?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
In developing countries, most childbirth occurs at home and is not assisted by skilled attendants. This situation increases the risk of death for both mother and child and has severe maternal and neonatal health complications. The purpose of this study was to explore pregnant women’s perceptions and utilization of traditional birth attendant (TBA) services in a rural Local Government Area (LGA) in Ogun State, southwest Nigeria.
Methods
A quantitative design was used to obtain information using a structured questionnaire from 250 pregnant women attending four randomly selected primary health care clinics in the LGA. Data were analyzed using Epi Info (v 3.5.1) statistical software.
Results
Almost half (48.8%) of the respondents were in the age group 26–35 years, with a mean age of 29.4 ± 7.33 years. About two-thirds (65.6%) of the respondents had been pregnant 2–4 times before. TBA functions, as identified by respondents, were: “taking normal delivery” (56.7%), “providing antenatal services” (16.5%), “performing caesarean section” (13.0%), “providing family planning services” (8.2%), and “performing gynaecological surgeries” (5.6%). About 6/10 (61.0%) respondents believed that TBAs have adequate knowledge and skills to care for them, however, approximately 7/10 (69.7%) respondents acknowledged that complications could arise from TBA care. Services obtained from TBAs were: routine antenatal care (81.1%), normal delivery (36.1%), “special maternal bath to ward off evil spirits” (1.9%), “concoctions for mothers to drink to make baby strong” (15.1%), and family planning services (1.9%). Reasons for using TBA services were: “TBA services are cheaper” (50.9%), “TBA services are more culturally acceptable in my environment” (34.0%), “TBA services are closer to my house than hospital services” (13.2%), “TBAs provide more compassionate care than orthodox health workers” (43.4%), and “TBA service is the only maternity service that I know” (1.9%). Approximately 8/10 (79.2%) of the users (past or current) opined that TBA services are effective but could be improved with some form of training (78.3%). More than three-quarters (77.1%) opposed the banning of TBA services. Almost 7/10 (74.8%) users were satisfied with TBA services.
Conclusion
Study findings revealed a positive perception and use of TBA services by the respondents. This underlines the necessity for TBAs’ knowledge and skills to be improved within permissible standards through sustained partnership between TBAs and health systems. It is hoped that such partnership will foster a healthy collaboration between providers of orthodox and traditional maternity services that will translate into improved maternal and neonatal health outcomes in relevant settings.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
According to the World Health Organization (WHO), current estimates of maternal mortality ratios are at more than 1000 per 100,000 live births in most African countries.Citation1 In developing countries, specifically in sub-Saharan countries, many women do not have access to skilled personnel during childbirth.Citation1 This lack of skilled attendance is one of the major factors responsible for the rising maternal and infant mortality.Citation1
The United Nations and the international community resolved through Goal 5 of the Millennium Development Goals (MDGs) to reduce the high maternal mortality ratio by three-quarters by 2015.Citation1,Citation2 Achieving this goal may be difficult, if urgent decisions are not taken to improve access to appropriate, adequate, and timely maternal health care.Citation3 Skilled personnel plus an enabling environment to provide essential obstetrics and neonatal care are necessary to achieve a significant reduction in maternal and infant mortality.
