Abstract
Background
This study investigated a novel fractional carbon dioxide (CO2) laser for treatment of symptoms associated with vulvovaginal atrophy (VVA) in perimenopausal women.
Methods
The study included 21 perimenopausal women (mean age 45±7 years) treated three times by CO2 laser resurfacing and coagulation of the vaginal canal tissue and mucosal tissue of the introitus. Vaginal health index (VHI) scores were computed by the investigator at baseline and follow-ups. Subjects reported on sexual function, satisfaction, and improvement with treatment. A visual analog scale was used to measure discomfort with treatment.
Results
Vaginal health and subject assessment of vaginal symptoms improved with successive treatments. At 12 weeks following the third treatment, 82% of the patients showed a statistically significant improvement in VHI (P<0.05). Additionally, 81% of subjects reported improvement in sexual gratification, 94% reported improvement in vaginal rejuvenation, and 100% reported satisfaction with treatment. VHI improvement remained significant at 6–8 months after treatments (P<0.01). Most patients (97%) reported no to mild discomfort with treatment. Responses were mild and transient following treatment, with itching being the most commonly reported (20%) side effect.
Conclusion
In this study, fractional CO2 laser treatment was associated with improvement of vaginal health and amelioration of symptoms of VVA, resulting in improved sexual function in perimenopausal women. Treatment time was quick, and there was minimal discomfort associated with treatment. Investigation of clinical outcome in a larger study population is warranted.
Introduction
Although the prevalence varies in early premenopausal to late postmenopausal women, vulvovaginal atrophy (VVA) is considered to be a common and underreported condition, with nearly 50% of postmenopausal women reporting symptoms.Citation1 Self-reported genital symptoms include dryness, irritation, soreness, and associated dyspareunia.Citation1–Citation3 According to the Vulvovaginal Atrophy Terminology Consensus Conference Panel, genitourinary syndrome of menopause (GSM) is a more medically accurate term for VVA and includes genital symptoms, as well as sexual symptoms of lack of lubrication, discomfort or pain, and impaired function and urinary symptoms of urgency, dysuria, and recurrent urinary tract infections.Citation4 Clinical findings include the presence of pale and dry vulvovaginal mucosa with petechiae.
Thinning of the epithelial lining and loss of lubrication during intercourse contribute to dyspareunia and can have a detrimental effect on sexual gratification. As sexual health is an important aspect of overall health that changes over a woman’s lifetime, problems in sexual health may adversely affect quality of life.Citation5 Many women with sexual health concerns are not aware that the changes in genitourinary anatomy and physiology that occur with age can impact sexual functioning. Findings from the Real Women’s Views on Treatment Options for Menopausal Vaginal Changes survey reported that these symptoms affected sexual satisfaction in 59% of women responding to the survey; in nearly one-fourth (23%) of respondents, these symptoms affected general temperament and general life enjoyment.Citation6
Current therapeutic approaches include topical treatments and hormones. The North American Menopause Society (NAMS) updated its position statement in 2013 on the management of symptomatic GSM in postmenopausal women to conclude that non-hormonal therapies provide relief for mild symptoms, while estrogen therapy is the most effective treatment for moderate to severe symptoms.Citation7 However, they further stated that endometrial safety has not been studied in long-term clinical studies, and there are insufficient data to confirm the safety of local estrogen in women with breast cancer. Therefore, NAMS noted that
Choice of therapy depends on the severity of symptoms, the effectiveness and safety of therapy for the individual patient, and patient preference.Citation7
While non-hormonal vaginal moisturizers and lubricants can be safely used for GSM symptoms, they need to be used regularly for optimal effect.Citation1 Vaginal estrogen appears to relieve symptoms more effectively than non-hormonal gels. Systemic estrogen therapy is sometimes used; however, 10%–20% of women may have residual GSM symptoms even while taking systemic estrogen.Citation8 Breast cancer treatment increases the prevalence of GSM symptoms, which negatively correlate with quality of life.Citation9 Local estrogen treatment for this group of women remains controversial. Moreover, many women prefer not to use hormonal therapy due to side effects, such as worsening of the symptoms of urinary incontinence.Citation10
Laser treatment is a novel non-hormonal treatment approach for GSM. The concept behind laser procedures to treat vulvovaginal conditions is to use a wavelength having high water absorption, such as the carbon dioxide (CO2) laser (10,600 nm), to ablate and coagulate vaginal and vulvar tissues.Citation11 The Er:YAG laser also stimulates non-ablative photothermal effects by thermal diffusion to the vaginal walls.Citation12 A wound response is initiated due to the heating and results in tissue remodeling with neoformation of collagen and elastic fibers in atrophic skin.Citation11,Citation12 The muscle tone of the vagina is then restored by tightening the supportive structures of the vulvovaginal complex.Citation13 CO2 laser treatment has previously demonstrated significant improvement in GSM symptoms in postmenopausal women.Citation11,Citation14–Citation16 Fractional CO2 laser application has also been shown to restore the vaginal mucosa structure in postmenopausal, non-estrogenized women.Citation17
In the published trials to date, only postmenopausal women have been studied,Citation11–Citation17 primarily with short-term follow-up of 12 weeks after treatment.Citation11,Citation13–Citation15 As symptoms of VVA can occur at any time in a woman’s life cycle, this study investigated the effects of fractional CO2 laser in perimenopausal women treated by resurfacing and coagulation of the vaginal canal tissues and mucosal tissues of the introitus. Clinical outcome was evaluated at 12 weeks and longer term at 6 months after the final treatment.
