Abstract
Intrauterine adhesions with symptoms like hypomenorrhea or infertility are known under the term Asherman’s syndrome. Although the syndrome has been widely investigated, evidence of both prevention of the syndrome and the ideal treatment are missing. Understanding the pathogenesis of intrauterine adherences is necessary for the prevention of the formation of intrauterine scarring. Intrauterine adhesions can develop from lesion of the basal layer of the endometrium caused by curettage of the newly pregnant uterus. The syndrome may also occur after hysteroscopic surgery, uterine artery embolization or uterine tuberculosis. For initial diagnosis the less invasive contrast sonohysterography or hysterosalpingography is useful. The final diagnosis is based on hysteroscopy. Magnetic resonance imaging is required in cases with totally obliterated uterine cavity. Intrauterine adherences are classified in accordance with different classification systems based on the hysteroscopic diagnosis of severity and localization of adherences. Classification is necessary for the planning of surgery, information on prognosis and scientific purposes. Surgery is performed in symptomatic patients with either infertility or with painful periods. Intrauterine adherences are divided with a hysteroscope using scissors or a power instrument working from the central part of the uterus to the periphery. Peroperative ultrasonography is useful in an outpatient setting for the prevention of complications. Hysteroscopy with fluoroscopy is a solution in difficult cases. Use of intrauterine devices like balloon catheters or intrauterine contraceptive devices seems to be the preferred methods for the prevention of re-occurrence of adhesions after treatment. Both primary prevention after hysteroscopic surgery or curettage and secondary prevention of new adhesions after adhesiolysis have been investigated. The aim of this review was to summarize the literature on diagnosis, classification, treatment and prevention, based on a literature search with a wide range of search terms.
Introduction
Intrauterine adhesions causing amenorrhea after curettage were first described by Fritsch in 1894.Citation1 Later AshermanCitation2 in 1950 described the history of 29 women with amenorrhea secondary to trauma of the uterine cavity, the Asherman’s syndrome (AS). AS is defined by the presence of intrauterine adhesions or adhesions in the endocervix with consequent risk of hypomenorrhea/amenorrhea, reduced fertility, pregnancy loss and abnormal placentation.
The recently pregnant uterus seems susceptible to trauma of the basal layer of the endometrium, which can develop into intrauterine adhesions and may give future problems for the patient. It is estimated that more than 90% of cases with AS occur after pregnancy-related curettage.Citation3
However, AS can develop without preceding pregnancy in cases with infection or surgery related to the uterus.
Hanstede et alCitation4 emphasizes that the presence of symptoms is essential for the term “Asherman’s syndrome,” as the increasing use of diagnostic hysteroscopy often will disclose clinically irrelevant adhesions.
In cases where intrauterine adhesions (IUA) are found accidentally without any symptoms one should avoid the term AS and instead apply the term “asymptomatic intrauterine adhesions.”Citation5
Intrauterine adhesions can be either primary after pregnancy-related curettage, alternatively after hysteroscopic surgery, or secondary when re-occurring after adhesiolysis has been performed.Citation6,Citation7
Although AS has been known for many years we still lack reliable non-invasive diagnostic methods, agreement about one classification only and sufficient methods to avoid re-occurrence of adhesions after surgical treatment of AS.
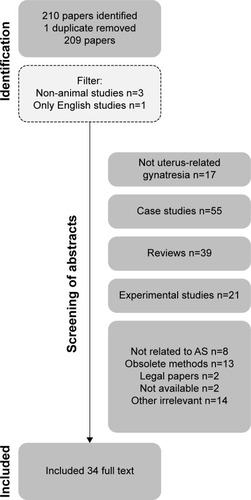
All eligible literature until September 2018 was identified using the keywords “Asherman’s syndrome,” “genital adhesions,” “intrauterine synechiae,” and “gynatraesia” and reviewed by electronic databases including PubMed, Web of Science and Scopus. Other relevant articles were found from citations in these publications. The selection of relevant papers based on the literature search is illustrated in the flowchart (). Excluded were non-English papers, studies of vagina, experimental and animal studies, most case-stories, minor case-series and reviews, except meta-analyses. Animal studies and experimental studies are included in the paragraph about stem cell treatment.
Occurrence
It is impossible to detect or estimate the true prevalence of all IUA, as probably most cases are without symptoms. However, the total number is irrelevant from a practical point of view. Only cases with AS, which imply pain, bleeding disorders or impaired fertility needs treatment.
Prevalence is dependent on the population studied as well as the diagnostic method and classification systems used. Thus, the prevalence is difficult to define as the diagnostic methods have changed over time and different classifications are used. If we wish to determine whether the prevalence is changing, we should at least agree about definition and classification.