In Nigeria, the choice to deliver outside hospital settings could be motivated by varying factors such as economic, social, physical, cultural, or institutional.Citation4 Outside the hospital setting, women can be assisted by an attendant who may be unqualified. This attendant could be a traditional birth attendant (TBA), village midwife, member of the family, or neighbor.Citation4
According to the Nigeria Demographic and Health Survey 2008,Citation5 between 2003 and 2008, only 46% of women living in rural areas received antenatal care from a skilled provider (ie, doctor, nurse/midwife, auxiliary nurse/midwife), 28% of births were assisted by a skilled provider, and 25% of deliveries took place in a health facility. Expectant mothers who cannot access these services are left to make do with “alternatives” such as TBA services.Citation5
A TBA, as defined by the United Nations, is a person who assists mothers during childbirth and acquired her skills by delivering babies herself or through apprenticeship to other TBAs.Citation6 Throughout history, TBAs have been the main human resource for women during childbirth. Their role varies across cultures and times, but, even today, they attend the majority of deliveries in rural areas of developing countries.Citation7,Citation8 There is little doubt that they have a significant role when it comes to cultural competence, consolation, empathy, and psychosocial support at birth, all of which are important benefits for the mother and also for the newborn child. The WHO observes that TBAs can potentially improve maternal and newborn health at community level and, while the role of TBAs in caring for pregnant women and conducting deliveries is acknowledged, it is noted that they are generally not trained to deal with complications.Citation9 TBAs and village midwives have been employed in many interventions to reduce maternal mortality and improve pregnancy outcomes in developing countries, with mixed results.Citation10,Citation11
In Mexico, TBAs attend approximately 45% of all deliveries. Citation12 In Ghana, the ministry of health enlisted the assistance of traditional midwives to promote births as a medical event that should not be managed by specialists alone. In this arrangement, TBAs are allowed to handle “routine” birth while complicated pregnancies are referred to the district hospital or local clinics. This is done with the hope that it will assist in ensuring safe motherhood.Citation13 In Sierra Leone, TBAs conduct approximately 70% of deliveries, provide a significant amount of prenatal care, and are authorities in native methods of family planning.Citation14 As part of efforts to reverse the high toll of human suffering and loss associated with giving birth in Sierra Leone, the US Agency for International Development launched a program in 2007 with World Vision as partner, to minimize the maternal and child mortality risk, the main idea of which is to train women in traditional birth attendance.Citation14
It is estimated that between 60% and 80% of all deliveries in developing countries occur outside modern health care facilities, with a significant proportion of these attended by TBAs.Citation15 TBAs deliver the majority of women in Nigeria as in other developing countries.Citation15 An eastern Nigerian study showed that although 93% of rural women registered for prenatal care, 49% delivered at home under the care of TBAs.Citation16 Similarly, a study of 377 women who delivered before arrival at the hospital in Ogbomosho, southwestern Nigeria, revealed that 65% of the mothers had been delivered by a TBA, while 73.7% had sought help from them for retained placenta with bleeding.Citation17 In Chanchaga LGA of Niger State in north central Nigeria, 84% of households interviewed utilized the services of a TBA or village health worker.Citation18
In a study done in Edo State, south Nigeria, to assess the role of TBAs in health care delivery, respondents believed that TBAs could play meaningful roles in family planning, screening for high-risk pregnant mothers, fertility/infertility treatment, and maternal and child care services. Rural dwellers prefer to use the services of TBAs as compared with their urban counterparts. Reasons for their preference included: the option of home delivery, TBAs’ availability, accessibility, inexpensive services, and rural dwellers’ faith in the efficacy of their services.Citation19
In yet another study in Edo State of 45 TBAs, which assessed the services provided by them and their management practices (ie, management of complications, umbilical cord care, and infection control methods), findings revealed their unsafe practices. It was recommended that a more holistic training program including monitoring and supervision should be provided to them.Citation20
Efforts to formalize the role of TBAs in maternal and neonatal health programs have had limited success. TBAs continued attendance at home deliveries suggests, however, their potential in influencing maternal and neonatal outcomes.Citation19,Citation21
A South African study to evaluate the training of TBAs in human immunodeficiency virus/acquired immunodeficiency syndrome care and service delivery revealed that after the training, significantly more TBAs conducted prenatal checkups, assessed the baby’s position in the uterus, and took the mother’s and baby’s pulse, and fewer TBAs conducted abnormal or complicated deliveries. Investigators concluded that training of TBAs can increase their knowledge, improve their attitudes, and reduce risk practices.Citation22
In recent years, there has been increasing debate over the usefulness of TBAs in maternal health care.Citation23,Citation24 Opponents of TBA care are of the view that TBAs have done little to improve maternal health. They opine that TBAs have frustrated laudable efforts made by governments in sub-Saharan Africa to reduce maternal mortality, while proponents have expressed the need for a sustained partnership with TBAs as a strategy to improve access to basic maternity care in rural areas to achieve significant reductions in maternal mortality. However, this debate has been between orthodox and traditional health workers,Citation7,Citation23–Citation26 and rarely has the opinion of the beneficiaries of such services (ie, pregnant women) been reported.Citation8
With the rising use of TBA services by pregnant women who also utilize modern maternity services, this study sought to determine their knowledge, perception, and use of TBAs and their services; in addition, the study aimed to determine factors influencing the use of TBA services. It is hoped that findings from this study will provide insights into pregnant women’s opinion of TBAs and their role in maternal health care and factors influencing pregnant women’s dual maternal health care-seeking behavior. This will assist in tailoring such services to their needs.
