Abstract
Background and purpose
Osteoporosis is common in the Saudi Arabian population, and its successful treatment requires full compliance. Patients who require antiresorptive therapy, such as oral bisphosphonates, may suffer from other diseases requiring medications, which increases the medication burden and ends up in drug noncompliance on the part of patients, making them vulnerable to osteoporosis-related fractures. We decided to undertake this study to analyze the concomitant medications that osteoporotic patients are receiving at King Fahd Hospital of the University, Al Khobar.
Methods
Osteoporotic patients receiving antiresorptive therapy (ART) at King Fahd Hospital of the University, Al Khobar, were identified through the database of the QuadraMed Patient Care system and cross-checked with the radiology database of the dual-energy X-ray absorptiometry scan and pharmacy drug-dispensing system between January 2009 and December 2009. Concomitant medication is defined as the use of other drugs for ≥30 days with oral bisphosphonates, calcium, and vitamin D. Medication burdens are defined as mild (≤1 concomitant medication), moderate (≥2 and ≤4 medications), and severe (≥5 medications). The demographic data, such as age, sex, and diagnosis, were collected from the medical records. The data were analyzed using the Statistical Package for the Social Sciences (SPSS).
Results
During the study period, 516 patients were diagnosed with osteoporosis, and 473 were on ART while the rest were using anabolic Teriperatide. Sixty-eight (14.4%) of the patients, with an average age of 50.15 ± 2.4 years, were on one medication besides ART, vitamin D, and elemental calcium; 129 (27.3%) of the patients, with an average age of 51.6 ± 9.7 years, were taking 3.32 medications, and 276 (58.3%) of the patients, with a mean age of 62.1 ± 10.7 years, were on 8.02 concomitant medications. The most common concomitant medications in use were cardiac, endocrine, systemic nonsteroidal anti-inflammatory drugs, and analgesics, in that order. This study suggests that the majority of Saudi women who are osteoporotic and undergoing oral bisphosphonate therapy have a concomitant medication burden of ≥5 other medications. For full compliance with the therapy, the patients’ medication burden should be considered prior to selecting the treatment route.
Introduction
Osteoporosis is a progressive disease that weakens the bones and makes them highly susceptible to fracture. Drug therapy can slow or reverse the condition, but the duration of the therapy is long and has side effects. At present, bisphosphonates are the most commonly used drug.Citation1–Citation5 Adherence and compliance with osteoporosis medication has been poor, due to the dosing requirement and the adverse effects of the drugs.Citation6 It was reported that 40%–45% of patients become noncompliant within the first six months of treatment with antiresorptives.Citation7–Citation10 Noncompliance with osteoporotic medication appears to be universal, and recent data published in Saudi ArabiaCitation11 indicates that after 18 months of dispensing osteoporotic medications, not only was there no improvement in bone mineral density, but 10.4% of patients undergoing the therapy sustained fragility fractures within 16 months.
The strict, daily dosing instructions for oral bisphosphonates is believed to be the main reason for noncompliance, and this has led pharmaceutical companies to develop once-weekly and monthly dosages.Citation12 Unfortunately, even after the introduction of weekly oral bisphosphonates, compliance has only increased marginally, to 65%,Citation13,Citation14 which has caused physicians to seek out other possible causes of noncompliance. One such previously overlooked cause that was identified was that the medication burden (MB) in patients receiving bisphosphonate therapy made them noncompliant.Citation15,Citation16 Kaufman et alCitation17 estimated that 12% of elderly US patients took ≥ 12 medications, and 23% took at least five prescription medications, causing them either to have to change their regimens in order to accommodate oral bisphosphonates or to become noncompliant.
Although osteoporosis and postmenopausal osteoporosis in Saudi Arabian females and males is reported to be approximately 30%–35%, the pattern of antiresorptive therapy and compliance is yet to be investigated. Moreover, the effect of MB on patients receiving therapy has not yet been studied in Saudi society. This study was undertaken in order to identify the number of concurrent medications that patients must take alongside oral bisphosphonates.
Methods
Osteoporotic patients receiving therapy at King Fahd Hospital of the University, Al Khobar, will be identified through the QuadMed Patient Care system’s database and will be cross-checked with the Radiology database of the dual-energy X-ray absorptiometry scan and pharmacy drug-dispensing system between January 2009 and December 2009. Information about osteoporosis drug therapy (oral bisphosphonates, vitamin D, and calcium) and concomitant medications dispensed by the pharmacy were collected and entered into the database. Concomitant medication is defined as the use of other drugs for ≥30 days with oral bisphosphonates, calcium, and vitamin D. The MB is categorized into a mild burden (≤1 concomitant medication), a moderate burden (≥2 and ≤4 medications), and a severe burden (≥5 medications). The demographic data, such as age, sex, and diagnosis, were determined from the patients’ medical records and were entered into the database. The data were analyzed using the Statistical Package for the Social Sciences (version 14.0; SPSS Inc, Chicago, IL).
