Abstract
Background
Despite the introduction of minimally invasive approaches for various benign uterine problems, hysterectomy is often still performed abdominally, but the vaginal route should be used whenever possible. The aim of this study was to identify the preoperative, intraoperative, and postoperative characteristics of women undergoing vaginal hysterectomy in the absence of uterine prolapse.
Methods
A prospective, descriptive, quantitative, noncomparative study was conducted in 117 women between August 2009 and February 2011 in Petropolis, Rio de Janeiro, Brazil. The women included had a uterine indication for hysterectomy, their surgeries were performed by the same team, and they were followed up for 12 months. An adapted Pelvic Organ Prolapse Quantification system was used to check for uterine prolapse.
Results
The age range of the women was 33–59 years, uterine volume was 300–900 mL, and 73.50% has undergone prior cesarean section. The main indication for hysterectomy was uterine myoma (64.95%), with a surgery time of 30–60 minutes in 55 (59.82%) and 19 (15.98%) cases, respectively. Uterine volume reduction was performed in 41 (35.05%) cases, salpingectomy was the most common associated surgery (81.19%), and anesthesia was subdural (68.37%). Common intraoperative complications included bladder lesions (8.54%), with conversion to the abdominal route being necessary in one case (1.28%), and the most common postoperative complication being vaginal cupola granuloma (32.47%). There was a statistically significant relationship between surgery time and uterine volume (χ2 = 17.367; P = 0.002).
Conclusion
This study suggests that vaginal hysterectomy is a safe surgical procedure in view of its good performance and low complication rate.
Introduction
Vaginal hysterectomy involves removal of the uterus via the vaginal route, with no abdominal incision, and should be performed whenever possible in preference to abdominal hysterectomy.Citation1 However, despite vaginal hysterectomy being recommended, and numerous studies supporting its benefits and safety, many hysterectomies are still performed abdominally,Citation3,Citation4 with several reasons, including lack of pelvic relaxation, a history of prior pelvic surgery, nulliparity, and large uterine size, being used as justification. US data show that the abdominal route is still used in about 66% of cases, while the vaginal route is used in 22% and laparoscopic hysterectomy in about 12% of cases.Citation5
A number of factors that can influence the choice of route of hysterectomy for benign diseases and presented reasons include uterine size and accessibility, uterine and vaginal shape, extrauterine disease, need for concomitant procedures, training and experience of the surgical team, hospital support with adequate material and available emergency sector, and patient preference.Citation6 A narrow pubic arch (<90 degrees), narrow vagina, uterine immobility, nulliparity, prior cesarean section, and a large uterine volume are considered by some authors to be contraindications to vaginal hysterectomy. However, other authors have shown that nulligravida and those with a history of cesarean section can have sufficient vaginal caliber to allow use of the vaginal route for hysterectomy.Citation7
Newer evidence indicates that the vaginal route is indeed safe for hysterectomy, even for larger uterine volumes,Citation8–Citation10 and the literature has demonstrated that, when feasible, vaginal hysterectomy is more cost-effective for uterine removal.Citation1 Even when the uterine volume is large, vaginal hysterectomy can be carried using uterine volume reduction techniques such as myomectomy, uterine morcellation, uterine hemisection, intramyometrial reduction (Lash’s technique), uterine wall wedge resection, and amputation of the uterine cervix, with the aim of obtaining access to the base of the uterus.Citation11 In a 2009 Cochrane review, Niebore et al reviewed 34 studies comparing abdominal, vaginal, and laparoscopic hysterectomy in 4495 patients, and found the best results for the vaginal route.Citation1 Doucette et al supported this finding, stating that it was their experience, ie, when the vagina is ample enough to allow access of uterosacral and cardinal ligaments, uterine mobility increases and allows accomplishment of vaginal hysterectomy even in those cases where uterine descending with initial traction is minimum.Citation12
We have performed vaginal hysterectomies for a long time, and our experience is that the vaginal route is a safe, rapid, and cost-effective way to perform this surgery. The purpose of this study was to evaluate preoperative, intraoperative, and postoperative parameters in women without uterine prolapse undergoing vaginal hysterectomy.
