Abstract
Osteosarcopenic obesity syndrome (OSO) has recently been identified as a condition encompassing osteopenia/osteoporosis, sarcopenia and obesity. OSO is especially deleterious in older adults (even if they are not obese by conventional measures), due to age-related redistribution of fat and its infiltration into bone and muscle. Osteoporosis and bone fractures in elderly increase the risk of sarcopenia, which, through decreased mobility, increases the risk of more falls and fractures, creating a vicious cycle. Obesity plays a dual role: to a certain extent, it promotes bone and muscle gains through mechanical loading; in contrast, increased adiposity is also a source of pro-inflammatory cytokines and other endocrine factors that impair bone and muscle. As the elderly population increases, changes in lifestyle to delay the onset of OSO, or prevent OSO, are warranted. Among these changes, dietary patterns and physical activity modifications are the first ones to be implemented. The typical Western diet (and lifestyle) promotes several chronic diseases including OSO, by facilitating a pro-inflammatory state, largely via the imbalance in omega-6/omega-3 fatty acid ratio and low-fiber and high-processed food consumption. Nutritional modifications to prevent and/or alleviate the OSO syndrome include adequate intake of protein, calcium, magnesium and vitamin D and increasing consumptions of foods containing omega-3 polyunsaturated fatty acids and fiber. Certain types of physical activity, often decreased in overweight/obese women and in elderly, might preserve bone and muscle, as well as help in reducing body fat accrual and fat infiltration. Habitual daily activities and some alternative modes of exercise may be more appropriate for older adults and play a crucial role in preventing bone and muscle loss and maintaining optimal weight. In conclusion, older adults who suffer from OSO syndrome may benefit from combined efforts to improve diet and physical activity, and such recommendations should be fostered as part of public health programs.
Introduction
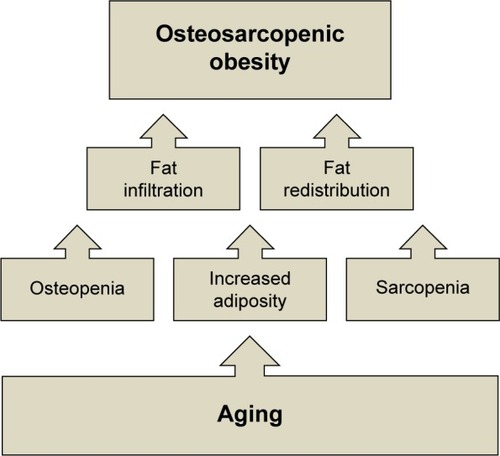
Osteosarcopenic obesity syndrome (OSO), a complex, whole-body condition related to aging and possibly to some other diseases, impacting body composition and mobility, has recently been identified and defined in older adults.Citation1,Citation2 OSO encompasses three conditions that reflect the impairment of body composition: 1) deterioration of bone health, manifested as osteopenia and/or osteoporosis; 2) decline in muscle strength and mass, manifested as sarcopenia; and 3) increased presence of fat (adipose) tissue or its ultimate redistribution and infiltration into muscle and bone.Citation1 Therefore, the components of OSO include osteopenic obesity and sarcopenic obesity (). It needs to be emphasized that “obesity” is not necessarily limited only to a clinical diagnosis of overweight/obesity but also to the redistribution of fat in muscle and bone, which is an ultimate consequence of aging.Citation1,Citation2 This redistribution of fat mass may not be detected by measuring weight or body mass index (BMI); therefore, body composition measurements might be more appropriate and useful in aging. OSO is also a result of the dysregulation of major metabolic pathways due to pro-inflammatory factors and endocrine imbalance, promoting the manifestation of osteoporosis, sarcopenia and increased adiposity, as well as low-grade chronic inflammation and insulin resistance.Citation3,Citation4 As the number of Americans over the age of 65 years surges, these diseases, separately or in combination, will become more prevalent.Citation5
Figure 1 Changes in bone fat and muscle tissues with aging, leading to osteosarcopenic obesity.
Our objective was to give more insight into the OSO syndrome and its individual components. We present briefly the possible diagnostic criteria;Citation2 still widely open for further modifications, as more knowledge is gained, and new technologies become available. We also address the impact of OSO on the overall health of individuals and society, provide some preliminary estimates of its prevalence and suggest some lifestyle measures, specifically nutrition and physical activity that might help in preventing or alleviating the OSO syndrome.
Diagnostic criteria
Some preliminary diagnostic criteria for OSO syndrome have been proposed recently.Citation2 Since OSO syndrome is a complex condition, the criteria for its identification and diagnosis must include the combination of its individual components: osteoporosis/osteopenia and/or osteopenic obesity, sarcopenia and/or sarcopenic obesity and increased adiposity. The most accurate methods in diagnosing body composition parameters, such as bone mass, lean mass and body fat, include dual-energy X-ray absorptiometry (DXA) and the magnetic resonance imaging (MRI) techniques.Citation6,Citation7 To assess osteopenia/osteoporosis, a DXA scan gives the bone mineral density (BMD) and the “T-score” by regions of the body (eg, spine and femoral sites), allowing the clinician or researcher to diagnose the osteoporosis status and to estimate the patient’s risk of bone fracture.Citation6,Citation7 However, it is also important to note that BMD presents only the proxy for the estimates of fracture risk. An important component of bone health is bone quality (bone turnover, geometry and microarchitecture), which cannot be measured directly or in vivo, and thus it is substituted by measuring BMD.Citation8
The DXA scan also yields the analysis of lean and fat mass, both for total body and specific regions (eg, abdominal and appendicular). A number of researchers have used appendicular lean mass (arms and legs) to assess sarcopenia and sarcopenic obesity.Citation9–Citation11 The ability of DXA to also assess percent of total or regional body fat is useful in assessing the accumulation of fat in more dangerous regions such as the abdomen, as opposed to in the lower extremities such as the thighs and hips.Citation7 The MRI technology provides much more precise measurements of muscle alone (rather than lean mass as with DXA),Citation12 and it also goes a step further by allowing the researcher to assess the fat infiltration into bone marrow and muscle, enabling more adequate diagnosis of osteopenic obesity and/or sarcopenic obesity.Citation13,Citation14 However, this technology is very costly and rarely available for wider use.
