Abstract
Background:
The purpose of this study was to review our experience and the challenges of using the da Vinci® surgical system robot during gynecological surgery at King Abdulaziz University Hospital.
Methods:
A retrospective study was conducted to review all cases of robot-assisted gynecologic surgery performed at our institution between January 2008 and December 2010. The patients were reviewed for indications, complications, length of hospital stay, and conversion rate, as well as console and docking times.
Results:
Over the three-year period, we operated on 35 patients with benign or malignant conditions using the robot for a total of 62 surgical procedures. The docking times averaged seven minutes. The mean console times for simple hysterectomy, bilateral salpingo-oophorectomy, and bilateral pelvic lymphadenectomy were 125, 47, and 62 minutes, respectively. In four patients, laparoscopic procedures were converted to open procedures, giving a conversion rate of 6.5%. All of the conversions were among the first 15 procedures performed. The average hospital stay was 3 days. Complications occurred in five patients (14%), and none were directly related to the robotic system.
Conclusion:
Our early experience with the robot show that with proper training of the robotic team, technical difficulty with the robotic system is limited. There is definitely a learning curve that requires performance of gynecological surgical procedures using the robot.
Introduction
Minimally invasive techniques for performing gynecologic surgery have been associated with shorter hospital stays and reduced patient morbidity.Citation1,Citation2 Use of robotic tools to assist surgical procedures can be tracked back as far as the 1980s.Citation3,Citation4 Since then, many different robotic devices have been developed for various purposes. Currently, the only available system for laparoscopic surgery is the da Vinci® surgical system developed by Intuitive Surgical Inc, Sunnyvale, CA. The three-dimensional vision system of the robot allows the surgeon to see fine structures at 10-fold magnification, thus providing visual advantages for more precise surgery. The instruments of the robotic system offer an articulating wrist that mimics the movements of the human hand. This articulating wrist has seven degrees of freedom, making it much easier to access structures deep in the pelvic cavity and perform ambidextrous movements with respect to suturing, excising, and reconstructing tissue, which is the major advantage over traditional laparoscopy.Citation5–Citation8 However, limited patient numbers, mainly due to the high costs involved in robotic surgery, have led to a lack of properly designed studies, which makes it difficult to assess what clinical benefits this new technology can offer to the surgical world. While noncomparative studies have demonstrated the general feasibility of using the robot for many procedures in various surgical subspecialties,Citation8–Citation11 other studies have shown that robotic surgery is comparable with conventional laparoscopy in terms of operating time, blood loss, patient morbidity, early and late complications, and other factors.Citation9,Citation10–Citation13 Still, time constraints due to the use of the da Vinci surgical system during surgery, leading to prolonged overall operating room times, have been reported in numerous studies.Citation7,Citation14,Citation15 A potential reason for these time constraints is the extra time needed for preparing the robot.
As a gynecological oncology practice at a teaching institution, we treat patients with malignant and benign diseases, which are often complex cases. Therefore, the purpose of this study was to evaluate the impact of using a robotic surgical system for gynecologic surgery in a university hospital setting. Operative (docking and console) times and morbidity were our main outcomes, including the learning curve.
Methods
This was a retrospective study of all gynecological surgery performed using the three arms of the da Vinci® robotic system between January 2008 and December 2010 at King Abdulaziz University Hospital. The ethics committee at our institution had approved the use of the surgical robotic system in gynecological surgery. Patients were selected based on a preoperative evaluation, absence of any absolute contraindications to standard conventional laparoscopy, and willingness to give informed consent. Before clinical application, a team with previous experience performing laparoscopic surgery was trained to use the robot in an animal laboratory model and also took training courses in order to learn to perform the procedures correctly. The aims of these training sessions were to familiarize the surgeons and nurses with the system (eg, startup, control, connection, wrapping the arms with sterile drapes, attaching the instruments) and how to drive the instruments with the remote “joysticks”. One senior surgeon at the console performed all of the robotic procedures, while an assistant stood at the patient’s side together with a scrub nurse.
The Intuitive Surgical system consists of two main components, ie, the surgeon’s console and the surgical cart. Perioperative antibiotics are administered. For deep venous thrombosis prophylaxis, lower extremity sequential compression devices and elastic stockings are used, as well as an anticoagulant. All procedures are performed under general anesthesia with the patient in the dorsal lithotomy position and using Allen stirrups. A gel pad is placed under the patient on the surgical table. The patient’s arms are tucked at the side, and shoulder blocks are placed to minimize shifting of the patient’s position and to prevent nerve injury.