Among an infertile population Baradwan et alCitation8 found the prevalence of AS to be 4.6%. After secondary removal of placental remnants or repeat curettage after incomplete abortion a prevalence of IUA was found in 40%.Citation9 Salzani et alCitation10 found IUA in 37.6% after curettage following abortion. The incidence of IUA varies between 15 and 40% after curettage.Citation10 The prevalence of AS in women with impaired fertility ranges from 2.8% to 45.5% depending on the subpopulation.Citation11 In a meta-analysis by Hooker et alCitation12 a prevalence of IUA of 19.1% was found by hysteroscopy within 1 year in women diagnosed with miscarriage treated expectantly, medically or surgically. The majority were mild to moderate adhesions. The incidence of AS has been investigated in different populations. Applying a strict definition, the incidence should only imply new cases in a given period. However, very often the cases described concern treatment of reoccurrences, often multiple treatments. In Denmark a total of 61 unique cases of AS was found during a 10-year period,Citation13 in Holland 638 women with AS were referred to a specialist center during a 10-year periodCitation4 and in Saudi Arabia, 41 women were referred with AS to a specialist center during an 8-year period.Citation8 Chen et alCitation14 found 357 cases of AS in a 4-year period in a large Women’s Hospital in China.
Risk factors
Trauma caused by surgical interventions, primarily curettage of the basal layer of the endometrium shortly after a pregnancy is the main reason for development of symptomatic IUA. These adhesions can result in partial or complete obstruction of the uterine cavity or the cervical canal. An incidence of 10% IUA after one curettage evaluated by HSG was seen in one randomized controlled trial.Citation15 However, in women with at least two curettages 30.6% (22/72) had IUA when evaluated by hysteroscopy 10 weeks after the curettages.Citation16
Two cohort studies including women with retained products of conception (RPOC) after delivery or miscarriage demonstrated significantly more IUAs after curettage compared to hysteroscopic removal (35.9% vs 4.2%).Citation9,Citation17
Usually the trauma is caused by curettage intending to remove placental remnants after a recent pregnancy. Even ultrasound-guided curettage is more traumatic than hysteros-copy when emptying the uterine cavity.Citation17 First trimester procedures appear to cause less severe adhesions, the majority grade 1–2 (ESGE classification) compared to postpartum procedures, where the majority had grade 3–5 in one study.Citation4
The incidence of curettage-related IUA in women seeking termination of pregnancy may be declining. The national rate of surgical termination in Denmark has declined from 87% to 36% from 2001 to 2017, as the rate of the more gently medical termination of a pregnancy has increased. Medical termination is insufficient in 4% of procedures leading to curettage. Surgical termination is insufficient in 2.7% leading to re-evacuation according to the National Danish Patient register, which covers all citizens and surgical procedures in Denmark. With these figures in mind the number of re-evacuations after legal abortion is more than halved (352 in 2001 and 145 in 2017) in Denmark from 2001 to 2017, as a consequence of increased use of medical abortions. Hopefully this reduced frequency of intrauterine trauma will result in fewer cases with AS in the future.Citation18
Other procedures or circumstances may create intrauterine adhesions. Thus, case stories mention embolization of the uterus, B-Lynch sutures, abdominal myomectomy, hysteroscopic myomectomy, genital tuberculosis and surgical treatment of Mullerian anomalies.Citation19–Citation24
Furthermore, a predisposition to intrauterine adhesions could be linked to unspecific factors like age, race, nutritional status and infectious processes.Citation25 However, such factors are not supported in the literature, where the dominant factor seems to be surgical trauma (frequent hysteroscopic surgery, repeat curettages and infection).Citation9,Citation25
Diagnosis of intrauterine adherences
Several diagnostic modalities have been evaluated for the diagnosis of intrauterine adhesions (IUA). IUA can be visualized by hysterosalpingography (HSG), ultrasonography including contrast sonohysterography (SHG), 3D ultrasonography, hysteroscopy and magnetic resonance imaging (MRI). Hysteroscopy is the gold standard in studies comparing different diagnostic modalities, and several classification systems are based on hysteroscopic findings. HSG gives the opportunity to simultaneously evaluate tubal patency, but details of filling defects are not visualized, and a high false-positive rate is documented.Citation26,Citation27 Transvaginal ultrasonography with evaluation of the endometrial thickness in women with AS showed substantially thinner endometrium compared to normal menstruating women, in a study of 16 women with AS and 50 controls.Citation28 Unenhanced trans-vaginal ultrasonography alone has very limited diagnostic capacity,Citation29 with both sensitivity and positive predictive value as low as 0%.Citation27 Contrast sonohysterography with infusion of sterile saline