Based on the abovementioned information, a recent analysisCitation11 assessed bone loss via DXA measurements using a T-score of L1–L4 and/or total femur or femoral neck <−1.0; sarcopenia assessed via appendicular lean mass measured by DXA, and obesity based on percent body fat (≥32%).Citation15 Moreover, the combination of different serum biomarkers specific for each tissue, such as sclerostin, skeletal muscle-specific troponin T (sTnT), leptin and adiponectin, could be used to further diagnose this syndrome.Citation16 However, the first and easiest tests would be to conduct the physical performance assessment, including handgrip strength, one-leg stance, gait speed and sit-to-stand chair test, as proposed recently.Citation2 Each of these measures has a specific cut off level for older women and men against which a certain impairment can be detected and a patient can then be referred for further evaluation to include analysis of serum biomarkers or body composition evaluation or both.
Despite the advanced technology, the precise detection of adipose tissue, either in the whole body or that infiltrated in bone marrow and muscle, still presents an obstacle for accurate assessment of body composition. Since adipose tissue has such a strong influence on bone and muscle, the following section gives more insight into those mechanisms.
Effect of adiposity on bone and muscle
Obesity and osteoporosis are still sometimes considered as mutually exclusive. Obesity (typically manifested as a higher weight) has been correlated with greater bone mass, bone strength and even bone quality over the life span, mostly as a result of increased mechanical loading.Citation17,Citation18 Mechanical loading stimulates bone formation by decreasing osteoblast apoptosis and also by increasing proliferation and differentiation of osteoblasts and osteocytes.Citation19 In addition to providing added mechanical loading, obesity stimulates higher extraglandular estrogenCitation20 and leptin secretion, both generally believed to preserve bone mass, decreasing susceptibility to fracture.Citation21
However, besides these metabolic and physiological changes, obese individuals may present with a higher risk of falls than nonobese adults and a subsequent higher fracture risk. Higher weight/fat tissue contributes to greater force in the course of a fall, possibly aggravating fracture risks and outcomes.Citation18,Citation19 While traditionally adipose tissue was considered primarily a site for energy storage, it is now regarded as an active endocrine organ involved in the secretion of many cytokines (adipokines), including tumor necrosis factor-alpha (TNF-α), interleukin (IL) and C-reactive protein (CRP),Citation3,Citation22 as well as leptin and adiponectin.Citation23 Excessive adiposity creates a type of pro-inflammatory state, which appears to favor fat accrual at the expense of bone and muscle and suppression of osteoblastogenesis and myogenesis. The hypothesized mechanism is that inflammation and increased systemic adipokine signaling force mesenchymal stem cells into the adipocyte lineage, resulting in higher adipogenesis, and declined osteoblastogenesis and myogenesis, ultimately resulting in fatty bones and muscle.Citation1,Citation24–Citation26
The inflammatory cytokines TNF-α and IL-1 activate osteoclasts, while IL-6 (also known as bone-resorbing factor) stimulates osteoclastogenesis.Citation3,Citation27,Citation28 Leptin and adiponectin are both inflammatory modulating adipokines.Citation23 Serum leptin is higher in overweight/obese individuals and promotes inflammationCitation23,Citation29 while adiponectin, the anti-inflammatory cytokine, is lower.Citation23,Citation30 These findings suggest that osteoclastogenesis and bone resorption are increased in response to increased inflammatory signals in obesity, second to a state of low-grade chronic inflammation, again perpetuated by obesity.Citation3 In addition to acting on a cellular level, increased adiposity may also compromise both bone and muscle mass, strength and quality on a physiological level.Citation31 There is an increased fat infiltration of bone and muscle in older adults, especially in the presence of obesity, which may further weaken and damage bone and muscle tissues. The relationship between obesity and osteoporosis, therefore, is a U-shaped curve, so that both underweight older adults and those with excessive body fat may be at risk. There appears to be a fine line at which adiposity stops being beneficial for bone and starts having adverse effects. In a cross-sectional study conducted in 471 healthy women in 2014, percent body fat higher than 33% was negatively correlated with BMD of several skeletal sites.Citation32 Although obesity has a role in malnutrition as a mediator of the effect on both osteoporosis and sarcopenia,Citation33 it may not always be a protective factor against osteoporosis or sarcopenia, especially in older women.Citation1,Citation32,Citation34
Impact
The increased risk of falls and fractures is probably the greatest concern for the osteosarcopenic obese population.Citation11,Citation35 Fall-related injuries are one of the major causes of mortality and morbidity among the elderly. These injuries could have a significant impact on health-related costs and quality of life.Citation36 The cost of treating osteoporosis and subsequent bone fractures has been estimated to be $19 billion annually.Citation37 Aging accompanied by a sedentary lifestyle leads to muscle wasting, sarcopenia and reduced muscular strength, thereby impacting physical function and the ability to live independently.Citation38 In 2014, one third of fall-related deaths were attributable to low BMD as well as muscle loss.Citation36 The estimated economic costs associated with sarcopenia were $18.5 billion in the US in 2000. It is estimated that a mere 10% reduction in the prevalence of sarcopenia would reduce health care costs by ~$1.1 billion per year.Citation39 Sarcopenia is associated with other complications prevalent in the elderly such as anorexia, frailty, osteoporosis, obesity and falls.Citation40,Citation41
The economic impact of the third component of OSO, overweight/obesity, is especially manifested in health care costs and long-term loss of productivity.Citation42,Citation43 The annual medical cost for an obese individual is on average $1,429 higher than that of a normal-weight healthy individual. The recent rise in the prevalence of obesity is associated with comorbidities such as type II diabetes mellitus, hypertension, hyperlipidemia, cardiovascular disease, stroke, asthma, obstructive sleep apnea, osteoarthritis, renal failure, cancer and others.Citation44 Aside from all these complications, obesity has been associated with a 6–20-year decrease in life expectancy.Citation45
While it is difficult to absolutely separate out single conditions/diseases, the impact of bone loss, muscle loss and excess adiposity, individually and combined, on comorbidities is clear. In addition, all are independently associated with significantly greater direct health care costs (insurance companies and government); however, the indirect (eg, work days lost, impact on family caregivers) impact of these conditions/diseases has not been evaluated.Citation46,Citation47 Thus, the combined condition of OSO could be associated with greater direct and indirect health care costs. Preventing and providing the appropriate treatment for OSO may reduce this economic burden and improve the quality of life of millions of people.
