Abstract
Background
The aim of this review is to discuss the role of aspirin for various conditions in women.
Methods
A nonsystematic review of articles published on PubMed® that examines the role of aspirin in women.
Results
Aspirin is associated with a significant reduction of stroke risk in women, which may be linked to age. However, despite this evidence, underutilization of aspirin in eligible women is reported. In women of reproductive age, it may also have a role to play in reducing early-onset preeclampsia and intrauterine growth restriction, and in the prevention of recurrent miscarriage in women with antiphospholipid antibodies; it may also reduce cardiovascular risk in associated systemic conditions such as lupus. Aspirin may reduce colorectal cancer risk in women, but its role in breast cancer warrants further data from controlled trials.
Conclusions
The risk–benefit threshold for aspirin use in women has been established for several conditions. Reasons why women are less likely to be prescribed aspirin have not been established, but the overall underuse of aspirin in women needs to be addressed.
Keywords:
Introduction
Aspirin has been available for over a century,Citation1 and to date, over 100 randomized clinical trials (RCTs) have established its efficacy and safety in men and women for the prevention of vascular conditions including acute myocardial infarction (MI), ischemic stroke, and peripheral arterial disease.Citation2 RCTs have also shown that aspirin reduces the risk of colorectal cancer recurrence in high-risk subjects,Citation3,Citation4 while observational studies have associated a decreased risk of colorectal adenomas with regular aspirin use.Citation5 A recently published, 20-year follow-up of randomized trials also found that low-dose aspirin reduced the incidence and mortality due to colorectal cancer in patients at no apparent increased risk for this malignancy.Citation6 Aspirin may also have a beneficial role in the prevention of breast, prostate, lung, stomach, and esophageal cancers.Citation7 Among women, aspirin may provide additional benefits in individuals at risk of preeclampsia, as was first postulated by Wallenburg et alCitation8 in 1986 and found in a number of RCTs thereafter,Citation9–Citation11 and in postmenopausal individuals with or at risk of osteoporosis, rheumatoid arthritis, or breast cancer.Citation12
Despite the compelling evidence that low-dose aspirin reduces morbidity and mortality in patients with cardiovascular disease (CVD), and numerous guidelines recommending its use,Citation13–Citation15 many eligible patients, especially women, are not receiving aspirin for this indication.Citation16–Citation18 Underutilization of aspirin may contribute to worsening morbidity, mortality, and health-related quality-of-life outcomes associated with vascular conditions in women compared with men.Citation18 The Women’s Health Initiative Observational Study (WHIOS), for example, which examined 8928 postmenopausal women with CVD, found that only 46% were taking aspirin. After 6.5 years of follow-up, however, adjusted aspirin use was associated with a significantly lower all-cause mortality (hazard ratio [HR]: 0.86; P = 0.04) and cardiovascular-related mortality (HR: 0.75; P = 0.01) in those women taking aspirin.Citation17 In addition to recommendations regarding the use of aspirin for the prevention of CVD and associated complications, numerous guidelines also recommend low-dose aspirin for women at risk of preeclampsia;Citation19–Citation21 but again, there is considerable variation in its use for this indication.Citation22
Aims and methods
The aim of this review is to discuss key issues in the use of aspirin for various conditions in women. A literature search was performed in Medline (PubMed®) using the title/abstract search terms “aspirin AND cardiovascular AND women” (n = 343), “aspirin AND women’s health study” (n = 29), “aspirin AND preeclampsia” (n = 14), “aspirin AND antiphospholipid syndrome” (n = 16), and “aspirin AND cancer AND women” (n = 88). Reviewed articles were limited to English-language publications, clinical trials, and meta-analyses, published within the last 5 years. All publications were manually searched. Articles of particular relevance known to the authors (including those earlier than 2005) have also been included. Although this approach may have introduced some bias, it ensured that key data published before 2005 were also included where relevant, such as the aspirin trials in CVD, but the focus of the article was the discussion of relatively recent data in women.
Cardiovascular disease
According to the American Heart Association, CVD was the cause of death in 432,709 US females in 2006, which was nearly twice that observed for death from all forms of cancer in women (N = 269,819).Citation23 Since 1984, the number of CVD deaths for females has exceeded those for males in the US.Citation23 The high incidence of CVD death among women has resulted in considerable interest in preventive interventions that have been evaluated specifically in women, and there is also increasing awareness among women about the impact of CVD, particularly in older women.Citation24,Citation25 Key studies providing data on the role for aspirin in preventing CVD include the Women’s Health study (WHS), The Nurses’ Health Study (NHS), the WHIOS, and the Antithrombotic Trialists’ (ATT) Collaboration.Citation17,Citation26–Citation29
The WHS, a double-blind RCT, evaluated the benefits of aspirin in the primary prevention of CVD in 39,876 apparently healthy women health professionals. During a follow-up of around 10 years, 477 first major cardiovascular events were confirmed in the aspirin group compared with 522 in the placebo group. While this represented a nonsignificant trend toward lower risk of major events associated with CVD by 9% (relative risk [RR]: 0.91, 95% confidence interval [CI]: 0.80–1.03; P = 0.13) with aspirin in the overall group, analysis by age indicated that aspirin significantly reduced major events in women aged ≥ 65 years (RR: 0.74, 95% CI: 0.59–0.92] in women aged ≥ 65 years vs (RR: 1.01, 95% CI: 0.81–1.26 in women aged 45–54 years). There was also a 34% reduction in the risk of MI in women aged ≥ 65 years (RR: 0.66, 95% CI: 0.44–0.97; P = 0.04). In addition, women taking aspirin experienced an overall 17% decrease in the risk of stroke (RR: 0.83, 95% CI: 0.69–0.99; P = 0.04), mostly due to significant reductions in ischemic stroke (RR: 0.76, 95% CI: 0.63–0.93; P = 0.009). The RR for stroke reduction was comparable across all age groups.Citation26