or gel in the uterine cavity and dynamic ultrasonography enables visualization of the uterine cavity.Citation30 Contrast sonohysterography has a high negative predictive value (98%), but a moderate positive predictive value (43%) when compared with hysteroscopy.Citation27,Citation29 In a Taiwanese study of 110 women, 3D sonography was compared with hysteroscopy, finding a confirmation range of 16%–100% in accordance to the number of morphological abnormalities, including marginal irregularity, thinning defects, obliteration, fibrosis and calcification.Citation31 Virtual hysteroscopy, a 4D virtual reconstruction of the uterine cavity may play a future role in the diagnosis of IUA.Citation32 HSG, SHG and hysteroscopy are all of limited diagnostic value when the cavity is totally obstructed. In these rare cases MRI can be valuable, although too expensive as a routine diagnostic tool.Citation33,Citation34 The application of ultrasound contrast for three-dimensional color power angiography has been evaluated in one study only.Citation35 When compared with hysteroscopy a positive likelihood ratio of 2.9 for detection of IUA was found, meaning moderate diagnostic ability. These findings have not been confirmed by others. Intraoperative fluoroscopy improves the imaging during surgery and is now preferred instead of simultaneous laparoscopy.Citation4
Classification of IUA and AS
Several classification systems have been proposed for the description of the severity of IUA and AS.Citation36–Citation42 They are all descriptive in different ways and are therefore non-comparable. Only two classification systems include symptoms regarding AS (obstetric or menstrual history). Three of the classifications are descriptive with three stages: minimal/mild, moderate, and severe based on the hysteroscopic assessment of the extent and type of adhesions (filmy, firm/dense).Citation36,Citation38,Citation39 Hamou et alCitation37 describe the adhesions as isthmic, marginal, central, and severe. The former European Society for HysteroscopyCitation41 operated with four grades with subtypes (seven stages in all), while DonnezCitation40 uses six grades based on hysteroscopy and HSG with postoperative pregnancy rate as primary driver. Finally, Nasr et alCitation42 have developed a complex system with hysteroscopic assessment combined with menstrual and obstetric history. None of the used classification systems have been validated or examined in relation to reproductive performance.
Intending to produce valid data for evaluation of treatment and prophylaxis, it is mandatory to agree about one of the systems. The ideal system should include extent and type of adhesions as well as fertility history, menstrual history is in our opinion less important.
Management of AS
Prevention of IUA after curettage
In an industry-sponsored randomized controlled trial there was significantly less IUA in women undergoing curettage with at least one previous curettage when hyaluronic acid gel was applied. However, selection bias may be present in the study of 149 women collected from eight different centers in a 3-year period, ie, six patients per center per year.Citation16 In a recent study of suction curettage in delayed miscarriage a significant reduction of moderate to severe IUA was seen in women treated with a new crosslinked hyaluronan gel finding 0.7% (1/137) vs 24% (33/137) respectively.Citation43 However these findings should be confirmed by future studies.
Prevention of IUA after hysteroscopic procedures
Taskin et alCitation44 found a high frequency of IUA after resection of solitary and multiple fibroids (31.3% respectively 45.5%). In another study, Mazzon et alCitation45 found a very low frequency of IUA after myomectomy with a combination of monopolar current and cold knife resection. The incidence of formation of IUA after resection of uterine septum is estimated to be up to 12% in untreated women.Citation21 In three prospective randomized studies, the administration of oral estrogen did not reduce the risk of IUA.Citation21,Citation46,Citation47 Hyaluronic acid gel or polyethylene oxide-sodium carboxymethylcellulose gel for the prevention of intrauterine adherences have been investigated demonstrating conflicting results. In a meta-analysis it is concluded that there is lack of reproducible evidence to prove that gel may decrease IUA after hysteroscopy.Citation48
Treatment of AS
In women with infertility and those with painful hypo-/amenorrhea, treatment of AS is indicated. For fertility, the initial goal of treatment is restoration of a normal calibrated uterine cavity covered with endometrial lining and free tubal ostia. However, further fertility treatment may be necessary, especially in cases where the tubes are blocked. In cases without infertility, where retained blood leads to cyclic pain, sufficient drainage is mandatory. As hysteroscopic equipment has improved over the years, hysteroscopic treatment has become the method of choice.Citation38,Citation49 Filmy adhesion alone can be divided by using the tip of the hysteroscope without any energy source or scissors.Citation49 The division of adhesions begins in the central and safe part of the uterus and moves laterally and toward the fundus.
