Abstract
Background
Breast cancer is an important public health problem worldwide. This study aimed to assess the effectiveness of an educational intervention based on fear appeals using the extended parallel process model (EPPM) to improve attitudes, intention, and early breast cancer diagnosis in Iranian women.
Methods
This was a cluster-randomized trial conducted in Tehran, Iran. A sample of women 40 years old and above was recruited and assigned either to intervention group or to control group. The intervention group received two pamphlets containing fear appeals specially designed for this study using the EPPM. The control group received nothing. The primary outcomes were changes in attitude, behavioral intention, and early breast cancer diagnosis. Participants responded to a questionnaire before intervention and at 3 months follow-up assessments. Independent t-tests and paired t-tests were used for comparison.
Result
In all, 600 women were entered into the study (277 in the intervention group and 323 in the control group). Of these, 162 were lost to follow-up assessment. Thus, the analysis was restricted to those for whom both baseline and follow-up information was available (n=438). The mean age of participants was 53.2 (SD=9.45) years, and the mean year education of participants was 9.4 (SD=4.12) years. There were no significant differences between two groups regarding demographic variables. However, comparing outcome variables (attitude, intention, and early breast cancer diagnosis) at baseline and follow-up assessments, we found that the intervention group showed significant improvements in attitude and intention (P=0.01 and P=0.001, respectively), but no significant improvement was observed for early breast cancer diagnosis (P=0.78). The control group did not show any changes.
Conclusion
The findings showed that fear appeals could not influence early breast cancer diagnosis among women. However, significant changes were observed for attitude and behavioral intention.
Introduction
Breast cancer is the most common cancer among women both in developed and developing countries.Citation1–Citation6 Each year 1.5 million women are diagnosed with breast cancer and ~15% die from the disease globally.Citation7 Thus, early detection of breast cancer is of paramount importance. Several strategies exist for early detection of breast cancer including raising awareness among women especially those who are at higher risk of the disease.Citation1,Citation8–Citation12 As such, providing necessary information to encourage women for early breast cancer diagnosis is a routine practice by health professionals worldwide.Citation6,Citation13–Citation17 It is argued that awareness might persuade women to take appropriate actions toward breast cancer care.Citation10–Citation12,Citation18–Citation20 However, studies showed that the effectiveness of health education interventions and health messages highly depends on whether they are theory-driven or not.Citation21–Citation24 Indeed, using persuasive messages applying fear appeals in attempt to influence women’s behaviors toward early breast cancer diagnosis is common in health education and health promotion programs.Citation11,Citation25–Citation35 The most recent development in this area backs to year 1992 where the extended parallel process model (EPPM) was proposed. The model argues that a fear appeal might work if certain conditions exist that include susceptibility and severity, self-efficacy, and response efficacy.Citation11,Citation33,Citation36–Citation41
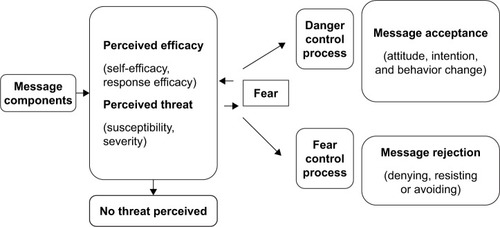
Susceptibility refers to one’s perception to vulnerability to the risk (eg, all women are prone to breast cancer). Severity refers to seriousness of the consequences if the recommended suggestions are not followed (eg, breast cancer is a fatal and serious disease and affects your family life and work). Self-efficacy refers to a person’s belief about his/her ability to follow the recommended suggestions successfully (eg, women can learn about early breast cancer diagnosis and manage their time to accomplish annual clinical breast examination). Response efficacy refers to beliefs about the effectiveness of the recommended suggestions to avert the threat (eg, annual clinical breast examination helps in early detection of breast cancer and thus a successful treatment).Citation32,Citation34,Citation35,Citation38,Citation39,Citation42,Citation43 The schematic picture of the EPPM is illustrated in .
The current study was an attempt to use the EPPM to encourage Iranian women to take necessary actions toward early detection of breast cancer. Breast cancer in Iran is increasing rapidly and unfortunately kills many women due to late diagnosis and poor treatment.Citation1,Citation2,Citation5,Citation8,Citation9,Citation12,Citation13,Citation16,Citation44–Citation48 It was hoped that the study results could help to improve women’s health in general and breast care in particular.