The NHS – a prospective study of 87,678 healthy female nurses in the age range 34–65 years and free of diagnosed CHD, stroke, and cancer at baseline – evaluated the association between regular aspirin use and the risk of a first MI and other cardiovascular events over 6 years. In this study, the use of 1–6 aspirin tablets per week was associated with a 32% reduced risk of a first MI among women (RR: 0.68, 95% CI: 0.52–0.89; P = 0.005).Citation27 Long-term, 24-year follow-up of this study showed that low-to-moderate doses of aspirin are associated with a 25% lower risk of all-cause mortality (RR: 0.75, 95% CI: 0.71–0.81) and a 38% reduced risk of CVD death (RR: 0.62, 95% CI: 0.55–0.71); these benefits were significant in older women and those with cardiac risk factors.Citation28 The WHIOS – an observational study to evaluate the relationship between aspirin use (81 or 325 mg) and clinical outcomes among postmenopausal women with stable CVD – found that aspirin use was associated with significantly lower risk of all-cause mortality, specifically cardiovascular mortality, among postmenopausal women with stable CVD.Citation17
Data from some of these key trials have been included in meta-analyses. The ATT CollaborationCitation29 was a meta-analysis of individual participant data on serious vascular events (MI, stroke, or vascular death) and major bleeds in six primary prevention trials (95,000 individuals at low average risk [~50,000 were women], 660,000 person-years, 3554 serious vascular events) and 16 secondary prevention trials (17,000 individuals at high average risk, 43,000 person-years, 3306 serious vascular events) that compared long-term aspirin vs control. Among women, the RR for primary prevention of a major coronary event was 0.95 (95% CI: 0.77–1.17); for ischemic stroke, 0.77 (95% CI: 0.59–0.99); and for a serious vascular event, 0.88 (95% CI: 0.76–1.01). In the secondary prevention trials among women, the RR for risk reduction for a major coronary event was 0.73 (95% CI: 0.51–1.03); for ischemic stroke, 0.91 (95% CI: 0.52–1.57); and for a serious vascular event, 0.81 (95% CI: 0.64–1.02). These findings clearly show that low-dose aspirin has an important role to play in the prevention of stroke, particularly in older women. This is important, as age-related stroke incidence is likely to increase dramatically in women compared with men over the next 40 years.Citation30 Stroke may also be linked (albeit rarely) to multiple pregnancies, eclampsia, the postpartum period, and migraine.Citation31
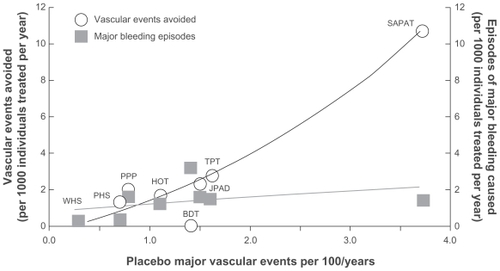
A number of cardiovascular studies have established the benefit–risk profile of aspirin use in a range of low-, medium- and high-risk patients, and in those with diabetes. The absolute benefit of treatment vs major bleeding risk in 1000 patients treated per year is illustrated in ,Citation32 which also indicates the position of the WHSCitation26 and in low-risk patients with diabetes enrolled in the Japanese Primary Prevention of Atherosclerosis with Aspirin for Diabetes (JPAD) study.Citation33 The vascular events avoided in women enrolled in the WHS vs major bleeds associated with aspirin treatment is in the bottom left-hand corner of the figure; this is largely due to the nonsignificant reduction of major cardiovascular events in this trial, but does not illustrate the benefits in terms of stroke reduction, where the threshold will be more favorable.Citation26 Largely as a result of the primary outcome of the WHS, the benefit–risk threshold and consequently the numbers needed to treat (NNT) to prevent one cardiovascular event is higher in women than in men when data are pooled in meta-analyses. In a meta-analysis of 95,456 subjects (51,342 women) from cardiovascular trials, the NNT to prevent one cardiovascular event was 333 for women and 270 men based on a mean follow-up of 6.4 years.Citation34
Figure 1 The absolute benefit (in terms of vascular events avoided/1000 treated/year) vs risks (major bleeds/1000 treated/year) associated with aspirin treatment in the key cardiovascular trials enrolling low-, medium-, and high-risk patients. Adapted with permission from the American College of Chest Physicians. Patrono C, et al. Platelet-active drugs: the relationships among dose, effectiveness, and side effects: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:234S–264S.
Cost-effectiveness of CVD prophylaxis with aspirin in women
Cost analyses in women are few, and are usually restricted to those that include sex as a subgroup. In general, these cost analyses have shown that aspirin is cost-effective in older women.Citation35 In one analysis, which predicted the number of cardiovascular events prevented with treatment, quality-adjusted life-years and cost over a 10-year period using a standard model, aspirin was found to be cost-effective as primary prevention in women aged > 65 years with high cardiovascular risk (10-year cardiovascular risk > 10%) and in women aged > 75 years with moderate cardiovascular risk (10-year cardiovascular risk > 15%).Citation36
Findings from single trials and meta-analyses have yielded similar results. One cost analysis of aspirin for primary prevention of cardiovascular events based on the findings from a single trial indicated a favorable cost–utility ratio for older women with moderate cardiovascular risk.Citation37 Similar findings were observed when the ATT Collaboration meta-analysis dataCitation29 were included in a model.Citation38
Guideline recommendations for CVD prevention in women
Based on findings from trials in women, there are now specific guidelines recommending the use of aspirin, mainly in stroke prevention and in high-risk women. The US Preventive Services Task Force (USPSTF) calculated the risk threshold (ie, the potential benefit of a reduction in ischemic strokes outweighs the potential harm of an increase in gastrointestinal [GI] hemorrhage) for aspirin use in stroke primary prevention at a risk level of 1%–20%.Citation15 For women aged 55–59 years, the 10-year stroke risk is 3%, and the benefits of stroke prevention outweigh the risk of a GI bleed; this increases to 8% in women aged 60–69 years and to 11% in women aged 70–79 years. The USPSTF guidelines have been endorsed by a panel of experts from the American Diabetes Association, the American Heart Association, and the American College of Cardiology Foundation.