Materials and methods
We carried out this prospective, descriptive, quantitative, noncomparative study in 117 women between August 2009 and February 2011 in Petropolis, Rio de Janeiro, Brazil. All the women had presented with an indication for hysterectomy, including myoma, endometrial hyperplasia, or abnormal uterine bleeding, and none had uterine prolapse. The subjects were assessed for vaginal hysterectomy after signing an informed consent form. All operations were performed by the same surgical team and the patients were followed up for 12 months, with assessments at 1, 2, 3, 6, 9, and 12 months following surgery to check for early or late complications and their evolution.
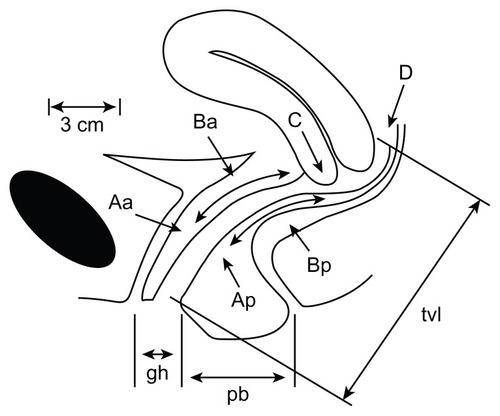
We used the Pelvic Organ Prolapse Quantification system criteria standardized by the International Continence SocietyCitation13 to exclude uterine prolapse. This system uses the hymenal caruncle as the fixed point of reference, with six defined points, ie, Aa, Ba, C, D, Ap, and Bp, and three additional landmarks, ie, the genital hiatus, total vaginal length, and perineal body. Each point is measured in cm above or proximal to the hymen (negative number) or cm below or distal to the hymen (positive number), with the plane of the hymen being defined as zero. The hymen was selected rather the introitus as the reference point because it is more precisely identified.Citation14 There are three reference points anteriorly (Aa, Ba, and C) and three posteriorly (Ap, Bp, and D). Points Aa and Ap are 3 cm proximal to or above the hymenal ring anteriorly and posteriorly, respectively. Points Ba and Bp are defined as the lowest points of the prolapse between Aa anteriorly or Ap posteriorly and the vaginal apex. Anteriorly, the apex is point C (cervix), and posteriorly is point D (pouch of Douglas). After hysterectomy, point C is the vaginal cuff and point D is omitted. Three other measurements are taken, ie, the vaginal length at rest, the genital hiatus from the middle of the urethral meatus to the posterior hymenal ring, and the perineal body from the posterior aspect of the genital hiatus to the mid anal openingCitation15 (see ).
Figure 1 Points and landmarks for Pelvic Organ Prolapse Quantification system examination.
Inclusion criteria were any medical indication for hysterectomy, including myoma, endometrial hyperplasia, uterine polyps, and cervical intraepithelial neoplasia. Exclusion criteria were any grade of uterine prolapse, uterine or cervical cancer, and confirmed or suspected primary adnexal pathology.
Preoperative variables recorded were patient age, surgical indication, uterine volume, parity, route of delivery, and prior (including gynecological) surgery. Intraoperative variables recorded were duration of surgery, type of anesthesia, need for conversion to abdominal surgery, bladder lesions, and hemorrhage. Postoperative variables recorded were duration of hospitalization, hemorrhage, infection at the surgical site, urinary tract infection, and development of vaginal cupola hematoma or granuloma.
Salpingectomy was indicated and performed in all patients, and oophorectomy was performed in those who were postmenopausal. Complementary surgeries, such as posterior culdoplasty and sacrospinal ligamentopexy, were carried out as indicated.
The data were analyzed using SPSS software (SPSS Inc, Chicago, IL), with frequency, median, and standard deviation used for quantitative variables. Chi-square testing was used to identify any statistically significant relationships between surgery time and uterine volume, associated surgery, and previous surgery. Findings were considered to be significant at P = 0.05.
Results
Preoperative characteristics
The mean age was 46 (range 33–59) years. Uterine volume was divided to three bands, ie, ≤300 mL (64.95%), 301–600 mL (21.36%), and 601–900 mL. Parity was similarly classified as one (9.40%), two (52.99%), and three or more fetuses (37.60%). Delivery had been by the vaginal route in 26.49% and by cesarean section in 73.50%. Indications for hysterectomy were uterine myoma (64.95%), abnormal uterine bleeding (23.93%), endometrial hyperplasia (5.98%), pelvic pain (3.41%), and endometrial cancer (1.70%). Associated surgical conditions were ovarian cyst, urinary incontinence, rectocele, cystocele, and hydrosalpinx. Prior related surgeries included fallopian tube ligation (44.44%), oophoroplasty/oophorectomy (5.12%), myomectomy (3.41%), and appendectomy (5.12%). More than one previous surgery was recorded for 29.91% of cases. General preoperative characteristics for the study population are summarized in .