Methods
Trial design
This was a cluster-randomized trial with two parallel groups (intervention and control). This was chosen to avoid contamination between intervention and control groups.Citation49–Citation51 Data were collected at baseline and 3 months after intervention. The study started at the beginning of October 2017. After about 3 months, follow-up assessments started at December 29, 2017.
Study setting
The study was conducted in Tehran, Iran. Tehran, a metropolitan city, is the capital of Iran and has a multicultural composite.
Participants
Eligible cases for this study were women who were at least 40 years old, could read and write, did not have a history of breast cancer herself or in her first-degree family, and did not have psychiatric disorders. Women were excluded if they did not meet the inclusion criteria.
Intervention
The intervention group received two pamphlets as educational materials, which were designed based on the EPPM. It is believed that written materials are the most commonly used, cost-effective, and time-efficient approach to communicate health messages.Citation11,Citation25,Citation40,Citation52
As explained before, the EPPM constructs are perceived threat (susceptibility and severity) and perceived efficacy (self-efficacy and response efficacy). Pamphlets contained messages designed based on these constructs and described about severity and hardness of the disease, and its painful and difficult outcomes on patients and their family, work, and community. A short clarification about cure modalities including surgery and chemotherapy was explained to make women conscious about the consequences of delay in seeking behaviors for breast cancer symptoms. In susceptibility section, it was explained that breast cancer is rising in Iran and all women are vulnerable in developing breast cancer, and some critical signs of breast cancer were demonstrated. Also it was announced that early diagnosis might proceed to favorable medication. The next part included response efficacy that explained visiting a physician when women see any signs and conducting annual clinical breast cancer examination are useful and effective behaviors in early detection of the disease. The last part presented self-efficacy messages that prescribed women to gain knowledge about breast cancer and arrange their time to do recommended behaviors. Also it was explained that the suggested behaviors are uncomplicated, effortless, and easily done. In assessing the content, a number of health education specialists and 15 women (who were similar to the study samples and were not included in the study) read and examined the pamphlets to make sure that the designed messages were simple, understandable, and frightening. The two pamphlets were organized differently in literature and pictures.
Control
The participants were allocated into control group at the study commence. They did not receive anything. This group received educational materials used in this study (pamphlets) after completion of the study.
Outcomes
Attitude, behavioral intention, and behavior scores were the primary outcomes and evaluated at baseline and 3 months follow-up by a questionnaire.
Measures
A questionnaire was designed specifically for the study in order to measure the study outcomes. The instrument consisted of the following sections:
Demographic characteristics: including items on age, education, employment, and marital status.
Attitude: it consisted of 15 questions on women’s belief and emotions about early breast cancer diagnosis and its importance with a five-point Likert scale response category ranging from completely agree to completely disagree. These were coded from 5 to 1, respectively. Then, overall attitude score was calculated by summing all items scored, giving a score ranging from 15 to 75. The higher score indicates the more positive attitude toward early breast cancer diagnosis.
Behavioral intention: two questions on women’s desire and wishes to attend for annual clinical breast cancer examination and physician visit when they see any sign in their breast. The response categories were “agree, no idea, and do not agree.” These were coded as 2, 1, and 0, respectively. Then, overall behavioral intention score was calculated by summing all items scored, giving a score ranging from 0 to 4. The higher score indicates the more positive behavioral intention toward early breast cancer diagnosis.
Behavior: two statements made the last part of the measure. Women were asked to answer whether they attended for annual clinical breast cancer examination and visited physician when they see an unusual sign in their breast. The response choices were “Yes, I do and No, I do not”, corresponding to 1 and 0 scores, respectively. Then, overall behavior score was calculated by summing all items scored, giving a score ranging from 0 to 2. The higher score indicates better behavior in women toward early breast cancer diagnosis.
To assess validity of the questionnaire, content and face validity were performed. Also reliability of the questionnaire was evaluated by Cronbach’s alpha coefficient.