The AHA’s Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women 2011 UpdateCitation39 specifies that aspirin 75–325 mg/day is recommended in high-risk women with CHD and is reasonable in women with diabetes unless contraindicated; aspirin 81 mg/day or 100 mg every other day can be considered in women aged ≥ 65 years, if blood pressure is controlled and benefits in terms of ischemic stroke and MI prevention are likely to outweigh the risk of GI bleeding and hemorrhagic stroke, and it appears cost-effective in women ≥ 65 years with moderate-severe CVD risk. Aspirin is recommended in women aged < 65 years, when benefit for ischemic stroke prevention is likely to outweigh adverse effects of therapy. Several guidelines also recommend aspirin for the prevention of stroke in women. Low-dose aspirin is recommended in women aged > 45 years (or < 65 years) who are not at increased risk for intracerebral hemorrhage and who have good GI tolerance.Citation14,Citation40 A number of other guidelines, including European guidelines, recommend the use of aspirin in patients with established CVD and in asymptomatic individuals at high risk of CVD, but do not specify different approaches for women.Citation41
Some studies have observed that women have greater residual platelet activity after high-dose aspirin compared with men treated with a lower dose of aspirin, suggesting that female patients may benefit from higher maintenance dosages or the use of alternative antiplatelet medications.Citation42–Citation44 Findings from the ATT Collaboration, however, show that the reduction in risk of major cardiovascular events is similar for men and women at similar doses, and thus, platelet reactivity may not justify differential dosing.Citation29
The expanding role of aspirin in obstetric conditions
Preeclampsia
Preeclampsia is a potentially fatal pregnancy-specific hypertensive syndrome affecting around 2%–8% of pregnancies.Citation45 For the unborn child, it is linked to poor intrauterine growth, prematurity, and sometimes death,Citation10,Citation45 and among mothers can lead to a spectrum of complications including eclampsia, stroke, (pulmonary) edema, and retinal problems. Preeclampsia/eclampsia is responsible for 10%–15% of direct maternal deaths, with intracranial hemorrhage as the most frequent cause. Reducing the occurrence of preeclampsia/eclampsia-related deaths is an important aspect of one of the World Health Organization Millennium Goals: to reduce the maternal mortality ratio by 75% between 1990 and 2015.Citation45,Citation46
In the long-term, preeclampsia among mothers is associated with an increased risk of developing CVD.Citation47 Indeed, a recent systematic analysis estimated that women with a history of preeclampsia/eclampsia have approximately double the risk of early cardiac, cerebrovascular, and peripheral arterial disease and cardiovascular mortality compared with women without such a history.Citation48 The reasons for this increased risk of CVD are unknown, but shared risk factors – including endothelial dysfunction, obesity, hypertension, hyperglycemia, insulin resistance, and dyslipidemia – have led to suggestions that metabolic syndrome may be an underlying mechanism common to CVDs and preeclampsia.Citation49 A recent systematic analysis of observational studies showed that women with a history of preeclampsia may also have an increased risk of microalbuminuria.Citation50
Children born to pregnancies complicated by preeclampsia and intrauterine growth restriction (IUGR) can also have long-term sequelae including type 2 diabetes mellitus, hypertension, and CVD.Citation51,Citation52 For example, the Helsinki Birth Cohort study, which examined 284 pregnancies complicated by preeclampsia and 1592 complicated by gestational hypertension, found that people born to mothers with these conditions were at increased risk of stroke (HR: 1.9; P = 0.01).Citation52 Mechanisms underlying the effects of preeclampsia and IUGR and long-term sequelae have not been elucidated, but proposals include fetal undernutrition, genetic susceptibility, and postnatal accelerated growth.Citation53 A potential role of epigenetic modifications in the process has also been suggested. Citation51 A recent study comparing normotensive IUGR cases vs 31 IUGR cases with preeclampsia suggested that IUGR is the key factor affecting cardiac function, rather than the preeclampsia itself.Citation54
The role of aspirin in preeclampsia
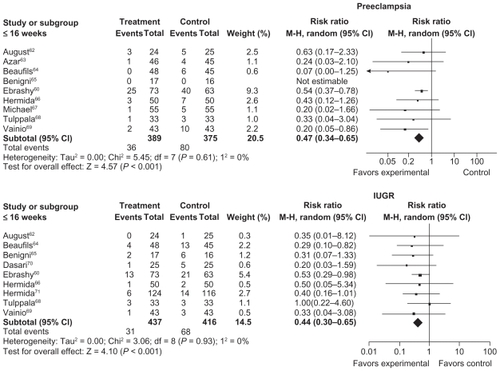
Causes of preeclampsia are not clear, but it is thought that individuals with preeclampsia have an imbalance of prostaglandin I2 (PG12) and thromboxane A2 (TXA2), which induces a vasoconstriction state. Aspirin is known to inhibit TXA2, a potent activator of platelet aggregation and vasoconstriction, thus reducing the balance between vasoconstriction and vasodilation. Findings from RCTs, observational studies and meta-analyses indicate that aspirin treatment initiated early in pregnancy is an efficient method of reducing the incidence of preeclampsia and its consequences ();Citation9,Citation10,Citation55–Citation60 only aspirin and calcium in a low-intake diet have been shown to have effects for the prevention of preeclampsia. Heparin or dalteparin and aspirin, however, may be superior to aspirin alone in women with inherited thrombophilias.Citation55
Table 1 Trials investigating the effects of aspirin on incidence of preeclampsia and fetal growth restriction
The most recent meta-analysis, which examined 27 studies involving 11,348 women, showed that low-dose aspirin was effective in reducing preeclampsia (RR: 0.47), severe preeclampsia (RR: 0.09), and IUGR (RR: 44) when used in early pregnancy (<16 weeks’ gestation) ().Citation61–Citation71 These findings support the results of earlier studies, including a meta-analysis of 14 trials involving 12,416 women, which showed that aspirin was beneficial in reducing perinatal death and preeclampsia, and increasing birth weight.Citation72 The benefits of aspirin in reducing blood pressure in pregnant women may also be linked to time of administration, with bedtime administration being more effective than at other times of day.Citation73 Findings from the Cochrane group, which have analyzed 59 trials to date (37,560 women), also suggest that the benefits of aspirin are greater in women at high risk of developing preeclampsia compared with low-risk women.Citation10 It may be important to develop a risk–benefit threshold in pregnant women based on risk factors for preeclampsia, safety issues (such as previous GI ulcers, Helicobacter pylori infection, etc), aspirin dose and timing, and duration of treatment. Preeclampsia could also be used to predict future increased risk of CVD, particularly hypertension, later in life,Citation74,Citation75 and could be introduced into risk calculation scores for women.
