Abstract
Background
Poor maternal health service utilization is one of the contributing factors to a high level of maternal and newborn mortality in Ethiopia. The factors associated with utilization of services are believed to differ from one context to another. We assessed the factors associated with skilled delivery service utilization in rural northern Ethiopia.
Subjects and methods
A community-based survey was conducted among mothers who gave birth in the 12 months preceding the study period, from January to February 2015, in the Tigray region of Ethiopia. Multistage sampling technique was used to select mothers from the identified clusters. Households within a 10 km radius of the health facility were taken as a cluster for a community survey. Data were collected using face-to-face interview at the household level. We compared the mothers who reported giving birth to the index child in a health facility and those who reported delivering at home, in order to identify the predictors of skilled delivery utilization. Multivariable logistic regression model was used to determine the predictors of skilled delivery service utilization. The results are presented with odds ratio (OR) and 95% confidence interval (CI).
Results
A total of 1,796 mothers participated in the study, with a 100% response rate. Distance to health facilities (adjusted odds ratio [AOR] =0.53 [95% CI: 0.39, 0.71]), perception of mothers to the availability of adequate equipment in the delivery service in their catchment area (AOR =1.5 [95% CI: 1.11, 2.13]), experiencing any complication during childbirth, using antenatal care, lower birth order and having an educated partner were the significant predictors of skilled delivery service utilization.
Conclusion
Implementing community-based intervention programs that will address the physical accessibility of delivery services, such as the ambulance service, road issues and waiting rooms, and improving quality maternity service will likely reduce the current problem.
Introduction
Pregnancy, birth and postpartum periods pose greater potential risk to maternal mortality and morbidity and a significant risk to the fetus and newborn as well.Citation1 The use of skilled delivery service during this period is found to be an effective intervention in attaining significant improvement in maternal and newborn health outcomes.Citation2,Citation3
Globally, an estimated 303,000 maternal death occurs each year, of which 99% occurs in developing countries.Citation4 Sub-Saharan Africa has the highest maternal mortality rate at 546 maternal deaths per 100,000 live births with poor progress in reduction.Citation5 Ethiopia has the highest maternal mortality statistics globally (353/100,000) and is one of the 10 countries that accounted for 59% of the global maternal deaths in 2015.Citation4 Overall, Ethiopia somehow shows a progress in reduction of maternal mortality, but still with high mortality and poor service utilization.Citation4,Citation5
Improving the maternal health service and increasing the number of deliveries attended by skilled personnel to 80% by 2020 is one of the strategies in the health sector plan of Ethiopia.Citation6 By 2016, 62% pregnant mothers visited for antenatal care and 28% of births were attended by skilled provider nationally; regional variations were very wide though, and there was a wide gap in skilled birth attendant use between urban and rural areas (from 80% to 21%).Citation7 Skilled birth attendant utilization in northern Ethiopia increased from 6% in 2005 to 59% in 2016.Citation7,Citation8 However, the current annual rate of improvement in skilled attendant use nationally is only 0.4%, which is the lowest among the six countries with the highest annual number of maternal deaths.Citation9
The impact of mothers’ factors on skilled delivery utilization has been studied by many scholars,Citation8,Citation10–Citation14 but has not been comprehensively assessed in Ethiopia,Citation11,Citation13,Citation14 in relation to the current available theoretical models developed by Gabrysch and Campbell.Citation15,Citation16 Many of the studies have not linked the perception of mothers to quality delivery service with skilled delivery use. Therefore, this study aims to assess the factors associated with skilled delivery utilization in rural parts of northern Ethiopia.
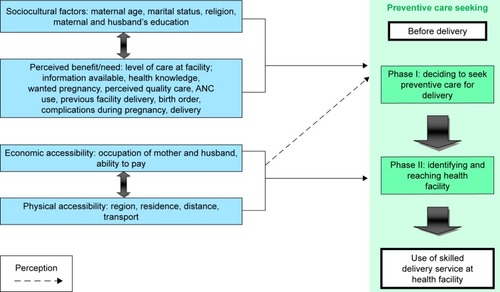
This framework stated the four factors (sociocultural, perceived benefit/need, economic and physical accessibility) that affect skilled delivery use, which are the main causes of Phase I and II delays. The framework further classified the factors as individual- and health facility-related factors. The individual-related factors include the mothers’ sociocultural factors and the perceived benefit/need of facility use in which both factors directly influence the mothers’ decision to seek care (Phase I). Economic and geographic accessibility mainly influences whether the woman actually identifies and reaches the health facility for delivery (Phase II), as shown in .Citation15
Figure 1 Conceptual framework of the factors affecting the use of skilled delivery service.