Sample size
Randomized block stratum was used in this study to achieve enough sample size. Tehran has 22 districts. Each district was considered as a stratum. Then within each stratum a number of blocks (clusters) were selected. Randomization was used to allocate the study groups (intervention or control). The number of clusters were related to population size of each district (stratum). There were more blocks in populated districts. Accordingly, a sample of 300 women in each study group (intervention and control) was estimated to achieve 80% power at 0.05 significance level. There were 29 clusters in intervention group and 35 clusters in control group. Ten women were estimated for each group based on experiments and near blocks added for sampling when the numbers of samples were not enough.Citation53–Citation56 Distribution-based clustering was used in this study.Citation57 presents the sampling construction.
Table 1 The study sample size and clusters in 22 districts in Tehran, Iran
Recruitment
Study samples were assigned to the two trial arms in equal quantities. The research team presented the allocation before home visits.
Sequence generation
To allocate blocks randomly as intervention or control groups, the Excel software was used. Some directions were applied to get the intended number of samples in the study. Tehran has 22 districts, which vary in socioeconomic and cultural status, so the study was conducted in all these parts. According to every district’s partake of all samples, some blocks were located and assigned as intervention or control randomly.
Implementation
Blocks were assigned as intervention or control by a statistician who did not take part in the study. Some skilled female interviewers learned about the study and were trained on how to collect data with the questionnaire. At first, they enacted home visits in selected parts (blocks), described the study intention, and made sure about inclusion criteria. Participants completed the written consent, and their phone number was taken for follow-up assessments. Participants were assured for confidentiality in the study. Research team monitored all study stages carefully to ascertain for correct implementation.
Blinding
No blinding was used in this study.
Statistical analysis
First, we calculated attitude, intention, and behavior scores for each respondent. As such, the score for attitude ranged from 15 to 75, for intention it ranged from 0 to 4, and for behavior it ranged from 0 to 2. In all instances, the higher scores indicated better conditions. Then, data from baseline and follow-up assessments were analyzed using mean and standard deviations, percentages, chi-square, t-test, and paired t-test. Finally, logistic regression analysis was performed using adjusted difference-in-difference analyses. In doing so, the follow-up scores were treated as dependent variables while baseline level of the outcomes and other individual characteristics were considered as independent variables.
Ethics
The study was conducted in accordance with the Declaration of Helsinki and the ethics committee of Tarbiat Modares University approved the study. All participants were asked to sign an informed consent form, and they were assured that all information provided would be kept confidential.
Results
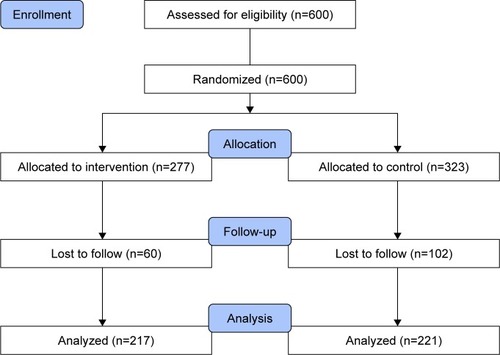
In all, 600 women were entered into the study (277 participants in intervention and 323 participants in control group). However, at follow-up, a number of participants were missed due to change in address (n=100) and dislike (n=62), giving 438 participants for whom both baseline and follow-up data were available for analysis (217 in intervention group and 221 in control group). The study flowchart is shown in . The mean age of participants was 53.2 (SD=9.45) years. There were no significant differences between the study groups with regard to age, education, employment, and marital status. The findings are shown in .
Table 2 Demographic information of the study groups at baseline and follow-up assessments
At baseline, there were no significant differences between the intervention and control groups in outcome measures (). However, at follow-up assessment, there were significant differences between the two study groups, indicating that the intervention group showed significant improvements in attitudes (P=0.03) and behavioral intention (P=0.01) but not for behavior ().
Table 3 Comparison of baseline assessment between the study groups (n=600)
Table 4 Comparison of follow-up assessment between the study groups (n=438)
The paired t-test showed significant changes in attitude and behavioral intention at baseline and follow-up assessments in intervention group (P=0.01 and P=0.001, respectively), while we did not observe such improvements in control group ().
