Abstract
Objective:
To compare the acceptability, efficacy, adverse effects, and user satisfaction of the levonorgestrel intrauterine system (LNG-IUS) and trans-cervical resection of the endometrium (TCRE) for the treatment of menorrhagia.
Method:
104 women with menorrhagia were divided into 2 groups: 52 women had the LNG-IUS inserted and 52 underwent TCRE. Menstrual pattern, pictorial blood loss assessment chart score, adverse effects, and rates of acceptability and satisfaction, were recorded at 6 and 12 months after the procedure.
Results:
After a year there were reductions of 93.9% and 88.4% in menstrual blood loss in the TCRE and LNG-IUS groups, respectively. Amenorrhea was more common in the TCRE group and spotting and systemic effects in the LNG-IUS group. Satisfaction rates of the TCRE group were higher than the LNG-IUS group (80.8% vs 69.2%), but the difference was not statistically significant.
Conclusion:
Although both treatments were found to be equally effective, LNG-IUS was less invasive and can be advised for younger women with a desire to preserve fertility.
Introduction
Menorrhagia constitutes a considerable problem for many women, causing discomfort, anxiety, and decreased quality of life. Menorrhagia is experienced by up to 30% of women of reproductive age and accounts for 60% of the general female population. It requires practice consultations for menstrual disorders and is the most common cause of iron deficiency anemia in healthy fertile women.Citation1,Citation2 Identifying new, less invasive, techniques, which are true alternatives to hysterectomy for treating menorrhagia, which would enable patients to resume their routine daily activities within a shorter period of time, represents a challenge to modern medicine.Citation3,Citation4
Medical management for dysfunctional uterine bleeding was, for a long time, hormonal therapy in the form of oral progesterone or the combined oral contraceptive pill. However, these methods have been revolutionized by newer modalities such as the levonorgestrel releasing intrauterine system (LNG-IUS: Mirena®, Schering AG, Berlin, Germany). LNG-IUS provides a non-surgical alternative treatment, which is reversible and spares fertility.Citation5 Endometrial ablation continues to play an important role in the management of dysfunctional uterine bleeding. Along with laser and roller ball ablation, hysteroscopic trans-cervical resection of the endometrium (TCRE) is still considered a gold standard.Citation6 In experienced hands, its complications are few but the operation requires hospitalization, and it is not suitable for women who want to preserve their fertility.
The aim of this study is to compare the efficacy, adverse effects, and rate of satisfaction and acceptability of LNG-IUS and TCRE in the treatment of menorrhagia.
Materials and methods
One hundred and four women with menorrhagia were enrolled in the study. The patients were considered eligible for the study if they were 35–45 years old, had heavy menstrual loss based on a pictorial blood assessment chart (PBAC) (score > 100) defined by Higham et alCitation7 and with no history of medical treatment for at least 6 months before the trial. The exclusion criteria were: a previous history of deep venous thrombosis, thromboembolism, liver disease, pelvic disease, active genital tract infection, abnormal endometrial histology, abnormal cervical cytology, previous endometrial resection and ablation, or any other pathology such as uterine prolapse or large myomas and pregnancy. Patients who were uncertain about their future wish for pregnancy were also excluded.
The patients were informed about both LNG-IUS and TCRE and allowed to choose either treatment in a series of sealed, opaque, sequentially numbered, envelopes prepared by an independent statistician, revealing the treatment code in a 1:1 individual randomization ratio. This was predetermined by computer-generated random number tables, which were in balanced blocks of 20. Written informed consent was obtained from all patients.
Routine investigations included hemogram, liver, kidney and thyroid function tests, and gynecological examination included endometrial biopsy by Pipelle sampling and cervical smears to rule out endometrial or cervical neoplasia. A trans-vaginal ultrasound scan was also carried out on all patients to ensure that no fibroids were visible. The maximal anterior–posterior diameter of the uterus and endometrial thickness was recorded. In the TCRE group, the operation was performed under general anesthesia 5 weeks after endometrial preparation with a single injection of triptorelin 3.76 mg and by a single operator. A Storz rigid resectoscope (Ch 26, model 27040 SL equipped with a Hopkins 27005 B 300 optic; Storz Tuttlingen, Germany) with a 4-mm resection loop was passed into the uterine cavity. Glycine 1.5% was infused for irrigation with an infusion pressure of 100 mmHg. A mixed diathermy current of 120 W was used. The depth of resection varied from 4 to 6 mm, depending on the preoperative endometrial preparation.