Results
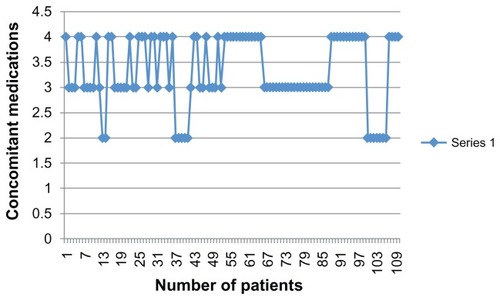
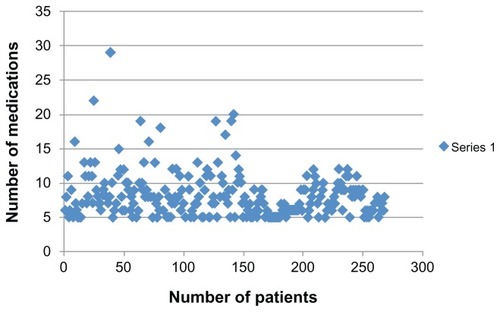
During the study period, 473 patients were on antiresorptive therapy (ART) and 43 patients were on injectable bone-forming agents. The average age was 57.63 ± 11 years (range: 35–95 years) with a mean concomitant MB of 4.11. All patients were receiving monthly bisphosphonate with daily vitamin D and elemental calcium. Sixty-eight (14.4%) of the patients, with an average age of 50.15 ± 2.4 years, were on one medication apart from the antiosteoporotic therapy. One hundred twenty-nine (27.3%) of the patients, with an average age of 51.6 ± 9.7, years, were taking 3.32 medications (). shows that the majority of the patients in this group were receiving between three and four concomitant medications. Two hundred seventy-six (58.3%) of the patients, with a mean age of 62.1 ± 10.7 years, were on 8.03 concomitant medications (range: 5–29 medications) (). In the group receiving ≥ 5 medications, the majority of patients were taking between 5 and 15 concomitant medications. The most common concomitant medications in use were cardiac, endocrine, systemic anti-inflammatory drugs, and analgesics, in that order ().
Table 1 The different types of concomitant medications
Discussion
Osteoporosis is a major public health issue the world over, and it results in increased morbidity and mortality due to osteoporosis-related fractures.Citation18,Citation19 Effective treatment options for reducing fracture risk are available, provided that patients adhere to the osteoporotic therapy. High medication adherence has been found to reduce the risk of all clinical fractures by 20%–45%,Citation20,Citation21 but nonadherence to the therapy has been a universal problem. Kothawala et alCitation22 in a meta-analysis of 24 observational studies, found that overall adherence to osteoporosis therapies was 40%–60%.
The causes of noncompliance with bisphosphonate therapy are multifactorial. The reasons strongly associated with noncompliance include the cost of drugs, the side effects of medication, the patients’ perceptions of the effectiveness of therapy,Citation23 the MB of patients taking osteoporotic medications,Citation15,Citation16 and the dosing regimens. In Saudi Arabia, the medications are distributed free of charge to all patients; hence, the cost of medications is not part of the equation, in terms of noncompliance. Therefore, there could be other causes of noncompliance, and our concern with MB as a cause of noncompliance with oral ART remains valid because it has not been studied enough among Saudi Arabian patients. We believe the issue of MB in Saudi patients appears to be an important one that needs to be addressed.
In adults in Great Britain, the >75-year age group takes a mean daily drug dosage of 2.5,Citation24 whereas Italians consume a mean dosage of 3.5 drugs dailyCitation25 and Danes a mean dosage of four drugs daily.Citation26 In our study, Saudi ≥ 65-year-old women with osteoporosis were taking additional daily medications at a mean of 7.78, which in comparison to the reported literature, is high. Polypharmacy is defined as the use of five or more drugs, and the prevalence of polypharmacy in the United Kingdom was found to be 15% in patients over 75 years old, whereas in the Saudi population, it was >50%.Citation24
It takes two years or even more to assess objectively significant increases in bone density after instituting ART. Patients consuming five or more drugs are less likely to adhere to the drug regimen unless certain strategies are used. One such strategy is supervised injectable antiresorptive therapy, available in the form of subcutaneous injections every six months and annual intravenous injections. Both Denasumab and Zoledronic acid have proven potency with a wide safety profile, and are in clinical use worldwide. These drugs have been found to have the highest probabilities of being most efficacious in the prevention of nonvertebral and vertebral fractures.Citation27 This will provide the clinician with a 100% guarantee of compliance and efficacy.
Limitations of the current study include the fact that the database was taken from the King Fahd Hospital of the University pharmacy to estimate the actual medications used by patients. It is assumed that the patients are taking the medications as prescribed to them and are following instructions. Furthermore, it is possible that patients are taking drugs from other institutions and retail pharmacies. Because King Fahd Hospital of the University is a tertiary care center, patients seen there will be similar to patients attending other centers. This study’s strongest point is that it has raised the MB issue as it relates to the Saudi population; MB could be one of the most important factors in noncompliance with ART. We conclude that MB could be one of the most important factors of noncompliance, and should not be ignored. Physicians should be involved in tailoring osteoporotic therapy to ensure adherence to it. Considering the various findings of the present study, the authors believe that further prospective studies on the subject should be undertaken to assess MB among elderly populations and its impact on compliance.