Table 5 Comparison of the study outcomes at baseline and follow-up within intervention and control groups
Finally, as explained in the Methods section, we performed difference-in-difference analysis to assess the association between the follow-up outcomes while controlling for baseline level of the outcomes and other individual characteristics. The results are presented in . As shown, baseline levels of the outcomes were significantly associated with the follow-up outcomes. However, for attitude in addition to baseline score, the OR for lower level of outcome in the control group was higher than that in the intervention group (OR=1.30, 95% CI=1.13–161, P=0.04). Again, this ratio for behavioral intention in the control group was higher than that in the intervention group (OR=1.77, 95% CI=1.02–3.05, P=0.03). For behavior, only baseline score was significant and other variables did not show any differences either among the study groups or for other characteristics studied.
Table 6 The OR for lower levels of outcomes at follow-up adjusted for baseline level of the outcomes and women’s characteristics
Discussion
The findings from this study indicated that encouraging women for early breast cancer diagnosis using fear appeal did not work. However, the findings showed that fear appeal might be useful message strategy for changing attitude and behavior intention. Studies showed that high threat and high efficacy messages help to influence attitudes and intentions toward recommended behaviors.Citation28,Citation29,Citation41,Citation59–Citation64 It is argued that high threat messages could make people feel vulnerable to undergo treatment if they do not follow the recommended messages, and thus, such messages might influence individuals’ attitudes and intentions.Citation59,Citation61
According to the EPPM, when exposing to threatening messages if an individual believes that he/she could manage the threat and have ability to overcome it successfully, then danger control process starts and the fear strategy might work. Thus, it is believed that when using fear appeal, we should try to move individuals to danger control process. Danger control is a cognitive process and leads to changing person’s attitudes, behavioral intention, and behaviors.Citation32,Citation33,Citation41,Citation58–Citation64 A meta-analysis of 88 attitude–behavior studies reported that attitudes predict the upcoming behavior considerably and substantially.Citation65 Intention is an important key on individual’s readiness for action. Several studies indicated that intention forecasts behaviors although intention–behavior gap should not be neglected.Citation66,Citation67
The current study showed that there was no significant improvement in women’s behavior toward early breast cancer diagnosis. Two reasons may be put forward to explain the findings. First, there are several factors that influence the effectiveness of fear appeals, including individual characters, norms, strength of fear, perceived threat, and perceived response efficacy.Citation23,Citation68 Therefore, if we could not see significant changes in women’s behavior as a result of the study intervention, this should be interpreted in the light of these factors. For instance, the amount of fear was not enough or women felt that they could not attend the annual clinical breast examination for any reason. Second, our observation might be due to the nature of the recommended behavior or the fact that improvement in one’s behavior could not be captured in a short-term basis. Perhaps the short follow-up assessment (women were followed only for 3 months) did not allow us to really see whether fear appeal could influence women’s behavior or not. The theoretical models of behavior change usually expect a longer time for modifying a problematic behavior or acquiring a positive and healthy behavior. For instance, the transtheoretical model argues that health behavior change involves different long-term processes and thus one should not expect to see a behavior change in a short period of time. The model also posits that not only a behavior change by itself is an important step toward adapting a healthy behavior but also the maintenance of such behaviors is crucial.Citation68
Above all as indicated in the regression analysis (), baseline level of the outcomes (attitude, behavioral intention, and behavior scores) showed significant association with the same outcome levels at follow-up. Such observation might indicate that those who usually do not have positive attitude toward early breast cancer diagnosis or do not have any intentions to act toward early breast cancer diagnosis regardless of exposure to fear appeals or other strategies might not follow recommended messages or benefit from interventions alone unless we raise awareness among such individuals.