Figure 2 The effect of aspirin treatment on preeclampsia (A) and IUGR (B) in pregnant women (≤16 weeks’ gestation). Adapted with permission from Bujold E, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy Obstet Gynecol. 2010;116:402–414, with permission from LWW.
Despite the data supporting the use of aspirin in high-risk pregnancy, considerable variation in its use for this condition is observed.Citation22 To date, there are no accurate tests that are suitable for use in routine clinical practice to predict the likelihood of preeclampsia in women not at high risk.Citation76
Prevention of miscarriage in women with antiphospholipid syndrome
The antiphospholipid syndrome can lead to thrombosis, pregnancy loss, and pre-term delivery, particularly in patients with preeclampsia.Citation77 It has been postulated that a procoagulant state is induced in the antiphospholipid syndrome, which is mediated by TXA2 ().Citation77 Reduction of this thrombogenic state could explain the benefits associated with aspirin use in these patients. A number of studies (summarized in )Citation78–Citation85 have demonstrated that aspirin, either alone or in combination with heparin, prevents recurrent miscarriage in patients with antiphospholipid antibodies (APLAs); these studies suggest that aspirin plus unfractionated heparin is associated with better outcomes than aspirin alone or aspirin plus low-molecular-weight heparin.
Figure 3 Pathogenesis of thrombosis in antiphospholipid syndrome and the mode of action of aspirin and heparin.Citation77
Adapted from The Lancet, Published online September 6, 2010, Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA. Antiphospholipid syndrome. Copyright (2011), with permission from Elsevier.
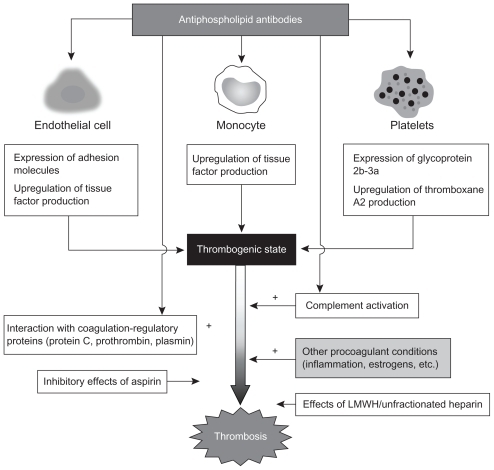
Table 2 Trials investigating the effect of aspirin on pregnancy outcomes in women with antiphospholipid syndrome
Based on these findings, the American College of Chest Physicians guidelines recommend aspirin plus heparin (unfractionated or low molecular weight) in pregnant patients with APLAs and a history of more than two early pregnancy losses or more than one late pregnancy loss, preeclampsia, IUGR, or abruption.Citation86 Aspirin in combination with heparin is also recommended in pregnant individuals without recurrent miscarriage and/or fetal loss if they are positive for APLAs and have a history of thromboembolism ().Citation77
Table 3 Suggested treatment regimens (involving aspirin) for conditions associated with antiphospholipid syndromeCitation77
Prevention in women with idiopathic recurrent miscarriage
Recurrent miscarriage (≥3 consecutive losses < 20 weeks postmenstruation) is a distressing problem that can affect as many as 0.5%–3% of fertile couples of reproductive age.Citation87 In many cases, no underlying cause (such as antiphospholipid syndrome) can be identified, and there is currently no treatment for this problem. A recently completed prospective study comparing patients with unexplained recurrent first-trimester pregnancy loss with matched control subjects found that those with unexplained recurrent miscarriage have significantly increased platelet aggregation in response to arachidonic acid.Citation87 The enhanced response to this agonist provides a strong rationale for the use of aspirin in management of this clinical condition. Small-scale trials investigating the use of aspirin in the prevention of recurrent miscarriage in women without antiphospholipid syndrome have so far found little benefit;Citation88 however, the findings regarding aggregation response to arachidonic acid lend support to reevaluating the benefit of aspirin in larger trials with a clearly defined cohort of individuals with recurrent miscarriage.