Methods
Study design
This prospective study was conducted at HM Montepríncipe University Hospital in Madrid, Spain. Study participants included perimenopausal women presenting to the clinic with irregular menstrual patterns and symptoms of VVA (vaginal dryness, irritation, soreness, or dyspareunia associated with this condition). Study exclusion were discontinuation of menstruation for 12 consecutive months; pregnancy; previous vaginal reconstructive surgery or treatment for vaginal tightening within the past 12 months; acute or recurrent urinary tract infections; active genital infections; undiagnosed vaginal bleeding; and suffering from hormonal imbalance or any serious disease or chronic condition that could interfere with study compliance. The study protocol was approved by the Hospital Ethics Committee, and informed written consent was obtained from study subjects.
Study protocol
Perimenopausal women were treated extravaginally and internally with a fractional CO2 laser (CO2RE Intima; Syneron Candela, Wayland, MA, USA). Treatment of the vaginal canal was performed using the following settings: square pattern and Deep Mode with the internal handpiece, fractional density of 4%–5%, and energy level of 40–55 mJ. The speculum cage was introduced into the introitus, and the handpiece was inserted to the interior edge of the treatment site (up to 11 cm in the vaginal canal). Several drops of baby oil were used for more comfortable insertion into the introitus. The handpiece was positioned with contact to the vaginal wall and pulses were applied at each 1 cm marking and then retracted, until a 4–5 cm depth. The handpiece was rotated 45°–90° and reinserted until 4–8 pulses were applied at each depth.
External treatments were performed with a separate handpiece, using Deep Mode and the hexagon or square pattern. Single passes, without overlapping, were administered at the energy level of 40 mJ and 3%–4% fractional density. Subjects received three treatments at 3- to 4-week intervals. The procedure was performed in the outpatient clinic and did not require analgesia/anesthesia. Patients were recommended to avoid coital sexual activity and tampon use for at least 7 days after treatment.
The primary objective in the study was to evaluate change in vaginal health index (VHI) at 12 weeks after the final treatment. Secondary objectives included change in VHI at 24 weeks after the final treatment and subject assessments of changes in VVA symptoms and sexual gratification.
Data assessments
The VHI, a quantitative assessment of vaginal health, was performed by the investigator to assess changes in vaginal elasticity, fluid volume, vaginal pH level, and epithelial integrity and moisture after treatment and at follow-ups after the final treatment (6, 12, and 24 weeks) compared to baseline. A visual analog scale was used to measure discomfort associated with treatment. A 5-point Likert scale questionnaire was completed by subjects to report on sexual function, satisfaction, and improvement following treatment. Differences between baseline and follow-up VHI scores were analyzed with Wilcoxon signed-rank test for paired data. Statistical significance was set at P<0.05.
Results
The study included 21 perimenopausal women (mean age 45±7 years) treated both internally and externally at three sessions (1 of the 21 subjects was treated just once) with fractional CO2 laser. Patients were assessed following each treatment and at the 12-week follow-up after the final treatment. Sixteen patients returned for a long-term follow-up visit at 6–8 months (24-week follow-up) after the final treatment.
Investigator qualitative VHI assessments
At baseline, the mean VHI score in the perimenopausal study population was 17.7±1.6 (range 15–20). Vaginal health improved significantly (P<0.01, Wilcoxon signed-rank test for single group median) with successive treatments with a mean improvement of 2.2 and 2.1 points in the VHI at the 12-week and 24-week follow-ups after treatment, respectively (). At 12 weeks following the third treatment, 82% of the patients showed a statistically significant increase in the VHI score (P<0.05, Wilcoxon signed-rank test for paired data) with a mean score of 20.0±2.1 (range 17–24). Six patients had a VHI score >20. Improvement remained statistically significant (P<0.01) compared to baseline at the 24-week follow-up with a mean VHI score of 19.7±1.4 (range 18–23).