It is known that there are several barriers, which inhibit the early breast cancer diagnosis, such as poverty, lack of health insurance, and aging. Also not having enough knowledge about screening methods, being busy, negligence, forgetfulness, and not feeling necessity for early breast cancer diagnosis are some other reasons that have been acknowledged in different studies.Citation3,Citation12
The women who participated in this study were not well educated. Studies have shown that low-educated women usually do not have enough information about breast cancer, its risk factors, and are most prone to not doing screening behaviors.Citation12,Citation14,Citation17 However, although education is a main factor in determining women’s socioeconomic status, there is a paradox between educational level and risk of breast cancer. Women in higher socioeconomic status usually are at higher risk of breast cancer, while women from lower socioeconomic position are at lower risk of breast cancer but they usually do not use preventive services.Citation12,Citation17 Studies from Iran found that Iranian women have relatively inadequate knowledge about breast cancer and its preventive measures. As such, it has been emphasized that Iranian women need more education and appropriate information about breast cancer and its early detection.Citation2,Citation9,Citation13,Citation47
The participants of this study were selected from women aged 40 years and above living in Tehran. This might limit the external validity of the study although there is evidence that a representative sample from Tehran could be a representative of Iranian people.Citation69 We did not use the risk behavior diagnosis to assess whether women were at danger control or fear control processes at different phases. Short follow-up time is also another limitation. Further studies are needed to investigate how fear appeal strategy might work in the long term in changing early breast cancer diagnosis among women. One another limitation for the current study is the fact that we did not collect information concerning women’s perception of benefits and intangible costs of breast screening (eg, false positive or overdiagnosis). This perception could be a confounding variable in the analysis. The recent literature suggests that in addition to raising awareness among women about early detection and breast cancer screening programs, persuasive communications should focus on informed decision-making in light of potential benefits and harms perceived by women.Citation70,Citation71 Finally, it is important to report that there was a substantial loss to follow-up. This means that the study did not achieve its designed power and this should be considered as a limitation.
Conclusion
The results showed that fear appeals could influence women’s attitude and behavioral intention but not early breast cancer diagnosis. Perhaps longitudinal studies are needed to be able to capture behavior changes when studying early cancer diagnosis.
Data sharing statement
The data presented in this paper are available from the corresponding authors on reasonable request.
Acknowledgments
This manuscript originated from a PhD thesis by VTZ at Department of Health Education and Promotion, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran. We acknowledge the help received from Mrs Koosha and her colleagues in Motamed Breast Cancer Institute, Breast Cancer Research Institute (IBCRC). The research team also is grateful to Iranian Students Polling Agency (ISPA) for their help.
Disclosure
The authors report no conflicts of interest in this work.
References
- Haji-MahmoodiMMontazeriAJarvandiSEbrahimiMHaghighatSHarirchiIBreast self-examination: knowledge, attitudes, and practices among female health care workers in Tehran, IranBreast J20028422222512100114
- MousaviSMMontazeriAMohagheghiMABreast cancer in Iran: an epidemiological reviewBreast J200713438339117593043
- MemonZAShaikhANRizwanSSardarMBReasons for patient’s delay in diagnosis of breast carcinoma in PakistanAsian Pac J Cancer Prev201314127409741424460311
- BigluMHBreast cancer in Iran: the trend of Iranian researchers’ studies in MEDLINE databaseBasic Clin Cancer Res201462232
- EbrahimiMVahdaniniaMMontazeriARisk factors for breast cancer in Iran: a case-control studyBreast Cancer Res200245R1012223127
- KrukJLifestyle components and primary breast cancer preventionAsian Pac J Cancer Prev20141524105431055525605138
- WHOBreast cancer prevention Available from: http://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/Accessed January 1, 2018
- MontazeriAEbrahimiMMehrdadNAnsariMSajadianADelayed presentation in breast cancer: a study in Iranian womenBMC Womens Health200331412846932