Methods
Study area
Ifo LGA, with its headquarters in Ifo town, is located in Ogun State, southwest Nigeria. It has a land area of 82,000 km2 and shares boundaries with Yewa South LGA in the west, Ewekoro LGA in the north, Obafemi-Owode LGA in the east and Ado-Odo/Ota in the south.Citation27 According to the 2006 census, Ifo LGA has a population of 524,837.Citation26
There are eleven wards: Ifo I, Ifo II, Ifo III, Agbado Central, Akute-Ajuwon, Isheri, Oke-Aro-Ibaragun, Ososun, Sunren, Coker, and Ibogun.Citation27 The population is predominantly Egba with Aworis and other subethnic groups also coexisting. The people are predominantly farmers and traders.Citation27
General infrastructure
The council area administrates urban and rural settlements. As Ifo shares a boundary with Ado-Odo/Ota, which shares a boundary with Lagos State, development of infrastructure is ongoing. The LGA has 63 public primary schools and eleven secondary schools. There is also an appreciable number of private educational institutions.Citation27 A range of social services such as health care delivery, primary education, motor parks, markets, and road maintenance are provided by the LGA.
Health services
One of the pioneer model primary health care (PHC) centers in the country is situated in Pakoto. The model PHC was set up to meet the diverse health needs of the people. In addition to this, the LGA has a general hospital, ten other PHC centers (including those in Olose, Pakoto, Ibogun, and Coker) and a number of private hospitals scattered across the LGA. Efforts of both the public and private hospitals and clinics are complemented by those of the TBAs, who take care of pregnant women in the villages (remote areas), where hospitals and PHCs are either sparse or nonexistent.
Study design
This was a descriptive cross-sectional study.
Study population
The study was carried out among registered pregnant women attending the antenatal clinics of selected PHCs in Ifo LGA.
Sample size estimation
This was done using the formula n = Z2pq/d2. Where n = sample size for a population > 10,000; Z = standard normal deviate = 1.96; p = prevalence rate, ie, proportion in target population estimated to have the particular characteristic of interest, 50%; q = 1 − p; and d = degree of accuracy, set at 0.05.
Therefore,
However, since the study population was <10,000, the sample size was calculated thus: nf = n/1 + (n/N). Where, nf = minimum sample size for population <10,000; n = minimum sample size for population >10,000; and N = estimated total population of pregnant women in Ifo LGA, which was approximately 600.
Therefore,
This was increased to 260 to allow for 10% nonresponse, giving a total of 260 questionnaires that were administered. Since four PHCs were used, 65 pregnant women were recruited from each PHC.
Sampling
A multiple-stage sampling method was used:
Stage 1: selection of 4/11 wards (namely, Ifo I, Ifo II, Ifo III, and Ibogun) by simple random sampling method.
Stage 2: in each of these wards, one PHC was randomly chosen (balloting). These were: Pakoto (Lagos University Teaching Hospital) PHC, Olose PHC, Ibogun PHC, and Coker PHC.
Stage 3: 65 pregnant women from each PHC were consecutively recruited between February and March 2010 until the desired sample was obtained.
Data collection
Data were collected using a semistructured interviewer-administered questionnaire, adapted from previous studies.Citation4,Citation26 The questionnaire was pretested among 30 pregnant women attending a PHC center in Obafemi-Owode LGA of Ogun State and amended as appropriate. Informed consent was obtained from the pregnant women after they received information about the study purpose and objectives. Information obtained included sociodemographic characteristics of respondents, knowledge of respondents concerning TBAs and their roles, and attitude to and utilization of TBA services in the LGA. Interviewers were eight trained medical students (five females and three males) in their penultimate year of study who were undergoing their rural health posting in the LGA at the time of the study.
