in which they live.
Most of the studies of women’s autonomy related to health care decision-making used definitions of autonomy that encompassed similar dimensions – the ability to obtain information and make decisions about one’s own concerns, have some control over finances and have some freedom of movement.Citation3–Citation5,Citation30,Citation31 Stemming from these definitions, a number of dimensions of women’s autonomy are recognized, including household and health care decision-making autonomy, movement autonomy, and economic autonomy.Citation13 Most studies measure three or more of these dimensions, while some attempt to measure all.
Although previous discussions about how to measure autonomy exist,Citation32,Citation33 a set of questions included in the national demographic and health surveys has led to a standard measure of women’s autonomy. A big advantage of the DHS system is that the same questions are asked across many women in many countries. Nonetheless, just four or five items measure autonomy in DHS (depending on the phase of the DHS), and these may not adequately capture the complexity of women’s autonomy. Also, it remains uncertain how well validated the DHS autonomy questions are, both internally and when compared with more detailed measures of autonomy. Indeed, it has been shown that dimensions of autonomy used in surveys are not always internally consistent.Citation20 One study examined internal consistency for autonomy measures in four dimensions each of which was measured with multiple items and showed Cronbach’s α ranging from 0.61 for domestic autonomy to 0.96 for economic autonomy.Citation13 Cronbach’s α is a measure of internal consistency for items on a scale (ranging in value from 0 for no internal consistency to 1 for the highest possible internal consistency). The wide variation observed (0.61–0.96) indicates that the items on autonomy measures often show different degrees of internal consistency for different dimensions of autonomy. Furthermore, different dimensions may show varying association with outcomes such as child nutritionCitation34 and husband’s involvement in maternal health care.Citation13 Alternative methods to the DHS method of measuring women’s autonomy are also employed in the identified literature. Several of the studies in this review included additional measures of financial control and freedom of movement to measure autonomy supplementing questions about health care and household decision-making.Citation6,Citation18 This observation raises questions, however, about the extent to which autonomy in decision-making over financial matters is measuring the same underlying concept as autonomy in making daily decisions for the household. Furthermore, survey item responses have limited ability to capture nuance and complexity, and the interpretation of the findings may not be so straightforward. In one study, for example, of 23 communities in five Asian countries, it was shown that wives and husbands differ in their assessment of the level of the wife’s autonomy.Citation35 Although this may be a reflection of the different perspectives of who is answering the questions, it may also point to geographical or contextual differences in sex roles and perceptions of women’s autonomy. For example, in societies where pregnancy or minor household issues are considered a “woman’s domain”, women may seem to have more autonomy than in societies where these are not considered women’s domain. Therefore, because of specific cultural characteristics of a society and differences in interpretation (among other reasons), the standard questions used in measuring autonomy may not be equally valid across different cultural contexts.
For such a complex and multifaceted concept, only one studyCitation13 used qualitative research methods to study autonomy. Qualitative methods have the advantage of being able to contextualize findings and capture nuance. For example, the qualitative component of Thapa and Niehof’sCitation13 study brought up issues such as women’s dependence on men’s consent for the use of specific medical services, husbands’ feeling of a sense of responsibility for maternal health care decisions, women valuing their husbands’ support and presence during pregnancy care (traditionally considered a woman’s domain), sociocultural norms that may stigmatize men for being too supportive during their wives’ maternity period, and changing social norms about the expected role of husbands in maternal health. Qualitative studies could help clarify, for example, which dimensions of women’s autonomy are relevant to their health care decisions and how to measure them. Qualitative studies could also further the understanding of how to distinguish women’s autonomy from social support in our measured constructs. For example, when a decision is made jointly with a husband/partner or others, it is often interpreted as indicating lower autonomy for the woman. Yet, making a decision alone may represent more autonomy or simply lack of support from a husband/partner who would rather not be involved.Citation34 Indeed, some studies have shown that a higher level of women’s autonomy, as measured by her sole final decision-making power, was associated with significantly lower male involvement in pregnancy health.Citation13,Citation36 However, as these findings were from survey responses, the reasons remain speculative.