The expanding role of aspirin in chronic inflammatory disorders
Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) – an inflammatory rheumatic disease of immunologic origin characterized by autoantibody production, polyarthritis, and protean clinical manifestations – affects considerably more women than men.Citation89 Cardiovascular morbidity and mortality is a frequent complication of SLE, particularly in females aged 35–44 years, in whom the risk of MI is raised 50-fold.Citation90 Traditional cardiac risk factors – including hyperlipidemia, hypertension, and sedentary lifestyle – are all prevalent in patients with SLE, but cannot fully account for the magnitude of this increased risk, suggesting that SLE itself may also confer increased risk.Citation91 Conventional wisdom in the field is that cardiac risk factors should be aggressively treated in SLE, although there are limited data on the effectiveness of individual interventions. The benefits observed with aspirin in the reduction of cardiovascular events in non-SLE populations suggest that it may also benefit women affected by the condition, although further investigation is warranted; however, as APLAs may also be involved in the development of SLE, it is likely that aspirin could prevent the thrombogenic state, as described previously.Citation77
The potential role of aspirin in cancer
The potential role of aspirin in cancer prevention is based on more than 30 years of research, with beneficial effects being mainly observed in colorectal adenoma and cancer prevention.Citation7 Aspirin may exert its beneficial anticancer effects through inhibition of cyclooxygenase (COX)-1 in platelets or COX-1 and/or COX-2 in nucleated cells.Citation92 This will result in the inhibition of COX-derived products that are involved in angiogenesis (TXA2) or apoptosis (PGE2/PGE2 receptors). Non-COX-dependent pathways may include modulation of oncogenic factors (eg, NFκB), other pathways (eg, β-catenin), genetic alterations (eg, DNA), or energy depletion of tumor cells by phosphorylation.Citation93
Colorectal cancer
Colorectal cancer is a serious concern among both men and women. It is estimated that in 2010, there will be 102,900 new cases of colorectal cancer (49,470 in men and 53,430 in women) and 39,670 new cases of rectal cancer (22,620 in men and 17,050 in women).Citation94 A recent analysis of studies in primary and secondary prevention of vascular events, involving > 14,000 patients, found that low-dose aspirin (75 mg/day) reduced the long-term incidence and mortality due to colorectal cancer.Citation6 In this analysis, the reductions in incidence and death due to colorectal cancer were greater for proximal colon tumors than for distal colon or rectal tumors. This is an important finding, as regular screening with sigmoidoscopy or colonoscopy is not effective in preventing tumors in this location.Citation6 A further study using participants from the NHS (n = 83,767) showed that aspirin use was associated with 29% reduction in the risk of colorectal cancer in women.Citation95
Breast cancer
Breast cancer is a significant concern among many women. In the US in 2006, breast cancer claimed the lives of 40,821 females.Citation23 Nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, inhibit COX and thereby reduce prostaglandin synthesis. The observation that abnormally upregulated COX and prostaglandins are features of breast cancer suggests that aspirin may have potential value in treatment and prevention of the disease. Results investigating effects of aspirin on incidence of breast cancer are inconsistent, with some studies identifying reduced incidence of breast cancer in women taking aspirin vs those not taking aspirin, and others finding no effect ();Citation96–Citation103 given this lack of consistent findings, further investigation is warranted. A recent prospective observational study based on responses from 4164 female registered nurses in the NHS who were diagnosed with stages I–III breast cancer has indicated that among women living ≥ 1 year after a breast cancer diagnosis, aspirin use was associated with a decreased risk of distant recurrence and breast cancer death.Citation96
Table 4 Trials investigating the effects of aspirin on breast cancer
Endometrial cancer
Although no prospective studies to date have explored the relationship between the use of aspirin, other NSAIDs, and acetaminophen and endometrial adenocarcinoma, data from a prospective cohort study suggest that while use of aspirin or other NSAIDs do not play important roles in endometrial cancer risk overall, risk is significantly lower for current aspirin users who are obese or who were postmenopausal and had never used postmenopausal hormones.Citation104 The potential effects of aspirin in these subgroups warrant further investigation.
Conclusion
Aspirin has a clear role in the secondary prevention of CVD in individuals. Although initial trials with aspirin had limited representation of women, subsequent large-scale, long-term studies have confirmed the relevance of the findings in women. RCTs and cohort studies show that aspirin is also consistent in reducing the risk of first events in appropriate patients and support the benefit–risk profile of aspirin in primary prevention. Beyond CVD, however, aspirin may provide additional benefits in women. Numerous trials have indicated the benefits of aspirin for preeclampsia, in reducing IUGR, and in preventing miscarriage in pregnant women with APLAs. Trials also suggest that there may be benefits for individuals diagnosed with breast cancer, although these findings require confirmation in larger, long-term studies. The low rates of uptake of aspirin among women in whom it is indicated remains a concern given the role of CVD in death among women. Reasons why women are less likely to have been prescribed aspirin have not been established, but the overall underuse of aspirin in women needs to be addressed. Although aspirin use in women is recommended in a number of CVD prevention guidelines, it is possible that the development of more extensive guidelines specific to women’s issues could address some of these concerns. A number of ongoing trials are looking at the role of aspirin in women only studies; these include breast cancer (in women on tamoxifen therapy), in preeclampsia (in combination with enoxaparin or progesterone), and in recurrent miscarriage (in combination with folic acid, steroids, or heparin).
Acknowledgment
Editorial assistance was funded by Bayer, Berlin, Germany.
Disclosure
The authors report no conflicts of interest in this work.