In LNG-IUS group, LNG-IUS was inserted within 7 days of the start of menstruation by a single gynecologist, based on the need for cervical dilatation on IUD insertion or not, which was classified as difficult or easy respectively. Any complications such as uterine perforation, hemorrhage, and abdominal cramps were recorded and the patients were observed for 1 hour before discharge. After the procedure, all patients were advised to keep a menstrual record including length of menstrual cycles, days of bleeding, number of stained towels in one day, amount of staining and note any adverse effects namely spotting, abdominal cramps and pains, breast tenderness, headaches, acne, mood changes, and weight gain.
The patients were visited by a single physician in the outpatient’s clinic 6 and 12 months posttreatment and the menstrual pattern of the preceding month and any adverse effects were noted. The primary outcomes included the menstrual pattern namely amenorrhea and reduction in bleeding score. The secondary outcome was the rate of patient satisfaction. “Amenorrhea” was defined as the absence of bleeding for at least 3 months, “no response” as continuous menorrhagia; and “regular cycles” when the bleeding occurred in an interval between 25 and 32 days and the length of bleeding was not more than 5 days. Patient satisfaction was recorded on a scale of 1 to 5, with 1 being “least satisfied” and 5 being “most satisfied”. This clinical trial was approved by the Ethics Committee of Tehran University of Medical Sciences.
Statistical methods
A sample of 52 patients was divided into two groups according to the study by Gupta et al,Citation11 in which a 97% and 94% reduction in menstrual blood loss was reported in the LNG-IUS and TCRE groups, respectively, as well as differences > 0.09 SD between the means of the two groups (quantitative variables), with a statistical power of 80% and a 95% confidence level.
Statistical analysis was performed using SPSS 16. Normal distribution of the data was verified using the Kolmogorov–Smirnov test. The variables were described as mean and SD. The statistical differences between the groups were tested using Student’s unpaired t test, Mann–Whitney test, and Chi square test. Significance level was established as P < 0.05.
Results
One hundred and four women with menorrhagia were divided into two groups: 52 women had the LNG-IUS inserted and 52 underwent TCRE. The two groups were similar in age, BMI, PBAC score, and menstrual duration. However, the menstrual interval and duration of complaint were lower in TCRE group (). The previous treatment of the two groups had been similar, and endometrial histology of most patients showed secretory endometrium. Endometrial thickness in LNG-IUS was 8.60 ± 4.5 and in TCRE was 8.41 ± 4.4 (P = 0.88).
Table 1 Baseline characteristics (with percentages rounded for clarity)
Twelve patients had systematic disorders including two patients with coagolopathy due to warfarin use in TCRE group (3.8%), three (5.8%) with diabetes, three (5.8%) with hypothyroidism, and two (3.8%) with corticotrophin-releasing factor (CRF) in each group. In the LNG-IUS group, two patients required cervical dilatation but there were no uterine perforations or cervical injury. All patients were discharged within 1 hour of the procedure. In TCRE group one case of uterine perforation with no hemorrhagic complication needed intervention. This patient was hospitalized for 1 day after TCRE. Of the remaining patients, one who had diabetes was observed for 48 hours post-procedure, but the others were discharged the same day. Because we had no access to twelve of the patients in the 12 months after the procedure for follow up, they were excluded from the trial (). The pictorial bleeding score was significantly decreased at 6 and 12 months post-procedure in the two groups (P < 0.0001) and was statistically similar between the 2. PBAC score after 6 months was 70.65 ± 115.61 and 60.38 ± 110.65 in the TCRE and LNG-IUS groups respectively. There was 44.7% amenorrhea in the TCRE group compared with 11.1% in the LNG-IUS group (P < 0.0001, difference 33.6%, 80% CI 15%–52%). The rate of no response to treatment was 4.2% in the TCRE group compared with 20% in the LNG-IUS group (P = 0.007, difference 15.8%, 80% CI 3%–29%) ().
Figure 1 Flow diagram of the trial.
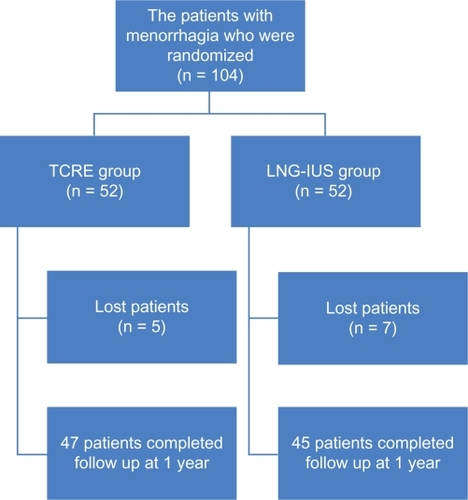
Table 2 The satisfaction and acceptability, menstrual status and symptoms at the 12th month post-procedure follow up
In TCRE group, one patient had uterine perforation and there were two cases of hematometra due to cervical stenosis which were released by cervical dilation. Two patients underwent hysterectomy for persistent menorrhagia in the 12th month post-procedure. In LNG-IUS group, nine patients reported expulsion of IUS and in six patients it was removed (five for continued menorrhagia and one for unacceptable spotting and weight gain). Six patients (12.7%) reported spotting. The adverse effects of LNG-IUS were cramps and pains in four (8.2%), spotting in 19 (38.8%), breast tenderness in ten (20.4%), headaches in nine (18.4%), acne in two (4.1%), mood changes in four (8.2%), weight gain in one (2%) and ovarian cyst in one (2%) patient. Satisfaction score of more than three was achieved in 42 patients (80.8%) and 36 patients (69.2%) of TCRE and LNG-IUS groups respectively and satisfaction score of less than three was recorded for seven patients (10.4%) and 16 patients (30.8%) of TCRE and LNG-IUS groups respectively. Mean satisfaction score was similar in the two groups (P = 0.43) ().