The patient is placed in a dorsal and steep Trendelenburg position. The lower limbs are spread in slight hyperextension to avoid contact with the arms of the robot and to ease mobilization of the uterus by a second assistant seated between the limbs. A Foley catheter is inserted, and a vaginal cup is connected using a uterine manipulator when indicated. CO2 insufflation is begun, either with a Veress needle or an open trocar, and continued until a pressure of 12 mmHg is reached. A 12 mm disposable trocar is inserted at the level of the umbilicus to host the camera. Two specific 8 mm trocars are introduced in each lower quadrant of the abdomen, lateral to the epigastric arteries, 2–3 cm below the umbilical level. A fourth assistant port (10–12 mm) is placed mid distance between the umbilicus and the left robotic arm. The procedure begins with a standard laparoscopy in order to explore the abdominal cavity, to perform adhesiolysis, and to retract the bowel for optimal exposure. The surgical cart is positioned between the legs of the patient, and behind the second assistant. The three robotic arms are docked to the trocars. A 0° endoscope attached on the camera arm is used for vision. EndoWrist bipolar forceps (Intuitive Surgical Inc) are attached on the left robotic arm in order to grasp and coagulate, while unipolar scissor apparatus is attached on the right robotic arm in order to dissect and coagulate. If a hysterectomy is performed totally by robot, closure of the vaginal cuff is performed by the robot, using interrupted 2–0 stitches. When indicated, bilateral pelvic lymph node dissection is performed. Lymph nodes are removed laparoscopically into a bag. A vacuum drain is inserted before closure of the orifices of the trocar. Trocar incisions larger than 10 mm are closed with two stitches. In agreement with the surgeon, patients decide when they are to be discharged, as soon as they feel able to take care of themselves without aid.
The robotic setup includes preparing the robot for surgery. This involves the connection of all necessary parts, such as sterile drapes and the connectors necessary for surgery, and also the calibration process. In our study, these steps were conducted by a core team of scrub nurses specifically trained in handling the robot while the patient is being prepared for surgery. Docking time is determined after an initial laparoscopy and placement of all trocars, beginning exactly with the first command to push the robot towards the patient and ending with the actual start of the robotic part of the procedure. The console time is the duration spent by the surgeon using the joystick.
Data from the robotic surgeries we performed were evaluated for docking times, console times, and the learning curve. Patients had special forms filled out immediately after the procedure and completed during the postoperative period, which is done routinely in our center. The form includes the surgical indication, complications, name of procedure(s) performed, and docking and console times. Data were analyzed and the rate of conversion to an open procedure was calculated.
Statistical analysis
Statistical analysis was done using the SPSS program version 16 (SPSS Inc, Chicago, IL). The data are presented as means, medians, standard deviations, and interquartile ranges, as appropriate. Pearson’s coefficient was used to study the correlation between time and number of operation. A P value < 0.05 was considered to be statistically significant.
Results
Over the three-year period, we performed a total of 62 procedures in 35 women. The number of patients who underwent procedures in the years 2008, 2009, and 2010 were four, four, and 27, respectively. Mean age was 49 (range 32–55) years. Mean body mass index was 28 (range 24–31) with an average parity of three (). Three patients (8.6%) had undergone a previous laparotomy. Five patients (14%) had pre-existing medical conditions, ie, hypertension in three and diabetes in three (one patient had both illnesses). No patient had cardiopulmonary impairment.
Table 1 Demographic data from a total of 35 women
shows the types of procedures performed using the robot. A total of 22 (63%) women had procedures performed for complex benign cases and 13 (37%) had procedures performed for a malignant indication ().
Table 2 Procedure type in robot-assisted gynecological surgery
Table 3 Indications for robot-assisted gynecological surgery in 35 women
Four of the cases of simple hysterectomy were completed vaginally, and the vault was closed vaginally at the initial procedure. However, three cases of simple hysterectomy and one case of bilateral pelvic lymphadenectomy were converted to an open approach, representing an overall conversion rate of 6.5%. The reasons for conversion were technical fault with the robotic system, uncontrolled intraoperative bleeding, suspected obturator nerve injury, and one case of poor selection of a patient who was found intraoperatively to have a 16-week uterus.