Data management
Epi Info (v 3.5.1; Centers for Disease Control and Prevention, Atlanta, GA) statistical software was used for data entry, validation, cleaning, and analysis. Frequency distributions were generated for all categorical variables and means and standard deviations were determined for continuous variables. Test of significant difference for associations was done using the chi-square test and multivariate analysis. P value was set at <0.05. Knowledge levels of TBA issues were categorized into good, fair, or poor based on responses to questions assessing who TBAs were, their functions/services in the community, whether complications can arise from TBA care, and, if yes, examples of such complications. Attitude to TBA care was also categorized as positive or negative depending on respondents’ answers to various questions, including on whether respondents perceived that: the services of TBAs were effective, TBAs had adequate knowledge and skills to manage obstetric conditions, they should be banned, or TBAs would do better with some form of training. Each correct response was rated one mark and each incorrect response did not attract any mark. Possible maximum score was determined and knowledge and attitude categories were determined based on the proportion of maximum score that was obtained.
Limitations
Insufficient funds limited the scope of the study. Questionnaires were distributed in the health centers for convenience of recruiting pregnant women.
Results
A total of 260 questionnaires were administered. Ten were discarded as they were incompletely filled out, yielding a response rate of 96.2%.
Sociodemographics of respondents
Almost half (48.8%) of the respondents were in the age group 26–35 years, with a mean age of 29.4 ± 7.33 years. More than three-quarters (76.8%) were married; slightly more than half (52.4%) were of the Christian faith, while 46.8% were of the Islamic faith. The predominant ethnic group was Yoruba, which constituted 78.4% of the respondents. Slightly above half (54.0%) had attained secondary education, while only 20% had attained tertiary education. Approximately 4/10 of the respondents were either unskilled (42.4%) or unemployed (38.4%). About two-thirds (65.6%) of the respondents had been pregnant 2–4 times previously, 14% had been pregnant more than four times previously, while another 0.4% were in their first pregnancy ().
Table 1 Sociodemographic data of respondents
Knowledge of TBAs and their services
Approximately 9/10 (92.4%) respondents were aware of who TBAs were. Of those who knew about TBAs, their mothers (31.2%) were their chief sources of information. Other sources included: other family members (including fathers and husbands) (33.8%), friends (17.7%), neighbors (13.9%), and health workers (3.5%) ().
Table 2 Knowledge concerning traditional birth attendants (TBAs) and their services
Functions of TBAs, as identified by the respondents, were: “taking normal delivery” (56.7%), “providing antenatal services” (16.5%), “performing cesarean section” (13.0%), “providing family planning services” (8.2%), and “performing gynecological surgeries” (5.6%) ().
Approximately 6/10 (61.0%) respondents either agreed or strongly agreed that TBAs have adequate knowledge and skills to care for pregnant women. Only 31.1% either disagreed or strongly disagreed that TBAs’ knowledge/skills were adequate to care for pregnant women. Forty-two percent of respondents either agreed or strongly agreed to the adequacy of the hygiene practices of TBAs. However, 49.7% either disagreed or strongly disagreed ().
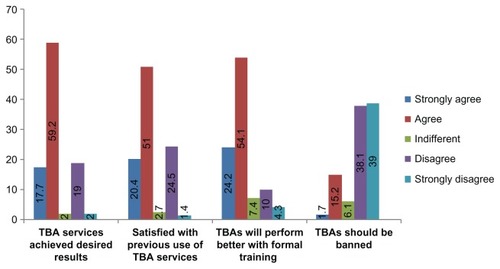
Figure 1 Respondents’ opinion on some issues concerning traditional birth attendant (TBA) services (numbers expressed in %).
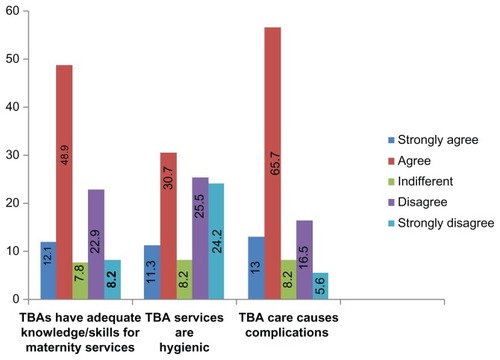
Almost 7/10 (69.7%) of the respondents either agreed or strongly agreed that complications could arise from TBA services. However, 22.1% either disagreed or strongly disagreed and 8.2% were indifferent to this opinion (). Concerning associated complications that could arise from TBA care, precisely 86.1% identified excessive/prolonged bleeding, 25.1% infections, 14.7% damage to the reproductive organs, and 13.0% thought that “TBAs could transfer witchcraft” ().