Abbreviation: ANC, antenatal care.
Subjects and methods
This study was part of a large community-based survey conducted among mothers who had given birth in the year preceding the survey in the Tigray region of Ethiopia. In this study, we compared mothers who reported giving birth to the index child at a health facility with a skilled birth attendant and those who reported delivering at home, in order to identify the predictors of skilled delivery utilization.
A multistage sampling technique was used. First, from the 90 Kebeles (the smallest administrative unit in Ethiopia) in the study area, 27 Kebeles were selected using lottery methods. Then, to select the study participants from the 27 rural communities linked with health facilities that provide maternity service in their catchment, we used cluster sampling techniques. All Kebeles within a radius of 10 km of each selected index health facility were taken as a cluster. A total sample size of 1,796 mothers was included in this study by including 67 mothers from each cluster. All eligible women who gave birth in the year preceding the survey were included in the study. Then mothers were classified as those who utilized skilled delivery or not, based on their report.
Data collection procedures
Data were collected through interviewer-guided survey, with mothers at their household. A structured questionnaire was adapted from the Demographic Health Survey and other similar literatures.Citation12,Citation13,Citation17 The questionnaire includes variables such as mothers’ sociodemographic and sociocultural factors, perceived need (birth order, wanted pregnancy, recent antenatal care use, history of complications during a recent pregnancy and childbirth, perceived quality care), economic accessibility (occupation of mothers and partners) and physical accessibility (distance to health facilities and ease of getting transport service to the nearest health facility). As a measure of data quality control, tools were translated into local language Tigrigna and back-translated into English by blind translators to check consistency. Pretest was also done outside the study areas and modification was made. Data were collected by 27 experienced health professionals who were recruited out of the selected community. They were trained prior to the study period. Data collection was supervised on a daily basis. Every day, the filled questionnaires were cross-checked for their completeness.
Measurements
The outcome variable of this study was skilled delivery service utilization and was coded 1 if mothers reported that they had attended delivery service by skilled health personnel (midwife, nurse or medical doctor) at the health facility for their recent birth; otherwise, it was coded 0. To assess the factors affecting the utilization of skilled delivery service, we adopted a conceptual framework from Gabrysch and Campbell,Citation15 and we assessed each independent variable based on the framework.
Distance to nearby health facility
This was measured from the report of mothers on the walking hours to the health facilities. This was coded 1 if mothers reported the walking hours to reach the nearby health facility to be ≥30 min; otherwise, it was coded 0.
Ease of getting transport service from home to the nearest health facility
This was measured from the report of mothers. It was coded 1 if the mothers reported and assumed that getting transport service from home to the nearest health facility was easy; otherwise, it was coded 0.
Mothers’ perception about the capability of service providers in managing complicated childbirths
This was measured from the report of mothers. It was coded 1 if the mothers reported and perceived that the service providers at the nearby health facility were capable of managing complicated childbirths; otherwise, it was coded 0.
Mothers’ perception of availability of adequate equipment in delivery service
This was measured from the report of mothers. It was coded 1 if the mothers reported and assumed that there was availability of adequate equipment in the delivery rooms; otherwise, it was coded 0.
Knowledge of mothers on danger signs during pregnancy and childbirth
This was coded 1 if the mothers reported they knew at least one danger sign during pregnancy and childbirth (eg, bleeding, fever, foul vaginal discharge, headache, vision problem, prolonged labor, convulsion); otherwise, it was coded 0.
Complications during childbirth
This was coded 1 if the mothers reported at least one complication during recent childbirth that occurred to themselves or newborns (eg, bleeding, prolonged labor >12 hours, leak of amniotic fluids before labor started, vaginal discharge, fever, retained placenta, convulsion, severe headache, epigastric pain, slow fetal movement, fetal distress); otherwise, it was coded 0.
Wealth index
This was measured using ownership of household assets: infrastructure (eg, homes and land ownership for agriculture, electricity), small equipment (eg, telephone, TV, radio) and domestic animals (cows/oxen, mule/donkey, sheep/goat). Items were coded into a relative index of household wealth using principal component analysis and calibrated into quintiles, with each representing 20% of the score, from 1 (very poor) to 5 (very wealthy) quintiles. Mothers were ranked by wealth quintiles using this index.