Different hysteroscopic instruments are useful in the treatment of AS, biopsy forceps, sharp or blunt scissorsCitation4,Citation11,Citation38 and division of strings with energy like monopolar diathermia,Citation50 bipolar diathermiaCitation51 or laser.Citation52,Citation53 Careful dissection with energy instruments is mandatory, as the energy may destroy otherwise healthy endometrium. Monopolar diathermia with special fluids is associated with a larger risk of fluid overload complications compared to bipolar diathermia with saline and therefore not recommended as first choice treatment.Citation54
Few studies have evaluated the outcome after hysteroscopic adhesiolysis. Overall restoration of normal menstruation is observed in 75%–100%.Citation4,Citation38,Citation50,Citation55,Citation56 The effect on fertility is influenced by several other factors, eg, the age of the patient, and whether infertility is primary or secondary. The pregnancy rate ranges between 25 and 76%Citation38,Citation56 and the term delivery rate, in women who achieved pregnancy, between 25 and 79.7%.Citation38,Citation56,Citation57
The success rate is dependable on the severity of adhesions.Citation38,Citation50 The hysteroscopic procedure is feasible and can be performed in an outpatient setting.Citation57 Intraoperative transabdominal ultrasonography, as an alternative to lapa-roscopy, can decrease complications in terms of perforation and false passageways. For severe cases intraoperative fluoroscopy with simultaneous X-ray is a possibility. Intracavitary distribution of contrast media facilitates visualization of hidden areas of endometrium and tubal patency can be evaluated during the procedure. The intraoperative fluoroscopy is an effective method to avoid uterine perforation, with better results than intraoperative ultrasonography.Citation4,Citation58
After primary hysteroscopic adhesiolysis, the formation of new adhesions is very frequent, and several modalities have been studied and suggested for the prevention of new adhesions. The recurrence rate is associated with the grade of adherences. Hanstede et alCitation4 found 21%–25% recurrence with grade 1–2a adherences, 29.1% with grade 3, 38.5% with grade 4, and 41.9% with grade five using the classification system of the former European Society of Hysteroscopy.
Second-look hysteroscopy with division of newly formed adherences has been studied in a retrospective setting of 151 patients, cumulative pregnancy rate (77% vs 56%) and live birth rate (77% vs 63%) seems to improve when early second-look is performed within 2 weeks to 2 months after primary adhesiolysis.Citation59 A small observational study recommended second-look hysteroscopy after 2 weeks, and up to four hysteroscopies after primary surgery. In this report 46% (7/15) were either pregnant or had delivered an infant at the end of the study.Citation60
There are several methods for secondary prevention. The use of estrogen has been studied in several set-ups, either as estrogen onlyCitation55,Citation61 or as ancillary treatment either with intrauterine deviceCitation11,Citation14,Citation24,Citation47,Citation62–Citation65 or Foley catheter.Citation11,Citation61,Citation65
Increased menstrual flow was seen when estrogen was used as ancillary treatment, except in one study including genital tuberculosis.Citation66 The effect on fertility depended upon the severity of AS and needs further investigation.Citation67 In studies where estrogen was used alone, pregnancy rates were generally lower (42%–53%)Citation51,Citation61,Citation68 compared to the ancillary use of estrogen with intrauterine contraceptive device (IUCD), Foley catheter or other device, where pregnancy rates were 51%–100%.Citation14,Citation61,Citation62,Citation65 Varying regimes of estrogen were used in the studies, leaving no conclusion on ideal dosage, timing of progesterone or route of administration (vaginal or oral). In a recent randomized study, 4 mg and 10 mg estradiol orally was compared. No superior effect of the high dosage was demonstrated.Citation69 When comparing 2 mg and 6 mg in a prospective, randomized trial, no benefit was demonstrated in the 6 mg arm.Citation70
Intrauterine application of gel for secondary prevention of adhesions has been investigated. Acunzo et al found a significant effect of hyaluronic acid compared to no treatment (14% in the hyaluroic acid arm, 32% in the no treatment arm P<0.05) in the only randomized controlled trial of gel barrier for prevention of new IUA after hysteroscopic adhesiolysis.Citation71 A study comparing intrauterine balloon, IUCD and hyaluronic acid gel demonstrated that the balloon and IUCD were more effective than hyaluronic acid when evaluated with AFS score. No data on menstrual flow or fertility were presented.Citation72
The use of other mechanical barriers is also suggested for the prevention of secondary adhesions. Orhue et alCitation62 compared an IUCD with a pediatric Foley catheter and found that the catheter was significantly more effective in terms of restoring normal menstruation and conception. The short-term use of the two devices was analyzed in two periods, each lasting 4 years. Cook Medical (Indianapolis, IN, USA) has designed a heart-shaped intrauterine balloon for prevention of secondary intrauterine adhesions. MarchCitation73 argues that this balloon is more effective in the prevention of marginal intrauterine adhesions than the Foley catheter. Lin et alCitation72 found in a blinded RCT study that balloon and IUCD were equally effective in the prevention of secondary adhesions.
The same group performed a retrospective cohort study comparing balloon, IUCD, hyaluronic acid and controls. In this study they were not able to detect a difference between balloon and IUCD. However, these two modalities were significantly more effective than hyaluronic acid. Hyaluronic acid was no better than no prophylaxis in the controls.Citation72
Infection and antibiotics
According to the literature the only specific infection that causes AS is genital tuberculosis.Citation19 There is no evidence in the literature that prophylactic antibiotics can prevent secondary intrauterine infectious complications.Citation87 However, when obvious infection is seen, antibiotics are mandatory.