An important philosophical issue is what it means for individuals to be autonomous within any culture or society. Given that people are always imbedded in their social context, their decisions often take into account consideration for others in their households and communities, and decisions may not be, or appear not to be fully autonomous. Indeed, questions about autonomous decision-making are especially pertinent in the context of health care and medical services in which the individual rarely “stands alone” in decision-making without consideration for and influence of family, loved ones, and caregivers. The concept of individual in contemporary Western cultures is often understood as independence, self-sufficiency, and self-directedness. However, autonomy as an individualistic ideal has been called into question for several reasons,Citation37–Citation40 including the fact that it overlooks or even devalues relationships of interdependence (such as friendships, loyalty, caring, and responsibility) and also ignores the fact that people are socially embedded, with part of their identity being constituted by their social relations. Authors writing from developing countries have found notions of individualistic autonomy to be particularly ill-suited to their environment. For example, Mumtaz and SalwayCitation41 identified the preeminence of communality rather than individuality as the social ethic in their empirical studies of Jatti society in Pakistan. They found that social relationships constitute an individual’s social identity and that an individual is not considered a construct separate from others. In summary, empirical researches from developing countries have called into question the adequacy and appropriateness of using a concept of individual autonomy as a basis for understanding several issues involving women’s decision-making. Some authors have proposed an alternative model of relational autonomy, which highlights the social context within which all individuals exist and acknowledges the emotional and embodied aspects of decision makers.Citation42 Relational autonomy may be particularly applicable to decision-making in health care, especially reproductive health care. Reproductive issues directly involve other members of the family. Health care decisions often impact the ability to live a healthy life, livelihoods, disability, and death and could also include risky (and often painful) procedures, lifelong treatment for chronic disease, major surgery, rehabilitation, and physical therapy. Individuals may be ill-equipped to deal with these kinds of decisions in an individualistic, autonomous manner. Relational autonomy explicitly acknowledges the supportive and interdependent roles played by other household members, caregivers, and others within the social context of the individual.
Despite the wide spectrum of women’s health care needs and health care utilization, most studies of women’s autonomy in developing countries focused on reproductive health. This could partly reflect developing countries’ national surveys that focus on fertility, contraception, reproductive health, or maternal and child health. For Western countries, there is a rich literature on women’s decision-making in other areas of health care, for example, cancer treatment.Citation43–Citation46 For developing countries, there are no comparable studies of women’s cancer treatment decision-making and simply no data that we could find on how women make decisions about many other important components of health care. Each of these components requires informed consent and involves crucial decision-making steps. To complicate matters, many of these areas have specific cultural implications that could influence decision-making. It is well recognized, for example, that blood transfusions are not acceptable in certain religious traditions (eg, Jehovah’s Witnesses). Furthermore, blood has a special place in tribal/cultural beliefs in various cultural contexts (especially in sub-Saharan Africa), which may introduce limits on decision-making autonomy. Currently, there remains a substantial gap in the literature on women’s decision-making about health care issues in developing countries outside of the realm of reproductive health.
Many factors were shown to affect women’s autonomy in the reviewed studies, including age, employment status, and wealth (or household income). Notably, these factors are highly correlated and, in general, show the expected relationship with women’s autonomy, ie, older women who are employed and in a certain income bracket have higher levels of decision-making autonomy. Education was also a factor influencing women’s autonomy in various studies. Highly educated women are more likely to be knowledgeable about their own health, have more self-confidence, and be more assertive than those with less or no education.
This review has certain limitations. First, as the reviewed studies come from a limited number of countries in South Asia, central Asia, and Africa, the findings may not be generalizable to other developing countries. Secondly, we only considered the English literature. There could be relevant scientific studies from countries in which the primary language is French, Spanish, Portuguese, or Arabic, which our review did not cover. Nonetheless, the review provides a synthesis of a wide range of studies examining women’s autonomy with regard to health care decision-making in developing or low-income country settings. Notably, we summarize factors found to be associated with women’s autonomy in empirical research, identify gaps in the literature, and highlight opportunities for further research.
Conclusion
Both enabling autonomous decision-making and respecting women’s autonomy are valuable and laudable goals. Educating and empowering women will promote their autonomy and contribute to addressing the sustainable development goals of good health, quality education, and sex equality. Autonomy is considered essential for decision-making in a range of situations, from health care seeking and utilization to choosing among treatment options. This review of published empirical research on women’s autonomy and decision-making in developing countries found that studies use operational definitions of autonomy that have common elements and use a small range of methods in measuring the level of women’s autonomy. Studies show that autonomy is positively associated with health care decision-making and better health outcomes, although the literature has predominantly examined reproductive health, and very few other health decisions affecting women. Age, education, and income level are factors that affect women’s autonomy, independent of the specifics of the country or culture in which they live.