References
- JackDBA hundred years of aspirinLancet19973504374399259670
- PatronoCRoccaBAspirin: promise and resistance in the new millenniumArterioscler Thromb Vasc Biol200828s25s3218174450
- SandlerRSHalabiSBaronJAA randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancerN Engl J Med200334888389012621132
- BaronJAColeBFSandlerRSA randomized trial of aspirin to prevent colorectal adenomasN Engl J Med200334889189912621133
- ThunMJHenleySJPatronoCNonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issuesJ Natl Cancer Inst20029425226611854387
- RothwellPMWilsonMElwinCELong-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of 5 randomised trialsLancet20103761741175020970847
- CuzickJOttoFBaronJAAspirin and non-steroidal anti- inflammatory drugs for cancer prevention: an international consensus statementLancet Oncol20091050150719410194
- WallenburgHCDekkerGAMakovitzJWLow-dose aspirin prevents pregnancy-induced hypertension and pre-eclampsia in angiotensin-sensitive primigravidaeLancet19861132867260
- AskieLMDuleyLHenderson-SmartDJAntiplatelet agents for prevention of pre-eclampsia: a meta-analysis of individual patient dataLancet20073691791179817512048
- DuleyLHenderson-SmartDJMeherSAntiplatelet agents for preventing pre-eclampsia and its complicationsCochrane Database Syst Rev20072CD00465917443552
- DekkerGSibaiBPrimary, secondary, and tertiary prevention of pre- eclampsiaLancet200135720921511213110
- ShiSYamazaTAkiyamaKIs Aspirin treatment an appropriate intervention to osteoporosis?Fut Rheumatol2008349950220428329
- MarshallTEvaluating national guidelines for prevention of cardiovascular disease in primary careJ Eval Clin Pract20051145246116164586
- BeckerRCMeadeTWBergerPBThe primary and secondary prevention of coronary artery disease: American College of Chest Physicians Evidence-based Clinical Practice Guidelines (8th Ed)Chest20081336 Suppl776S814S18574278
- US Preventive Services Task ForceAspirin for the prevention of CVD: US Preventive Services Task Force recommendation statementAnn Intern Med200915039640419293072
- CannonCPRheeKECaliffRMCurrent use of Aspirin and antithrombotic agents in the United States among outpatients with atherothrombotic disease (from the REduction of Atherothrombosis for Continued Health [REACH] Registry)Am J Cardiol201010544545220152237
- BergerJSBrownDLBurkeGLAspirin use, dose, and clinical outcomes in postmenopausal women with stable CVD: the Women’s Health Initiative Observational StudyCirc Cardiovasc Qual Outcomes20092788720031819
- EnriquezJRPratapPZbilutJPWomen tolerate drug therapy for coronary artery disease as well as men do, but are treated less frequently with aspirin, beta-blockers, or statinsGend Med20085536118420166
- BrenneckeSPBrownMACrowtherCAAspirin and prevention of preeclampsia. Position statement of the use of low-dose aspirin in pregnancy by the Australasian Society for the Study of Hypertension in PregnancyAust N Z J Obstet Gynaecol19953538417771997
- VisintinCMugglestoneMAAlmerieMQManagement of hypertensive disorders during pregnancy: summary of NICE guidanceBMJ2010341c220720739360
- Société française d’anesthésie et de réanimation (Sfar); Collège national des gynécologues et obstétriciens français (CNGOF); Société française de médecine périnatale (SFMP); Société française de néonatalogie (SFNN)Multidisciplinary management of severe pre-eclampsia (PE). Experts’ guidelines 2008. Société française d’anesthésie et de réanimation. Collège national des gynécologues et obstétriciens français. Société française de médecine périnatale. Société française de néonatalogieAnn Fr Anesth Reanim200928275281 French19321292
- ChappellLCSeedPEnyeSClinical and geographical variation in prophylactic and therapeutic treatments for pre-eclampsia in the UKBJOG201011769570020175876
- AHA Women and CVD – Statistics 2010 Available at: http://www.americanheart.org/downloadable/heart/1260905040318FS10WM10.pdfAccessed June 29, 2010
- MoscaLMochari-GreenbergerHDolorRJTwelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart healthCirc Cardiovasc Qual Outcomes2010312012720147489
- VerheugtFWSmithSCJrThe lady aspirin for cardiovascular diseaseLancet20053661148115016198753
- RidkerPMCookNRLeeIMA randomized trial of low-dose aspirin in the primary prevention of CVD in womenN Engl J Med20053521293130415753114
- MansonJEStampferMJColditzGAA prospective study of aspirin use and primary prevention of CVD in womenJAMA19912665215272061978
- ChanATMansonJEFeskanichDLong-term aspirin use and mortality in womenArch Intern Med200716755625672
- Antithrombotic Trialists’ (ATT) CollaborationAspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trialsLancet20093731849186019482214
- ReevesMJBushnellCDHowardGSex differences in stroke: epidemiology. Clinical presentation, medical care, and outcomesLancet Neurol2008791592618722812
- KurthTBousserM-GStroke in women: an evolving topicStroke2009401027102819211478
- PatronoCCollerBGarretAPlatelet-active drugs: the relationships among dose, effectiveness, and side effects: the Seventh ACCP Conference on Antithrombotic and Thrombolytic TherapyChest2004126234S264S15383474
- OgawaHNakayamaMMorimotoTLow-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trialJAMA20083002134214118997198
- BergerJSRoncaglioniMCAvanziniFAspirin for the primary prevention of cardiovascular events in women and men. A sex-specific meta-analysis of randomized controlled trialsJAMA200629530631316418466
- HillegassWBDorfmanTAAspirin was cost-effective for primary prevention of cardiovascular events in older women at moderate riskACP J Club20071472417608389
