Abstract
The proposal to restore vaginal microbiota using biotherapeutic agents ended with controversial results. Vaginal microbiota modifications from eubiosis to dysbiosis (desquamative inflammatory vaginitis, “aerobic vaginitis”) and pathobiosis have recently been demonstrated to have a pivotal role in women’s clinical health. Bacterial vaginosis (BV) and its related women’s pathology seem to be “the most common vaginal infections” in women; the Center for Disease Control (CDC) recommended treatment for this pathology: metronidazole, clyndamicin or other well known treatment such as dequalinium chloride, unfortunately, has been demonstrated to fail in control of this infection and especially in its recurrence rates. A long-lasting vaginal approach with a symbiotic drug (Lactobacillus rhamnosus BMX 54 + lactose) (NORMOGIN™) has demonstrated on a large sample of women enrolled in clinical trials (more than 3000 patients) not only to be able to significantly reduce the BV recurrences, after the CDC standard of care administration, but also to control the vaginal pathobiosis pathway, restoring the physiological eubiosis from dysbiosis. These results are really very encouraging and clearly demonstrate that a symbiotic long-lasting vaginal application of a selected Lactobacillus population plus a prebiotic could be helpful if added to the recommended standard of care.
Bacterial vaginosis (BV) is a common vaginal condition among worldwide and US women:Citation1 a recent analysis of the National and Nutrition Examinations Surveys demonstrated that almost one-third of women were found positive for BV.Citation2 BV is a polymicrobial clinical syndrome resulting in replacement of the normal production of Lactobacillus spp. in the vagina with a high concentration of facultative pathogens anaerobic gram – bacteria such as Gardnerella Vaginalis, Ureaplasma, Prevotella, Mobiluncus, Ureaplasma and Mycoplasma.Citation3
Considering that almost one-third of the worldwide women are affected by this pathology and that the relationship between BV and women’s disease such as pelvic inflammatory diseases, infertility and sexually transmitted infections plus a condition such as pregnancy complications are widely demonstrated, it seems obvious to consider BV as a threat for women’s health.Citation4
Moreover, from a symptomatic point of view, BV is a “Silent Vaginitis” as the only AMSEL criteria for BV diagnosis perceived from women, the “vaginal discharge”, can often be lived by women as a “kind of physiologic condition affecting every women”.Citation4
The standard of care for BV treatment recommended from the CDC (Center for Disease Control) as metronidazole or clyndamicin for 7 days, or other treatment such as dequalinium chloride or Fluomizin, have failed to control relapses of BV (almost 40% of the recurrence rate at 3 months and 50% of relapses at 6 months), representing a public health related problem for women’s health.Citation4
We also have to remember that the vaginal ecosystem “eubiosis” seems to become “pivotal” in women’s health considering the correlation of the relationships between vaginal microbiota and vaginal microbioma in vaginal health.Citation4,Citation5
Human vaginal microbiota is “relatively stable” in healthy women and, according to what Albert Doderlein said in 1892 by using culture methods, it possesses a predominance of gram+ rods named after him “Doderlein Lactobacillus”.Citation6
More than 120 years later it was universally recognized and accepted that the lactobacilli are the predominant species of the human vaginal microbiota for women in good health and that they have a “key role” in maintaining an acidic environment able to protect women against virus and bacteria responsible for opportunistic infections or sexually transmitted diseases (STDs).Citation7