This review identified important gaps in the literature, including lack of data on other health care decisions beyond reproductive/maternal health (such as surgical procedures, hospital admissions, or blood transfusions) and lack of qualitative studies to provide nuance and explain the relationship between developing country, women’s autonomy, and their ability to make health care decisions, including clarifying the role of social support, sex roles, and cultural norms in relation to women’s autonomy. Further validation of the measures of autonomy that have been used, including those based on the widely used DHS questions, would help illuminate these issues across countries and time. These and other themes are vital areas for future research to help understand and promote autonomous decision-making among women.
Acknowledgments
The authors appreciate the comments and suggestions of David DeGrazia, Joe Millum, Adebowale Adeyemo, Katie Byron, and Boniface Ushie.
Supplementary material
Terms used to search PubMed
(women’s health [MeSH] or women’s health services [MeSH] or maternal health services [MeSH] or prenatal care [MeSH] or pregnancy [MeSH] or pregnancy, unwanted [MeSH] or family planning services [MeSH] or contraception [MeSH] or abortion, induced [MeSH] or reproductive rights [MeSH] or breastfeeding [MeSH] or mass screening [MeSH] or hiv [MeSH] or neoplasms [MeSH] or communicable diseases [MeSH] or bacterial infections and mycoses [MeSH] or parasitic diseases [MeSH] or virus diseases [MeSH] or noncommunicable disease* [tw])
AND
(decision* [ti] or decision-making [MeSH] or autonom* [tiab] or voluntariness [tiab] or empower* [tiab] or self-determination [tw] or power [MeSH]) AND (women [mh] or women* [tiab])
AND
((develop* [tw] or underdevelop* [tw] or under develop* [tw] or underserved [tw] or under served [tw] or deprived [tw] or poor [tw] or third-world [tw] or low* income [tw] or middle income [tw]) AND (nation* [tw] or countr* [tw] or world [tw] or afric* [tw] or asia* [tw] or latin america* [tw] or south america* [tw]))
Terms used to search Scopus
(“decision-making autonomy” OR women’s autonomy) AND (female* OR women OR woman) AND (health OR medical OR clinical OR disease* OR hospital OR clinic*) AND TITLE-ABS-KEY (“developing countr*” OR “third world” OR rural OR “low or middle income” OR africa OR “sub-sahara” OR asia).
Disclosure
The opinions expressed are the authors’ and do not necessarily reflect the positions or policies of the National Institutes of Health or the US Department of Health and Human Services. The first author is a postdoctoral fellow in the Department of Bioethics, NIH Clinical Center. The authors report no conflicts of interest in this work.
References
- WoldemicaelGTenkorangEYWomen’s autonomy and maternal health-seeking behavior in EthiopiaMatern Child Health J201014698899819882240
- BeauchampTLChildressJFPrinciples of Biomedical EthicsNew York, NYOxford University Press2001
- DysonTMooreMOn kinship structure, female autonomy, and demographic behavior in IndiaPopul Dev Rev1983913560
- BasuAMCulture, the Status of Women, and Demographic Behaviour: Illustrated with the case of IndiaOxford, UKClarendon Press1992
- MasonKGender and Demographic Change: What do we KnowLiege, BelgiumInternational Union for the Scientific Study of Population1995331
- BloomSSWypijDDas GuptaMDimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian cityDemography2001381677811227846
- RahmanMMMostofaMGHoqueMAWomen’s household decision-making autonomy and contraceptive behavior among Bangladeshi womenSex Reprod Healthc20145191524472384
- UpadhyayUDHindinMJDo higher status and more autonomous women have longer birth intervals?: results from Cebu, PhilippinesSoc Sci Med200560112641265515814188
- AndersonSEswaranMWhat determines female autonomy? Evidence from BangladeshJ Dev Econ2009902179191
- AcharyaDRBellJSSimkhadaPvan TeijlingenERRegmiPRWomen’s autonomy in household decision-making: a demographic study in NepalReprod Health201071520630107
- Al RiyamiAAfifiMMabryRMWomen’s autonomy, education and employment in Oman and their influence on contraceptive useReprod Health Matters2004122314415415242223
- DharmalingamAPhilip MorganSWomen’s work, autonomy, and birth control: evidence from two south Indian villagesPopul Stud1996502187201
- ThapaDKNiehofAWomen’s autonomy and husbands’ involvement in maternal health care in NepalSoc Sci Med20139311023906115
- WadoYWomen’s Autonomy and Reproductive Healthcare-seeking Behavior in EthiopiaCalverton, MDUnited States Agency for International Development [USAID]2013