Statistical analysis
All the questionnaires were checked visually, coded and entered into EpiData version 3.1, and exported to Stata version 12 for analysis. Then, the data were cleaned to check for errors, and missed values and any error identified were corrected. Descriptive statistics were used to calculate the frequency distribution and proportions for categorical variables. For the normally distributed continuous variables, mean with SD was also used. Data related to the wealth of the mothers were assessed using household assets and were measured using principal component analysis. The bivariate logistic regression model was used to assess the factors associated with skilled delivery service utilization. Variables with a p-value of <0.25 were entered into multivariable model. A p-value of <0.05 was considered as the cutoff point for statistical significance. The degree of association between dependent and independent variables was assessed using odds ratio with 95% CI. Hosmer–Lemeshow test was used to compare and rule out the goodness of fit of the models. Multicollinearity was also examined, and all covariates having a value of variance inflation factor of <10 were tolerated.Citation18 The results are presented in the form of tables and text.
Ethical considerations
The study was approved by Mekelle University Institutional Review Board (ERC0427/2014), and a formal letter of permission was obtained from the Tigray Regional Health Bureau. Informed verbal consent was obtained from each mother.
Results
Sociodemographic characteristics
A total of 1,796 mothers participated in the study. There was no refusal to participate in the study. The average age of mothers was 27 (SD ±6) years. Most of the mothers were married (1,578 [87.9%]) and Orthodox Christian followers (1,620 [90.2%]). More than half of the mothers did not attend formal school (824 [45.9%]) and were housewives (717 [39.9%]) and farmers (617 [34.4%]). Regarding the wealth index, most of the mothers were categorized as poor (731 [40.7%]), as shown in .
Table 1 Sociodemographic characteristics of mothers who participated in the study in northern Ethiopia, 2015
Mothers’ perception to quality delivery service and accessibility
Accessibility to health facilities and the perceived quality were associated with the use of facilities delivery services. About half, 897 (49.9%), of the mothers reported that the distance from home to facility took >30 min on foot. About 644 (35.9%) mothers reported that it was difficult to get the transportation service from home to the nearby health facility. About 741 (41.3%) mothers perceived that the service providers at the nearby health facility were not capable of solving birth-related complications. More than half, 940 (52.3%), of the mothers perceived that there was inadequate equipment for delivery service at the nearby health facility ().
Table 2 Perception of mothers toward the accessibility and quality of maternity services in their catchment area in northern Ethiopia, 2015
Skilled delivery service utilization
In this study, 1,411 (78.6% [95% CI: 0.77–0.80]) mothers’ recent delivery was assisted by skilled birth attendants. About 659 (36.7%) mothers had at least four antenatal care visits, while majority of the mothers visited only once (1,581 [88%]). Almost all mothers did not attend postnatal care during the first week of birth (1,735 [96.6%]).
Factors associated with skilled delivery service utilization
After controlling for confounders, those living far from health facility were less likely to utilize skilled delivery services (adjusted odds ratio [AOR] =0.53 [95% CI: 0.39, 0.71]) and those who perceived facilities as having adequate equipment in the delivery were more likely to utilize skilled delivery services (AOR =1.5 [95% CI: 1.11, 2.13]). In addition, antenatal care use (AOR =0.17 [95% CI: 0.12, 0.25]), birth order (AOR =0.29 [95% CI: 0.16, 0.51]), experiencing of any complications during childbirth in the recent pregnancy (AOR =1.98 [95% CI: 1.44, 2.71]) and having an educated partner (AOR =2.15 [95% CI: 1.31, 3.52]) were the significant predictors of skilled delivery service utilization ().
Table 3 Factors associated with skilled delivery service utilization in northern Ethiopia, 2015
Discussion
The aim of the study was to identify the predictors of skilled delivery utilization. Based on this, distance to health facilities, perception of mothers on availability of adequate equipment in the delivery service in their catchment area, having an educated partner, using antenatal care, lower birth order and experiencing any complication during childbirth were the significant predictors of skilled delivery service utilization.
The longer the walking distance to reach the nearest health facility, the lesser was the mothers likely to utilize skilled delivery service. Lack of easy transportation service to the nearest health facility was also reported as an important challenge. These findings are consistent with the findings of studies conducted in Nepal,Citation19 ZambiaCitation20 and Ethiopia,Citation21 wherein physical distance to the maternity facility and lack of geographic access were reported as barriers for the place of delivery. On the other hand, freely available transport service for the pregnant mothers was reported to cause substantially reduced pregnancy-related mortality in Ethiopia.Citation22 It is, however, important to note that the distance to a health facility in this study was assessed based on the mothers’ report, which is subjective; it may over- or underestimate the actual distance to the health facilities and may affect the associations. If a mother perceived that the distance to a health facility is considered to be a barrier, they are less likely to utilize services.