Stem cell treatment in AS
Regeneration of endometrium through stem cell treatment has been evaluated both in animal modelsCitation74–Citation78 and in small experimental human studies.Citation79–Citation82 Bone-marrow derived stem cells, mesenchymal stem cells and autologous menstrual blood derived stromal cells have been investigated. Different application methods have been used, eg infusion in spiral arterioles through catheters,Citation81 transmyometrial administration to the subendometrial areaCitation80 and direct installation of stromal cells in uterine cavity after endometrial scratching.Citation82 Stem cells arranged in spheroids were successful in a rat model of damaged endometrium.Citation78 In a study by Singh et alCitation80 five out of six women started menstruation again. Santa Maria et alCitation81 included 15 women with AS, who attained increased endometrial thickness and regular menses with hormonal replacement therapy. Four women conceived, one with a live birth. In the study of Tan et alCitation82 seven women with refractory AS who were treated with autologous menstrual blood-derived stromal cells, had increased endometrial thickness. Three patients conceived, with one on-going pregnancy. Future randomized trials are needed to prove if stem cell treatment will have a clinical role in AS.
Complications of AS
When fertility is restored after treatment of AS, even obstetric complications may occur, eg reduced fetal weight and placenta-related complications. Only one case–control study describes the potential hazards for the foetus when the mother had IUA.Citation83 This study found a significantly lower birthweight in cases with IUA, increased incidence of preterm delivery and retained placenta in 10.7% of the patients. However, the material only comprises 14 cases and 42 controls. Preterm delivery was also described by Roy et alCitation47 and Zikopoulos et alCitation63 after surgical treatment of AS.
Friedman et alCitation84 described three patients with placenta accreta, uterine sacculation and paper-thin uterine fundus in pregnancies after surgical treatment of intrauterine adhesions. Siegler and ValleCitation85 found placenta accreta in 8% of pregnant women after treatment for AS. The occurrence of placenta accreta has only been described in the recent literature in case stories.Citation86
Conclusion
The prevention and treatment of AS are still a challenge, as the syndrome appears only occasionally after termination of pregnancy and after emptying of the recently pregnant uterus.
Focus on the information about effective contraception is necessary to minimize the number of legal abortions. If legal abortion is indicated, the medical termination of pregnancy seems to reduce the frequency of surgical evacuation and re-evacuation and consequently might be less prone to induce intrauterine adhesions. If evacuation of retained products of conception is needed, it is important to be as gentle as possible without increasing the risk for re-evacuation and consequently increasing the risk of AS. In cases with RPOC, hysteroscopy is preferred due to the significantly reduced risk of IUA compared to curettage. Hysteroscopy is more effective in avoiding incomplete removal of RPOC.
AS should be suspected if the patient complains about change in menstrual pattern, menstrual pain or infertility after intrauterine instrumentation. Ultrasonography with saline infusion can in some cases show filling defects of the uterine cavity.
If AS is suspected, a hysteroscopy should be performed, and adhesions should be separated without use of electric current or with bipolar current to prevent complications.
To avoid re-occurrence of adhesions the use of balloon catheters or IUCD (without progesterone) seems advisable. Complementary treatment with low-dose estrogen might be helpful.
AS is rather infrequent, and the surgery is difficult. Therefore, it is important to refer severe cases to specialized centers with surgeons skilled in advanced intrauterine surgery.
Disclosure
The authors report no conflicts of interest in this work.
References
- FritschHEin fall von volligen Schwund Der Gebärmutterhohle nACh AuskratzungZentralbl Gynaekol18941813371342
- AshermanJGTraumatic intra-uterine adhesionsJ Obstet Gynaecol Br Emp195057689289614804168
- SchenkerJGMargaliothEJIntrauterine adhesions: an updated appraisalFertil Steril1982375595610
- HanstedeMMFvan der MeijEGoedemansLEmanuelMHResults of centralized Asherman surgery, 2003–2013Fertil Steril201510461561156826428306
- YuDWongYMCheongYXiaELiTCAsherman syndrome – one century laterFertil Steril200889475977918406834