Attitude of respondents to TBA services
More than three-quarters (76.9%) of the ever users either agreed or strongly agreed that TBA services were effective. However, 21.0% either disagreed or strongly disagreed. About 8/10 (78.3%) respondents either agreed or strongly agreed that services of TBAs could be improved with some form of training. However, 14.3% either disagreed or strongly did so ().
Less than one-fifth (16.9%) of respondents either agreed or strongly agreed that TBA services should be banned. However, more than three-quarters (77.1%) either disagreed or strongly disagreed that TBA services should be banned. Less than one-tenth (6.1%) were indifferent to this opinion ().
Utilization of TBA services
Almost two-thirds (63.6%) of those who were aware of TBA services had ever used such services, while 44.6% of them were currently using TBA services at the time of the study. About two-thirds (61.9%) of previous users said they were continuing to use TBA services for their current pregnancies. Among respondents that had ever used TBA services, 81.0% used them for routine antenatal care, 36.1% used them for normal delivery service, 2% for “special maternal bath to ward off evil spirits,” 15.6% to provide “concoctions for mothers to drink to make baby strong,” and 23.1% for family planning services (). Among ever users of TBA services, 76.2% were satisfied with their services and 22.5% were dissatisfied with their services. Reasons for using TBA services among ever users were: “TBA services are cheaper” (49.3%), “TBA services are more culturally acceptable in my environment” (36.1%), “TBA services are closer to my house than hospital services” (12.5%), “TBAs provide more compassionate care than orthodox health workers” (43.5%), and “TBA service is the only maternity service that I know” (2.1%) (data not shown).
Table 3 Utilization of traditional birth attendant (TBA) services
Among current users, 80.6% used TBAs for routine antenatal services, 29.1% for normal delivery service, 2.9% to obtain “maternal bath to ward off evil spirits,” 15.5% to obtain “concoctions to make baby strong,” and 2.9% for family planning services (). Of current users, 74.7% were satisfied with their services, while 25.2% were not satisfied. Reasons for using TBAs were: “TBA services are cheaper” (55.3%), “TBA services are more culturally acceptable in my environment” (30.1%), “TBA services are closer to my house than hospital services” (12.6%), “TBAs provide more compassionate care than orthodox health workers” (52.4%), and “TBA services are the only maternity services that I know” (1.9%) (data not shown).
Respondents’ levels of knowledge concerning TBAs and issues relating to their services revealed that less than half (43.3%) of the respondents had good knowledge of TBA issues, 42.9% fair knowledge, and 13.9% poor knowledge. Slightly less than half (49.4%) of the respondents had a positive attitude to TBA services.
Comparing respondents’ sociodemographics with knowledge levels of issues relating to TBA services, attitude to TBA services, and utilization of TBA services, only respondents’ religion (P = 0.0049), educational level (P = 0.0393), and current use (P = 0.0119) were significantly related with levels of knowledge of TBA services (data not shown). Educational level (P = 0.000), occupation (P = 0.0016), ever use (P = 0.000), and current use of TBA services (P = 0.000) were significantly associated with a positive attitude toward TBA services.
All the sociodemographics (age, marital status, religion, ethnicity, educational level, occupation, and number of previous pregnancies) were significantly associated with respondents that had ever used TBA services (). Also, having a positive attitude toward TBA services and satisfaction with services provided was significantly associated with ever users. However, only educational level, occupation, a positive attitude, and satisfaction with TBA services were significantly associated with current use (). Those with less education, who were unskilled or unemployed, and had a positive attitude to and satisfaction with TBA services tended to currently use TBA services. Sociodemographics (except gravidity) were however not significantly associated with reasons for using TBA services among ever users. Similarly, none of the sociodemographics were significantly associated with reasons for use among current users. Only religion (P = 0.0000) and gravidity (P = 0.0078) were significantly associated with services obtained from TBAs among ever users, while, for current users, religion (P = 0000) was the only sociodemographic characteristic associated with services obtained from TBAs.
Table 4 Association between sociodemographics and respondents’ use of traditional birth attendant (TBA) services (ever users)
Table 5 Association between sociodemographics and respondents’ use of traditional birth attendant services (current users)
For ever users, none of the sociodemographics was significantly associated with satisfaction with services obtained from TBAs, while, for current users, age (P = 0.0079), ethnicity, and educational level (P = 0.0287) were significantly associated with satisfaction with services obtained from TBAs.