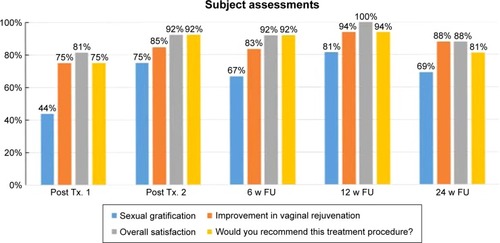
Subjective assessments
Subject assessment of vaginal and sexual symptoms also improved with successive treatments (). At 12 weeks following the third treatment, 81% of subjects reported an improvement in sexual gratification (more friction with a greater number and improved orgasms), and 94% reported an improvement in vaginal rejuvenation (increased vaginal tightening and improvement in dryness and atrophy). All subjects (100%) reported satisfaction with treatment and 94% would recommend the procedure. At 24 weeks after treatment, subjective improvement in vaginal rejuvenation and overall satisfaction remained high at 88%, while sexual gratification decreased to findings similar to those at the 6-week follow-up assessments ().
Safety findings
Treatments did not require analgesia/anesthesia. Mean treatment time, including examination of the area and prep (cleaning the treatment area with a disinfecting solution), was 19±3 minutes. Most patients (97%) reported that both internal and external treatment phases were accompanied with none to mild pain (mean discomfort of 1.6±1.4 and 2.49±1.36 for the internal and external treatments, respectively). Immediate treatment responses were mild and transient, resolving within 1–2 days and included burning sensation (20%), itching (20%), bruising (4%), swelling (4%), twinging sensation (4%), numbness (4%), and purpura (2%). There were no treatment complications, and adverse effects were limited to a 50-year-old patient with a mild urinary infection following her first treatment that resolved completely after a weekly course of oral antibiotics. The patient did not experience a recurrence of the infection or any other adverse symptoms following the two additional treatments.
Discussion
CO2 lasers have long been considered as a precise and predictable treatment modality to rejuvenate photoaged skin by ablation of abnormal tissues with subsequent regeneration and remodeling of collagen and through heat-induced collagen contraction.Citation18,Citation19 Histologic changes induced by CO2 laser pulses in human skin have been studied and compared with tissue contraction of wound healing caused by resurfacing with erbium lasers.Citation19,Citation20 Single-pass CO2 laser treatment versus multiple-pass Er:YAG laser resurfacing produced equivalent thermal injury on immediate postoperative biopsies and subsequent degree of fibroplasia at 3 or 6 months.Citation20 Collagen tightening induced by three passes of CO2 laser persisted at 6 months after the procedure.Citation19 Fractional techniques result in new collagen formation and skin tightening with the added benefit of short-term postoperative erythema and a favorable benefit-risk ratio.Citation21 Fractional CO2 laser resurfacing has also been used to improve genital skin condition and mucosal tissues in females with lichen sclerosus.Citation22,Citation23
The regenerative effects of collagen remodeling have been applied to treatment of genitourinary changes, such as thinning in the epithelial lining of the vagina and atrophy, which occur due to a fall in estrogen levels. Heat-induced thermal remodeling with new collagen deposition improves the tissue quality of the vaginal canal, while ablation to the external labia produces tissue regeneration. CO2 laser is capable of restoring the pH of the vaginal mucosa by liberating glycogen and acidic mucins from the epithelium.Citation17 Symptoms of dryness and itching, dysuria, and recurrent infections can be alleviated by increasing the glycogen that rebalances lactobacilli, which inhibit the growth and virulence of pathogenic bacteria.Citation17
CO2 laser treatment has previously demonstrated significant improvement in GSM symptoms in postmenopausal women.Citation11,Citation14–Citation16 However, the effects of laser treatment in perimenopausal women, experiencing childbirth and age-related vaginal and sexual symptoms of VVA, have not been previously reported. Similar to other studies in postmenopausal women,Citation11,Citation14 data from our study indicated a significant increase in VHI scores in perimenopausal women who underwent three sessions of fractional CO2 laser vaginal treatment. Improvement in VHI scores approached significance (P=0.053) after two treatments. Relevant VVA symptoms also improved after two treatments, with the majority of patients reporting improvement in sexual gratification and tightening effects (vaginal rejuvenation). Findings were highly significant (P<0.01) following three treatments. Although clinical improvement in facial wrinkling and photodamage have been observed at 12 months postoperatively following CO2 laser resurfacing,Citation18 support for long-term effect beyond 3 months is lacking for vaginal CO2 laser treatment. The perimenopausal population studied here, though limited in sample size, does support that there is still significant improvement in vaginal health and VVA symptoms up to 8 months following three treatments. Future maintenance treatments may be warranted in this study population, and the effect of collagen remodeling on emerging climacteric symptoms in these women is unknown. The role of CO2 laser treatment, as a non-hormonal treatment option, during this transition stage to potentially prevent or reduce GSM symptoms during menopause should be explored.