- MistryRGalalOLuMWomen’s autonomy and pregnancy care in rural India: a contextual analysisSoc Sci Med200969692693319656604
- FotsoJCEzehACEssendiHMaternal health in resource-poor urban settings: how does women’s autonomy influence the utilization of obstetric care services?Reprod Health20096919531235
- KamiyaYWomen’s autonomy and reproductive health care utilisation: empirical evidence from TajikistanHealth Policy20111022–330431321592608
- NigatuDGebremariamAAberaMSetegnTDeribeKFactors associated with women’s autonomy regarding maternal and child health care utilization in Bale Zone: a community based cross-sectional studyBMC Womens Health2014147924990689
- BrunsonEKShell-DuncanBSteeleMWomen’s autonomy and its relationship to children’s nutrition among the Rendille of northern KenyaAm J Hum Biol2009211556418792063
- KishorSSubaiyaLUnderstanding womens empowerment: a comparative analysis of Demographic and Health Surveys (DHS) dataCalverton, MarylandDHS Comparative Reports No. 202008
- MasonKOThe impact of women’s social position on fertility in developing countriesSociological Forum198724718745
- Miles-DoanRBisharatLFemale autonomy and child nutritional status: the extended family residential unit in Amman, JordanSoc Sci Med19903177837892244220
- Safilios-RothschildCFemale power autonomy and demographic change in the Third WorldLondonCroom Helm1982117132
- SenGBatliwalaSEmpowering women for reproductive rightsOxford, EnglandOxford University Press20001536
- SenarathUGunawardenaNSWomen’s autonomy in decision making for health care in South AsiaAsia Pac J Public Health200921213714319190000
- AllendorfKCouples’ reports of women’s autonomy and health-care use in NepalStud Fam Plann2007381354617385381
- RominskiSDGuptaMAborigoRFemale autonomy and reported abortion-seeking in Ghana, West AfricaInt J Gynaecol Obstet2014126321722224920181
- SaleemSBobakMWomen’s autonomy, education and contraception use in Pakistan: a national studyReprod Health20052816242030
- HaqueSERahmanMMostofaMGZahanMSReproductive health care utilization among young mothers in Bangladesh: does autonomy matter?Womens Health Issues2012222e171e18021968029
- BalkDIndividual and community aspects of women’s status and fertility in rural BangladeshPopul Stud19944812145
- SchulerSRHashemiSMCredit programs, women’s empowerment, and contraceptive use in rural BangladeshStud Fam Plann199425265768059447
- AgarwalaRLynchSMRefining the measurement of women’s autonomy: an international application of a multi-dimensional constructSoc Forces200684420772098
- KabeerNResources, agency, achievements: reflections on the measurement of women’s empowermentDev Change1999303435464
- CarlsonGJKordasKMurray-KolbLEAssociations between women’s autonomy and child nutritional status: a review of the literatureMatern Child Nutr201511445248224521434
- GhumanSJLeeHJSmithHLMeasurement of women’s autonomy according to wives and their husbands: evidence from five Asian countriesPaper presented at: Annual Meeting of the Population Association of AmericaMarch 2002Washington, DC
- MullanyBCHindinMJBeckerSCan women’s autonomy impede male involvement in pregnancy health in Katmandu, Nepal?Social Science & Medicine20056191993200615922498
- CodeLWhat can she Know?: Feminist Theory and the Construction of KnowledgeIthaca, NYCornell University Press1991
- NedelskyJReconceiving autonomy: sources, thoughts and possibilitiesYale J L Feminism198917
- CarstenJSubstantivism, antisubstantivism, and anti-antisubstantivismFranklinSarahMcKinnonSusanRelative Values: Reconfiguring Kinship StudiesDurham, NCDuke University Press20012953
- JefferyPJefferyRLyonALabour pains and labour power: women and childbearing in IndiaLondon, UKZed Books1989
- MumtazZSalwaySUnderstanding gendered influences on women’s reproductive health in Pakistan: moving beyond the autonomy paradigmSoc Sci Med20096871349135619232810
- Walter, Ross. 2014.
- DrewEMSchoenbergNEDeconstructing fatalism: ethnographic perspectives on women’s decision making about cancer prevention and treatmentMed Anthropol Q201125216418221834356
- GilbarRGilbarOThe medical decision-making process and the family: the case of breast cancer patients and their husbandsBioethics200923318319218410461
- PrimoWQGarrafaVEthical issues of diagnosis disclosure and treatment in patients with genital or breast cancerRev Assoc Méd Bras201056439740220835634
- TwomeyMAutonomy and reason: treatment choice in breast cancerJ Eval Clin Prac201218510451050
- MoherDLiberatiATetzlaffJAltmanDGThe PRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med200966e100009719621072