Mothers’ perception of how well a facility is equipped was significantly associated with utilization of skilled delivery services. This kind of perception could be based on previous self and friends/relative exposures to the service. Perception of poor quality reduces the likelihood of utilizing maternal service and pushes them to take risks by delaying service-seeking even in the face of serious complications.Citation19,Citation20,Citation23 Previous studies in Ethiopia have reported poor and inadequate supply of essential equipment in health facilities.Citation24 Similarly, a study in Zambia indicated that poor perception has an effect on poor utilization of skilled delivery service.Citation20 As a limitation of this study, measuring the perception using only quantitative approach may not be adequate to know the feeling of mothers.
Those mothers who reported they did experience any complications during labor and delivery in their recent pregnancy were more likely to use skilled delivery service. This indicated that mothers are not likely to use skilled delivery service unless they had experienced complications. This could be due to the poor knowledge of mothers on the complications and birth preparedness plan, cultural influence or poor counseling during pregnancy.Citation16
We found that mothers giving birth have repeatedly been less likely to use skilled delivery service, compared to those giving birth for the first time. This indicates multipara mothers neglect the service for their subsequent pregnancy and births. This may be due to their previous bad experience of health outcome at the facility, cultural influence or poor perception of the complications. The finding is consistent with those of studies done in EthiopiaCitation16 and the Democratic Republic of Congo,Citation25 wherein it was reported that mothers do not use skilled birth care as the birth order increases. This shows emphasis is needed to educate multipara mothers during antenatal care visits. Moreover, mothers who did not attend antenatal care for the index pregnancy were less likely to use skilled delivery service. Having pervious exposure to health facility may influence mothers to continue the service.Citation14,Citation15 Mothers having an educated partner were more likely to use skilled delivery service. The association between education and service utilization is also in line with previous reports from Ethiopia and other African countries.Citation14,Citation15,Citation26
Similar to previous observations, mothers who did not know about the danger signs during pregnancy, birth and postpartum period were less likely to use delivery service.Citation27 Birth preparedness has a clear positive effect on the decision making for skilled providers.Citation27 Thus, awareness creation and offering client-centered counseling to mothers and families at an early stage of pregnancy during antenatal care or home visits at community are important.
Conclusion
Distance to the health facility, perception of mother to availability of adequate equipment in the delivery service in their catchment area, experiencing any complication during childbirth, using antenatal care, lower birth order and having an educated partner were the significant predictors of skilled delivery service utilization. Implementing community-based intervention programs that will address the physical accessibility of delivery service, such as the ambulance service and road issues; improving quality maternity service; revising the protocol for admission of mothers during the latent phase of labor, especially for those mothers who come from distant places; preparing adequate waiting rooms at the facility; and awareness creation, especially for mothers with high birth order, will likely reduce the current problem.
Author contributions
GF, YB, AW and WT conceived and designed the study, performed data analysis and wrote the paper. All authors read and approved the final manuscript.
Acknowledgments
Our heartfelt thanks go to Mekelle University and Addis Continental Institute of Public Health for all-round support. We thank the African Population and Health Research Center (APHRC) for the African Doctoral Dissertation Research Fellowships (ADDRF) toward financial and technical support (grant number ADF005).