Discussion
Heavy menstrual bleeding is a significant health problem that impairs the quality of life. The perception of heavy bleeding is highly subjective, however, and management of the condition usually depends on both the amount of bleeding and the degree of discomfort found acceptable by the individual woman.
Hysterectomy was once the only surgical option for heavy menstrual bleeding, and almost half of the hysterectomies currently performed worldwide are carried out for this reason, but it is a major surgical intervention associated with surgical risks and substantial costs.Citation8 Endometrial destruction techniques, which aim to destroy or remove the endometrial tissue, include roller-ball ablation and trans-cervical resection under direct hysteroscopic vision and second generation non-hysteroscopic techniques.Citation9 LNG-IUS provides a nonsurgical alternative, which is reversible and spares fertility.Citation10
The results of this study demonstrate that both LNG-IUS and TCRE clearly reduce menstrual blood loss. Responses to treatment at the end of 1 year follow up showed no significant difference between the two groups (93.9% for TCRE and 88.4% for LNG-IUS), but the rate of amenorrhea in the TCRE group was higher (P < 0.0001). In the study by Gupta et al,Citation11 97% and 94% reductions were observed in menstrual blood loss in the LNG-IUS and TCRE groups respectively. However, Crosignani et al and Istre and Trolle reported a significantly higher reduction in menstrual blood loss with TCRE than with LNG-IUS insertion.Citation12,Citation13 Based on the meta-analysis of six randomized clinical trials, the efficacy of the LNG-IUS in the management of heavy menstrual bleeding appears to have similar therapeutic effects to that of endometrial ablation up to 2 years after treatment.Citation14 In our study, amenorrhea was more common in the TCRE group than in LNG-IUS at 12 months posttreatment (44.7% vs 11.1% respectively) and spotting was more common in LNG-IUS group (38% vs 12%). In Hidalgo et al, 44% of the women who had LNG-IUS inserted reported amenorrhea at the 6th month of use. This rate maintained stability in 50% of these women after 12 and 24 months of use and spotting was present in 25% of the users at 6 months, decreasing to 11% at 24 months. This rate maintained stability at 50% after 12 and 24 months of use.Citation15 Wide dissemination of information on the expected bleeding patterns after LNG-IUS insertion is necessary, so that it can reduce unnecessary, more radical, surgery.
In our study, similar to that of Gupta et al, the systemic effects such as breast tenderness, acne, mood changes, headaches, and bloating were more common in LNG-IUS group than TCRE group and the most common side effect in LNG-IUS group was spotting.Citation10 In de Souza et al, both the LNG-IUS and thermal balloon ablation appear to be effective in controlling heavy menstrual bleeding, although post treatment uterine bleeding patterns may vary between the 2 methods.Citation16
Satisfaction rates of TCRE group in our study were higher than in LNG-IUS group (80.8% vs 69.2%) but their difference was not statistically significant. A meta-analysis of heavy menstrual bleeding treatment stated that at around 12 months posttreatment, both first- and second-generation endometrial destruction techniques were associated with greater dissatisfaction than hysterectomy, although rates were low for all treatments. Absolute differences were small compared with endometrial destruction and LNG-IUS. There was comparable efficacy, although studies of LNG-IUS were generally small and consequently imprecise.Citation17 The results of our study clearly demonstrate that both LNG-IUS and TCRE clearly reduce menstrual blood loss and their satisfaction rate is similar. Also in our study, twelve patients with a systemic disorder such as coagolopathy and CRF responded to the treatment as well as others.