Conclusion
In this study population, fractional CO2 laser treatment was associated with improvement of vaginal health and amelioration of symptoms of VVA, resulting in improved satisfaction with sexual intimacy in perimenopausal women. Improvement was maintained at the 24-week follow-up. Treatment time was quick, and there was minimal discomfort associated with treatment. Investigation of long-term clinical outcome, up to 12 months post-treatment, in a postmenopausal population is currently ongoing at a multi-center study in the USA.
Acknowledgments
Study equipment was provided by Syneron Candela.
Disclosure
The author reports no conflicts of interest in this work.
References
- Mac BrideMBRhodesDJShusterLTVulvovaginal atrophyMayo Clin Proc2010851879420042564
- PalmaFVolpeAVillaPCagnacciAWriting group of AGATA studyVaginal atrophy of women in postmenopause. Results from a multicentric observational study: The AGATA studyMaturitas201683404426421474
- BarberoMMichelettiLBorgnoGCavannaLPretiMGhiringhelloBVulvar dystrophies in young and premenopausal womenJ Reprod Med19883365555583404518
- PortmanDJGassMLVulvovaginal Atrophy Terminology Consensus Conference PanelGenitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause SocietyMaturitas201479334935425179577
- IvankovichMBFentonKADouglasJMJrConsiderations for national public health leadership in advancing sexual healthPublic Health Rep2013128Suppl 110211023450891
- KingsbergSAWysockiSMagnusLKrychmanMLVulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women’s Views of Treatment Options for Menopausal Vaginal ChangEs) surveyJ Sex Med20131071790179923679050
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause SocietyMenopause201320988890223985562
- NotelovitzMUrogenital aging: solutions in clinical practiceInt J Gynaecol Obstet199759Suppl 1S35S399386214
- GuptaPSturdeeDWPalinSLMenopausal symptoms in women treated for breast cancer: the prevalence and severity of symptoms and their perceived effects on quality of lifeClimacteric200691495816428125
- SteinauerJEWaetjenLEVittinghoffEPostmenopausal hormone therapy: does it cause incontinence?Obstet Gynecol20051065 Pt 194094516260510
- PerinoACalligaroAForlaniFVulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laserMaturitas201580329630125596815
- GambaccianiMLevanciniMCervigniMVaginal erbium laser: the second-generation thermotherapy for the genitourinary syndrome of menopauseClimacteric201518575776326029987
- LeeMSTreatment of vaginal relaxation syndrome with an erbium: YAG laser using 90° and 360° scanning scopes: a pilot study & short-term resultsLaser Ther201423212913825071312
- SokolERKarramMMAn assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophyMenopause201623101102110727404032
- SalvatoreSNappiREParmaMSexual function after fractional microablative CO2 laser in women with vulvovaginal atrophyClimacteric201518221922525333211
- SalvatoreSLeone Roberti MaggioreUAthanasiouSHistological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo studyMenopause201522884584925608269
- ZerbinatiNSeratiMOrigoniMMicroscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatmentLasers Med Sci201530142943625410301
- FitzpatrickREGoldmanMPSaturNMTopeWDPulsed carbon dioxide laser resurfacing of photo-aged facial skinArch Dermatol199613243954028629842
- FitzpatrickRERostanEFMarchellNCollagen tightening induced by carbon dioxide laser versus erbium: YAG laserLasers Surg Med200027539540311126433
- RossEVMillerCMeehanKOne-pass CO2 versus multiple-pass Er:YAG laser resurfacing in the treatment of rhytides: a comparison side-by-side study of pulsed CO2 and Er:YAG lasersDermatol Surg200127870971511493293
- MansteinDHerronGSSinkRKTannerHAndersonRRFractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injuryLasers Surg Med200434542643815216537
- PetersonCMLaneJERatzJLSuccessful carbon dioxide laser therapy for refractory anogenital lichen sclerosusDermatol Surg20043081148115115274708
- LeeALimAFischerGFractional carbon dioxide laser in recalcitrant vulval lichen sclerosusAustralas J Dermatol2016571394325755049