Table 1 General preoperative characteristics in the study population (n = 117)
Intraoperative characteristics
Surgery time was up to 30 minutes in 55 (59.82%) cases, 31–60 minutes in 43 (24.78%) cases, and more than 60 minutes in 19 (15.98%) cases. Uterine volume reduction techniques were not necessary in 76 (64.95%) cases, but were needed in 41 (35.04%) to complete the hysterectomy. The most commonly associated surgery was salpingectomy (81.19%), but several patients had gynecological surgery additional to salpingectomy, including ovarian surgery in 31 (26.49%) cases, a transobturator sling procedure in 18 (15.38%) cases, and posterior culdoplasty in 43 (36.75%) cases. The most commonly used anesthesia was subdural (68.37%). Complications encountered during the surgical procedure were bladder lesions (8.54%) and hemorrhage (1.28%), with conversion to abdominal surgery being necessary in one case (1.28%) because of bleeding. General intraoperative characteristics for the study population are summarized in .
Table 2 General intra-operative characteristics in the studied population (n = 117)
Postoperative characteristics
Hospitalization time ranged from 24 hours to 48 hours (82.05% and 17.94%, respectively). The most common complications were vaginal cupola granuloma in 32.47%, urinary tract infection in 12.82%, and vaginal cupola hematoma in 2.56% of cases. Chi-square testing showed a statistically significant relationship between surgery time and uterine volume (χ2 = 17.367; P = 0.002), but not for surgery time and associated surgery (χ2 = 0.640; P = 0.726), or surgery time and previous related surgery (χ2 = 3.063; P = 0.216). General postoperative characteristics from the study population and comparisons between surgery time and uterine volume, surgery time and associated surgery, surgery time and need for additional surgery, and surgery time and prior surgery are summarized in –. All women in this study were already patients attending the outpatient clinics of the operating surgeons, so there were no dropouts or patients lost to follow-up.
Table 3 General postoperative characteristics in the studied population (n = 117)
Table 4 Descriptive analysis for quantitative variables (n = 117)
Table 5 Correlation between surgery time and uterine volume (n = 117)
Table 6 Correlation between surgery time with- or no-complementary surgery achievement (n = 117)
Table 7 Correlation between surgery time in presence, or not, of previous surgery (n = 117)
Discussion
Hysterectomy is the most common surgical procedure performed for uterine disease, with up to 20% women undergoing the procedure by the age of 60 years in the 20th century.Citation16 Despite the introduction of minimally invasive approaches to treat various benign uterine problems, and the long time period for which the vaginal route has been used to perform hysterectomy for benign uterine disease, hysterectomy is still performed abdominally in most cases, and the vaginal approach is used in only 20%–25% of women who undergo the procedure in the US regardless of the indication.Citation4,Citation8,Citation10,Citation17,Citation18
It has been shown that the vaginal route is more advantageous than any other approach to hysterectomy for a number of reasons, including a shorter recovery time, less pain in the postoperative period, a rapid return to former activity levels, and absence of visible scarring.Citation9,Citation10,Citation19
The aim of our study was to evaluate preoperative, intraoperative, and postoperative characteristics of women undergoing removal of the uterus. Our results are similar to those of other studies in the literature, which have reported a patient age range of 41–50 years,Citation9,Citation10,Citation20–Citation25 myoma as the main indication, spinal anesthesia as the most commonly used anesthetic procedure,Citation22–Citation24 volume uterine reduction often being performed, a surgery time of about 75 minutes, and oophorectomy being a frequently associated procedure.Citation10,Citation20,Citation22,Citation26
In a similar study of 190 women reported by Prota,Citation11 the mean patient age was 44.6 years, 91% of women had had at least one prior pregnancy, and 72.1% had undergone a cesarean section. The most common indication for surgery was uterine myoma causing abnormal vaginal bleeding. Uterine volume reduction was performed in 50% of cases, and surgery additional to the main procedure was performed in 22.6%. Spinal anesthesia was frequently performed, and the duration of surgery was up to 75 minutes in 58.9% of cases. Postoperative complications were observed in 3.7%, with bladder lesions being the most common, and patient recovery time was less than 48 (mean 31.5) hours in 87.4% of cases.