Prevalence
Currently, there are no estimates for the number/percentage of people suffering from the combined condition of the OSO syndrome, because the syndrome itself is a newly identified one and the diagnostic criteria are just being developed, as described earlier.Citation1,Citation2 However, the statistics on its components is available. For example, regarding the bone health, at least 54 million Americans currently have osteopenia and/or osteoporosis, and one in two American women will experience a bone fracture.Citation37,Citation48 Additionally, ∼5%–13% of adults >65 years old and ∼50% of adults >80 years old have sarcopenia.Citation49,Citation50 Ironically, hip or any other osteoporotic fracture accelerates the onset of sarcopenia in older adults; and sarcopenia, which impairs overall physical function, increases the risk of falls and fractures;Citation11,Citation49 thus, these two conditions feed perpetually into each other. Obesity, once believed to be protective of bone and muscle mass, is increasingly linked to deterioration in bone and muscle, especially with aging,Citation1,Citation51,Citation52 although, a recent study suggested the existence of OSO syndrome in a younger-age overweight adult, causing the changes in body composition similar to those seen in elderly populations.Citation53
One component of OSO, the osteopenic obesity,Citation1 a combined condition of bone loss and increased/redistributed body fat, may accelerate physical decline. Osteoblasts and adipocytes share common mesenchymal stem cell lineages. In the aged bone microenvironment where low-grade chronic inflammation persists, there is an increase in adipogenesis and suppression of osteoblastogenesis.Citation1,Citation24–Citation26 In our previous analysis, osteopenic obese women had significantly lower physical performance (such as normal walking speed) than obese-only women (those without significant bone loss or muscle loss), suggesting that bone plays an important role in functional performance.Citation11
Sarcopenic obesity, like osteopenic obesity, was once overlooked, due to the fact that overweight/obese individuals have greater overall mass, including muscle mass, thus it was believed that they were protected from age-related loss of muscle mass, strength and even mobility.Citation51 However, new findings show that the greater amount of lean mass (as a result of overall greater body weight) may not be adequate for an overweight/obese older adult to maintain overall function.Citation1,Citation9,Citation51 Sarcopenic obesity is the result of increased fat mass and fat infiltration into muscle, leading to lower muscle mass, quality and functionality and possibly increased frailty.Citation11,Citation54 However, increased percent body fat, especially when combined with decreased lean mass with age, is particularly deleterious for bone in women.Citation52,Citation54 Therefore, older adults with osteosarcopenic obesity have significantly higher risk of mobility deterioration, which is reflected in weaker grip strength, slower walking speed and poorer balance than older women presenting with obesity only, as shown recently.Citation11,Citation34 Impaired functional performance will lead to increased incidence for falls and subsequent fractures. Therefore, effective preventative measures to delay or even reverse OSO are highly warranted.
The increasing rise in obesity is well known,Citation55–Citation57 and it will not be discussed further in this review. However, an important point to note again is the age-related, or some other chronic condition-related, infiltration of fat into bone marrow and muscle, probably replacing the bone and muscle cells and impairing the function of each tissue. Therefore, it is important to focus not only on obesity as determined by conventional measures (BMI, percent of body fat) but also on the “hidden fat”, although the latter one might not be easy to detect.
Regarding the prevalence of OSO, there are some estimates derived from a few preliminary studies. A post hoc analysis conducted in ∼500 overweight/obese women across a wide age range revealed that 25% had osteosarcopenic obesity.Citation58 However, another study conducted in overweight/obese postmenopausal women estimated that a more conservative 12% of the women could be diagnosed with OSO.Citation11 Surprisingly, the osteosarcopenic obesity phenotype was recently identified in overweight/obese young (18–21 years) women and men. The study was conducted in over 2,500 people, and those who were overweight/obese showed unfavorable body composition and higher pro-inflammatory markers, compared to their normal-weight counterparts.Citation53 A recent pilot study conducted in older women (ages 65+) found ∼18% of participants presenting with OSO syndrome (unpublished data; doctoral dissertations in progress).Citation16,Citation59 In all these studies (except for one in younger populationCitation53), sarcopenic obesity was identified by comparing appendicular lean mass with fat mass (measured by DXA) in a linear regression model,Citation9 and osteopenia/osteoporosis was identified with T-scores <−1 for lumbar spine and/or total femur or femoral neck.Citation60
Management
Although chronic diseases, drug therapy, genetic predisposition and environmental factors are the major determinants in the etiology of OSO, lifestyle factors such as dietary patterns and physical activity are important as well. The latter two play a substantial role in metabolic homeostasis, determining to what extent an individual is able to preserve bone mass, muscle mass and overall function, while still preserving an optimal body weight or reducing obesity with age.Citation61,Citation62
Nutrition
Although American adults consume more food and total energy than people of many other cultures worldwide, evidence points to an increased malnutrition risk with age and a link between the so-called “Western diet” and development of some chronic diseases, including bone, muscle and fat tissue disorders.Citation3 Some of the reasons why older adults in the US are potentially at nutritional risk include increased consumption of high-energy and low-nutrient dense types of food, inadequate dietary fiber consumption and decreased ability to absorb or utilize some essential nutrients.Citation61–Citation63 The Western diet being heavily based on processed food provides an increased amount of energy but decreased amount of many essential nutrients. Over time, this may promote the metabolic deregulation of major systems in the body, leading to bone loss, muscle loss and increased adiposity, as well as increased insulin resistance and low-grade chronic inflammation.Citation3 A typically low dietary fiber intake in older Americans is associated with insulin resistance and increased inflammation, especially in the obese.Citation64 The Western diet is also characterized by a high ratio of omega-6 to omega-3 polyunsaturated fatty acids, which contributes to low-grade chronic inflammation and other unfavorable physiological outcomes.Citation3,Citation61,Citation62 Besides the relatively unwholesome diet, older adults also often consume less nutrients secondary to decreased appetite, side effects from medications, dementia or a desire for weight loss. Particularly affected nutrients are protein, calcium, magnesium and vitamin D, all needed to maintain and build bone and muscle.Citation65 Additionally, absorption and utilization of most vitamins and minerals are also decreased with aging.Citation66 depicts the nutritional recommendations for bone and muscle health and reduction/maintenance of body weight.