A multivariate analysis of sociodemographic characteristics of respondents, knowledge about TBA services, attitude to TBA services, reasons for using, services obtained, and satisfaction with services revealed that only marital status (odds ratio [OR] = 8.499, P = 0.000), religion (OR = 0.399, P = 0.039), number of previous pregnancies (OR = 3.590, P = 0.004), positive attitude to TBA services (OR = 47.190, P = 0.000), and satisfaction with services (OR = 3.743, P = 0.003) were significantly associated with those who had ever used TBA services (likelihood ratio: 136.031, degree of freedom = 11, P = 0.0000). Positive attitude to TBAs and their services was noted to have the strongest association with the ever users (OR = 47.190). Only positive attitude to TBA services (P = 0.000, OR = 25.057) was significantly associated with current use of TBA services (likelihood ratio: 116.915, degree of freedom = 6, P = 0.0000) (data not shown).
Discussion
The study assessed the 250 pregnant women’s knowledge of TBAs, their attitudes toward and utilization of TBA services, and factors influencing these variables. Almost half of the respondents were within the age group 26–35 years, more than three-quarters were married, and of the Yoruba ethnic group (consistent with the study area, which is in southwest Nigeria, where the predominant tribe is Yoruba). Just over half (54%) of the respondents had secondary education while only 20% had tertiary education and 4/10 of the women were either unskilled or unemployed. This is to be expected in a rural setting where women have limited access to formal or higher education and which translates into either unemployment or low income–generating employment. Almost two-thirds of the respondents had been pregnant 2–4 times previously, while 14% had had more than four previous pregnancies. The fertility trend among the respondents is in contrast to the expectation of a typical rural African setting, where a relatively higher fertility rate usually characterizes such settings. Limited knowledge, access, and sociocultural barriers influence the use of family planning.
Virtually all respondents knew who TBAs were and family members were the most popular source of information about TBAs and TBA services, which thus reflects the considerable family influence in maternal health–seeking behavior. More than half of the respondents identified TBAs’ role as delivering, with <20% of them either saying TBAs provide antenatal or family planning services, or, erroneously, cesarean sections or gynecological surgeries. This is indicative of the poor level of knowledge respondents have about TBAs and their roles, which may be due to their relatively low level of education, and has serious implications for the health-seeking behavior of these respondents as they could demand services from TBAs that they are not trained to provide, leading to adverse health consequences for these women and their babies. This is corroborated by the observation that >60% of respondents either agreed or strongly agreed that TBAs have adequate knowledge and skills to manage pregnant women. This compares to a study done in Ado-Odo/Ota LGA of Ogun State, in which about 53.0% of the respondents felt TBAs had adequate skills to manage obstetric conditions (unpublished data), but contrasts with a study done in Oredo LGA of Edo State, in which only 24% of the respondents felt TBAs had adequate skills to manage obstetric conditions.Citation17 However, some 7/10 respondents acknowledged that complications such as excessive/prolonged bleeding, infections, damage to reproductive organs, and transfer of witchcraft could arise from utilizing TBA services, which is in contrast with the Edo State study, in which about 52% of the respondents did not associate TBA patronage by pregnant women with possible complications.Citation17
That more than 70% of respondents believed that TBA services are effective and could be improved with adequate training is indicative of their acceptance of TBAs and their services. A study done in Sokoto in northwest Nigeria showed that trained TBAs are able to recognise high-risk pregnancies and deliveries for referral to health institutions. In addition, trained TBAs provided some form of maternal and child health services such as antenatal care, advice on immunization for pregnant women and their children, and referral for postpartum care including family planning services;Citation27 7/10 previous users of TBA services reported to have been satisfied with such services. Interestingly, some 77.1% of respondents opposed or strongly opposed the banning of TBAs.