- GrevingJPBuskensEKoffijbergHCost-effectiveness of aspirin treatment in the primary prevention of cardiovascular disease events in subgroups based on age, gender, and varying cardiovascular riskCirculation20081172875288318506010
- PignoneMEarnshawSPletcherMJAspirin for the primary prevention of CVD in women: a cost-utility analysisArch Intern Med200716729029517296886
- AlgraAGrevingJPAspirin in primary prevention: sex and baseline risk matterLancet20093731821182219482200
- MoscaLBenjaminEJBerraKEffectiveness-based guidelines for the prevention of cardiovascular disease in women 2011 Update: a guideline from the American Heart AssociationCirculation20111231243126221325087
- European Stroke OrganisationGuidelines for management of ischemic stroke and transient ischaemic attack 2008Cerebrovasc Dis20082545750718477843
- De BackerGAmbrosioniEBorch-JohnsenKEuropean guidelines on CVD prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical PracticeEur Heart J2003241601161012964575
- ZuernCSLindemannSGawazMPlatelet function and response to aspirin: gender-specific features and implications for female thrombotic risk and managementSemin Thromb Hemost20093529530619452405
- QayyumRBeckerDMYanekLRPlatelet inhibition by aspirin 81 and 325 mg/day in men versus women without clinically apparent cardiovascular diseaseAm J Cardiol20081011359136318435972
- BeckerDMSegalJVaidyaDSex differences in platelet reactivity and response to low-dose aspirin therapyJAMA20062951420142716551714
- DuleyLThe global impact of pre-eclampsia and eclampsiaSemin Perinatol20093313013719464502
- World Health Organization2010Millennium Development Goals Available at: http://www.who.int/topics/millennium_development_goals/maternal_health/en/index.htmlAccessed November 17, 2010
- HudaSSFreemanDJNelsonSMShort- and long-term strategies for the management of hypertensive disorders of pregnancyExpert Rev Cardiovasc Ther200971581159419954320
- McDonaldSDMalinowskiAZhouQCardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analysesAm Heart J200815691893019061708
- HarskampREZeemanGCPreeclampsia: at risk for remote cardiovascular diseaseAM J Med Sci200733429129518030186
- McDonaldSDHanZWalshMWKidney disease after preeclampsia: a systematic review and meta-analysisAm J Kidney Dis2010551026103920346562
- XuXFDuLZEpigenetics in neonatal diseasesChin Med J (Engl)20101232948295421034612
- KajantieEErikssonJGOsmondCPre-eclampsia is associated with increased risk of stroke in the adult offspring. The Helsinki Birth Cohort StudyStroke2009401176118019265049
- GeelhoedJJJaddoeVWEarly influences on cardiovascular and renal developmentEur J Epidemiol20102567769220872047
- CrispiFComasMHernández-AndradeEDoes pre-eclampsia influence fetal cardiovascular function in early-onset intrauterine growth restriction?Ultrasound Obstet Gynecol20093466066519827117
- LeducLDuboisETakserLDalteparin and low-dose aspirin in the prevention of adverse obstetric outcomes in women with inherited thrombophiliaJ Obstet Gynaecol Can20072978779317915061
- BujoldEMorencyAMRobergeSAcetylsalicylic acid for the prevention of preeclampsia and intra-uterine growth restriction in women with abnormal uterine artery Doppler: a systematic review and meta- analysisJ Obstet Gynaecol Can20093181882619941706
- LambersMJGroeneveldEHoozemansDALower incidence of hypertensive complications during pregnancy in patients treated with low-dose aspirin during in vitro fertilization and early pregnancyHum Reprod2009242447245019608566
- UrbanGVerganiPTironiRAntithrombotic prophylaxis in multiparous women with preeclampsia or intrauterine growth retardation in an antecedent pregnancyInt J Fertil Womens Med200752596718320863
- RuanoRFontesRSZugaibMPrevention of preeclampsia with low-dose aspirin – a systematic review and meta-analysis of the main randomized controlled trialsClinics (Sao Paulo)20056040741416254678
- EbrashyAIbrahimMMarzookAUsefulness of aspirin therapy in high-risk pregnant women with abnormal uterine artery Doppler ultrasound at 14–16 weeks pregnancy: randomized controlled clinical trialCroat Med J20054682683116158479
- BujoldERobergeSLacasseYPrevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancyObstet Gynecol201011640241420664402
- AugustPHelsethGEdersheimTSustained release, low-dose aspirin ameliorates but does not prevent preeclampsia (PE) in a high risk populationProceedings of the 9th International Congress, International Society for the Study of HypertensionMarch 15–18, 1994Sydney, AustraliaHypertension in Pregnancy72
- AzarRTurpinDEffect of antiplatelet therapy in women at high risk for pregnancy-induced hypertensionProceedings of 7th World Congress of Hypertension in PregnancyOctober 1990Perugia, Italy257
- BeaufilsMUzanSDonsimoniRPrevention of pre-eclampsia by early antiplatelet therapyLancet198518408422858710
- BenigniAGregoriniGFruscaTEffect of low-dose aspirin on fetal and maternal generation of thromboxane by platelets in women at risk for pregnancy-induced hypertensionN Engl J Med19893213573622664523
- HermidaRCAyalaDEIglesiasMTime-dependent effects of low-dose aspirin administration on blood pressure in pregnant womenHypertension1997305895959322987
- MichaelCAWaltersBNJLow-dose aspirin in the prevention of pre-eclampsia: current evaluationTeohESRatnamSSMacnaughtonMCMaternal physiology and pathology. The current status of gynaecology and obstetrics seriesCarnforth, UKParthenon Publishing Group Ltd1992183189
- TulppalaMMarttunenMSoderstrom-AnttilaVLow-dose aspirin in prevention of miscarriage in women with unexplained or autoimmune related recurrent miscarriage: effect on prostacyclin and thromboxane A2 productionHum Reprod199712156715729262298