Clearly, the issue of MB in patients taking oral ART is a valid one, and could be an important factor in noncompliance among Saudi Arabian patients. Physicians should play a major role in tailoring interventions for the individual patient, which should be aimed at promoting patient compliance. New treatment options, with semiannual and annual dosages, will change the future management of osteoporotic patients, provided these drugs remain safe, with fewer side effects in long-term use.
Disclosure
The authors report no conflicts of interest in this work.
References
- RizzoliRLong-term outcome of weekly bisphosphonatesClin Orthop Relat Res2006443616516462427
- TostesonANMeltonLJIIIDawson-HughesBCost-effective osteoporosis treatment thresholds: the United States perspective [for the National Osteoporosis Foundation Guide Committee]Osteoporosis Int200819437447
- WeissTWHendersonSCMcHorneyCACramerJAPersistence across weekly and monthly bisphosphonates: analysis of US retail pharmacy prescription refillsCurr Med Res Opin20072392193220317686228
- Van den BoogaardCHBreekveldt-PostmaNSBorggreveSEGoettschWGHeringsRMPersistent bisphosphonate use and the risk of osteoporotic fractures in clinical practice: a database analysis studyCurr Med Res Opin20062291757176416968579
- BorgstromFCarlssonASintonenHThe cost-effectiveness of risedronate in the treatment of osteoporosis: an international perspectiveOsteoporos Int200617996100716570118
- PapaionnouAKennedyCCDolovichLLauEAdachiJDPatient adherence to osteoporosis medications: problems, consequences and management strategiesDrugs Aging2007241375517233546
- SolomonDHAvornJKatzJNCompliance with osteoporosis medicationsArch Intern Med20051652414241916287772
- HamiltonBMcCoyKTaggartHTolerability and compliance with residronate in clinical practiceOsteoporos Int200314259126212730745
- TostesonANGroveMRHammondCSEarly discontinuation of treatment for osteoporosisAm J Med200311520921612947959
- CramerJASilvermanSPersistence with bisphosphonate treatment for osteoporosisAm J Med20061194 Suppl 1S12S1716563936
- Sadat-AliMAl-DakheelDAl-TurkiHAAl-ElqACan drug therapy alone increase bone mineral density and reduce the incidence of osteoporosis-related fractures?Ind Pract2009628507510
- MillerPDOptimizing the management of postmenopausal osteoporosis with bisphosphonates: the emerging role of intermittent therapyClin Ther20052736137615922811
- ReckerRRGallagherRMacCosbePEEffect of dosing frequency on bisphosphonate medication adherence in a large longitudinal cohort of womenMayo Clin Proc20058085686116007889
- CramerJAAmonkarMMHebbornAAltmanRCompliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosisCurr Med Res Opin2006211453146016197664
- GurwitzJHPolypharmacy: a new paradigm for quality drug therapy in the elderlyArch Intern Med20041641957195915477428
- RollasonVVogtNReduction of the polypharmcy in the elderly: a systematic review of the role of the pharmacistDrugs Aging20032081783212964888
- KaufmanDWKellyJPRosenbergLRecent pattern of medication use in the ambulatory adult population of the United States: the Slone surveyJAMA200228733734411790213
- US Department of Health and Human ServicesBone Health and Osteoporosis: A Report of the Surgeon GeneralRockville, MDUS Department of Health and Human Services, Office of the Surgeon General2004
- BurgeRDawson-HughesBSolomonDHIncidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025J Bone Miner Res20072246547517144789
- SirisESHarrisSTRosenCJAdherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databasesMayo Clin Proc20068181013102216901023
- Penning-van BeestFJErkensJAOlsonMHeringsRMLoss of treatment benefit due to low compliance with bisphosphonate therapyOsteoporos Int200819451151717874028
- KothawalaPBadamgaravERyuSMillerRMHalbertRJSystematic review and meta-analysis of real-world adherence to drug therapy for osteoporosisMayo Clin Proc200782121493150118053457
- McHorneyCASchousboeJTClineRRWeissTWThe impact of osteoporosis medication beliefs and side-effect experiences on nonadherence to oral bisphosphonatesCurr Med Res Opin200723123137315217988435
- ChenYFDeweyMEAveryAJSelf-reported medication use for older people in England and WalesJ Clin Pharm Ther200126129124011350536
- NobiliATettamantiMFratturaLDrug use by the elderly in ItalyAnn Pharmacother1997314164229101001
- BaratIAndreasenFDamsgaardEMThe consumption of drugs by 75-year-old individuals living in their own homesEur J Clin Pharmacol20005650150911049014
- HopkinsRBGoereeRPullenayegumEThe relative efficacy of nine osteoporosis medications for reducing the rate of fractures in post-menopausal womenBMC Musculoskelet Disord20111220921943363