Table 1 Nutritional and physical activity recommendations for bone and muscle health and reduction/maintenance of body weightTable Footnote*
The important role of calcium and vitamin D in bone health has been thoroughly reported previously. Likewise, the intake of energy, protein and calcium has been shown to be independently related to BMD in several skeletal sites.Citation67 Low-calcium diets could increase the circulating 1,25-dihydroxyvitamin D (calcitriol), which then stimulates adipogenesis via a specific-membrane vitamin D receptor.Citation68 Insufficient energy, and especially protein intake, can also increase muscle wasting.Citation69 Anorexia of aging and the change in gastrointestinal hormones deprive the skeletal muscles of amino acids required for protein synthesis, thereby causing protein degradation.Citation69,Citation70 The current recommended dietary allowance (RDA) for protein is 0.8 g/kg/d for adults. However, nitrogen balance studies suggest that older adults need to consume a higher amount of protein (1.4–1.6 g/kg/d).Citation71–Citation73 In a recently published review, protein intake of 1.0–1.3 g/kg/d has been recommended to reduce muscle loss in elderly populations.Citation74 Inadequate protein intake in aging adults combined with physical inactivity may further exacerbate the decline in muscle protein synthesis associated with aging. For example, in a 14-week study conducted in 2001, men and women aged 54–78 years were provided with eucaloric diets of 0.8 g/kg protein per day. A 21% reduction in nitrogen excretion was reported and was significantly correlated (r=0.83) with a decrease in thigh muscle cross-sectional area.Citation75 A negative nitrogen balance, with a simultaneous decrease in muscle mass, indicates compromised muscle protein synthesis in order to conserve total body protein (all in response to lower protein intake). These findings indicate that the RDA for protein (0.8 g/kg/d) may not be adequate for the maintenance of skeletal muscle in aging adults. However, it needs to be noted that with an adequate consumption of energy from fat and carbohydrate, less protein will be utilized for energy needs, and thus it will be spared.Citation49 A recent analysis of National Health and Nutrition Examination Survey (NHANES) data shows that energy imbalance, and lower protein intakes, in addition to excess of simple carbohydrates, and low long-chain polyunsaturated fatty acid intakes may contribute to OSO.Citation61
Carbohydrate intake is controversial regarding bone health. A randomized control crossover trial showed that there is no significant difference in serum osteocalcin (marker of bone formation), carboxyl- (C–) terminal cross-linking telopeptides of type I collagen (marker of bone turnover), bone-specific alkaline phosphatase (marker of bone formation) and urinary (N–) terminal cross-linking telopeptides of type I collagen (marker of bone turnover) between a control and a low carbohydrate diet.Citation76 Regarding polyunsaturated fatty acids, in addition to the beneficial effects of omega-3 fatty acids on numerous health outcomes, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), specifically, were shown to promote bone formation and reduce the negative effects of adiposity on bone.Citation77 The combination of low protein, high simple carbohydrates, deficiencies of calcium, magnesium and potassium and excess of phosphorus, sodium and iron may be associated with lower bone mass, sarcopenia and obesity and, therefore, OSO syndrome.Citation61,Citation62 Overall, the nutrient composition of the Western diet, distribution and amounts, for both macro and micronutrients may not promote healthy aging and may be contributing to the development of OSO syndrome.
Physical activity
In general, physical activity is needed for maintenance and improvement of all components of body composition, as well as the physiological and mental health in people of all ages.Citation78 Specifically for the OSO syndrome, physical activity, even in the form of low intensity or habitual activity, is needed to maintain or improve BMD,Citation67,Citation79,Citation80 maintain muscle strength and quality, improve balance and reduce adiposity and inflammation, with aging.Citation80,Citation81 Different studies have revealed that the rate at which BMD is lost can be slowed by weight-bearing physical activity, even in old age.Citation82,Citation83 Therefore, specific means of physical activity have been prescribed for the prevention and treatment of osteoporosis and overall bone health. A comprehensive exercise program for older adults should include aerobic, strength, flexibility and balance training.Citation84 All the four components are crucial for the maintenance of body composition and healthy aging. A comprehensive exercise program serves to reduce the risk of falls, increase functional ability and improve the quality of life among older individuals.Citation85,Citation86 lists the recommendations of physical activity modes for bone and muscle health and reduction/maintenance of body weight.