- VainioMKujansuuEIso-MustajarviMLow dose acetylsalicylic acid in prevention of pregnancy-induced hypertension and intrauterine growth retardation in women with bilateral uterine artery notchesBr J Obstet Gynecol2002109161167
- DasariRNarangAVasishtaKEffect of maternal low dose aspirin on neonatal platelet functionIndian Pediatr19983550751110216644
- HermidaRCAyalaDEFernandezJRAdministration time-dependent effects of aspirin in women at differing risk for preeclampsiaHypertension1999341016102310523401
- CoomarasamyAHonestHPapaioannouSAspirin for prevention of preeclampsia in women with historical risk factors: a systematic reviewObstet Gynecol20031011319133212798543
- HermidaRCAyalaDEIglesiasMAdministration time-dependence influence of aspirin on blood pressure in pregnant womenHypertension2003413 Pt 265165612623974
- CraiciIWagnerSGarovicVDPreeclampsia and future cardiovascular risk: formal risk factor or failed stress test?Ther Adv Cardiovasc Dis2008224925919124425
- HertigAWatnickSStevensHHow should women with pre-eclampsia be followed up? New insights from mechanistic studiesNat Clin Pract Nephrol2008450350918628742
- MeadsCACnossenJSMeherSMethods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modellingHealth Technol Assess200812iiiiv1270
- Ruiz-IrastorzaGCrowtherMBranchWAntiphospholipid syndromeLancet20103761498150920822807
- MakACheungMWCheakAACombination of heparin and aspirin is superior to aspirin alone in enhancing live births in patients with recurrent pregnancy loss and positive anti-phospholipid antibodies: a meta-analysis of randomized controlled trials and meta-regressionRheumatology (Oxford)20104928128819965971
- BramhamKHuntBJGermainSPregnancy outcome in different clinical phenotypes of antiphospholipid syndromeLupus201019586419897518
- ZiakasPDPavlouMVoulgarelisMHeparin treatment in antiphospholipid syndrome with recurrent pregnancy loss: a systematic review and meta-analysisObstet Gynecol20101151256126220502298
- CohnDMGoddijnMMiddeldorpSRecurrent miscarriage and antiphospholipid antibodies: prognosis of subsequent pregnancyJ Thromb Haemost201082208221320704646
- LaskinCASpitzerKAClarkCALow molecular weight heparin and aspirin for recurrent pregnancy loss: results from the randomized, controlled HepASA trialJ Rheumatol20093627928719208560
- DendrinosSSakkasEMakrakisELow-molecular-weight heparin versus intravenous immunoglobulin for recurrent abortion associated with antiphospholipid antibody syndromeInt J Gynaecol Obstet200910422322519116178
- GoelNTuliAChoudhryRThe role of aspirin versus aspirin and heparin in cases of recurrent abortions with raised anticardiolipin antibodiesMed Sci Monit200612CR13213616501426
- EmpsonMLassereMCraigJPrevention of recurrent miscarriage for women with antiphospholipid antibody or lupus anticoagulantCochrane Database Syst Rev200518CD00285915846641
- BatesSMGreerIAHirshJUse of antithrombotic agents during pregnancy: the Seventh ACCP Conference on Antithrombotic and Thrombolytic TherapyChest2004126S Suppl627S644S15383488
- FloodKPeaceAKentEPlatelet reactivity and pregnancy lossAm J Obstet Gynecol2010203281e1e520684942
- KaandorpSDi NisloMGoddijnMAspirin or anticoagulants for treating recurrent miscarriage in women without antiphospholipid syndromeCochrane Database Syst Rev2009CD00473419160241
- McCartyDJManziSMedsgerTAJrIncidence of systemic lupus erythematosus. Race and gender differencesArthritis Rheum199538126012707575721
- HaqueSBruceINTherapy insight: systemic lupus erythematosus as a risk factor for cardiovascular diseaseNat Clin Pract Cardiovasc Med2005242343016119705
- CostenbaderKHKarlsonEWGallVBarriers to a trial of atherosclerosis prevention in systemic lupus erythematosusArthritis Rheum20055371872316208639
- MarkowitzSDAspirin and colon cancer-targeting prevention?N Engl J Med20073562195219817522404
- SchrörKAcetylsalicylic AcidWeinheim, GermanyWiley-Blackwell2009
- American Cancer SocietyCancer Facts and Figures 2010Atlanta, GaAmerican Cancer Society2010 Available at: http://www.cancer.org/acs/groups/content/@nho/documents/document/acspc-024113.pdfAccessed November 15, 2010
- WeiEKColditzGAGiovannucciELCumulative risk of colon cancer up to age 70 years by risk factor status using data from the Nurses’ Health StudyAm J Epidemiol200917086387219723749
- HolmesMDChenWYLiLAspirin intake and survival after breast cancerJ Clin Oncol2010281467147220159825
- BardiaAOlsonJEVachonCMEffect of aspirin and other NSAIDs on postmenopausal breast cancer incidence by hormone receptor status: results from a prospective cohort studyBreast Cancer Res Treat201112614915520669045
- McTiernanAWangCYSorensenBNo effect of aspirin on mammographic density in a randomized controlled clinical trialCancer Epidemiol Biomarkers Prev2009181524153019423529
- ZhaoYSZhuSLiXWAssociation between NSAIDs use and breast cancer risk: a systematic review and meta-analysisBreast Cancer Res Treat200911714115018979210
- TakkoucheBRegueira-MéndezCEtminanMBreast cancer and use of nonsteroidal anti-inflammatory drugs: a meta-analysisJ Natl Cancer Inst20081001439144718840819
- ZhangSMCookNRMansonJELow-dose aspirin and breast cancer risk: results by tumour characteristics from a randomised trialBr J Cancer20089898999118268496
- MangiapaneSBlettnerMSchlattmannPAspirin use and breast cancer risk: a meta-analysis and meta-regression of observational studies from 2001 to 2005Pharmacoepidemiol Drug Saf20081711512417955496
- CookNRLeeIMGazianoJMLow-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized trialJAMA2005294475515998890
- ViswanathanANFeskanichDSchernhammerESAspirin, NSAID, and acetaminophen use and the risk of endometrial cancerCancer Res2008682507251318381460