Several trials have compared the two modalities, but to our knowledge the present study is the second of its kind conducted in an Islamic country. In the religion of Islam, prolonged bleeding or spotting is a problem for performing religious activities (eg, such women are not allowed to say prayers or fast) and consequently affects patient quality of life. The results of another study in Egypt were similar to ours.Citation18
Perhaps one of the biggest limitations of our study was the likeliness that patients would choose to undergo LNG-IUS rather than TCRE, after becoming informed about these treatments. Regarding the efficacy of LNG-IUS in the medical management of dysfunctional uterine bleeding that is similar to endometrial resection, this treatment can be used as first- or second-line option for the medical management of dysfunctional uterine bleeding and due to its reversibility and contraceptive effect, it may become a first-line treatment for younger patients especially in developing countries where resources and experiences of operative hysteroscopy are limited. In addition, the cost of TCRE is almost 3 times that of LNG-IUS in Iran (US$300 vs US$120).
Conclusion
The LNG-IUS is a contraceptive device that has dramatic effects in lowering bleeding intensity in menorrhagia. It is further characterized by reversibility and may be the first-line treatment in younger women with menorrhagia. Due to its low systemic steroidal dose, the adverse events are mild and few. Although TCRE is even more effective in reducing blood loss, it is irreversible and needs operative facilities. Overall, the tolerability of both treatments is good. The findings of this study can guide gynecologists and hospital administrators in choosing the appropriate treatment method for menorrhagia.
Acknowledgements
This article is based on a post-doctoral dissertation by Fatemeh Bakhtiari. The authors would like to thank Seyed Muhammed Hussein Mousavinasab for his sincere cooperation in editing this work.
Disclosure
The authors declare no conflicts of interest in relation to this paper.
References
- ShawRWAssessment of medical treatment for menorrhagiaBr J Obstet Gynaecol19941018158043559
- LiuZDoanQVBlumenthalPDuboisRWA systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleedingValue Health20071018319417532811
- ClarkeABlackNRowePMottSHowleKIndications for and outcome of total abdominal hysterectomy for benign disease: a prospective cohort studyBr J Obstet Gynaecol19951026116207654638
- BanuNSManyondaITAlternative medical and surgical options to hysterectomyBest Pract Res Clin Obstet Gynaecol20051943144915985257
- StewartACumminsCGoldLJordanRPhillipsWThe effectiveness of the levonorgestrel-releasing intrauterinesystem in menorrhagiaBr J Obstet Gynaecol20011087486
- LethabyAHickeyMGarryREndometrial destruction techniques for heavy menstrual bleedingCochrane Database Syst Rev200519CD00150116235284
- HighamJMO’BrianPMSShawRWAssessment of menstrual blood loss using a pictorial chartBr J Obstet Gynecol19909077347399
- MareshMJAMetcalfeMAMcPhersonKOvertonCHallVHargreavesJThe VALUE national hysterectomy study: description of the patients and their surgeryBr J Obstet Gynaecol2002109302312
- AbbottJGarryRThe surgical management of menorrhagiaHum Reprod Update2002878
- LethabyAECookeIReesMProgesterone or progestogen-releasing intrauterine systems for heavy menstrual bleedingCochrane Database Syst Rev20054CD00212616235297
- GuptaBMittalSMisraRDekDDadhwalVLevonorgestrel-releasing intrauterine system vs transcervical endometrial resection for dysfunctional uterine bleedingInter J Gynecol Obstet200695261266
- CrosignaniPGVercelliniPMosconiPMSciDBOldaniSCortesiILevonorgestrel-releasing intrauterine device versus hysteroscopic endometrial resection in the treatment of dysfunctional uterine bleedingObstet Gynecol1997902572639241305
- IstreOTrolleBTreatment of menorrhagia with the levonorgestrel intra uterine system versus endometrial resectionFertil Steril20017630430911476777
- KaunitzAMMeredithSInkiPKubbaASanchez-RamosLLevonorgestrel-releasing intrauterine system and endometrial ablation in heavy menstrual bleeding: a systematic review and meta-analysisObstet Gynecol20091131104111619384127
- HidalgoMBahamondesLPerrottiMDiazJDantas-MonteiroCCarlosPBleeding patterns and clinical performance of the levonorgestrelreleasing intrauterine system (Mirena) up to two yearsContraception20026512913211927115
- de SouzaSSCamargosAFde RezendeCPPereiraFANAraújoCAASilva FilhoALA randomized prospective trial comparing the levonorgestrel-releasing intrauterine system with thermal balloon ablation for the treatment of heavy menstrual bleedingContraception20108122623120159179
- MiddletonLJChampaneriaRDanielsJPHysterectomy, endometrial destruction, and levonorgestrel releasing intrauterine system (Mirena) for heavy menstrual bleeding: systematic review and meta-analysis of data from individual patientsBMJ 201;341C3929
- MalakKAManagement of menorrhagia with the levonorgestrel intrauterine system versus endometrial resectionGynaecol Surg20063275280