- MontazeriAHarirchiIVahdaniMAnxiety and depression in Iranian breast cancer patients before and after diagnosisEur J Cancer Care200093151157
- BoulosDNGhaliRRAwareness of breast cancer among female students at Ain Shams University, EgyptGlob J Health Sci20136115416124373275
- DavisSMMartinelliDBraxtonBKutrovacKCroccoTThe impact of the extended parallel process model on stroke awarenessStroke200940123857386319797185
- MontazeriAVahdaniniaMHarirchiIBreast cancer in Iran: need for greater women awareness of warning signs and effective screening methodsAsia Pac Fam Med20087619099595
- MousaviSMHarirchiIEbrahimiMScreening for breast cancer in Iran: a challenge for health policy makersBreast J200814660560619000044
- HarrisRYeattsJKinsingerLBreast cancer screening for women ages 50 to 69 years a systematic review of observational evidencePrev Med201153310811421820465
- FarmaKKJaliliZZarebanIPourMSEffect of education on preventive behaviors of breast cancer in female teachers of guidance schools of Zahedan city based on health belief modelJ Educ Health Promot201437725250343
- HowellAAndersonASClarkeRBRisk determination and prevention of breast cancerBreast Cancer Res201416544625467785
- AhmadianMSamahAAA literature review of factors influencing breast cancer screening in Asian countriesLife Sci J20129585594
- ShindeSDKadamSBBreast cancer awareness among women in Vikhroli: a suburban area of Mumbai, Maharashtra, IndiaInt J Community Med Public Health2017322812286
- EvansREMorrisMSekhonMIncreasing awareness of gynaecological cancer symptoms: a GP perspectiveBr J Gen Pract201464623e372e38024868075
- LostaoLJoinerTEPettitJWChorotPSandínBHealth beliefs and illness attitudes as predictors of breast cancer screening attendanceEur J Public Health200111327427911582606
- GlanzKRimerBKViswanathKHealth Behavior and Health Education: Theory, Research, and Practice4th edNew YorkJohn Wiley2008
- RuiterRAKesselsLTPetersGJKokGSixty years of fear appeal research: current state of the evidenceInt J Psychol2014492637024811876
- PetersGJRuiterRAKokGThreatening communication: a qualitative study of fear appeal effectiveness beliefs among intervention developers, policymakers, politicians, scientists, and advertising professionalsInt J Psychol2014492717924811877
- Murray-JohnsonLWitteKBoulayMFigueroaMEStoreyDTweedieIUsing health education theories to explain behavior change: a cross-country analysis. 2000–2001Int Q Community Health Educ2005251–218520717686703
- NoarSMHallMGFrancisDBRibislKMPepperJKBrewerNTPictorial cigarette pack warnings: a meta-analysis of experimental studiesTob Control201625334135425948713
- NandakumarNSivakumaranBKalroASharmaPThreat, efficacy and message framing in consumer healthcareMarket Intell Plann2017354442457
- HallIJJohnson-TurbesAUse of the persuasive health message framework in the development of a community-based mammography promotion campaignCancer Causes Control201526577578425724414
- ShiJJSmithSWThe effects of fear appeal message repetition on perceived threat, perceived efficacy, and behavioral intention in the extended parallel process modelHealth Commun201631327528626305152
- PaekHJOhSHHoveTHow fear-arousing news messages affect risk perceptions and intention to talk about riskHealth Commun20163191051106226789555
- DillardJPAndersonJWThe role of fear in persuasionPsychol Market20042111909926
- NanXMaddenKRichardsAHoltCWangMQTracyKMessage framing, perceived susceptibility, and intentions to vaccinate children against HPV among African American parentsHealth Commun201631779880526646190
- LewisIWatsonBWhiteKMExtending the explanatory utility of the EPPM beyond fear-based persuasionHealth Commun2013281849823330861
- StephensonMTWitteKFearWKFear, threat, and perceptions of efficacy from frightening skin cancer messagesPublic Health Rev199826214717410327830
- BatchelderAMatusitzJ“Let’s Move” campaign: applying the extended parallel process modelSoc Work Public Health201429546247225068611
- ThrasherJFSwayampakalaKBorlandRInfluences of self-efficacy, response efficacy, and reactance on responses to cigarette health warnings: a longitudinal study of adult smokers in Australia and CanadaHealth Commun201631121517152627135826
- HatchellACBassett-GunterRLClarkeMKimuraSLatimer-CheungAEMessages for men: the efficacy of EPPM-based messages targeting men’s physical activityHealth Psychol2013321243223316850
- MckayDLBerkowitzJMBlumbergJBGoldbergJPCommunicating cardiovascular disease risk due to elevated homocysteine levels: using the EPPM to develop print materialsHealth Educ Behav200431335537115155045
- SoJA further extension of the Extended Parallel Process Model (E-EPPM): implications of cognitive appraisal theory of emotion and dispositional coping styleHealth Commun2013281728323330860