Utilization of TBA services among respondents revealed that almost two-thirds of them had ever used TBA services, with >60% of previous users continuing to use TBAs for their current pregnancies. Some 4/10 of them were first-time users of TBA services. Antenatal care was the most popular service sought from TBAs among ever users or current users followed by normal delivery and family planning services. An interesting observation is the procurement of “special maternal birth to ward off evil spirits” or “concoctions for mothers to drink to make baby strong.” This observation highlights the influence of sociocultural beliefs on health-seeking behavior and the implications it has on health outcomes – in this case, risk of damage to maternal organs and occurrence of congenital disorders. That more than 7/10 previous or current users expressed satisfaction with services obtained and would recommend such services to families and friends suggests respondents’ firm belief in TBA care. However, in spite of this firm belief, it was observed that respondents combined TBA care with orthodox maternity care. What could inform the use of both orthodox and traditional maternity care? The answer may be due to compelling limitations in terms of geographic and financial access. Cultural and attitudinal factors may also have influenced the use of both services concurrently. Further studies using qualitative techniques may provide answers.
Exploring respondents’ positive attitude to and consequent utilization of TBA services revealed that reasons for use varied from cost and proximity limitations, cultural acceptability, to TBAs providing more compassionate care than orthodox health workers. Again, these echo the factors influencing care-seeking behavior. TBAs have been reported to be more compassionate in patient care, hence promoting their patronage.Citation17,Citation18,Citation22
Although respondents were limited in their knowledge of services that should be provided by TBAs, this was not reflected in their attitude to and utilization of TBA services. The majority were of the opinion that, although TBAs have limited knowledge and skills when compared with orthodox health workers, the knowledge and skills they do have were believed to be adequate enough for the TBAs to provide effective services for pregnant women. Could these perceptions have been as a result of respondents’ limitations in terms of geographic and financial access, perceived empathy from TBAs, satisfaction with services received, and cultural influence, among others? Again, these questions will require further exploration using qualitative studies.
In exploring the likely association between sociodemographics of respondents and their knowledge, attitude to, and utilization of TBA services, educational level (P = 0.005), occupation (P = 0.039), religion (P = 0.015), and current use (P = 0.012) were found to be significantly associated with knowledgeable, older, married, secondary-educated, Muslim, Yoruba, and unskilled/unemployed respondents, who had better knowledge of TBAs and their services. Regarding attitude, educational level (P = 0.000), occupation (P = 0.002), and previous (P = 0.000) and current use (P = 0.000) were significantly associated with positive or negative attitudes. Respondents with secondary education as their highest educational attainment, who were unskilled/unemployed, and who were past and/or current users tended to have a positive attitude to TBAs and their services.
Disaggregating ever and current users revealed that all sociodemographics of the respondents (age, marital status, religion, ethnicity, educational level, occupation, and gravidity) were significantly associated with those who had ever used. Having a positive attitude toward TBA services and satisfaction with services obtained from TBAs was also significantly associated with those who had ever used TBA services. For current users, educational level, occupation, and a positive attitude to and satisfaction with use of TBA services were significant. Logistic regression analysis showed, however, that marital status, religion, ethnicity, gravidity, and positive attitude to and satisfaction with TBA services were still significantly associated with ever use, while positive attitude to TBA services was the only factor significantly associated with current use. Ever users with positive attitude to TBA services were 47× more likely to use such services, while current users with positive attitude were 25× more likely to use TBA services. This truly revealed that positive attitude toward TBAs and their services is the strongest influencing factor on past or current use. This attitude may be influenced by different factors including access (geographic, financial) and sociocultural beliefs. Future interventions to improve access to maternity services should take these into consideration.
Conclusion
This study has revealed respondents’ very positive attitude to TBA services in spite of their limited knowledge of TBA roles in maternal health care, as evidenced by their call for more training for TBAs to improve their knowledge and skills in maternal health care delivery. This confidence in TBA care is further corroborated by their relatively high use of these services.
In view of the “perceived vital” role of TBAs as seen by these respondents, equipping them with knowledge and skills within accepted standards is therefore recommended. This will ensure that users receive optimum care within their limits of practice. Such partnerships should incorporate supportive supervision and skills to recognize and refer high-risk pregnancies in a timely manner. This will ensure that women who cannot access orthodox maternity services can be guaranteed appropriate, accessible, and adequate care in close proximity to their residence.
Disclosure
The authors declare no conflicts of interest in this work.