- DiamondMPFreemanMLClinical implications of postsurgical adhesionsHum Reprod Update20017656757611727865
- HellebrekersBWTrimbos-KemperTCTrimbosJBEmeisJJKooistraTUse of fibrinolytic agents in the prevention of postoperative adhesion formationFertil Steril200074220321210927033
- BaradwanSBaradwanAAl-JaroudiDThe association between menstrual cycle pattern and hysteroscopic March classification with endometrial thickness among infertile women with Asherman syndromeMedicine20189727e1131429979403
- WestendorpICAnkumWMMolBWVonkJPrevalence of Asherman’s syndrome after secondary removal of placental remnants or a repeat curettage for incomplete abortionHum Reprod19981312334733509886512
- SalzaniAYelaDAGabiattiJREBedoneAJMonteiroIMUPrevalence of uterine synechia after abortion evacuation curettageSao Paulo Med J2007125526126418094891
- MarchCMIsraelRMarchADHysteroscopic management of intrauterine adhesionsAm J Obstet Gynecol19781306653657637078
- HookerABLemmersMThurkowALSystematic review and meta-analysis of intrauterine adhesions after miscarriage: prevalence, risk factors and long-term reproductive outcomeHum Reprod Update201420226227824082042
- KjerJJAsherman syndrome in a Danish populationActa Obstet Gynecol Scand201493442542724484072
- ChenLZhangHWangQReproductive outcomes in patients with intrauterine adhesions following hysteroscopic adhesiolysis: experience from the largest women’s hospital in ChinaJ Minim Invasive Gynecol201724229930427856386
- TsapanosVSStathopoulouLPPapathanassopoulouVSTzingounisVAThe role of Seprafilm bioresorbable membrane in the prevention and therapy of endometrial synechiaeJ Biomed Mater Res2002631101411787023
- HookerABde LeeuwRvan de VenPMPrevalence of intrauterine adhesions after the application of hyaluronic acid gel after dilatation and curettage in women with at least one previous curettage: short-term outcomes of a multicenter, prospective randomized controlled trialFertil Steril201710751223123128390688
- ReinDTSchmidtTHessAPVolkmerASchöndorfTBreidenbachMHysteroscopic management of residual trophoblastic tissue is superior to ultrasound-guided curettageJ Minim Invasive Gynecol201118677477822024264
- Early pregnancy complication and abortion database [Danish] Available from: https://www.sundhed.dk/content/cms/67/4667_tigrab_aarsrapport_2017_offentlig.pdfAccessed March 13, 2019
- SharmaJBRoyKKPushparajMGenital tuberculosis: an important cause of Asherman’s syndrome in IndiaArch Gynecol Obstet20082771374117653564
- GoojhaCACaseAPiersonRDevelopment of Asherman syndrome after conservative surgical management of intractable postpartum hemorrhageFertil Steril20109431098.e11098.e520347081
- TongucEAVarTYilmazNBatiogluSIntrauterine device or estrogen treatment after hysteroscopic uterine septum resectionInt J Gynaecol Obstet2010109322622920152976
- PapoutsisDGeorgantzisDDaccòMDA rare case of Asherman’s syndrome after open myomectomy: sonographic investigations and possible underlying mechanismsGynecol Obstet Invest201477319420024557451
- SongDLiuYXiaoYLiT-CZhouFXiaEA matched cohort study comparing the outcome of intrauterine adhesiolysis for Asherman’s syndrome after uterine artery embolization or surgical traumaJ Minim Invasive Gynecol20142161022102824842805
- YuXYuhanLDongmeiSEnlanXTinchiuLThe incidence of postoperative adhesion following transection of uterine septum: a cohort study comparing three different adjuvant therapiesEur J Obstet Gynecol Reprod Biol2016201616427062103
- di Spiezio SardoACalagnaGScognamiglioMO’DonovanPCampoRde WildeRLPrevention of intrauterine post-surgical adhesions in hysteroscopy. A systematic reviewEur J Obstet Gynecol Reprod Biol201620318219227337414
- Roma DalfóAÚbedaBÚbedaADiagnostic value of hysterosal-pingography in the detection of intrauterine abnormalities: a comparison with hysteroscopyAJR Am J Roentgenol200418351405140915505312
- SoaresSRBarbosa dos ReisMMCamargosAFDiagnostic accuracy of sonohysterography, transvaginal sonography, and hysterosalpingography in patients with uterine cavity diseasesFertil Steril200073240641110685551
- StLRamsayPPiersonREndometrial thickness measured by ultrasound in women with uterine outlet obstruction due to intrauterine or upper cervical adhesionsHuman Reprod2008232306309
- SalleBGaucherandPde Saint HilairePRudigozRCTransvaginal sonohysterographic evaluation of intrauterine adhesionsJ Clin Ultrasound199927313113410064410
- BerridgeDLWinterTCSaline infusion sonohysterography: technique, indications, and imaging findingsJ Ultrasound Med20042319711214756358
- KimMJLeeYLeeCAccuracy of three dimensional ultrasound and treatment outcomes of intrauterine adhesion in infertile womenTaiwan J Obstet Gynecol201554673774126700995