Harmanli et al conducted a comparative study of the vaginal and abdominal routes for hysterectomy, and reported results similar to ours for mean patient age and parity, frequency of adnexal removal, and indications for hysterectomy (mainly uterine fibroids, menometrorrhagia, pelvic pain).Citation3 An apparent limitation of our study is the lack of a control group against which to compare our results; however, follow-up was continued for at least 12 months, which is arguably adequate to assess the outcome of vaginal hysterectomy.
Some authors have cited a number of factors that may influence the route of hysterectomy for benign causes, including the size and shape of the vagina and uterus, accessibility to the uterus, extent of extrauterine disease, need for concurrent procedures, surgeon training and experience, available hospital technology and support, emergency or scheduled cases, and the preference of the informed patient.Citation5 A narrow pubic arch (less than 90 degrees), an undescended immobile uterus, nulliparity, and prior cesarean delivery have also been proposed by some authors as contraindications for vaginal hysterectomy,Citation6 but were not confirmed in our study.
In our series, vaginal hysterectomies were performed in many women who had never given birth vaginally and in some with a uterine volume larger than 300 mL but with adequate vaginal caliber to allow successful completion of surgery, with no complications or additional surgical time needed. Doucette et al have reported that if the vagina can allow access to divide the uterosacral and cardinal ligaments, uterine mobility is usually increased enough to allow vaginal hysterectomy, even in cases where there is minimal uterine descent, and when the uterus is enlarged, vaginal hysterectomy often can be accomplished safely by using uterine size reduction techniques, such as wedge morcellation, uterine bisection, and intramyometrial coring.Citation12
When performing routinely bilateral salpingo-oophorectomy where possible we make it hidrosalpinx and ovarian cancer prevention, and so in this work we reached levels of 81.19% for salpingectomy and 26.49% for oophorectomy associate to vaginal hysterectomy. Reports in the literature indicate that most ovaries are visible and readily accessible during vaginal surgery, and it is generally safe to perform bilateral salpingo-oophorectomy at the time of vaginal hysterectomy.Citation26,Citation27 We believe that the elective decision to perform routine bilateral salpingo-oophorectomy is not a contraindication to performing vaginal hysterectomy. The most common recovery time was 24 hours, which we consider advantageous compared with abdominal hysterectomy, after which the recovery time is usually 48 hours. The most common postoperative complication was vaginal cupola granuloma (32.47%) which we considered to be irrelevant in terms of both frequency and severity. The other postoperative complications were vaginal cupola hematoma in 2.56% of cases and urinary infection in 12.82%.
In a randomized trial, Benassi et al compared the outcomes of the two methods of hysterectomy for a uterine weight of 200 g or more. They found that the complication rates were not significantly different, except for postoperative fever, which occurred more often after an abdominal procedure.Citation9
Our results show a shorter recovery time, what is economically appealing, and reiterates the results of other studies showing that vaginal hysterectomy is a safe surgical approach in women with any indication for hysterectomy, and with a low complication rate. It is likely that many patients would choose the vaginal route if it is presented as an option that eliminates abdominal wound complications and leaves no visible scars.Citation3
Conclusion
Vaginal hysterectomy is a safety surgical route for hysterectomy, with favorable performance and a low complication rate.
Disclosure
The authors report no conflicts of interest in this work.
