Abstract
Purpose
Limited research has examined the factors associated with female permanent contraception procedures. This study evaluated the temporal trend in the use of hysteroscopic sterilization (HS) vs laparoscopic sterilization (LS) and characteristics of commercially insured and Medicaid-insured women in the US who have had the procedures.
Methods
Women aged 15–49 years with claims for HS and LS procedures were identified from two MarketScan databases, one consisting of commercial claims and the other Medicaid claims, during the time period of January 1, 2003 to December 31, 2012 and January 1, 2006 to December 31, 2011, respectively. Proportions and characteristics of women who underwent HS or LS procedures were determined. Multivariable logistic regressions were used to identify characteristics associated with the use of HS vs LS.
Results
Commercially insured women who had HS (n=32,012) vs LS (n=64,725) were slightly older (37.2 years vs 36.4 years, respectively, P<0.001) but had similar Charlson Comorbidity Index scores. Among commercially insured women, those who had a sterilization procedure during 2008–2012 were more likely to undergo HS (odds ratio: 7.1, P<0.001) than those who had a sterilization procedure during 2003–2007. Medicaid-insured women who had HS (n=2,001) were also slightly older than women who had LS (n=12,523; 30.1 years vs 28.8 years, respectively, P<0.001) but had a higher mean Charlson Comorbidity Index score (0.32 vs 0.25, respectively, P<0.001). Among Medicaid-insured women, the likelihood of having HS vs LS increased 3.3-fold (P<0.001) in years 2009–2011 compared to years 2006–2008. Among both populations, older age, obesity, and the use of oral contraceptives within the previous 12 months were associated with having HS vs LS.
Conclusion
Among both commercially insured and Medicaid-insured women, the likelihood of having HS vs LS increased over time.
Introduction
Female sterilization is the second most common contraceptive method used in the US, with 15.5% of women aged 15–44 years having used this method during years 2011–2013.Citation1 Female permanent birth control methods performed as interval procedures (ie, any time remote from delivery) include laparoscopic sterilization (LS) and hysteroscopic sterilization (HS). LS involves one or two abdominal wall skin incisions followed by the insertion of a laparoscope into the peritoneal cavity, insufflation of the cavity with carbon dioxide, and ligation of the fallopian tubes.Citation2 The procedure generally requires use of general anesthesia.Citation2 In November 2002, a hysteroscopic method of female sterilization, the Essure system (Bayer HealthCare Pharmaceuticals Inc., Whippany, NJ, USA), was approved by the US Food and Drug Administration (FDA) in the US for permanent birth control.Citation3 The Essure procedure is a nonincisional method of female sterilization, which involves the insertion of a 4 cm long implant into each fallopian tube via hysteroscopy.Citation3,Citation4 The implant consists of a flexible Nitinol (nickel–titanium alloy) outer coil that anchors the device in the fallopian tube and an inner coil containing polyethylene terephthalate fibers.Citation4 The polyethylene terephthalate fibers induce benign tissue in-growth that permanently occludes the fallopian tubes.Citation4 This process occurs over the course of 3 months, and an alternative contraception method must be used in the interim.Citation3 An Essure Confirmation Test (a modified hysterosalpingogram) is performed at 3 months to confirm appropriate location of the devices and occlusion of the tubes.Citation3
A second hysteroscopically placed device, Adiana (Hologic, Inc., Bedford, MA, USA), was approved by the FDA in 2009.Citation5 Adiana achieves tubal occlusion by tissue in-growth into a silicone matrix placed bilaterally within the fallopian tubes.Citation5 After the application of radiofrequency energy inside the fallopian tubes, the silicone matrix is deployed into the tubal lumen where the lesion was formed.Citation5 The endothelial damage caused by the radiofrequency energy encourages a tissue in-growth response primarily consisting of fibroblasts infiltrating the porous structure of the silicone matrix, thereby resulting in occlusion in ~3 months.Citation5 As with Essure, alternative contraception must be used until bilateral tubal occlusion is confirmed by a hysterosalpingogram confirmation test.Citation5 Adiana was discontinued from the market in 2012 due to financial reasons.Citation6 In contrast to laparoscopic methods, HS avoids entry into the peritoneal cavity.Citation3,Citation4 The procedure does not require use of general anesthesia and may be performed in an outpatient setting.Citation3,Citation4 The hysteroscopic approach avoids the major morbidity associated with general anesthesia and abdominal surgery.Citation7 LS, on the other hand, does not require interim contraception for 3 months or a confirmation test.
A US study reported that the annual number of tubal sterilizations declined between 1995 and 2006, and the decline may be attributed to demographic, economic, social, and cultural factors.Citation8 This study and others have reported that certain characteristics are associated with a greater likelihood of undergoing sterilization procedures.Citation8,Citation9 These include race (eg, more African American than Caucasian women undergo sterilization), insurance status (eg, more women with no or public insurance than women with private insurance undergo sterilization), and other factors such as education level, parity, and poverty level.Citation8,Citation9 Despite the availability of these permanent female contraception procedures for over 10 years, there is a lack of information on the characteristics of women who have HS vs LS. Therefore, the objectives of this study were to evaluate the temporal trend in the use of HS vs LS and the characteristics of women in the US who had the procedures from two large claims databases.
Methods
Study populations
Data of women aged 15–49 years with inpatient or outpatient claims for HS and LS procedures, identified by Current Procedural Terminology codes, were extracted from two Truven Health claims databases (Truven Health Analytics, Ann Arbor, MI, USA), the MarketScan Commercial and Medicaid claims databases during the time period of January 1, 2003, to December 31, 2012, and January 1, 2006, to December 31, 2011, respectively. The MarketScan commercial database encompasses >60 million employees, spouses, and dependents located in all ten US census regions and consists of health care claims data from >100 different insurance companies. The MarketScan Medicaid database pools claims from >36 million Medicaid enrollees from eleven geographically dispersed states. Claims from these databases consist of inpatient and outpatient information, fully integrated health and productivity data, and laboratory data, reflecting treatment patterns and costs in routine clinical practice. The databases facilitate longitudinal studies by providing integrated, standardized, data spanning, extensive time periods and have been used for the analysis of contraceptive use patterns in prior studies.Citation10–Citation12 In compliance with the Health Insurance Portability and Accountability Act of 1996, the databases consist of fully deidentified data sets, with synthetic identifiers applied to patient-level and provider-level data to protect the identities of both the patients and data contributors. This study was exempt from internal review board oversight in accordance with the Department of Health and Human Services Policy for Protection of Human Research Subjects (45 CFR §46.101(b)(4)).
The study was carried out using these two databases to provide a more comprehensive evaluation of the use of HS and LS among these different study populations. Given the differences in methodology and available data contents, it is not possible to combine information from the two databases. The different timelines are due to the fact that the databases have different data availability. As the data included years 2009–2012, both Adiana and Essure HS procedures could have been used during these years. Women were required to have 12 months of continuous health and prescription drug coverage prior to the date of the sterilization procedure (index event). Women were excluded if they had another sterilization procedure in the 12 months prior to the index event or if they had a pregnancy or delivery claim within 6 weeks prior to the index event in order to limit the analysis to just the interval procedures.
Measurements
The proportions of women who received HS and LS were determined from the commercially insured and Medicaid-insured study populations separately, as well as stratified by year of index event. Demographics and clinical characteristics, including age, health plan type, US geographic region (commercially insured population only), race (Medicaid- insured population only), prior oral contraceptive use during the 12-month preindex time period, and most recently used prescription contraceptive type prior to sterilization procedure, were evaluated for each study cohort within the study populations. Charlson Comorbidity Index (CCI) scores, which are predictive of 1-year mortality based on a range of comorbid conditions (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatologic disease, peptic ulcer disease, mild liver disease, diabetes, hemiplegia, renal disease, diabetes with end organ damage, tumor without metastasis, leukemia, lymphoma, moderate or severe liver disease, metastatic solid tumor, and acquired immune deficiency syndrome),Citation13 were determined for each woman in the study cohorts as a measure of general comorbidity. Additionally, the proportions of women who had inflammatory bowel disease, asthma, hypothyroidism, obesity, rheumatoid arthritis, diabetes, hypertension, and systemic lupus erythematosus, which were identified by the International Classification of Diseases, Ninth Revision, Clinical Modification Codes, were determined. These chronic conditions were previously examined by DeNoble et alCitation14 because of their prevalence in reproductive-aged women.
Statistical analyses
For study cohorts, Student’s t-tests were used to compare differences in age and CCI scores. Other measured demographics and clinical characteristics, along with year groups, were described using descriptive statistics. Logistics regressions were used to identify characteristics of women associated with different likelihoods of having HS vs LS procedures in the two study populations separately. All statistical analyses were carried out using SAS (SAS Institute Inc., Cary, NC, USA).
Results
Study populations
shows the process of selection of women included in the study cohorts. Demographics of cohorts within the commercially insured study population are listed in . Among the commercially insured study population, 32,012 had HS and 64,725 had LS. Women who had HS vs LS were slightly older (37.2 years vs 36.4 years, respectively, P<0.001). The use of HS increased among women over time from 9.7% in years 2003–2007 to 42.9% in years 2008–2012, while the use of LS decreased over time from 90.3% in years 2003–2007 to 57.1% in years 2008–2012.
Figure 1 A patient flow diagram of the selection of women in the commercially insured and Medicaid-insured study populations.
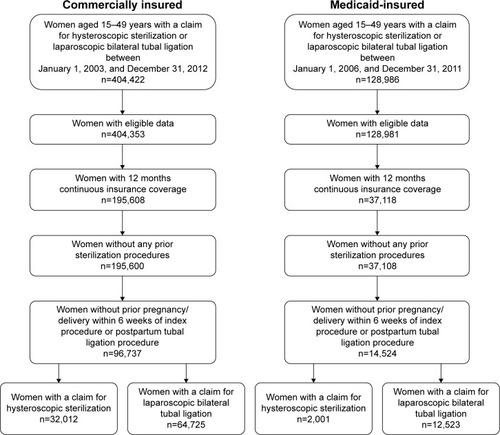
Table 1 Demographics of study cohorts within commercially insured study population
Demographics of cohorts within the Medicaid-insured study population are listed in . Among the Medicaid insured study population, 2,001 had HS and 12,523 had LS. Women who had HS vs LS were also slightly older (30.1 years vs 28.8 years, P<0.001). Greater proportions of black women (16.4%) and Hispanic women (21.4%) had HS in comparison to white women (11.3%). The use of HS increased among women over time from 7.1% in years 2006–2008 to 20.6% in years 2009–2011, while the use of LS decreased over time from 92.9% in years 2006–2008 to 79.4% in years 2009–2011.
Table 2 Demographics of study cohorts within Medicaid-insured study population
Clinical characteristics of study populations
Clinical characteristics of both study populations are listed in . In the commercially insured study population, fewer women in the HS group used prescription contraception in the 12 months prior to sterilization than did women who had LS (38.9% vs 55.5%, respectively). No information on nonprescription contraceptive methods is available. The most common type of prescription contraception most recently used prior to having either HS or LS was oral contraceptives (33%–39%). The mean CCI scores of women who had HS and of women who had LS did not significantly differ. Of the chronic conditions evaluated, the most prevalent for both study cohorts within the commercially insured study population were hypertension, hypothyroidism, asthma, and obesity.
Table 3 Clinical characteristics of study cohorts within commercially insured and Medicaid-insured study populations
Among the Medicaid-insured study population, the proportion of women not using any prescription contraception during the 12 months prior to having a sterilization procedure was smaller for women who had HS than those who had LS (33.9% vs 54.4%). Among women who had HS, the most common type of prescription contraception most recently used prior to having HS was injectable contraceptives (37.3%), and for women who had LS, it was oral contraceptives (22.2%). The mean CCI score of women who had HS was significantly higher than that for women who had LS (0.32 vs 0.25, P<0.001). Except for rheumatoid arthritis, the evaluated chronic conditions were more prevalent among women who had HS than women who had LS. The proportion of women who were obese in the HS cohort was twice that of women in the LS cohort (15.6% vs 7.4%).
Differences in characteristics of women having HSvs LS
Results of the logistic regression of the characteristics of women having HS vs LS in the commercially insured study population are presented in . Women who had a sterilization procedure during years 2008–2012 were more likely to undergo HS (odds ratio [OR]: 7.1, P<0.001) than those who had it during years 2003–2007. Older age was associated with a slightly greater likelihood of having HS (OR: 1.03, P<0.001). Women in the Northeast were less likely to use HS than women in other US regions (all P<0.001). Compared to women in a comprehensive health plan, women with other health plans (eg, exclusive provider organization and consumer-driven health plans) were more likely to use HS (all P<0.001), with the exception of women in a point-of-service plan with capitation. Obesity (OR: 1.08, P=0.03) was associated with a greater likelihood of using HS, while chronic conditions of asthma (OR: 0.89, P<0.001) and hypertension (OR: 0.82, P<0.001) were associated with lower likelihoods of using HS. Women with oral contraceptive use during the 12-month preindex period (OR: 1.53, P<0.001) were more likely to use HS.
Table 4 Differences in characteristics of commercially insured women having HS vs LS
Characteristics of women having HS vs LS for the Medicaid-insured study population are presented in . The likelihood of using HS in years 2009–2011 increased 3.3-fold (P<0.001) compared to years 2006–2008. Obesity (OR: 1.73, P<0.001) and hypertension (OR: 1.18, P=0.03) were associated with greater likelihoods of HS use. Additionally, age (OR: 1.03, P<0.001), race (black vs white, OR: 1.48, P<0.001; Hispanic vs white, OR: 1.58, P<0.001; other race vs white, OR: 2.50, P<0.001), and having had prior oral contraceptive use (OR: 1.42, P<0.001) were all associated with greater likelihoods of using HS vs LS.
Table 5 Differences in characteristics of Medicaid-insured women having HS vs LS
Discussion
In both the commercially- and Medicaid-insured study populations, the use of HS vs LS as an interval sterilization procedure increased over time. Among women who were commercially insured, the use of HS vs LS increased approximately 7-fold from years 2003–2007 to years 2008–2012. The increase was 3.3-fold from years 2006–2008 to years 2009–2011 among Medicaid-insured women. These findings are similar to those observed in a study of women who underwent interval and postpartum sterilization procedures at the Detroit Medical Center between 2002 and 2007, in which the use of Essure HS increased 51%.Citation15 Among both commercially insured and Medicaid-insured study populations, in comparison to women who had LS, fewer women who had HS were not using any prescription contraception method in the 12 months prior to the procedure. Additionally, the use of oral contraceptives during the 12-month preindex period was associated with a greater likelihood of having HS vs LS for both study populations. Among Medicaid-insured women, women who had HS were more likely to have used injectable contraception most recent to the procedure than women who had LS (37.3% vs 13.3%), which may be related to the need for 3 months of contraception after the procedure. The use of prescription contraception requires an encounter with a health care professional. It is therefore possible that women who underwent HS had more health care encounters in the year prior to their sterilization procedure. This may have influenced the selection of HS vs LS. A recent survey study found that among women who received factual information from a nurse about Essure HS and LS procedures, the majority (93%) chose Essure HS over LS.Citation16 The primary reasons for choosing Essure HS over LS by women who took this survey were cost, fear of incision, and general anesthesia.Citation16
Among both commercially insured and Medicaid-insured women, older age was associated with a slightly greater likelihood of having HS than LS; although, it is not likely to be clinically significant. In this study, we did observe that among both commercially insured and Medicaid-insured women, obesity was associated with a greater likelihood of having HS than LS. The association of obesity with having HS vs LS was more prominent among Medicaid-insured women than commercially insured women, which may be related to the higher prevalence of obesity among Medicaid-insured women. Among Medicaid-insured women, women who had HS had higher comorbidity severity than those who had LS, as measured by the CCI score. It is unknown if this finding is related to a desire to avoid peritoneal entry and general anesthesia in women with higher risk factors. It will be interesting in a future study to examine the impact of chronic conditions on the use of HS vs LS now that the Affordable Care Act has mandated complete coverage for the full range of FDA approved contraceptive methods, including interval sterilization procedures.
Education and increasing the availability of contraceptive methods are of great importance, as the National Survey of Family Growth (NSFG) reports that the unintended pregnancy rate is ~50% in the US.Citation17 A secondary analysis of the NSFG 2006–2010 data on the use of family planning services found that in adult women, 21–45 years old, who conceived between 2006 and 2010, 41% of pregnancies were unintended. Of these unintended pregnancies, 40% occurred in women who had decided that they were finished with childbearing.Citation18 Choice of contraceptive may help explain this finding. The NSFG data show that in sexually active women who stated that they were finished with childbearing, 56% were using permanent contraception methods; however, 36% were using nonpermanent methods (eg, oral contraceptives, condoms, intrauterine devices, timed intercourse) and 8% were not using any contraception method.Citation18 This indicates that a large proportion of women who have completed childbearing remain at risk for unintended pregnancy. Although, in comparison to women using other nonpermanent methods, those using intrauterine devices have a much lower risk (0.1%–0.8% first-year failure rate) for unintended pregnancy, which is comparable to the efficacy of HS (0.7%)Citation3 and LS methods (0.5%–0.7%).Citation19
Limitations and strengths of the study
The MarketScan claims databases consist of claims submitted by health care providers for reimbursement, and such claims are subject to possible coding errors. Since the databases are based on large samples, the samples are not random and may fail to generalize well to other populations. There is a lag in data availability for the Medicaid and commercial databases, such that at the time of this study, data were not available for women beyond years 2011 and 2012, respectively. Additionally, due to privacy consideration, the Medicaid database does not allow for the identification of which states were included. As there is variability in the access to sterilization procedures in certain states, this may have had an effect on the characteristics of women who had the different sterilization procedures. A few studies have been conducted on small populations of women who underwent Essure HS or LS;Citation15,Citation16 however, this study is the first to evaluate the use of HS vs LS among large populations of women with different insurance types, demographics, and clinical characteristics. By design, this study was useful for differentiating certain characteristics of commercially insured and Medicaid-insured women who had HS vs LS, which will likely be informative for health care providers and payers in the US. Although, due to limitations of the databases (eg, Medicaid database does not include data from specific states), the results may not be generalizable to the entire US populations of women with either commercial insurance or coverage by Medicaid. Furthermore, the claims data within the databases does not contain information regarding counseling on the procedures, and this study did not yield data regarding whether women were offered a choice in the two different sterilization procedures.