- TesarikJMendoza-TesarikRMendozaNVirtual ultrasonographic hysteroscopy followed by conventional operative hysteroscopy, enabling pregnancyAm J Obstet Gynecol20172162188.e127640941
- LetterieGSHaggertyMFMagnetic resonance imaging of intrauterine synechiaeGynecol Obstet Invest199437166688125415
- BacelarACWilcockDPowellMWorthingtonBSThe value of MRI in the assessment of traumatic intra-uterine adhesions (Asherman’s syndrome)Clin Radiol199550280837867273
- YanLWangABaiRApplication of SonoVue combined with three-dimensional color power angiography in the diagnosis and prognosis evaluation of intrauterine adhesionEur J Obstet Gynecol Reprod Biol2016198687226799772
- MarchCMIsraelRMarchADHysteroscopic management of intrauterine adhesionsAm J Obstet Gynecol19781306653657637078
- HamouJSalat-BarouxJSieglerAMDiagnosis and treatment of intrauterine adhesions by microhysteroscopyFertil Steril19833933213266825866
- ValleRFSciarraJJIntrauterine adhesions: hysteroscopic diagnosis, classification, treatment, and reproductive outcomeAm J Obstet Gynecol19881586 Pt 1145914703381869
- The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Müllerian anomalies and intrauterine adhesionsFertil Steril19884969449553371491
- DonnezJNisolleMHysteroscopic adhesiolysis of intrauterine adhesions (Asherman syndrome)DonnezJAtlas of Laser Operative Laparoscopy and HysteroscopyLondon, UKParthenon Publishing Group1994305322
- WamstekerKDiagnostic hysteroscopy: technique and documentationSuttonCDDiamondMEndoscopic Surgery for GynecologistsLondon, UKWB Saunders1998511524
- NasrALAl-InanyHGThabetSMAboulgharMA clinicohysteroscopic scoring system of intrauterine adhesionsGynecol Obstet Invest200050317818111014950
- LiXWuLZhouYNew crosslinked hyaluronan gel for the prevention of intrauterine adhesions after dilation and curettage in patients with delayed miscarriage: a prospective, multicenter, randomized, controlled trialJ Minim Invasive Gynecol2019261949929678756
- TaskinOSadikSOnogluARole of endometrial suppression on the frequency of intrauterine adhesions after resectoscopic surgeryJ Am Assoc Gynecol Laparosc20007335135410924629
- MazzonIFavilliACoccoPDoes cold loop hysteroscopic myomectomy reduce intrauterine adhesions? A retrospective studyFertil Steril2014101129429824182410
- DabirashrafiHMohammadKMoghadami-TabriziNZandinejadKMoghadami-TabriziMIs estrogen necessary after hysteroscopic incision of the uterine septum?J Am Assoc Gynecol Laparosc1996346236259050699
- RoyKKNegiNSubbaiahMKumarSSharmaJBSinghNEffectiveness of estrogen in the prevention of intrauterine adhesions after hysteroscopic septal resection: a prospective, randomized studyJ Obstet Gynaecol Res20144041085108824612233
- HealyMWSchexnayderBConnellMTIntrauterine adhesion prevention after hysteroscopy: a systematic review and meta-analysisAm J Obstet Gynecol2016215326727527173082
- SugimotoODiagnostic and therapeutic hysteroscopy for traumatic intrauterine adhesionsAm J Obstet Gynecol19781315539547677196
- PabuçcuRAtayVOrhonEUrmanBErgünAHysteroscopic treatment of intrauterine adhesions is safe and effective in the restoration of normal menstruation and fertilityFertil Steril1997686114111439418714
- FernandezHGervaiseAde TayracROperative hysteroscopy for infertility using normal Saline solution and a coaxial bipolar electrode: a pilot studyHum Reprod20001581773177510920101
- NewtonJRMackenzieWEEmensMJJordanJADivision of uterine adhesions (Asherman’s syndrome) with the Nd-YAG laserBr J Obs Gyn1989961102104
- ChapmanRChapmanKThe value of two stage laser treatment for severe Asherman’s syndromeBr J Obstet Gynaecol199610312125612588968248
- IstreOBjoennesJNaessRHornbaekKFormanAPostoperative cerebral oedema after transcervical endometrial resection and uterine irrigation with 1.5% glycineLancet19943448931118711897934539
- Capella-AlloucSMorsadFRongières-BertrandCTaylorSFernandezHHysteroscopic treatment of severe Asherman’s syndrome and subsequent fertilityHum Reprod19991451230123310325268
- YamamotoNTakeuchiRIzuchiDHysteroscopic adhesiolysis for patients with Asherman’s syndrome: menstrual and fertility outcomesReprod Med Biol201312415916629662367
- BougieOLortieKShenassaHChenISinghSSTreatment of Asherman’s syndrome in an outpatient hysteroscopy settingJ Minim Invasive Gynecol201522344645025497164
- BroomeJDVancaillieTGFluoroscopically guided hysteroscopic division of adhesions in severe Asherman syndromeObstet Gynecol19999361041104310362178
- XuWZhangYYangYZhangSLinXEffect of early second-look hysteroscopy on reproductive outcomes after hysteroscopic adhesiolysis in patients with intrauterine adhesion, a retrospective study in ChinaInt J Surg201850495429203342