References
- World Health Organization (WHO)World Health Report 2005: Make Every Mother and Child CountGenevaWHO2005
- WHORevised 1990 Estimates of Maternal Mortality: A New Approach by WHO and UNICEFGenevaWHO1998
- HodgesAChildren and Women’s Rights in Nigeria, a Wake-up call: Situation and Analysis 2001AbujaNational Planning Commission2001
- AhmedOAOdunukweNNAkinwaleOPKnowledge and practices of traditional birth attendants in prenatal services in Lagos State, NigeriaAfr J Med Sci20053415558
- National Population Commission and ICF MacroNigeria Demographic and Health Survey 2008AbujaNational Population Commission and ICF Macro2009
- WHOTraditional Birth Attendants: A Joint WHO/UNFPA/UNICEF StatementGenevaWHO1992
- BergströmSGoodburnEThe role of traditional birth attendants in the reduction of maternal mortalityStudies in HSO&P2001178589
- JemalYTedlaMTilahunNDawitSRevisiting the exclusion of traditional birth attendants from formal health systems in EthiopiaAMREF Discussion Paper Series20103 Discussion Paper No. 003/2010
- WHOGlobal Action for Skilled Attendants for Pregnant WomenGenevaWHO2004
- GloydSFloranoFSeundaMChadrequeMANyangeziJMPlatasAImpact of traditional birth attendant training in Mozambique: a controlled studyJ Midwifery Womens Health20014621021611603632
- RayAMSalihuHMThe impact of maternal mortality interventions using traditional birth attendants and village midwivesJ Obstet Gynaecol200424151114675972
- ChakravartyJBhattacharyaSCameyXCTraditional birth attendants in Mexico: advantages and inadequacies of care for normal deliveriesSoc Sci Med19964321992078844924
- GeurtsKLWell-being and birth in rural Ghana: local realities and global mandatePaper prepared for the Fifth Annual African Studies Workshop “Cross-Currents in Africa,”University of Pennsylvania, Philadelphia, PAOctober 17, 1997 Available from: http://www.africa.upenn.edu/Workshop/geurts.htmlAccessed November 14, 2011
- US Agency for International Development (USAID)Sierra Leone Training traditional birth attendants educating pregnant women and mothers [web page on the Internet]Washington DCUSAID2009 [updated March]. Available from http://www.usaid.gov/sl/sl_new/news/tba.htmAccessed November 15, 2011
- TsuiAOWasserheitJNHaagaJGReproductive Health in Developing Countries: Expanding Dimensions, Building SolutionsWashington DC1996
- ImogieOIThe practice of traditional birth attendants and women’s health in Nigeria25th Congress Medical Women’s International Association2000 Available from: http://www.regional.org.au/au/mwia/papers/full/28_imogie.htmAccessed January 16, 2012
- FajemilehinRBFactors influencing high rate of ‘born-before-arrival’ babies in Nigeria – a case control study in OgbomoshoInt J Nurs Stud199128113181856028
- ItinaSMCharacteristics of traditional birth attendants and their belief and practices in the Ofot clan, NigeriaBull World Health Organ1997756537538
- ImogieAOAgwubikeEOAlukoKAssessing the role of traditional birth attendants (TBAs) in health care delivery in Edo State, NigeriaAfr J Reprod Health2002629410012476721
- OfiliANOkojieOHAssessment of the role of traditional birth attendants in maternal health care in Oredo Local Government Area, Edo State, NigeriaJournal of Community Medicine and Primary Health Care20051715560
- FalleTYMullanyLCThatteNPotential role of traditional birth attendants in neonatal healthcare in rural southern NepalJ Health Popul Nutr2009271536119248648
- PeltzerKHendaNTraditional birth attendants, HIV/AIDS and safe delivery in the Eastern Cape, South Africa – evaluation of a training programmeS Afr J Obstet Gynaecol2006123140145
- SibleyLMSipeTATransition to skilled birth attendance: is there a future role for trained traditional birth attendants?J Health Popul Nutr200624447247817591344
- AnaJAre traditional birth attendants good for improving maternal and perinatal health? YesBMJ2011342d331010.1136/bmj.d331021673001
- LartsonLISodipeOAEbrahimGJAbelRPerspectives in primary care: the trained traditional birth attendant: a study of her role in two culturesJ Trop Paediatr1987332934
- WikipediaIfo [web page on the Internet] Available from: http://en.wikipedia.org/wiki/ifo,_NigeriaAccessed March 14, 2010
- AkpalaCOAn evaluation of knowledge and practices of trained birth attendants in Bodings, Sokoto state, NigeriaJournal of Tropical Medical Hygiene1994974650