References
- NieboerTEJohnsonNLethabyASurgical approach to hysterectomy for benign gynaecological diseaseCochrane Database Syst Rev20093CD00367719588344
- FarquharCMSteinerCAHysterectomy rates in the United States 1990–1997Obstet Gynecol20029922923411814502
- HarmanliOHGentzlerCKByunSDandoluVGrodyMHTA comparison of abdominal and vaginal hysterectomy for the large uterusInt J Gynaecol Obstet200487192315464771
- American College of Obstetricians and GynecologistsPrecis IV: An Update in Obstetrics and GynecologyWashington, DC1989 [CD-ROM]
- WuJMWechterMEGellerEJNguyenTVViscoAGHysterectomy rates in the United States, 2003Obstet Gynecol20071101091109517978124
- [No authors listed]ACOG Committee Opinion No 444. Choosing the route of hysterectomy for benign diseaseObstet Gynecol20091141156115820168127
- TohicALDhainautCYazbeckCHallaisCLevinIMadelenatPHysterectomy for benign uterine pathology among women without previous vaginal deliveryObstet Gynecol200811182983718378741
- DevalBRafiiASorianoDSamainELevardonMDaraiEMorbidity of vaginal hysterectomy for benign tumors as a function of uterine weightJ Reprod Med20034843544012856514
- BenassiLRossiTKaihuraCTAbdominal or vaginal hysterectomy for enlarged uteri: a randomized clinical trialAm J Obstet Gynecol20021871561156512501064
- HwangJLSeowKMTsaiYLHuangLWHsiehBCLeeCComparative study of vaginal, laparoscopically assisted vaginal and abdominal hysterectomies for uterine myoma larger than 6 cm in diameter or uterus weighing at least 450 g: a prospective randomized studyActa Obstet Gynecol Scand2002811132113812519109
- ProtaFEPre, intra and postoperative parameters of women undergoing vaginal hysterectomy in the absence of uterine prolapseThesis (PhD) Parâmetros pré, intra e pós-operatórios de mulheres submetidas à histerectomia vaginal na ausência de prolapso uterino Tese (Doutorado)Universidade Estadual de Campinas2006
- DoucetteRCSharpHTAlderSCChallenging generally accepted contraindications to vaginal hysterectomyAm J Obstet Gynecol20011841386138911408857
- International Continence Society, Committee on Standardisation of TerminologyThe standardization of terminology of lower urinary tract functionOstergardDRBentAEUrogynecology and Urodynamics: Theory and Practice3rd edBaltimore, MDWilliams and Wilkins1991
- BumpRCMattiassonABoKThe standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunctionAm J Obstet Gynecol199617510178694033
- PersuCChappleCRCauniVGutueSGeavletePPelvic Organ Prolapse Quantification System (POP–Q) – a new era in pelvic prolapse stagingJ Med Life20114758121505577
- Royal College of Obstetricians and GynaecologistsThe management of menorrhagia in secondary careLondonRCOG Press1999 (Evidence-based clinical guideline No 5)
- MagosABournasNOSinhaRRichardsonREO’ConnorHVaginal hysterectomy for the large uterusBr J Obstet Gynecol1996103246251
- DickerRCGreenspanJRStraussLTComplications of abdominal and vaginal hysterectomy among women of reproductive age in the United States: the Collaborative Review of SterilizationAm J Obstet Gynecol19821448418487148906
- HoffmanMSDeCesareSKalterCAbdominal hysterectomy versus transvaginal morcellation for the removal of enlarged uteriAm J Obstet Gynecol19941713093138059807
- Figueiredo NettoOFigueiredoEGFigueiredoPGPelosiMAPelosiMAIIIRDVaginal removal of the benign non-prolapsed uterus: experience with 300 consecutive operationsObstet Gynecol19999434835110472857
- RibeiroSCRibeiroRMSantosNCPinottiJAA randomized study of total abdominal, vaginal and laparoscopic hysterectomyInt J Gynaecol Obstet200383374314511870
- MiskryTMagosARandomized, prospective, double-blind comparison of abdominal and vaginal hysterectomy in women without uterovaginal prolapseActa Obstet Gynecol Scand20038235135812716320
- DaraiESorianoDKimataPLaplaceCLecuruFVaginal hysterectomy for enlarged uteri, with or without laparoscopic assistance: randomized studyObstet Gynecol2001975 Pt 171271611339921
- OttosenCLingmanGOttosenLThree methods for hysterectomy: a randomised, prospective study of short term outcomeBr J Obstet Gynaecol200010713801385
- SorianoDGoldsteinALecuruFDaraiERecovery from vaginal hysterectomy compared with laparoscopy-assisted hysterectomy: a prospective, randomized, multicenter studyActa Obstet Gynecol Scand20018033734111264609
- ShethSSThe scope of vaginal hysterectomyEur J Obstet Gynecol Reprod Biol200411522423015262361
- KovacSRHysterectomy outcomes in patients with similar indicationsObstet Gynecol20009578779310831967