It was remarkable to observe that the human species is the only one with this relative abundance of lactobacilli inside the vagina (more than 70%) while other mammalians present no more than 1% of lactobacilli in their vaginal microbiota.Citation4,Citation7
Since the CDC standard of care for BV (metronidazole/clyndamicin) or other treatments such as dequalinium chloride or Fluomizin have shown to be ineffective to control BV recurrence rates and to restore vaginal eubiosis, there is a need to look for an alternative medical approach able to do it.Citation4
Biotherapeutic agents (living microorganisms used to prevent or to treat human diseases by interacting with the natural microbial ecology of the host) have been used to treat also vaginal infections during time.Citation8
Vaginal biotherapeutic agents can be divided into three different classes:
1) Prebiotic (usually carbohydrates that typically stimulate the growth of the body’s indigenous lactobacilli)Citation8
2) Probiotic (living microorganisms – usually lactobacilli)Citation8
3) Symbiotic (a combination of the two previous concepts – prebiotics plus probiotics)Citation8
A lot of clinical trials have been done using probiotics (usually lactobacilli) in order to treat BV and to restore vaginal eubiosis, but they ended with controversial results;Citation8 unfortunately, a review published in EFSA journal pointed out the ineffectiveness of probiotics for oral use in restoring vaginal microbiotaCitation9 and another review published by Cochrane showed that probiotics clinical trials were inconsistent to demonstrate clinical efficacy in women affected by BV.Citation10
An interesting strategy to treat women affected by an intractable BV seems to be the vaginal microbiome transplantation (VMT) but its therapeutic efficacy should be further determined in randomized, placebo-controlled clinical trials.Citation11
Lactobacillus rhamnosus BMX 54 + lactose is a vaginal drug in tablets indicated to restore vaginal eubiosis containing a symbiotic vaginal biotherapeutic agent and is composed of:
Lactobacillus rhamnosus BMX 54 as probiotic – a specific lactobacillus deposited at Institute Pasteur of Paris under the Budapest Treaty
Lactose as prebiotic
This drug is manufactured by Laboratori Baldacci in Italy and available in Italy, Europe (Portugal) and South America (Brazil).
About 3000 women affected by BV have been enrolled in clinical trials and treated with this symbiotic biotherapeutic agent in the form of vaginal tablets, demonstrating that a combination therapy between standard of care for BV (metronidazole 500 mg twice daily for 1 week) followed by a long-term course of Lactobacillus rhamnosus BMX 54 + lactose leads to a significant reduction in the recurrence rates of BV not only during treatment but also during the following 6 months.Citation4,Citation5,Citation12–Citation22
Figure 1 Number of women with BV or restored vaginal flora after 2 months (A), after 6 months (B) and after 9 months (C) of treatment with metronidazole alone (group A) or metronidazole plus NORMOGIN™ (group B). A significant statistical difference has been shown after 2 months (p < 0.04), 6 months (p < 0.0001) and 9 months (p < 0.0001) of treatment between group B and group A.
Note: Reproduced by permission from Springer Nature. Arch Gynecol Obstet. Recine N, Palma E, Domenici L, et al. Restoring vaginal microbiota: biological control of bacterial vaginosis. A prospective case-control study using Lactobacillus rhamnosus BMX 54 as adjuvant treatment against bacterial vaginosis. 23(1):101–107. Copyright (2016).Citation16
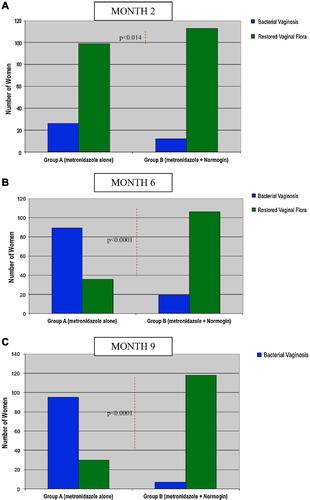
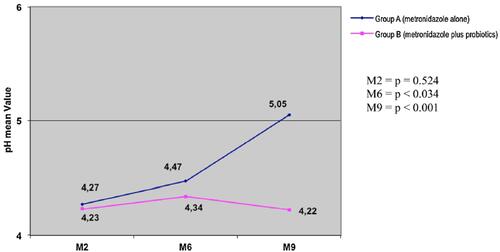
Figure 2 Vaginal pH values after 2, 6 and 9 months of treatment with metronidazole alone (group A) or metronidazole plus NORMOGIN™ (group B). A significant statistical difference has been shown after 6 months (p < 0.034) and 9 months (p < 0.001) of treatment between group B and group A.