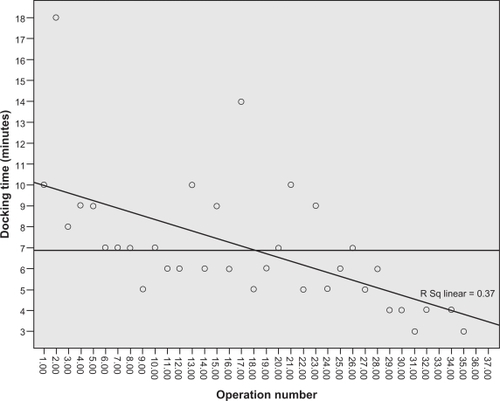
The average docking time was 6.89 minutes, with a median of 6 minutes. Those times were recorded for operations 16 and 17. Docking time improved markedly after operation 23. There was a significant inverse correlation between number of operations and docking time (P < 0.001, see ).
The mean robotic console operative time for all of the procedures was 92 minutes and the range was 40–240 minutes. Mean operative console time for simple hysterectomy was 125 (range 48–190) minutes, with an average operative time of 100 minutes, achieved at operation 5. There was marked improvement in operative time after operation 9. There was a significant inverse correlation between number of operations and operative time (P < 0.001, ). Mean operative console time for bilateral salpingo-oophorectomy was 47 (range 15–120) minutes, with an average time of 52.8 minutes. This time was achieved at operation 7. The operative time was markedly improved after operation 8. There was a significant inverse correlation between operation number and operative time (P = 0.047, ).
Figure 2 Operative console time has learning curves for (A) simple hysterectomy, (B) bilateral salpingo-oophorectomy, and (C) bilateral pelvic lymphadenectomy.
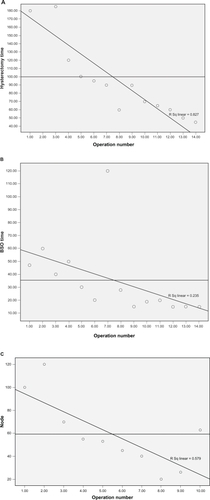
The mean operative console time for bilateral pelvic lymphadenectomy was 62 (range 20–120) minutes, with average time for node removal of 59.8 minutes. This time was achieved at operation 4. The operative time was markedly improved after operation 5. There was a significant inverse correlation between operation number and operative time (P = 0.017, )
Two radical hysterectomies were performed for early-stage cancer of the cervix, with a mean console time of 195 (range 180–210) minutes. The final pathology revealed these patients to be at high risk for recurrent disease, so they received postoperative radiation. One patient who had undergone subtotal hysterectomy for a leiomyosarcoma was referred to us, and underwent robot-assisted trachelectomy and bilateral pelvic lymphadenectomy, with a mean console time of 240 minutes until completion.
Mean estimated blood loss was 150 (range 100–1000) mL, as shown in . Complications occurred in five patients (see ). One patient whose procedure was converted to an open approach received two units of packed red blood cells. Another patient developed a ureteric fistula after simple hysterectomy for dysfunctional uterine bleeding and extensive endometriosis that required ureteric stents. Upon review, we found this was due to delayed thermal damage by the UltraCision harmonic scalpel. No case of wound infection occurred. Mean hospital stay was 3 days, with a range of 1–5 days.