- RobinsonJKColimonLMSIsaacsonKBPostoperative adhesiolysis therapy for intrauterine adhesions (Asherman’s syndrome)Fertil Steril200890240941418571166
- DawoodAAl-TalibATulandiTPredisposing factors and treatment outcome of different stages of intrauterine adhesionsJ Obstet Gynaecol Can201032876777021050509
- OrhueAAEAzikenMEIgbefohJOA comparison of two adjunctive treatments for intrauterine adhesions following lysisInt J Gynaecol Obstet2003821495612834941
- ZikopoulosKAKolibianakisEMPlatteauPLive delivery rates in subfertile women with Asherman’s syndrome after hysteroscopic adhesiolysis using the resectoscope or the Versapoint systemReprod Biomed Online20048672072515169591
- MyersEMHurstBSComprehensive management of severe Asherman syndrome and amenorrheaFertil Steril201297116016422100167
- SalmaUXueMMd SayedASXuDEfficacy of intrauterine device in the treatment of intrauterine adhesionsBiomed Res Int201420145115
- MalhotraNBahadurAKalaivaniMMittalSChanges in endometrial receptivity in women with Asherman’s syndrome undergoing hysteroscopic adhesiolysisArch Gynecol Obstet2012286252553022535194
- JoharyJXueMZhuXXuDVeluPPEfficacy of estrogen therapy in patients with intrauterine adhesions: systematic reviewJ Minim Invasive Gynecol2014211445423933351
- ThomsonAJMAbbottJAKingstonALenartMVancaillieTGFluoroscopically guided synechiolysis for patients with Asherman’s syndrome: menstrual and fertility outcomesFertil Steril200787240541017109860
- LiuLHuangXXiaEZhangXLiTCLiuYA cohort study comparing 4 mg and 10 mg daily doses of postoperative oestradiol therapy to prevent adhesion reformation after hysteroscopic adhesiolysisHum Fertil20184817
- GuoJLiTCLiuYA prospective, randomized, controlled trial comparing two doses of oestrogen therapy after hysteroscopic adhesiolysis to prevent intrauterine adhesion recurrenceReprod Biomed Online201735555556128784336
- AcunzoGGuidaMPellicanoMEffectiveness of auto-cross-linked hyaluronic acid gel in the prevention of intrauterine adhesions after hysteroscopic adhesiolysis: a prospective, randomized, controlled studyHum Reprod20031891918192112923149
- LinXNZhouFWeiMLRandomized, controlled trial comparing the efficacy of intrauterine balloon and intrauterine contraceptive device in the prevention of adhesion reformation after hysteroscopic adhesiolysisFertil Steril2015104123524025936237
- MarchCMManagement of Asherman’s syndromeReprod Biomed Online2011231637621549641
- KilicSYukselBPinarliFAlbayrakABoztokBDelibasiTEffect of stem cell application on Asherman syndrome, an experimental rat modelJ Assist Reprod Genet201431897598224974357
- AlawadhiFDuHCakmakHTaylorHSBone marrow-derived stem cell (BMDSC) transplantation improves fertility in a murine model of Asherman’s syndromePLoS One201495e9666224819371
- WangJJuBPanCApplication of bone marrow-derived mesenchymal stem cells in the treatment of intrauterine adhesions in ratsCell Physiol Biochem20163941553156027614987
- GanLDuanHXuQHuman amniotic mesenchymal stromal cell transplantation improves endometrial regeneration in rodent models of intrauterine adhesionsCytotherapy201719560361628285950
- DomninaANovikovaPObidinaJHuman mesenchymal stem cells in spheroids improve fertility in model animals with damaged endometriumStem Cell Res Ther2018915029482664
- NagoriCBPanchalSYPatelHEndometrial regeneration using autologous adult stem cells followed by conception by in vitro fertilization in a patient of severe Asherman’s syndromeJ Human Reprod Sci201141434821772740
- SinghNMohantySSethTShankarMBhaskaranSDharmendraSAutologous stem cell transplantation in refractory Asherman’s syndrome: a novel cell based therapyJ Hum Reprod Sci201472939825191021
- SantamariaXCabanillasSCervellóIAutologous cell therapy with CD133+ bone marrow-derived stem cells for refractory Asherman’s syndrome and endometrial atrophy: a pilot cohort studyHum Reprod20163151087109627005892
- TanJLiPWangQAutologous menstrual blood-derived stromal cells transplantation for severe Asherman’s syndromeHum Reprod201631122723272927664218
- BaradwanSBaradwanABashirMAl-JaroudiDThe birth weight in pregnant women with Asherman syndrome compared to normal intrauterine cavity: a case-control studyMedicine20189732e1179730095642
- FriedmanADefazioJDecherneyASevere obstetric complications after aggressive treatment of Asherman syndromeObstet Gynecol19866768648673703411
- SieglerAMValleRFTherapeutic hysteroscopic proceduresFertil Steril19885056857013053254
- EngelbrechtsenLLanghoff-RoosJKjerJJIstreOPlacenta accreta: adherent placenta due to Asherman syndromeClin Case Rep20153317517825838908
- ThinkhamropJLaopaiboonMLumbiganonPProphylactic antibiotics for transcervical proceduresCochrane Database Syst Rev20073CD005637