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization (WHO)Safe mother hood, Care in Normal birth: a practical guide1996Reproductive Health and Research, WHOGeneva, Switzerland Available from: http://whqlibdoc.who.int/hq/1996/WHO_FRH_MSM_96.24.pdf?ua=1Accessed July 7, 2014
- HultonLAMatthewsZStonesRWA framework for the evaluation of care in maternity services: the question should not be why do women not accept the service that we offer, but why do we not offer a service that women will accept?2000University of Southampton and Opportunity and Choice Available http://www.mamaye.org/sites/default/files/u436/Hulton_2000_Framework%20for%20maternity%20QoC.pdfAccessed December 16, 2015
- World Health Organization (WHO)Mother-baby Package: implementing Safe motherhood in countriesGenevaWHO1996 Available from: http://www.who.int/maternal_child_adolescent/documents/who_dhe_msm_9411/en/Accessed December 14, 2015
- WHOUNICEFUNFPAWorld Bank Group and the United Nations Population DivisionTrends in Maternal Mortality 1990 to 20152015World Health OrganizationGeneva, Switzerland Available from: http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/Accessed November 2, 2016
- Central Statistical Agency [Ethiopia]Ethiopia Mini Demographic and Health Survey 20142014Addis Ababa, Ethiopia Available from: http://www.dktethiopia.org/publications/ethiopia-mini-demographic-and-health-survey-2014Accessed September 15, 2016
- Federal Democratic Republic of Ethiopia Ministry of Health (FDRE MOH)Health Sector Transformation Plan (HSTP) from 2015/16 up to 2019/20, Draft_V152014 Available from: http://www.emtct-iatt.org/wp-content/uploads/2016/01/Ethiopia-HSSP-2015-2020.pdfAccessed April 27, 2017
- Central Statistical Agency (CSA) [Ethiopia] and ICFEthiopia Demographic and Health Survey 2016: Key Indicators Report2016Addis Ababa, Ethiopia and Rockville, Maryland, USA, CSA and ICF Available from: https://dhsprogram.com/pubs/pdf/PR81/PR81.pdfAccessed April 25, 2017
- Central Statistics Agency (CSA)Ethiopian demographic and health surveyAddis AbabaCSA, ORC Macro2005 Available from: https://www.unicef.org/ethiopia/DHS_2005_Ethiopia.pdfAccessed March 3, 2017
- CroweSUtleyMCostelloAPagelCHow many births in sub-Saharan Africa and South Asia will not be attended by a skilled birth attendant between 2011 and 2015?BMC Pregnancy Childbirth201212422251749
- AwokeWMuhammedJAbejeGInstitutional delivery service utilization in Woldia, EthiopiaSci J Public Health2013111823
- BayuHFissehaGMulatAYitayihGWoldayMMissed opportunities for institutional delivery and associated factors among urban resident pregnant women in South Tigray Zone, Ethiopia: a community-based follow-up studyGlob Health Action2015828082
- Central Statistics Agency (CSA), and ICF Macro Calverton, Ethiopia Demographic and Health Survey 2011Addis AbabaCSA2011 Available from: https://www.unicef.org/ethiopia/ET_2011_EDHS.pdfAccessed March 2, 2017
- TeferraASAlemuFMWoldeyohannesSMInstitutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia: A community-based cross sectional studyBMC Pregnancy Childbirth2012127422849421
- WorkuAGYalewAWAfeworkMFFactors affecting utilization of skilled maternal care in Northwest Ethiopia: a multilevel analysisBMC Int Health Hum Rights2013132023587369
- GabryschSCampbellOMRStill too far to walk: Literature review of the determinants of delivery service useBMC Pregnancy Childbirth200993419671156
- ThaddeusSMaineDToo far to walk: maternal mortality in contextSoc Sci Med1994389109111108042057
- FotsoJCMukiiraCPerceived quality of and access to care among poor urban women in Kenya and their utilization of delivery care: harnessing the potential of private clinics?Health Policy Plan201227650551522080515
- DarmawanIKeevesJPSuppressor variables and multilevel mixture modelingInt Educ J200672160173
- WagleRRSabroeSNielsenBBSocioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from NepalBMC Pregnancy Childbirth200441815154970
- GabryschSCousensSCoxJCampbellOMThe influence of distance and level of care on delivery place in rural Zambia: a study of linked national data in a geographic information systemPLoS Med201181e100039421283606
- KebedeAHassenKTeklehaymanotANFactors associated with institutional delivery service utilization in EthiopiaInt J Wom Health20168463475
- GodefayHKinsmanJAdmasuKByassPCan innovative ambulance transport avert pregnancy-related deaths? One-year operational assessment in EthiopiaJ Glob Health20166101041027231545
- ParkhurstJOSsengoobaFAssessing access barriers to maternal health care: measuring bypassing to identify health centre needs in rural UgandaHealth Policy Plan200924537738419520736
- BerhanYAbdelaAEmergency obstetric performance with emphasis on operative delivery outcome: does it reflect the quality of care?Ethiop J Health Deve200418296106
- Abel NtambueMLFrançoise MalongaKDramaix-WilmetMDonnenPDeterminants of maternal health services utilization in urban settings of the Democratic Republic of Congo – a case study of Lubumbashi CityBMC Pregnancy Childbirth2012126622780957
- FekaduMRegassaNSkilled delivery care service utilization in Ethiopia: analysis of rural-urban differentials based on national demographic and health survey (DHS) dataAfr Health Sci201414497498425834510
- KabakyengaJKÖstergrenPOTuryakiraEPetterssonKOInfluence of birth preparedness, decision-making on location of birth and assistance by skilled birth attendants among women in South-Western UgandaPLoS One201274e3574722558214