Table 4 Summary of complications of robotic gynecology surgery in 35 women
Discussion
Robotic surgery can overcome the two main problems of laparoscopic surgery, ie, the limitation of four degrees of freedom of the instruments and two-dimensional vision on a television screen. Since the surgical robot was approved by the US Food and Drug Administration for use in gynecologic procedures in 2005, robot-assisted laparoscopic surgery has gained acceptance in the management of complex benign conditions and malignant disease. With experience, it has been shown to be effective and safe, with low morbidity and fewer conversions to open surgery than procedures performed by conventional laparoscopic techniques.Citation16,Citation17
The literature regarding use of robotic surgery in gynecologic surgery is limited. The first report of robotic hysterectomy was in 2002 by Diaz-Arrastin et al, who reported on 11 women who underwent robotic hysterectomy for a variety of conditions, one of which was endometrial cancer with conversion to an abdominal approach.Citation18 In a second report by the same group of investigators involving 41 patients, no patient had their procedure converted to an open approach.Citation19
The weakness of our study is that it was not randomized and involved a combination of different procedures performed for benign and malignant conditions. However, the study was strengthened by the fact that the patient population represents consecutive cases that were completed by a surgeon with extensive previous experience of both laparoscopic and difficult open pelvic surgery. Thomas and colleagues reported that their overall conversion rate for conventional laparoscopy surgery was five times higher (20% versus 4%) when compared with robotic-assisted surgery.Citation16 In addition, they found that conversion from a conventional laparoscopic approach to an open approach in hysterectomy did not decrease over time, whereas using the robotic assistant, with increasing experience, there was a lower incidence of conversion to abdominal hysterectomy. In our series, we found that most of the cases of conversion to an open procedure were in the first 15 patients. The overall conversion rate was 6.5%, and reasons for conversion included poor selection of patients for the robotic technique, in addition to some technical problems with the robotic system itself. The robotic setup and docking can be performed in a time-efficient manner. Although both setup and docking can be initially time-consuming, they are easy techniques to learn and have steep learning curves. Furthermore, our data show that draping for robotic surgery can be completed while the patient is in preparation for surgery (usually during anesthesia), so draping time need not affect overall operating room time. Our experience with the use of the da Vinci robot showed that docking time averaged 7 minutes and was 3–4 minutes for the last seven cases.
The docking process does require extra preoperative time compared with a laparoscopic or conventional procedure, but this can be achieved in less than 10 minutes with a relatively small amount of training. A seven-minute docking time represented a small proportion of the overall operating room time in our cases. Iranmanesh et al reported on 96 patients who underwent robot-assisted surgery over a 30-month period, with a median setup time of 22 (range 9–50) minutes and a median docking time of 10 (range 2–70) minutes. Surgeons with previous docking experience were significantly faster than inexperienced surgeons, with docking times of 8 (range 2–50) minutes versus 17.5 (range 10–70) minutes, respectively.Citation20 Therefore, docking times of 7 minutes appear to be acceptable. A longer operative time has been attributed to the combination of robot preparation and docking, as well as console time, which may be one of the drawbacks of robotic surgery. Our operative time in terms of console time was mainly dependent on the indication for surgery, with a mean time spent for simple hysterectomy of 125 (range 48–190) minutes compared with the range of 80–159 minutes reported in the literature.Citation20,Citation21 Diaz-Arrastia et al reported an operative time ranging from 4.5 to 10 hours.Citation18 Thomas et al reported that the mean operative time for a laparoscopic hysterectomy was 92.4 minutes, whereas the mean operative time for a hysterectomy with robotic assistance was 119.4 minutes. This difference was statistically significant (P < 0.0001). In their experience, the robotic console time also showed a significant learning curve, starting at a mean of 105.6 minutes in the first 25 cases and reducing to a mean of 49.4 minutes in the last 25 cases.Citation16
Our experience shows that there is definitely a learning curve for robotic surgery, and that the operative time decreases as one masters the technique of using the robot. However, in one of the cases of bilateral salpingo-oophorectomy (case 7), the robotic console time was prolonged; this was a case of tubo-ovarian abscess that was very difficult, but it was completed with the robot successfully with no complications ().
The complication rates for computer-enhanced hysterectomies were 17% in the report by Iranmanesh et alCitation20 and 11% in the report by Diaz-Arrastia et al,Citation18 with no urinary complications requiring conversion or a second surgical procedure. These complication rates are in the same range as those reported for classic laparoscopy, which range from 6% to 28%.Citation21–Citation23 In our series, the overall complication rate was 14%, but none of the complications were attributed to the use of the robot.
The drawback of the robotic system is its cost. The end point of this study was not an evaluation of the actual economic costs of robotic surgery, although costs will decrease as the market expands. From this point of view, it is essential to decide which procedures are most likely to benefit from the robot-assisted laparoscopic approach. Our experience can justify the use of such systems for operations that are carried out within confined spaces, such as extended hysterectomy with pelvic lymph node dissection, where the advantages of the system are clearly appreciated by the surgeon.
Because our study represents a single institution’s experience, its findings remain to be validated by a prospective multi-institutional or national Saudi registry. Given that more and more centers in Saudi Arabia are adopting the use of robots in their gynecological practice, the community will witness a steady progression toward robot-assisted gynecological surgery. This small series of patients who underwent robot-assisted gynecological surgery is the first experience of this technique reported by our institution. It appears to be a safe and practical surgical option. Our early experience shows that with proper training of the robotic team, technical difficulties with the robotic system are limited. Our experience also shows that there is a learning curve that requires performance of gynecological surgical procedures using the robot, in order to master this promising new technique in surgical technology.