Note: Reproduced by permission from Springer Nature. Arch Gynecol Obstet. Recine N, Palma E, Domenici L, et al. Restoring vaginal microbiota: biological control of bacterial vaginosis. A prospective case-control study using Lactobacillus rhamnosus BMX 54 as adjuvant treatment against bacterial vaginosis. 23(1):101–107. Copyright (2016).Citation16
The vaginal administration of Lactobacillus rhamnosus BMX 54 + lactose is usually done for almost 6 months after the standard of care treatment indicated for BV and it needs to be done according to this specific treatment protocol: 1 vaginal tablet daily (at bedtime before sleeping) for 6–12 days followed by 2 vaginal tablets weekly for 2 months and then 1 vaginal tablet weekly for 6 months.Citation4,Citation5,Citation12–Citation22
In a clinical trial performed in pregnant women, the use of this symbiotic vaginal drug for 12 weeks once a week vs no-treatment (used as control group) supported its effectiveness in preventing the development of abnormal vaginal microflora and in controlled cervical parameters that could represent risk factors for preterm delivery.Citation18
A very long-lasting clinical trial (24 months) clearly demonstrated the effectiveness of this vaginal approach in the control of vaginal pH in 40 women affected by BV during long-term treatment with the weekly administration of a vaginal tablet.Citation14
Considering the large sample size of women enrolled in the clinical trials during the last years and the consequent obtained results, it seems that this drug present in vaginal tablets manufactured by Laboratori Baldacci SpA, Italy, and available in Italy, Europe (Portugal) and South America (Brazil), could be useful for women affected by BV to control its recurrence rates.Citation4,Citation5,Citation12–Citation22
This “symbiotical vaginal approach” seems to be useful especially if administered for a long time course (almost 6 months) to restore vaginal microflora and to prevent BV recurrences, mutually supporting the use of standard of care treatment for BV.Citation4,Citation5,Citation12–Citation22
This probably means that the use of a specific Lactobacillus sp. together with the right prebiotic could add complementary effectiveness vs the single treatment with vaginal probiotics or prebiotics resulting in an interesting option to prevent vaginal dysbiosis/pathobiosis.Citation4
Recently we have demonstrated that a vaginal eubiosis “rechallenge”, from “dysbiosis” and “pathobiosis”, by a vaginal application of the biotherapeutic agent (Lactobacillus rhamnosus BMX 54 + lactose), has been able to restore not only the health of the vaginal ecosystem but also has been demonstrated effective against the HPV (human papillomavirus) vaginal-related pathologies and infections, clearly indicating that vaginal microbiota influences vaginal microbioma even modifying vaginal healthy cells.Citation19,Citation21,Citation22
A controlled trial performed in 117 women affected by BV/vaginitis and associated HPV infection showed a significant decrease in HPV-related cytological anomalies (71.9% vs 36.6%: p = 0.04) and in HPV clearance (33.3% vs 13.3%: p = 0.04); the trial was performed by testing a long-term vaginal application (8 months) of metronidazole/fluconazole plus Lactobacillus rhamnosus BMX 54 + lactose vs a short-term vaginal application (2 months) of metronidazole/fluconazole plus Lactobacillus rhamnosus BMX 54 + lactose.Citation19,Citation21
Symbiotic vaginal tablets were administered after metronidazole or fluconazole treatment with an accurate long term schedule (once a day for 10 days followed by 1 tablet every 3 days for a month, 1 tablet every 5 days till the second months and then 1 tablet weekly for 6 months).Citation19,Citation21 These results have been confirmed in an observational clinical trial performed on 2010 women attending the hospital for the screening of sexually transmitted diseases (STDs): of 2010 women analyzed, 1210 were found with “altered vaginal microflora” while 800 were found with “normal vaginal microflora”.Citation22 Of the 1210 women with altered microflora, 645 were detected affected by an STD; all of these 645 patients have been topically treated with Lactobacillus rhamnosus BMX 54 + lactose according to a long-lasting protocol (1 tablet once a day for 15 days, followed by 1 tablet twice a week for 15 days and then 1 tablet once a week for 6 months), the use of a long term course (8 months) vs a short term course (2 months) of the vaginal drug significantly decreased the number of STD infection (p < 0.001) and the recurrence rate of the STDs after 12 months (p < 0.003), demonstrating that reestablishing eubiosis in the vaginal ecosystem could be helpful to reduce bacterial and viral predominance leading to lower susceptibility to infections.Citation22
Vaginal microbioma “continuously” exchanges informations between species and this allows any “living microorganisms“ to follow its natural destiny: a programming and ordinate “cell duplication”.Citation5
The “dynamisms” of the microbiota system give to the cells a continuum in “progression” and “regression” with a clinical result of healthy and pathological status.Citation5
So we can consider that a “pathobiosis pathway” in the human vagina, well marked by a progressive but reversible deviation from a “lactobacillocentric vaginal ecosystem” (eubiosis) to its modification with the predominance of other bacteria like virus or fungi spp., will end with the disappearance of the lactobacilli.Citation5
The message’s coding DNA-mediated, losing the coordination between symbiotic spp. of vaginal microbiome, will lead to clinical different pathologies during the different steps of the “pathobiosis path” up to an uncontrolled cellular replication or an atypical cellular apoptosis.Citation5
The data obtained in more than 800 women treated with Lactobacillus rhamnosus BMX 54 + lactose vaginal tablets using the long-lasting protocol in HPV regressionCitation4,Citation5,Citation18,Citation20,Citation21 have been really surprising, demonstrating that “restoring vaginal eubiosis seems to encourage in this direction”.
Concluding, this symbiotic drug vaginal application could become a new, safe and strategic approach to control HPV-related CIN and cancer.Citation4,Citation5
The eubiosis rechallenge obtained in vaginal microbiota/microbioma by long-lasting use of a well known and well identified vaginal symbiotic (Lactobacillus rhamnosus BMX 54 + lactose) could be useful for women’s health not only in decreasing the recurrence rate of BV but also in controlling the “pathobiosis path” progression, allowing the right message exchanges between the human vaginal cells for a “controlled cellular replacement”.Citation4,Citation5
Disclosure
Filippo Baldacci and Mara Baldacci are employees of Laboratori Baldacci SpA and Marco Bertini is the R&D manager of Laboratori Baldacci SpA. The authors report no other conflicts of interest for this work.
References
- Wiesenfeld HC, Hiller SL, Krohn MA, et al. Lower genital tract infection and endometritis: insight into subclinical pelvic inflammatory disease. Obstet Gynecol. 2002;100:453–456.
- Ness RB, Kip KE, Hiller SL, et al. A cluster analysis of bacterial vaginosis-associated microflora and pelvic inflammatory disease. Am J Epidemiol. 2005;162:585–590. doi:10.1093/aje/kwi243
- Spear GT, Glibert D, Landay AL, et al. Pyrosequencing of the genital microbiotas of HIV-sieronegative women reveals Lactobacillus iners as the predominant Lactobacillus species. Appl Environ Microbiol. 2011;77:378–381. doi:10.1128/AEM.00973-10
- Bertini M. Bacterial vaginosis and sexually transmitted diseases: relationship and management. In: Serdaroglu S, Kutlubay Z, editors. Fundamentals of Sexually Transmitted Infections. INTECH Open; 2017:75.
- Palma E, Bertini M. Vaginal microbiota and the pathobiosis path: its role in the evolution of the HPV cervical intraephitelial neoplasia and cancer. Eur J Gynaecol Oncol. 2019;40(4):534–537.
- Albert DM, Doderlein G. A critical view to the bibliographies of two German Professor. Zentralbl Gynakol. 2006;128(2):56–59.
- Miller EA, Beasley DE, Dunn RR, Archie EA. Lactobacilli dominance and vaginal pH: why is the human vaginal microbiome unique? Front Microbiol. 2016;7:1936.
- GaGhazzewiFH A, Teser RF. Biotherapeutic agents and vaginal health. J Appl Microbiol. 2016;121(1):18–27. doi:10.1111/jam.13054
- Balkus JE, Jakho W, Temmerman M, et al. The post-trial effect of oral periodic presuntive treatment for vginal infection on the incidence of bacterial vaginosis and Lactobacillus colonization. Sex Transm Infect. 2012;29:361–365.
- Serok AC, Verstraelen H, Temmerman M, Botta GA. Probiotics for the treatment of bacterial vaginosis. Cochrane Database Syst. Rev. 2009;(4):CD006289.
- Lev-Sagie A, Glodman-Wohl D, Cohen Y. Vaginal microbiome transplantation in women with intractable bacterial vaginosis. Nat Med. 2019;25:1500–1504. doi:10.1038/s41591-019-0600-6
- Parma M, Stella Vanni V, Bertini M, Candiani M. Probiotics in the prevention of recurrences of bacterial vaginosis. Altern Ther Health Med. 2014;20:52–57.
- Recine N, Musciola A, Moreira E. The benefits of topical vaginal therapy with Lactobacillus casei sub-rhamnosus in preventing bacterial vaginosis relapses. In: Abstract Book of the X National IBAT Conference Naples; January 26 – 28, 2018.
- Rossi A, Rossi T, Bertini M. The use of Lactobacillus rhamnosus in the therapy of bacterial vaginosis. Evaluation of clinical efficacy in a population of 40 women treated for 24 months. Arch Gynecol Obstet. 2010;281:1065–1069. doi:10.1007/s00404-009-1287-6
- Bertini M. Is Lactobacillus rhamnosus BMX 54 vaginal application a strategy to counteract bacterial vaginosis recurrences?: Proceedings of 18th World Congress on Controversis in Obstetrics, Gynecology and Infertility (COGI), WienOctober 24 – 27, 2013
- Recine N, Palma E, Domenici L, et al. Restoring vaginal microbiota: biological control of bacterial vaginosis. A prospective case-control study using Lactobacillus rhamnosus BMX 54 as adjuvant treatment against bacterial vaginosis. Arch Gynecol Obstet. 2016;23(1):101–107. doi:10.1007/s00404-015-3810-2
- Marcone V, Rocca B, Lichtner M, Calzolari E. Long-term vaginal administration of Lactobacillus rhamnosus as a complementary approach to management of bacterial vaginosis. Int J Obstet Gynecol. 2010;110:223–226. doi:10.1016/j.ijgo.2010.04.025
- Stojanovic N, Plecas D, Plesinac S. Normal vaginal flora disorders and application of probiotics in pregnancy. Arch Gynecol Obstet. 2012;286(2):325–332. doi:10.1007/s00404-012-2293-7
- Recine N, Palma E, Domenici L, Giorgini M, Pierangeli A, Benedetti Panici P Long-term probiotic implementation to re-create a balanced vaginal ecosystem: a promising boost against HPV. In: Abstract Book of International Scientific Conference on Probiotics and Prebiotics; June 21 – 23, 2016; Budapest Hungary.
- Luzi G, Iazzetta E, Cecconi L, et al. Lactobacillus rhamnosus BMX 54 vaginal application usefulness as adjuvant therapy for preterm premature rupture of membranes (PPROM) in the second trimester of pregnancy. Int J Pediatr Neonatal Health. 2018;2(1):14–18.
- Palma E, Recine N, Domenici L, Giorgini M, Pierangeli A, Panici PGB. Long-term Lactobacillus rhamnosus BMX 54 application to restore a balanced vaginal ecosystem: a promising solution against HPV infection. BMC Infect Dis. 2018;18(1):1–7.
- Recine N, Domenici L, Bracchi C, Palma E, Benedetti Panici PG.How vaginal microbiota re-establishment can reduce sexually trasmitted diseases: an observational study on 2010 patients.Abstract Book of 2018 COGI Congress (London) OP 1 204.75