- LavoieNRQuickBLWhat is the truth? An application of the extended parallel process model to televised truth® adsHealth Commun2013281536223330858
- FehrenbachKSDesigning Messages to Reduce Meat Consumption: A Test of the Extended Parallel Process Model [PhD dissertation]AZ, USAArizona State University2015
- LatourMSSnipesRLBlissSJDon’t be afraid to use fear appeals: an experimental studyJ Advert Res1996365968
- KriegerJLSargeMAA serial mediation model of message framing on intentions to receive the human papillomavirus (HPV) vaccine: revisiting the role of threat and efficacy perceptionsHealth Commun201328151923330854
- NapperLEHarrisPRKleinWMCombining self-affirmation with the extended parallel process model: the consequences for motivation to eat more fruit and vegetablesHealth Commun201429661061824138335
- MajidiASalimzadehHBeikiOCancer research priorities and gaps in Iran: the influence of cancer burden on cancer research outputs between 1997 and 2014Public Health2017144424728274383
- EnayatradMAmooriNSalehiniyaHEpidemiology and trends in breast cancer mortality in IranIran J Public Health201544343043125905094
- Khazaee-PoolMMontazeriAMajlessiFRahimi ForoushaniANedjatSShojaeizadehDBreast cancer-preventive behaviors: exploring Iranian women’s experiencesBMC Womens Health20141414124606758
- AtaollahiMSedighiSMasoumiSZNutritional and unhealthy behaviors in women with and without breast cancerIran Red Crescent Med J2014169e1968425593731
- BlandJMKerrySMTrials randomised in clustersBMJ199731571086009302962
- CampbellMKMollisonJSteenNGrimshawJMEcclesMAnalysis of cluster randomized trials in primary care: a practical approachFam Pract200017219219610758085
- MobergJKramerMA brief history of the cluster randomised trial designJ R Soc Med2015108519219826022551
- CuevaKCuevaMDignanMLandisKPrint material in cancer prevention: an evaluation of three booklets designed with and for Alaska’s community health workersJ Cancer Educ201631227928425865398
- van BreukelenGJCandelMJCalculating sample sizes for cluster randomized trials: we can keep it simple and efficientJ Clin Epidemiol201265111212121823017638
- EldridgeSMAshbyDKerrySSample size for cluster randomized trials: effect of coefficient of variation of cluster size and analysis methodInt J Epidemiol20063551292130016943232
- RutterfordCCopasAEldridgeSMethods for sample size determination in cluster randomized trialsInt J Epidemiol20154431051106726174515
- CampbellMKThomsonSRamsayCRMaclennanGSGrimshawJMSample size calculator for cluster randomized trialsComput Biol Med200434211312514972631
- DonnerABirkettNBuckCRandomization by cluster. Sample size requirements and analysisAm J Epidemiol198111469069147315838
- FraleyCRafteryEHow many clusters? Which clustering method? Answers via model-based cluster analysisComput J1998418578588
- HineDWGiffordRFear appeals, individual differences, and environmental concernJ Environ Educ19912313641
- EmerySLSzczypkaGAbrilEPKimYVeraLAre you scared yet? Evaluating fear appeal messages in tweets about the tips campaignJ Commun20146427829525429162
- TannenbaumMBHeplerJZimmermanRSAppealing to fear: a meta-analysis of fear appeal effectiveness and theoriesPsychol Bull201514161178120426501228
- RedmondMLDongFFrazierLMDoes the extended parallel process model fear appeal theory explain fears and barriers to prenatal physical activity?Womens Health Issues201525214915425648489
- HalkjelsvikTLundKEKraftPRiseJFear appeals in advanced tobacco control environments: the impact of a national mass media campaign in NorwayHealth Educ Res201328588889723766451
- WitteKAllenMA meta-analysis of fear appeals: implications for effective public health campaignsHealth Educ Behav200027559161511009129
- KrausSJAttitudes and the prediction of behavior: a meta-analysis of the empirical literaturePers Soc Psychol Bull19952115875
- SheeranPIntention – behavior relations: a conceptual and empirical reviewEur Rev Soc Psychol2002121136
- AjzenIFisbbeinMFactors influencing intentions and the intention-behavior relationHuman Relations1974271115
- RogersRWA protection motivation theory of fear appeals and attitude change1J Psychol19759119311428136248
- ProchaskaJOVelicerWFThe transtheoretical model of health behavior changeAm J Health Promot1997121384810170434
- MontazeriAGoshtasebiAVahdaniniaMEducational inequalities in self-reported health in a general Iranian populationBMC Res Notes2008115018710503
- HerschJJansenJMccafferyKDecision-making about mammographic screening: pursuing informed choiceClimacteric201821320921329419315
- SicsicJPelletier-FleuryNMoumjidNWomen’s benefits and harms trade-offs in breast cancer screening: results from a discrete-choice experimentValue Health2018211788829304944