With society’s emphasis on weight loss, studies have shown that weight loss also results in the reduction of both bone and muscle mass, which is relevant for postmenopausal women. Several studies have shown decreased BMD in overweight or obese women both during and after weight loss.Citation87–Citation91 Either intentional or unintentional weight loss is accompanied by bone loss and thus can raise the risk of fractures in older women.Citation23,Citation90 It has been shown that diet-induced weight loss reduced bone mass due to decreased mechanical loading on the skeleton.Citation92 Regarding preservation of lean mass (muscle), recent findings show that resistance exercise increases lean mass most effectively, but the best exercise for older adults is what they are able to do, as reviewed recently.Citation80 Besides improving bone remodeling, mechanical loading can also positively affect myogenesis. Strength training has been shown to inhibit muscle protein breakdown and may help to maintain and increase muscle mass.Citation93,Citation94 Reducing adiposity through both aerobic and strength training is substantial in attenuating the inflammatory environment and thereby reducing bone and muscle loss and inhibiting the progression of OSO syndrome.Citation95,Citation96
It is important to consider that physical activity or exercise in middle-aged to older adults may be more beneficial for reducing the rate of bone or muscle loss rather than a significant increase in each.Citation97 Exercise programs that have included brisk walking, stair climbing and descending, jogging, rowing and weight lifting can be effective in attenuating bone loss in older women.Citation97,Citation98 Aside from some medium to high-impact activities, habitual and low-impact physical activities including heavy housework, gardening, do-it-yourself activities, recreational activities and walking have been shown to be beneficial for bone in postmenopausal women.Citation67 Any period of immobility and immobilization should be avoided as much as possible among elderly. When an individual is sick or injured, even brief daily walking or any type of weight-bearing movements may help to protect BMD and muscle functioning. Other alternative exercises such as tai chi, yoga and pilates, as well as whole body vibration, could be used to support favorable body composition and prevent bone loss. It has also been shown that these types of exercise are associated with an increase in quality of life of older individuals.Citation80 Overall, older adults may require special considerations such as tailoring progression of exercise intensity and beginning at a lower intensity. Furthermore, the low-impact physical activity and alternative exercises should be the focus for older individuals and those with higher risk of fall and injuries.Citation99,Citation100
Conclusion
OSO syndrome is a multifactorial condition of age-related changes in body composition including bone and muscle loss combined with increased or redistributed adiposity. This complex condition is not caused by one single component, but by an amalgamation of elements, such as poor nutrition, lack of physical activity, low-grade chronic inflammation, and aggravated in the milieu of some chronic diseases, as well as the metabolic consequences of all these factors over time. Treatment for the OSO syndrome or its management requires the combination of healthy/optimal nutrition and exercise training or different modes of physical activity to attenuate the progression or even to prevent it (). For the best prevention, efforts should be made to achieve peak bone mass before the age of 30 years, gain/maintain muscle mass at all ages and maintain a healthy body weight. In addition, due to its complex etiology and treatment requirements, body composition measures may be helpful. As discussed in this review, nutritional modifications to prevent and/or alleviate the OSO syndrome include adequate protein, fiber and energy intake, adequate calcium, magnesium and vitamin D and consumptions of food containing omega-3 polyunsaturated fatty acids (flaxseed oil, fish oil, walnuts and soybeans), the latter to avoid low-grade chronic inflammation. Equally important would be the treatment of the age-related anorexia and diminished absorption and utilization of vitamins and minerals. In addition, physical activity, including strength training and aerobic exercise, supports the maintenance of bone mass and skeletal muscle and thus attenuates osteopenia/osteoporosis as well as sarcopenia. Both aerobic exercise and strength training stimulate lipolysis, and thereby contribute to the reduction of obesity. As discussed in this review, habitual daily activity and some alternative modes of exercise may be more appropriate for older adults and thus play a crucial role in preventing bone and muscle loss and maintaining optimal weight. In conclusion, nutritional interventions, in combination with physical activity and exercise training, are essential for the prevention and management of OSO syndrome.
Disclosure
The authors report no conflicts of interest in this work.
References
- IlichJZKellyOJInglisJEPantonLBDuqueGOrmsbeeMJInterrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levelsAgeing Res Rev201415516024632496
- IlichJZKellyOJInglisJEOsteosarcopenic obesity syndrome: what is it and how can it be identified and diagnosed?Curr Gerontol Geriatr Res2016201617
- IlichJZKellyOJKimYSpicerMTLow-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosisArh Hig Rada Toksikol201465213914824945416
- InglisJEIlichJZThe microbiome and osteosarcopenic obesity in older individuals in long-term care facilitiesCurr Osteoporos Rep201513535836226272433
- Administration for Community Living [webpage on the Internet]Aging Statistics Available from: http://www.aoa.acl.gov/Aging_Statistics/index.aspxAccessed January 1, 2016
- NIH Consensus StatementOsteoporosis Prevention, Diagnosis, and Therapy2000171145 Available from: https://consensus.nih.gov/2000/2000Osteoporosis111PDF.pdfAccessed November 29, 2016.
