Abstract
Objective
To investigate the awareness and use of folic acid in European women of child-bearing age, particularly in the setting of pregnancy and pregnancy planning.
Methods
Between November 2009 and December 2009, women aged 15–49 years old from 18 European countries completed a 30-minute structured questionnaire either online or via face-to-face interviews. To achieve nationally representative samples for each country quotas were set for age, education, income, and regional distribution.
Results
A total of 22,925 women participated in the survey. Of the respondents, 58% had at least one biological child, and of these 38% reported that their first pregnancy was not planned. Nearly 60% of women who planned their pregnancy indicated that they had stopped using their method of contraception without first consulting a doctor or another health care professional. Overall, 70% reported that they had heard of folic acid and 40% stated that they knew the benefits of folic acid. However, when prompted to indicate which diseases and/or birth defects folic acid can protect against, only 17% knew that folic acid can reduce the risk of neural tube defects/spina bifida.
Conclusions
A large proportion of European women of child-bearing age in this survey were unaware that periconceptional folic acid supplementation reduces the risk of birth defects.
Introduction
“Neural tube defects” (NTDs) is a term used to describe a range of potentially debilitating and sometimes fatal conditions, the most common of which are anencephaly (characterized by total or partial absence of the brain) and spina bifida (characterized by the presence of a bony vertebral defect).Citation1 NTDs are the second most common birth defect after congenital cardiac malformations,Citation2 the latter including septal defects, patent ductus arteriosus, and narrowing of the valves.Citation3 The main cause of NTDs are abnormalities that occur during neurulation, a process that results in the formation of the neural tube and ultimately the spinal cord, brain, and central nervous system.Citation1 Neurulation is usually complete by 28 days postconception.Citation1
There is well-documented evidence that the occurrence of NTDs can be reduced if women receive folate supplementation in the periconceptional period.Citation4 Many countries currently recommend that women planning to become pregnant receive 400 μg/day of folic acid at least 1 month prior to conception and for up to 3 months postconception.Citation5–Citation7 Despite such recommendations, the decline in the prevalence of NTDs has fallen short of expectations;Citation8,Citation9 in the UK and Ireland, for example, NTD prevalence has declined by 32% since the implementation of folic acid supplementation policies,Citation9 far short of the 72% reduction suggested by a Cochrane review of five clinical trials.Citation4
There is, therefore, an urgent need to better understand the awareness and behavior of women regarding pregnancy and folic acid consumption. A number of studies have examined the awareness and use of folic acid in individual countries.Citation10–Citation17 To our knowledge, there have been no large-scale surveys conducted to date to examine the overall awareness and use of folic acid among women in a wide range of European countries. This report aims to investigate the awareness and use of folic acid in women of child-bearing age, mainly in the setting of pregnancy and pregnancy planning, in Europe.
Methods
During November 2009 and December 2009, a European survey was conducted online (or face-to-face where necessary) in 18 countries: Austria, Czech Republic, Denmark, France, Germany, Greece (face-to-face), Italy, The Netherlands, Norway, Poland, Portugal (face-to-face), Russia, Spain, Sweden, Switzerland, Turkey (face-to-face), the Ukraine (face-to-face), and the UK. Face-to-face interviews were deemed necessary in countries where the overall female population was incongruent with the online female population, thus restricting the sampling procedure. In Turkey, Greece, the Ukraine, and Portugal, internet utilization overall tends to be restricted primarily to the upper education and income segments. In addition, in Turkey and the Ukraine, online access is restricted primarily to urban regions. Countries were selected with the aim of ensuring the highest possible coverage of the European female population. The 30-minute structured questionnaire was pretested in two countries (Germany and the UK) by performing three or four pilot interviews via a web conference. For the majority of the questions in the survey, the answers were predefined.
Data were collected by GfK Healthcare, