Abstract
Although much emphasis has been placed on the primary presentations of breast cancer, little focus has been placed on how systemic illnesses may affect the breast. In this article, we discuss systemic illnesses that can manifest in the breast. We summarize the clinical features, imaging, histopathology, and treatment recommendations for endocrine, vascular, systemic inflammatory, infectious, and hematologic diseases, as well as for the extramammary malignancies that can present in the breast. Despite the rarity of these manifestations of systemic disease, knowledge of these conditions is critical to the appropriate evaluation and treatment of patients presenting with breast symptoms.
Introduction
Although breast cancer is the most worrisome problem involving the breast, systemic illnesses can affect the breast and cause concern related to diagnosis and treatment. In this article, we focus on the varying impact of different systemic illnesses on breast tissue.
Women exhibiting breast manifestations of systemic disease may present with a breast lump, skin changes, focal pain, and/or mammographic abnormalities. Evaluation of these symptoms depends on the overall presentation and may include diagnostic mammogram, breast ultrasound, biopsy of suspicious lesions, and, in some cases, magnetic resonance imaging of the breast. After exclusion of a primary breast malignancy or benign primary breast lesion, one must consider evaluation for systemic disease. This article provides an overview of breast manifestations of systemic disease and their evaluation.
Endocrine disease
Diabetic mastopathy
Diabetic mastopathy typically presents as a palpable breast mass that may be nontender, solitary or multiple, and unilateral or bilateral. It is most commonly identified in premenopausal women with long-standing type 1 diabetes mellitus.Citation1–Citation3 Diabetic mastopathy accounts for less than 1% of benign breast disease but can be present in up to 13% of patients with type 1 diabetes.Citation4 There have also been reports of diabetic mastopathy in older women in association with long-standing type 2 diabetes mellitus,Citation5 but this finding was not reproduced in another retrospective cross-sectional study.Citation3 Some cases have been identified in nondiabetic patients as well. Although the etiology of diabetic mastopathy is poorly defined, it remains debatable as to whether it is actually a complication of diabetes mellitus. The lesions may spontaneously regress but the likelihood of recurrence is fairly high.Citation1 There is no associated breast cancer risk.
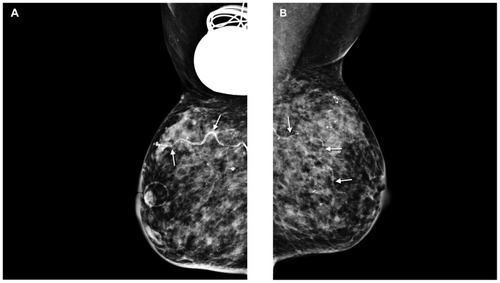
On mammography, diabetic mastopathy is typically seen as a solid mass with asymmetric density, or it may appear as architectural distortion with features highly suggestive of malignancy. On sonograms, the lesions have a concerning appearance, most often irregular hypoechoic masses with worrisome features (). If the patient has a known history of diabetes mellitus, it is possible to make the diagnosis of diabetic mastopathy on core needle biopsy, thus eliminating the need for an excisional biopsy. Magnetic resonance scanning of the breast has no role yet in establishing the diagnosis of diabetic mastopathy.
Figure 1 Diabetic mastopathy: ultrasound of a palpable abnormality shows an ill-defined mass-like area with decreased echogenicity and concerning features.
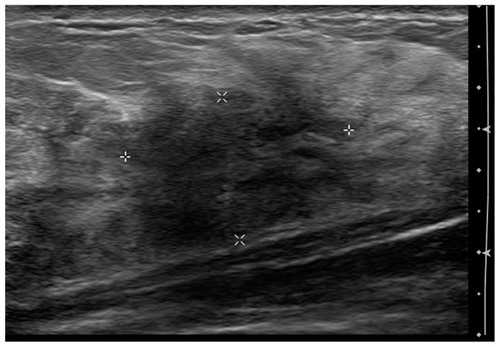
Diabetic mastopathy is a fibroinflammatory proliferation of breast tissue. Microscopic findings of lymphoid infiltrate of the periductal, perilobular, and perivascular structures are variably observed and may be patchy. In addition, dense keloid fibrosis is generally seenCitation6 ().
Figure 2 Breast biopsy showing lymphocytic mastitis consistent with diabetic mastopathy. Hematoxylin-eosin stains: Left, original magnification 400×; right top, original magnification 400×; right bottom, original magnification 400×.
Excision of diabetic mastopathy is rarely necessary. There are no measures known to prevent its development or to lead to its resolution. Routine clinical examination is recommended and, in patients with a documented history of diabetic mastopathy, new occurrences can generally be managed conservatively unless suspicion of malignancy is raised on imaging.Citation7
Vascular disease
Calciphylaxis
The rare, systemic medial calcification of arterioles, leading to ischemia and subcutaneous necrosis, has been labeled “calciphylaxis.” This condition occurs most commonly in patients who have end-stage renal disease and are on hemodialysis or who have undergone renal transplantation recently.Citation8 Only a few cases of calciphylaxis occurring in the breast have been reported in the medical literature,Citation9 with six cases involving the breast after internal mammary artery harvesting. Five of these six patients were on dialysis for end-stage renal disease.Citation10–Citation12 Breast findings included erythematous skin, peau d’orange, and large areas of ischemic necrosis.Citation9
Mammographic findings include multiple and diffuse bilateral calcifications with dystrophic or vascular morphologyCitation13 and trabecular thickening indicative of parenchymal edema. Citation14 Ultrasonographic changes include tissue edema and shadowing foci suggestive of extensive macrocalcification.Citation14 Definitive diagnosis requires a biopsy.
Breast biopsy findings include fat necrosis, fibrosis, calcium deposits in the vessel walls, and calcifications of nonvascular tissue. The differential diagnosis includes breast cancer, especially inflammatory breast cancer. Most cases of calciphylaxis of the breast are treated with partial or total mastectomy. Complete healing of the breast lesion has been reported with total parathyroidectomy.Citation13
Diffuse dermal angiomatosis
Diffuse dermal angiomatosis is a rare, acquired, cutaneous, reactive vascular disorder that was first described in 1994.Citation15 The benign vascular proliferation is characterized by poorly circumscribed, erythematous to violaceous painful lesions with frequent ulceration generally involving the extremities of patients who have severe vascular disease and other comorbid conditions. Diffuse dermal angiomatosis involving the breast is characterized by painful, violaceous, nonhealing, ulcerating macules arising from an erythematous background on both breasts. The vascular-like lesions preferentially involve the underside of the breast.Citation16–Citation19 No specific findings on mammogram or ultrasound have been described in the medical literature. The diagnosis is made by punch biopsy of the skin lesion. The characteristic histologic features of diffuse dermal angiomatosis are the diffuse extravascular, interstitial proliferation of endothelial cells within the dermal stroma. An immunohistochemical stain for CD31 can be obtained for confirmation. Focal areas of proliferating cells may show an epithelioid morphology, vacuolated cytoplasm, and formation of small vascular channels.Citation20 Treatment with isotretinoin, which has an antiangiogenic effect, has been reported to be beneficial in diffuse dermal angiomatosis involving the breast.Citation16
Cardiovascular disease
The prevalence of breast arterial calcification in women presenting for screening mammography has been reported to be about 14%.Citation21 No clinical breast findings have been associated with breast arterial calcification detected by mammography. However, the presence of breast arterial calcification on mammograms indicates a substantially increased risk for development of cardiovascular disease or stroke. When an arterial wall is imaged longitudinally, breast arterial calcification can be detected along the periphery of a tapered structure as two straight parallel calcium deposits (). In contrast, when an arterial wall is imaged en face, breast arterial calcification can have a calcific ring configuration typical of arteries and distinct from breast ducts.Citation21 Mammography is diagnostic for breast arterial calcification, and breast biopsies are not indicated for it. The pathologic findings of arterial calcifications in breast arterial vasculature are similar to those of cardiovascular disease. On mammograms, breast arterial calcification is an incidental finding and no specific treatment is indicated. However, since breast arterial calcification on a mammogram may be considered to be a marker for development of cardiovascular disease, risk stratification and risk factor counseling are advisable.Citation21
Systemic inflammatory disease
Giant cell arteritis
Although giant cell arteritis is a systemic disease, on rare occasions the breast may be the primary organ of manifestation. In a review of the English medical literature up to 2008, Kadotani et alCitation22 identified 20 reported cases, all of which were postmenopausal elderly women. Single or multiple lumps due to arteritis were present in 80% (16 of 20 patients), and redness and tenderness in the absence of lumps were present in 10%. Breast involvement was bilateral in 50% of the patients. Spontaneous breast pain and tenderness were presenting features in 85% of the patients.Citation22 Systemic symptoms such as low-grade fever, arthralgia, myalgia, and those suggestive of polymyalgia rheumatica were present in 65% of the patients.
There have been no reports of mass lesions or other distinctive findings by mammography or ultrasonography. In a recent case reportCitation23 of a patient presenting with a lump in her breast and a negative mammogram, ultrasound of a stringlike thickening in the right axillary tail of the breast revealed a “halo sign” (hypoechoic circumferential wall thickening indicating edema), which, compared with biopsy, has been reported to have a sensitivity of 69% and a specificity of 82% for diagnosis of arteritis.Citation24 In most cases reported in the medical literature, the diagnosis was made after excisional biopsy (a considerable amount of tissue is required to make the diagnosis of giant cell arteritis). In rare cases, the diagnosis was established before biopsy on the basis of systemic symptomsCitation22 and ultrasound findings. Citation23 Pathology shows fragmentation of the elastica in association with giant cell infiltration, intimal proliferation, and narrowing of the vascular lumina. Inflammatory cancer was suspected in four of seven cases reported by Kadotani et al.Citation22
Prednisone is the treatment of choice. It has been shown to improve both general symptoms and breast-specific manifestations of giant cell arteritis.Citation22
Polyarteritis nodosa
Polyarteritis nodosa of the breast is rare, with about a dozen cases reported in the medical literature.Citation25 The clinical presentation ranges from localized disease involving the breast (skin and/or parenchyma) to breast manifestations as part of systemic polyarteritis nodosa. Polyarteritis nodosa can mimic breast cancer in patients presenting with a mass, and it can mimic breast infections such as mastitis or necrotizing fasciitis.
Imaging modalities have not been very helpful in establishing the diagnosis. Mammographic findings have not been reported in all cases, and those that have been reported have been negative except for findings in twoCitation25,Citation26 patients who had calcification of arteries in both breasts as a prominent feature. The diagnosis of polyarteritis nodosa involving the breast is made by evaluating an adequate tissue sample from the breast.
Polyarteritis nodosa is characterized by segmental transmural inflammation of muscular arteries. Polymorphonuclear leukocytes and mononuclear cells are found in the cellular infiltrate. Leukocytoclasis may also be noted. Arterial wall necrosis results in fibrinoid necrosis, which has a homogeneous, eosinophilic appearance. Disruptions of the internal and external elastic lamina may contribute to the development of aneurysmal dilatation. Lesions that appear to be of different ages are typically found within a single sample.Citation27 Polyarteritis nodosa mimics breast cancer, inflammatory carcinomatosis, or breast infections, such as mastitis and necrotizing fasciitis.
Treatment of polyarteritis nodosa is guided by how the patient with disease presents. Débridement of localized necrotic skin and necrotic mammary tissue may be necessary to manage the defect. If a tissue biopsy confirms the diagnosis of polyarteritis nodosa, then immunosuppressive treatment can commence.Citation25
Wegener’s granulomatosis
Breast involvement is rare in patients with the uncommon disease of Wegener’s granulomatosis. Approximately 28 cases of breast involvement have been reported as occurring in women between the third and seventh decades of life.Citation28 Breast involvement may occur as the presenting symptom of Wegener’s granulomatosis or as a synchronous or metachronous lesion in patients with systemic disease. Presenting symptoms include unilateral or bilateral breast masses, breast abscesses, necrotic lesions, and ulcerations.Citation28,Citation29
Mammographic findings have been reported as ill-defined or irregular masses suspicious for carcinoma.Citation30 Ultrasonographic findings include irregular hypoechoic masses.Citation30 The diagnosis is made by breast biopsy, but it can be difficult to establish if there are only small fragments of core needle biopsy material available versus an adequate tissue specimen.
Wegener’s granulomatosis is characterized by vasculitis of the medium-sized vessels that affects capillaries, venules, arterioles, and arteries. Necrotizing granulomatous inflammation with central necrosis is the hallmark of the disease.Citation28 Associated with the granulomatous inflammation are multinucleated giant cells, plasma cells, lymphocytes, and neutrophils. Wegener’s granulomatosis may mimic breast cancer or granulomatous mastitis.
The initial treatment of most patients described in the medical literature has been corticosteroids and cyclophosphamide. In several cases, patients underwent excision of the breast lesion or a mastectomy. In almost all cases, symptoms improved substantially after immunosuppressive therapy.Citation28
Sarcoidosis
Sarcoidosis is characterized as a systemic granulomatous disorder with no known etiology that can involve any organ system but frequently affects the lungs, hilar lymph nodes, eyes, skin, and joints. Breast involvement is rare, occurring in less than 1% of cases.Citation31 Breast involvement can be either the sole manifestation, which is termed “primary mammary sarcoidosis,” or it can be part of a more obvious systemic disease. Patients may present either with a mass or without symptoms but with a mass detected on a mammogram.Citation32
The mammographic abnormality is typically a mass, asymmetry, or an area of architectural distortion.Citation33,Citation34 Mammographic and ultrasonographic features are usually worrisome for malignancy. Biopsy, either surgical or image-guided core needle, is required for diagnosis. Pathologic findings are noncaseating granulomas. Giant cells may or may not be seen. The differential diagnosis includes idiopathic granulomatous mastitis, tuberculosis, fungal infection, cat-scratch disease, and other autoimmune disorders with granulomatous inflammation.Citation32
The usual first-line therapy is systemic corticosteroids. For patients with disease solely in the breast who do not respond to corticosteriods, there may be a role for surgical excision although this has not been established as a first- line therapy.Citation31
Lupus mastitis
Lupus mastitis occurs in approximately 2% of patients with systemic lupus erythematosus.Citation35 Up to 70% of patients have associated discoid skin lesions. Lupus mastitis is rarely the presenting symptom. Fewer than 25 cases have been described in the medical literature, with four cases reported in men. Breast findings on clinical examination include single or multiple subcutaneous nodules, which may be tender or painful and can progress to ulcerated lesions.Citation35
The lesions are ill-defined on mammograms and sonograms and may or may not be associated with calcifications. Alternatively, calcifications may be present alone, which is suggestive of fat necrosis.Citation35 Image-guided or excisional biopsy is needed to differentiate this lesion from breast cancer.
Pathologically, immune complex depositions are noted at the basement membrane of the dermal-epidermal junction and in the blood vessels in the area of the panniculitis.Citation35 Key histopathologic findings are lobular lymphocytic panniculitis and hyaline fat necrosis.Citation36 Lymphocytic vasculitis is also a common feature.
If insufficient biopsy tissue is present, the lesion may be mistaken for primary medullary carcinoma of the breast, especially if the tissue contains predominantly lymphoplasmacytic inflammatory component. Diabetic mastopathy may also be in the differential diagnosis.Citation35
Initial treatment typically consists of antimalarial agents or corticosteroids. Surgery can be considered in cases that do not respond to medical treatment.Citation36
Infectious disease
Breast involvement in systemic infections is a rare condition but has been reported with tuberculosis, echinococcosis and other parasitic diseases, and actinomycosis. Breast tuberculosis may become a relevant problem with the increasing occurrence of tuberculosis related to acquired immune deficiency syndrome and tuberculosis as a global health concern.
Tuberculosis of the breast is a rare condition generally secondary to systemic infection, with breast tissue infection resulting from hematogenous lymphatic spread or from spread from a contiguous infection such as one in the chest wall.Citation37,Citation38 Clinical presentation is generally a breast lump that is firm to hard in consistency and can be mistaken for malignancy, but it can also present as an ulcer or a discharging sinus on the skin overlying the breast, as a nipple discharge, or as peau d’orange if it is associated with extensive axillary disease.
Mammography is often inconclusive because the lesion may be seen as a round mass with ill-defined margins. On ultrasound, lesions are often hypoechoic or present as complex cysts. Ultrasound-guided cyst aspiration with cytology of the fluid may show epitheloid cell granulomas and necrosis but is often inconclusive. Histopathologic findings of biopsy specimens of the mass demonstrate necrotizing granulomas.
Treatment of tuberculosis infection of the breast is with multidrug antitubercular therapy. Surgical intervention is needed only for drainage of a breast abscess or for incisional or excisional biopsy of the mass. In some instances, a residual breast mass after antitubercular therapy may require surgical excision.Citation37
Hematologic disease
Malignant lymphoma
Lymphoma of the breast can present as primary lymphoma, implying that there is no extramammary organ involvement, and as secondary lymphoma with known extramammary disease. Both conditions are rare, with primary breast lymphoma comprising about 0.1%–0.5% of all breast neoplasms and secondary breast lymphoma being slightly more common.Citation39 Primary lymphoma can present as diffuse infiltration or as discrete and sometimes multiple nodules. Wong et alCitation39 reviewed the Mayo Clinic experience with primary non-Hodgkin’s lymphoma of the breast over 25 years (1973–1998) and identified 26 patients, 25 of whom were women with a median age of 60 (range 12–80) years at diagnosis. Twenty-four of the 26 patients presented with a breast lump. The median tumor size was 3.3 (range 1–10) cm. In contrast with tumors in primary breast lymphoma, breast masses in secondary breast lymphoma have been reported to be smaller, perhaps because of the shorter duration of the disease within the breast.Citation40
Sabate et alCitation40 noted significant differences between breast lymphoma and carcinoma on mammograms. The mean size of the tumor was larger in patients in the lymphoma group (4.6 cm versus 2–3 cm in patients in the carcinoma group). Architectural distortion was not noted in the lymphoma masses but was evident in the carcinoma group. Calcifications were not observed in any patients in the lymphoma group but were evident in 50% of those in the carcinoma group. Although a core biopsy may be adequate for diagnosis of a breast lymphoma, an excisional biopsy may be necessary to obtain adequate tissue for lymphoma subtyping.
Most primary breast lymphomas are non-Hodgkin’s lymphoma. Although all histologic types of lymphoma have been described, primary breast lymphomas are most commonly B-cell lymphomas; about one-half are diffuse large B-cell lymphomas. Less common are breast lymphomas with an indolent histology (ie, follicular non-Hodgkin’s lymphoma or extranodal marginal zone lymphoma).
Treatment consists of local excision of the breast lymphoma, radiotherapy, and chemotherapy. The choice of chemotherapy is based on the histologic subtype. Mastectomy does not appear to improve survival.Citation41
Plasmacytoma
Plasmacytoma may present as a palpable breast mass or, more unusually, as an incidental finding on mammography. It may occur as the initial presentation or in the setting of known multiple myeloma.Citation42,Citation43 In contrast with solitary plasmacytoma of the bone, extramedullary plasmacytoma is associated with symptomatic multiple myeloma in only 15% of patients.Citation44
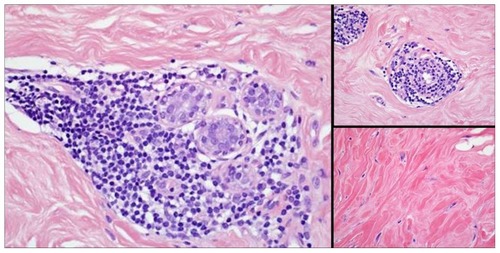
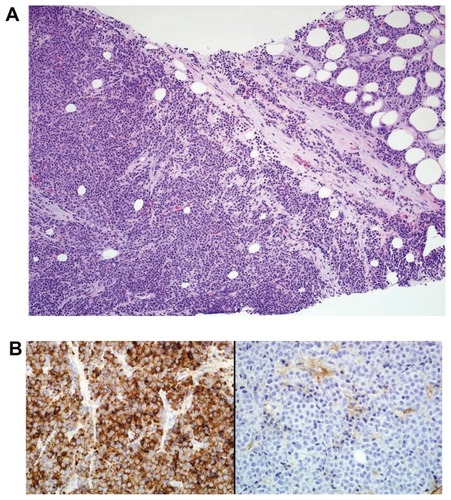
Mammographic findings include rounded, oval, and lobulated masses, which can be solitary or multiple or both (). Occasionally, they present as diffuse infiltration of the breast. Ultrasound typically shows a hypoechoic mass that can be either well defined or ill defined ().Citation42 Core biopsy is needed to differentiate plasmacytoma from primary breast cancer. Immunohistochemical staining reveals clonal plasma cells () positive for κ or λ light chainsCitation44 ().
Figure 4 Plasmacytoma of the breast. Left mammogram shows (A) a small well defined mass (circle) in the left craniocaudal view and (B) an abnormal lymph node (arrows) in the mediolateral oblique view. (C) Ultrasound shows a hypoechoic mass (arrows) with hyperechoic rim.
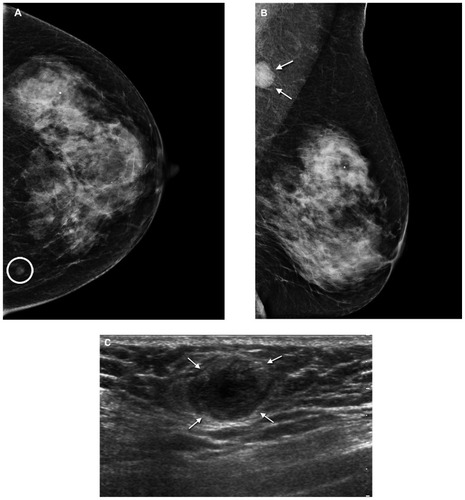
Figure 5 Breast biopsy. (A) Breast biopsy shows plasma cell neoplasm (hematoxylineosin stain, original magnification 200×). (B) Left, κ immunoglobulin antibody light chain stain is positive (original magnification 400×) and, right, λ immunoglobulin antibody light chain stain is negative (original magnification 400×).
Treatment consists of radiotherapy to the extramedullary plasmacytoma,Citation44 unless there is significant systemic multiple myeloma, in which case treatment is for the systemic disease.
Amyloid
Amyloid of the breast is either localized or more commonly associated with systemic amyloidosis. As part of the systemic form, breast amyloid usually occurs as a late presentation of known amyloidosis in other visceral organs. In a case series from Boston Medical Center, Charlot et alCitation45 found that localized amyloidosis of the breast represented only 0.5% of all the patients referred to the amyloid treatment center. Patients may present with either a breast massCitation40,Citation46,Citation47 or no breast findings on clinical examination.Citation48
Mammographic findings include incidental masses, clustered microcalcifications, and focal asymmetry.Citation49 Core needle biopsy or excisional biopsy aids diagnosis. Macroscopic examination of biopsy specimens shows well-circumscribed solid gray tumors, whereas microscopic examination shows abundant hyaline pink material. Focal microcalcifications may be apparent, and amyloid stains are positive.Citation50
Treatment for primary breast amyloidosis is surgical excision of the affected area. Treatment for secondary amyloidosis is done by treatment of the underlying systemic disease.Citation45
Metastases from other solid organ primaries
Breast cancer is the most common type of primary malignancy in women, but metastatic spread to the breast from other solid organs, although rare, has been reportedCitation51–Citation53 and may be the first sign of malignancy.Citation54 On the basis of histologic diagnosis in clinical studies, the frequency of metastatic tumors in the breast from extramammary malignancies has been estimated to range from 0.2% to 1.3%.Citation55 In a review from the Royal London Hospital of secondary neoplasms from other solid organs that metastasized to the breast, Georgiannos et alCitation56 reported that, over 90 years, metastases to the breast were found to emanate from primary lung cancer, melanoma, or gastric, renal, endometrial, pancreatic, esophageal, and thyroid cancers (in descending order of frequency).
Williams et alCitation57 found in a series of patients that a single mass was identified on mammography in 39.5% of patients and that multiple masses were identified in 33.7% of patients. However, of those patients who underwent breast imaging, 16.3% had mammograms with no abnormal findings. The recommended diagnostic approach to metastases from other solid organ primaries is core biopsy for tissue diagnosis.
Immunohistochemistry is considered beneficial in distinguishing between primary breast cancers and metastases from other organs.Citation57 In addition to findings of standard and specialized stains, estrogen-, progesterone-, and HER-2 receptor–negative findings can help to differentiate metastatic tumors from primary breast cancers.
Treatment is focused on management of the primary cancer rather than on the metastatic lesion to the breast. However, Williams et alCitation57 noted that if the metastatic disease burden is low, lumpectomy might be considered.
Conclusion
In summary, this review reports on breast lesions associated with systemic disorders and details the clinical presentation, imaging findings, pathologic findings, and treatment. Although such presentations are rare, an awareness of these associations and knowledge about the diagnosis and treatment of patients with such breast lesions is critical to determining appropriate evaluation and treatment. However, breast cancer always needs to be strongly considered in the differential diagnosis of breast abnormalities in such patients.
Acknowledgments
We would like to acknowledge the Division of General Internal Medicine, Mayo Clinic, for their support. We would also like to acknowledge Carol Reynolds, MD, Division of Anatomic Pathology, Mayo Clinic, for her kind assistance.
Disclosure
The authors have no conflicts of interest to disclose.
References
- ElyKATseGSimpsonJFClarfeldRPageDLDiabetic mastopathy: a clinicopathologic reviewAm J Clin Pathol2000113454154510761456
- GouveriEPapanasNMaltezosEThe female breast and diabetesBreast201120320521121414785
- KudvaYCReynoldsCO’BrienTPowellCObergALCrottyTBDiabetic mastopathy, or sclerosing lymphocytic lobulitis, is strongly associated with type 1 diabetesDiabetes Care200225112112611772912
- HunfeldKPBasslerRLymphocytic mastitis and fibrosis of the breast in long-standing insulin-dependent diabetics: a histopathologic study on diabetic mastopathy and report of ten casesGen Diagn Pathol1997143149589269908
- SotomeKOhnishiTMiyoshiRAn uncommon case of diabetic mastopathy in type II non-insulin dependent diabetes mellitusBreast Cancer200613220520916755119
- SeidmanJDSchnaperLAPhillipsLEMastopathy in insulin-requiring diabetes mellitusHum Pathol19942588198248056424
- ThorncroftKForsythLDesmondSAudisioRAThe diagnosis and management of diabetic mastopathyBreast J200713660761317983405
- JaniganDTHirschDJKlassenGAMacDonaldASCalcified subcutaneous arterioles with infarcts of the subcutis and skin (“calciphylaxis”) in chronic renal failureAm J Kidney Dis200035458859710739777
- BenesKOlubowaleOStephensonTFernandoMNon healing ulcer of the breast due to calciphylaxisBreast J200915554154219671115
- MorrisDJFischerAHAbboudJBreast infarction after internal mammary artery harvest in a patient with calciphylaxisAnn Thorac Surg1997645146914719386727
- RashidAHaj BasheerMKhanKBreast necrosis following harvest of internal mammary arteryBr J Plast Surg200457436636815145743
- WongMSKimJYeungCWilliamsSHBreast necrosis following left internal mammary artery harvest: a case series and a comprehensive review of the literatureAnn Plast Surg200861436837418812704
- CampaninoPPTotaDBagneraSBreast calciphylaxis following coronary artery bypass grafting completely resolved with total parathyroidectomyBreast J201016554454720722652
- BukhmanRScheriRPSelimMABakerJASonography in the identification of calciphylaxis of the breastJ Ultrasound Med201029112913320040786
- KrellJMSanchezRLSolomonARDiffuse dermal angiomatosis: a variant of reactive cutaneous angioendotheliomatosisJ Cutan Pathol19942143633707798394
- McLaughlinERMorrisRWeissSWArbiserJLDiffuse dermal angiomatosis of the breast: response to isotretinoinJ Am Acad Dermatol200145346246511511849
- YangHAhmedIMathewVSchroeterALDiffuse dermal angiomatosis of the breastArch Dermatol2006142334334716549710
- VillaMTWhiteLEPetronic-RosicVSongDHThe treatment of diffuse dermal angiomatosis of the breast with reduction mammaplastyArch Dermatol2008144569369418490610
- Wahner-RoedlerDLSwansonEAMortonMJReynoldsCDiffuse dermal angiomatosis of the breast [Abstract]33rd Annual Symposium of the American Society of Breast Disease Book of AbstractsApril 2–4, 200911
- DraperBKBoydASDiffuse dermal angiomatosisJ Cutan Pathol200633964664816965341
- RotterMASchnatzPFCurrierAAJrO’SullivanDMBreast arterial calcifications (BACs) found on screening mammography and their association with cardiovascular diseaseMenopause200815227628117917612
- KadotaniYEnokiYItoiNKojimaFKatoGLeeCJGiant cell arteritis of the breast: a case report with a review of literaturesBreast Cancer201017322523219459029
- HinzeSHartYMAdamsRFLumpy breasts and headache: a crucial ultrasoundBr J Radiol201184100038638721415304
- BlockmansDBleyTSchmidtWImaging for large-vessel vasculitisCurr Opin Rheumatol2009211192819077714
- KhalilHHMarsdenJAkbarNGordonPRobertsJSchulteKMPolyarteritis nodosa of the breast: presentation and managementInt J Surg20097544645019540945
- YamashinaMWilsonTKA mammographic finding in focal polyarteritis nodosaBr J Radiol19855868591922866009
- NgWFChowLTLamPWLocalized polyarteritis nodosa of breast: report of two cases and a review of the literatureHistopathology19932365355397906244
- AllendeDSBoothCNWegener’s granulomatosis of the breast: a rare entity with daily clinical relevanceAnn Diagn Pathol200913535135719751914
- ComasAGDianaCACrespoCCCebolladaMMLinanMAVilaJVWegener’s granulomatosis presented as recurrent breast abscessBreast J2010161828419968659
- Neralic-MenigaIIvanovi-HercegZMazuranicIWegener’s granulomatosis of the breastWien Klin Wochenschr20061183–412012316703257
- PanzacchiRGalloCFoisFPrimary sarcoidosis of the breast: case description and review of the literaturePathologica2010102310410721171514
- TakahashiRShibuyaYShijuboNAsaishiKAbeSMammary involvement in a patient with sarcoidosisIntern Med200140876977111518121
- GisvoldJJCrottyTBJohnsonRESarcoidosis presenting as spiculated breast massesMayo Clin Proc200075329329510725958
- HermannGNagiCMesterJTiersteinAUnusual presentation of sarcoidosis of the breastBr J Radiol200881969e231e23318769011
- KinonenCGattusoPReddyVBLupus mastitis: an uncommon complication of systemic or discoid lupusAm J Surg Pathol201034690190620410809
- SummersTAJrLehmanMBBarnerRRoyerMCLupus mastitis: a clinicopathologic review and addition of a caseAdv Anat Pathol2009161566119098467
- TewariMShuklaHSBreast tuberculosis: diagnosis, clinical features and managementIndian J Med Res2005122210311016177466
- LinTLChiSYLiuJWChouFFTuberculosis of the breast: 10 years’ experience in one institutionInt J Tuberc Lung Dis201014675876320487616
- WongWWSchildSEHalyardMYSchombergPJPrimary non-Hodgkin lymphoma of the breast: the Mayo Clinic experienceJ Surg Oncol2002801192511967901
- SabateJMGomezATorrubiaSLymphoma of the breast: clinical and radiologic features with pathologic correlation in 28 patientsBreast J20028529430412199758
- JenningsWCBakerRSMurraySSPrimary breast lymphoma: the role of mastectomy and the importance of lymph node statusAnn Surg2007245578478917457172
- BremRFRevelonGWilleySCGatewoodOMZeigerMABilateral plasmacytoma of the breast: a case reportBreast J20028639339512390367
- SurovAFiedlerEHolzhausenHJRuschkeKSchmollHJSpielmannRPMetastases to the breast from non-mammary malignancies: primary tumors, prevalence, clinical signs, and radiological featuresAcad Radiol201118556557421393030
- International Myeloma Working GroupCriteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working GroupBr J Haematol2003121574975712780789
- CharlotMSeldinDCO’HaraCSkinnerMSanchorawalaVLocalized amyloidosis of the breast: a case seriesAmyloid2011182727521501022
- DeolekarMVLarsenJMorrisJAPrimary amyloid tumour of the breast: a case reportJ Clin Pathol200255863463512147664
- SahooSReevesWDeMayRMAmyloid tumor: a clinical and cytomorphologic studyDiagn Cytopathol200328632532812768639
- TooheyJMIsmailKLonerganDLewisCRAmyloidosis of the breast mimicking recurrence in a previously treated early breast cancerAustralas Radiol200751659459617958699
- CaoMMHoytACBassettLWMammographic signs of systemic diseaseRadiographics20113141085110021768240
- WilkinsonIThomasJBreast diseases associated with systemic medical disordersDiagn Histopathol2009158402408
- AkcayMNMetastatic disease in the breastBreast200211652652814965721
- LeeSKKimWWKimSHCharacteristics of metastasis in the breast from extramammary malignanciesJ Surg Oncol2010101213714020082359
- YoungJLJrWardKCWingoPAHoweHLThe incidence of malignant non-carcinomas of the female breastCancer Causes Control200415331331915090726
- HambyLSMcGrathPCCibullMLSchwartzRWGastric carcinoma metastatic to the breastJ Surg Oncol19914821171211656147
- LeeAHThe histological diagnosis of metastases to the breast from extramammary malignanciesJ Clin Pathol200760121333134118042689
- GeorgiannosSNChinJGoodeAWSheaffMSecondary neoplasms of the breast: a survey of the 20th centuryCancer20019292259226611745279
- WilliamsSAEhlersRA2ndHuntKKMetastases to the breast from nonbreast solid neoplasms: presentation and determinants of survivalCancer2007110473173717582626