- KimKYunSHJangMJOhKWBody fat percentile curves for Korean children and adolescents: a data from the Korea National Health and Nutrition Examination Survey 2009–2010J Korean Med Sci201328344323487528
- BrownbillRAIlichJZMeasuring body composition in overweight individuals by dual energy x-ray absorptiometryBMC Med Imaging200551115748279
- NewmanABKupelianVVisserMHealth ABC Study InvestigatorsSarcopenia: alternative definitions and associations with lower extremity functionJ Am Geriatr Soc200351111602160914687390
- BaumgartnerRNWatersDLGallagherDMorleyJEGarryPJPredictors of skeletal muscle mass in elderly men and womenMech Ageing Dev1999107212313610220041
- IlichJZInglisJEKellyOJMcGeeDLOsteosarcopenic obesity is associated with reduced handgrip strength, walking abilities, and balance in postmenopausal womenOsteoporos Int201526112587259526025288
- PahorMManiniTCesariMSarcopenia: clinical evaluation, biological markers and other evaluation toolsJ Nutr Health Aging200913872472819657557
- HanrahanCJShahLMMRI of spinal bone marrow: part 2, T1-weighted imaging-based differential diagnosisAJR Am J Roentgenol201119761309132122109284
- LiuYTangGTangRPengYLiWAssessment of bone marrow changes in postmenopausal women with varying bone densities: magnetic resonance spectroscopy and diffusion magnetic resonance imagingChin Med J (Engl)2010123121524152720819505
- Ace FitAce Fitness [webpage on the Internet]What are the guidelines for percentage of body fat loss?2009 Available from: https://www.acefitness.org/acefit/healthy-living-article/60/112/what-are-the-guidelines-for-percentage-of-body-fatAccessed January 1, 2016
- JafariNasabianPAnalyzing Bone, Muscle and Adipose Tissue Biomarkers to Identify Osteosarcopenic Obesity Syndrome in Older Women [dissertation]In press2017
- CastroJPJosephLAShinJJDifferential effect of obesity on bone mineral density in White, Hispanic and African American women: a cross sectional studyNutr Metab (Lond)200521915817133
- TravisonTGAraujoABEscheGRMcKinlayJBThe relationship between body composition and bone mineral content: threshold effects in a racially and ethnically diverse group of menOsteoporos Int2008191293817660933
- CaoJJPickloMJInvoluntary wheel running improves but does not fully reverse the deterioration of bone structure of obese rats despite decreasing adiposityCalcif Tissue Int201597214515525903229
- DouchiTYamamotoSOkiTDifference in the effect of adiposity on bone density between pre- and postmenopausal womenMaturitas200034326126610717492
- BergRMWallaschofskiHNauckMPositive association between adipose tissue and bone stiffnessCalcif Tissue Int2015971404925929703
- WellenKEHotamisligilGSInflammation, stress, and diabetesJ Clin Invest200511551111111915864338
- JafariNasabianPChiY-CIlichJZAdipokines as mediators of bone density in overweight/obese postmenopausal women after 6-month weight loss programFASEB J2015291738.4
- DeshpandeSJamesAWBloughJReconciling the effects of inflammatory cytokines on mesenchymal cell osteogenic differentiationJ Surg Res2013185127828523972621
- GimbleJMZvonicSFloydZEKassemMNuttallMEPlaying with bone and fatJ Cell Biochem200698225126616479589
- RosenCJBouxseinMLMechanisms of disease: is osteoporosis the obesity of bone?Nat Clin Pract Rheumatol200621354316932650
- DoddsRAMerryKLittlewoodAGowenMExpression of mRNA for IL1 beta, IL6 and TGF beta 1 in developing human bone and cartilageJ Histochem Cytochem19944267337448189035
- KrisherTBar-ShavitZRegulation of osteoclastogenesis by integrated signals from toll-like receptorsJ Cell Biochem2014115122146215425079212
- CanavanBSalemROSchurginSEffects of physiological leptin administration on markers of inflammation, platelet activation, and platelet aggregation during caloric deprivationJ Clin Endocrinol Metab200590105779578516076944
- OuchiNKiharaSAritaYAdiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathwayCirculation2000102111296130110982546
- ScottDDalyRMSandersKMEbelingPRFall and fracture risk in sarcopenia and dynapenia with and without obesity: the role of lifestyle interventionsCurr Osteoporos Rep201513423524426040576
- LiuP-YIlichJZBrummel-SmithKGhoshSNew insight into fat, muscle and bone relationship in women: determining the threshold at which body fat assumes negative relationship with bone mineral densityInt J Prev Med20145111452146325538842
- RondanelliMGuidoDOpizziAFalivaMAPernaSGrassiMA path model of sarcopenia on bone mass loss in elderly subjectsJ Nutr Health Aging2014181152124402383
- ShinHLiuP-YPantonLBIlichJZPhysical performance in relation to body composition and bone mineral density in healthy, overweight, and obese postmenopausal womenJ Geriatr Phys Ther201437171623685966
- Hita-ContrerasFMartínez-AmatACruz-DíazDPérez-LópezFROsteosarcopenic obesity and fall prevention strategiesMaturitas201580212613225533145
- Sànchez-RieraLCarnahanEVosTThe global burden attributable to low bone mineral densityAnn Rheum Dis20147391635164524692584
- National Osteoporosis FoundationNational Osteoporosis Foundation Prevalence Report2014 Available from: https://www.nof.org/about-us/nof-background/Accessed February 9, 2014
- RosenbergIHSarcopenia: origins and clinical relevanceJ Nutr19971275 suppl990S991S9164280
- JanssenIBaumgartnerRNRossRRosenbergIHRoubenoffRSkeletal muscle cutpoints associated with elevated physical disability risk in older men and womenAm J Epidemiol2004159441342114769646
- RollandYAbellan van KanGGillette-GuyonnetSVellasBCachexia versus sarcopeniaCurr Opin Clin Nutr Metab Care2011141152121076295
- Cruz-JentoftAJBaeyensJPBauerJMEuropean Working Group on Sarcopenia in Older PeopleSarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older PeopleAge Ageing201039441242320392703