Acknowledgements
The author thanks Dr Nisrin Anfinan and Dr Ahmad Al Marstani for helping with the robot-assisted surgery described in this report, as well as our anesthesia and nursing staff for their help.
Disclosure
The author reports no conflict of interest in this work.
References
- BonillaDJMainsLWhitakerRCrawfordBFinanMMagnusMUterine weight as a predictor of morbidity after a benign abdominal and total laparoscopic hysterectomyJ Reprod Med20075249049817694966
- ClaerhoutFDeprestJLaparoscopic hysterectomy for benign diseasesBest Pract Res Clin Obstet Gynaecol20051935737515985252
- KwohYSHouJJonckheereEAHayatiSA robot with improved absolute positioning accuracy for CT guided stereotactic brain surgeryIEEE Trans Biomed Eng1988351531603280462
- LanfrancoARCastellanosAEDesaiJPMeyersWCRobotic surgery: a current perspectiveAnn Surg2004239142114685095
- VidovszkyTJSmithWGhoshJAliMRRobotic cholecystectomy: learning curve, advantages, and limitationsJ Surg Res200613617217817059837
- IselinCFateriFCaviezelASchwartzJHauserJUsefulness of the Da Vinci robot in urologic surgeryRev Med Suisse2007327662768 French.18183810
- AdvinculaAPSurgical techniques: robot-assisted laparoscopic hysterectomy with the da Vinci surgical systemInt J Med Robot2006230531117520648
- NezhatCSaberiNSShahmohamadyBNezhatFRobotic-assisted laparoscopy in gynecological surgeryJSLS20061031732017212887
- HeemskerkJvan DamRvan GemertWGFirst results after introduction of the four-armed da Vinci surgical system in fully robotic laparoscopic cholecystectomyDig Surg20052242643116479111
- ChitwoodWRJrRodriguezEChuMWRobotic mitral valve repairs in 300 patients: a single-center experienceJ Thorac Cardiovasc Surg200813643644118692654
- RogersCGMetwalliABlattAMRobotic partial nephrectomy for renal hilar tumors: a multi-institutional analysisJ Urol20081802353235618930263
- AyavABreslerLBrunaudLBoisselPEarly results of one-year robotic surgery using the Da Vinci system to perform advanced laparoscopic proceduresJ Gastrointest Surg2004872072615358334
- GuttCNOniuTMehrabiAKashfiASchemmerPBüchlerMWRobot-assisted abdominal surgeryBr J Surg2004911390139715386325
- WeiseESWinfieldHNRobotic computer-assisted pyeloplasty versus conventional laparoscopic pyeloplastyJ Endourol20062081381917094760
- MuhlmannGKlausAKirchmayrWDa Vinci robotic-assisted laparoscopic bariatric surgery: is it justified in a routine setting?Obes Surg20031384885414738668
- ThomasNPayneMDFrancisRDauteriveMDA comparison of total laparoscopic hysterectomy to robotically assisted hysterectomy: surgical outcomes in a community practiceJ Minim Invasive Gynecol20081528629118439499
- LenihanJPJrKovandaCSeshadri-KreadenUWhat is the learning curve for robotic assisted gynecologic surgery?J Minim Invasive Gynecol20081558959418722971
- Diaz-ArrastiaCJurnalovCGomezGTownsendCJrLaparoscopic hysterectomy using a computer-enhanced surgical robotSurg Endosc2002161271127312085153
- FieldJBBenoitMFDinhTADiaz-ArrastiaCComputer-enhanced robotic surgery in gynecologic oncologySurg Endosc20072124424617186433
- IranmaneshPMorelPWagnerOJInanIPuginFHagenMESet-up and docking of the da Vinci surgical system: prospective analysis of initial experienceInt J Med Robot20106576020047195
- WattiezASorianoDCohenSBThe learning curve of total laparoscopic hysterectomy: comparative analysis of 1647 casesJ Am Assoc Gynecol Laparosc2002933934512101332
- GarryRFountainJMasonSThe EVALUATE study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomyBMJ200432812913314711749
- PomelCAtallahDLe BouedecGLaparoscopic radical hysterectomy for invasive cervical cancer: 8-year experience of a pilot studyGynecol Oncol20039153453914675672