Conclusion
The use of HS as an interval sterilization method has substantially increased among both commercially insured and Medicaid-insured women. For many, HS is an alternative permanent contraception method that does not require general anesthesia or entry into the peritoneal cavity and can be done in an outpatient setting.
Author contributions
PC, JL, FX, and AL participated in the design of the study, data analysis and interpretation, drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Acknowledgments
Editorial assistance was provided by Melissa Lingohr-Smith, PhD, of Novosys Health. This research was supported by Bayer HealthCare Pharmaceuticals Inc.
Disclosure
PC, AL, and FX are employees of Bayer HealthCare Pharmaceuticals Inc. JL is an employee of Novosys Health and served as a paid consultant to Bayer HealthCare Pharmaceuticals Inc. for the development of this study and manuscript. The authors report no other conflicts of interest in this work.
References
- DanielsKDaughertyJJonesJCurrent contraceptive status among women aged 15–44: United States, 2011–2013NCHS Data Brief20141731825500343
- McMarinKHysteroscopic tubal sterilization: an evidence-based analysisOnt Health Technol Assess Ser20131321135
- Essure® Permanent Birth ControlInstructions for UseNew JerseyBayer HealthCare Pharmaceuticals Inc2013
- MunroMGNicholsJELevyBVleugelsMPVeersemaSHysteroscopic sterilization: 10-year retrospective analysis of worlwide pregnancy reportsJ Minim Invasive Gynecol201421224525124126261
- Adiana® Permanent Contraception. [Instructions for Use and Radiofrequency Generator Operator’s Manual]MaineHologic, Inc2009
- Investors.hologic.com. [webpage on the Internet]Hologic Announces Second Quarter Fiscal 2012 Operating ResultsMaineHologic, Inc2012 Available from: http://investors.hologic.com/index.php?s=43&item=447Accessed April 18, 2015
- American College of Obstetricians and GynecologistsACOG Practice Bulletin No 133: benefits and risks of sterilizationObstet Gynecol20131212 pt 139240423344305
- ChanLMWesthoffCLTubal sterilization trends in the United StatesFertil Steril20109411620497790
- BorreroSSchwarzEBReevesMFBostJECreininMDIbrahimSARace, insurance status, and tubal sterilizationObstet Gynecol200710919410017197593
- LawALeeYCGorritzMPlouffeLDoes switching contraceptive from oral to patch or vaginal ring change the likelihood of timely prescription refill?Contraception201490218819424835829
- PaceLEDusetzinaSBFendrickAMKeatingNLDaltonVKThe impact of out-of-pocket costs on the use of intrauterine contraception among women with employer-sponsored insuranceMed Care2013511195996324036995
- XuXMacalusoMOuyangLKulczyckiAGrosseSDRevival of the intrauterine device: increased insertions among US women with employer-sponsored insurance, 2002–2008Contraception201285215515922067778
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- DeNobleAEHallKXuXZochowskiMKPiehlKDaltonVKReceipt of prescription contraception by commercially insured women with chronic medical conditionsObstet Gynecol201412361213122024807345
- ShavellVIAbdallahMEShadeGHJrDiamondMPBermanJMTrends in sterilization since the introduction of Essure hysteroscopic sterilizationJ Minim Invasive Gynecol2009161222718996773
- ChapaHOVenegasGPreprocedure patient preferences and attitudes toward permanent contraceptive optionsPatient Prefer Adherence2012633133622563241
- MosherWDJonesJUse of contraception in the United States: 1982–2008Vital Health Stat 23201029144 National Center for Health Statistics20939159
- cdc.gov [webpage on the Internet]An Analysis of Data From the National Survey of Family Growth (2006–2010)GeorgiaCenters for Disease Control and Prevention2015 Available from: http://www.cdc.gov/nchs/nsfg.htmAccessed April 18, 2015
- FritzMASperoffLClinical Gynecologic Endocrinology and InfertilityPhiladelphia, PAWolters Kluwer2010