- ColditzGAEconomic costs of obesity and inactivityMed Sci Sports Exerc19993111 supplS663S66710593542
- CawleyJMeyerhoeferCThe medical care costs of obesity: an instrumental variables approachJ Health Econ201231121923022094013
- ReillyJJKellyJLong-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic reviewInt J Obes (Lond)201135789189820975725
- LeBlancEO’ConnorEWhitlockEPPatnodeCKapkaTScreening for and management of obesity and overweight in adultsEvid Synth2011 11-05159-EF-1
- SpecchiaMLVenezianoMACadedduCEconomic impact of adult obesity on health systems: a systematic reviewEur J Public Health201525225526225320051
- FeinbergLReinhardSCHouserAChoulaRValuing the Invaluable: 2011 Update – The Growing Contributions and Costs of Family CaregivingAARP Public Policy Inst Available from: http://assets.aarp.org/rgcenter/ppi/ltc/i51-caregiving.pdfAccessed November 29, 2016
- Osteoporosis/Bone Health in Adults as a National Public Health Priority Available from: http://newsroom.aaos.org/media-resources/Press-releases/american-academy-of-orthopaedic-surgeons-releases-new-guidelines-on-hip-fractures-in-older-adults-acl-injuries-and-infant-dysplasia-of-the-hip.htmAccessed January 1, 2016
- MorleyJEAnkerSDvon HaehlingSPrevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology-update 2014J Cachexia Sarcopenia Muscle20145425325925425503
- DizJBMde QueirozBZTavaresLBPrevalence of sarcopenia among the elderly: findings from broad cross-sectional studies in a range of countriesRev Bras Geriatr e Gerontol2015183665678
- DomicianoDSFigueiredoCPLopesJBDiscriminating sarcopenia in community-dwelling older women with high frequency of overweight/obesity: the São Paulo Ageing & Health Study (SPAH)Osteoporos Int201324259560322588184
- ZhuKHunterMJamesALimEMCookeBRWalshJPDiscordance between fat mass index and body mass index is associated with reduced bone mineral density in women but not in men: the Busselton Healthy Ageing StudyOsteoporos Int Epub2016729
- StefanakiCPeppaMBoschieroDChrousosGPHealthy overweight/obese youth: early osteosarcopenic obesity featuresEur J Clin Invest201646976777827434725
- GoisserSKemmlerWPorzelSSarcopenic obesity and complex interventions with nutrition and exercise in community-dwelling older persons – a narrative reviewClin Interv Aging2015101267128226346071
- OgdenCLCarrollMDKitBKFlegalKMPrevalence of obesity among adults: United States, 2011–2012NCHS Data Brief201318 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24152742Accessed December 16, 2016
- FlegalKMCarrollMDKitBKOgdenCLPrevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010JAMA2012307549149722253363
- Center for Disease Control and Prevention [webpage on the Internet]Prevalence of obesity in the United States, 2009–2010 Available from: http://www.cdc.gov/nchs/data/databriefs/db82.htm#Ref6Accessed January 22, 2016
- InglisJEPantonLBOrmsbeeMJKellyOJIlichJZ webpage on the InternetDefining osteosarcopenic obesity and identifying its prevalence in women across the age spanJ Bone Miner Res2013 Available from: http://www.asbmr.org/education/AbstractDetail?aid=da7d06cc-1551-4abf-8445-51dc6e53bcf7Accessed January 11, 2017
- InglisJEIdentifying Osteosarcopenic Obesity in a Group of Older Women [Dissertation]In press2017
- KanisJAJohnellOOdenADawsonADe LaetCJonssonBTen year probabilities of osteoporotic fractures according to BMD and diagnostic thresholdsOsteoporos Int2001121298999511846333
- KellyOJGilmanJCKimYIlichJZMacronutrient intake and distribution in the etiology, prevention and treatment of osteosarcopenic obesityCurr Aging Sci Epub201659
- KellyOJGilmanJCKimYIlichJZMicronutrient intake in the etiology, prevention and treatment of osteosarcopenic obesityCurr Aging Sci Epub201659
- InglisJEJafariNasabianPGilmanJCKellyOJIlichJZPossible nutritional etiology of osteosarcopenic obesity syndromeFASEB J2016301156.8
- LattimerJMHaubMDEffects of dietary fiber and its components on metabolic healthNutrients20102121266128922254008
- PriceCTLangfordJRLiporaceFAEssential nutrients for bone health and a review of their availability in the average North American DietOpen Orthop J2012614314922523525
- PrayLBoonCAnn MillerEPillsburyL webpage on the InternetProviding Healthy and Safe Foods as We Age: Workshop SummaryInstitude Med Natl Acad2010 Available from: http://www.nap.edu/catalog/12967.htmlAccessed October 16, 2016
- IlichJZBrownbillRAHabitual and low-impact activities are associated with better bone outcomes and lower body fat in older womenCalcif Tissue Int200883426027118815824
- ZemelMBRichardsJMilsteadACampbellPEffects of calcium and dairy on body composition and weight loss in African-American adultsObes Res20051371218122516076991
- MorleyJEAnorexia, sarcopenia, and agingNutrition2001177–866066311448592
- BalesCWRitchieCSSarcopenia, weight loss, and nutritional frailty in the elderlyAnnu Rev Nutr20022230932312055348
- CampbellWWCrimMCDallalGEYoungVREvansWJIncreased protein requirements in elderly people: new data and retrospective reassessmentsAm J Clin Nutr19946045015098092084
- Churchward-VenneTABreenLPhillipsSMAlterations in human muscle protein metabolism with aging: protein and exercise as countermeasures to offset sarcopeniaBiofactors201440219920524105883
- BreenLPhillipsSMInteractions between exercise and nutrition to prevent muscle waste during ageingBr J Clin Pharmacol201375370871522957963
- NowsonCO’ConnellSProtein requirements and recommendations for older people: a ReviewNutrients2015786874689926287239
- CampbellWWTrappeTAWolfeRREvansWJThe recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscleJ Gerontol A Biol Sci Med Sci2001566M373M38011382798
- FitzmauriceDDoyleLThe effect of a low-carbohydrate diet on biomarkers of bone health in pre- and post-menopausal females: a randomized control crossover trialProc Nutr Soc201170OCE6E355
- KellyOJGilmanJCKimYIlichJZLong-chain polyunsaturated fatty acids may mutually benefit both obesity and osteoporosisNutr Res201333752153323827126
- BoothFWGordonSECarlsonCJHamiltonMTWaging war on modern chronic diseases: primary prevention through exercise biologyJ Appl Physiol200088277478710658050
- HughesVAFronteraWRWoodMLongitudinal muscle strength changes in older adults: influence of muscle mass, physical activity, and healthJ Gerontol A Biol Sci Med Sci2001565B209B21711320101
- KellyOJGilmanJCCan unconventional exercise be helpful in the treatment, management and prevention of osteosarcopenic obesity?Curr Aging Sci Epub201659
- DeckxNWensINuytsAH12 weeks of combined endurance and resistance training reduces innate markers of inflammation in a randomized controlled clinical trial in patients with multiple sclerosisMediators Inflamm20162016678927626903712
- WolffIvan CroonenborgJJKemperHCKostensePJTwiskJWThe effect of exercise training programs on bone mass: a meta-analysis of published controlled trials in pre- and postmenopausal womenOsteoporos Int199991112
- LanyonLEFunctional strain as a determinant for bone remodelingCalcif Tissue Int198436suppl 1S56S616430523
- GarberCEBlissmerBDeschenesMRAmerican College of Sports MedicineQuantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exerciseMed Sci Sports Exerc20114371334135921694556
- GillespieLDRobertsonMCGillespieWJInterventions for preventing falls in older people living in the communityCochrane Database Syst Rev20122CD007146
- FrancoMRPereiraLSFerreiraPHExercise interventions for preventing falls in older people living in the communityBr J Sports Med2014481086786823314888
- ShapsesSASukumarDBone metabolism in obesity and weight lossAnnu Rev Nutr20123228730922809104
- ChaoDEspelandMAFarmerDEffect of voluntary weight loss on bone mineral density in older overweight womenJ Am Geriatr Soc200048775375910894313
- CompstonJELaskeyMACroucherPICoxonAKreitzmanSEffect of diet-induced weight loss on total body bone massClin Sci (Lond)19928244294321315653
- EnsrudKEEwingSKStoneKLStudy of Osteoporotic Fractures Research GroupIntentional and unintentional weight loss increase bone loss and hip fracture risk in older womenJ Am Geriatr Soc200351121740174714687352
- PritchardJENowsonCAWarkJDBone loss accompanying diet-induced or exercise-induced weight loss: a randomised controlled studyInt J Obes Relat Metab Disord19962065135208782726
- JensenLBKollerupGQuaadeFSørensenOHBone minerals changes in obese women during a moderate weight loss with and without calcium supplementationJ Bone Miner Res200116114114711149478
- LittleJPPhillipsSMResistance exercise and nutrition to counteract muscle wastingAppl Physiol Nutr Metab200934581782819935843
- GloverEIPhillipsSMResistance exercise and appropriate nutrition to counteract muscle wasting and promote muscle hypertrophyCurr Opin Clin Nutr Metab Care201013663063420829685
- MengS-JYuL-JOxidative stress, molecular inflammation and sarcopeniaInt J Mol Sci20101141509152620480032
- ChungHYLeeEKChoiYJMolecular inflammation as an underlying mechanism of the aging process and age-related diseasesJ Dent Res201190783084021447699
- KohrtWMBloomfieldSALittleKDNelsonMEYinglingVRAmerican College of Sports MedicineAmerican College of Sports Medicine Position Stand: physical activity and bone healthMed Sci Sports Exerc200436111985199615514517
- KelleyGAKelleyKSTranZVResistance training and bone mineral density in women: a meta-analysis of controlled trialsAm J Phys Med Rehabil2001801657711138958
- KemmlerWvon StengelSAlternative exercise technologies to fight against sarcopenia at old age: a series of studies and reviewJ Aging Res2012201210901322500224
- Choices N [webpage on the Internet]Physical activity guidelines for older adults – Live Well – NHS Choices Available from: http://www.nhs.uk/Livewell/fitness/Pages/physical-activity-guidelines-for-older-adults.aspxAccessed November 29, 2016
- BastinSGambleGDGreyAReidIRCalcium Dietary Supplement Fact SheetBethesda, MDNational Institute of Health, Office of Dietary Supplements2016
- Magnesium Fact Sheet for Health Professionals [webpage on the Internet]National Institute of Health, Office of Dietary Supplements Available from: https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/Accessed December 16, 2016
- National Institute of Health, Office of Dietary Supplements [webpage on the Internet]Vitamin D Fact Sheet for Health Professionals Available from: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/Accessed December 16, 2016
- National Institute on Aging [webpage on the Internet]Falls and Fractures Available from: https://www.nia.nih.gov/health/publication/falls-and-fracturesAccessed December 16, 2016
- AloiaJFCohnSHOstuniJACaneREllisKPrevention of involutional bone loss by exerciseAnn Intern Med1978893356358686549
- PedersenBKMuscle as a secretory organCompr Physiol2013331337136223897689
- RoussetSPatureau MirandPBrandoliniMMartinJ-FBoirieYDaily protein intakes and eating patterns in young and elderly FrenchBr J Nutr20039061107111514641970
- SymonsTBSheffield-MooreMMamerowMMWolfeRRPaddon-JonesDThe anabolic response to resistance exercise and a protein-rich meal is not diminished by ageJ Nutr Health Aging201115537638121528164
- JakicicJMExercise in the treatment of obesityEndocrinol Metab Clin North Am200332496798014711070
- PitsavosCPanagiotakosDWeinemMStefanadisCDiet, exercise and the metabolic syndromeRev Diabet Stud20063311812617487335
- CokerRHWilliamsRHKortebeinPMSullivanDHEvansWJInfluence of exercise intensity on abdominal fat and adiponectin in elderly adultsMetab Syndr Relat Disord20097436336819196080
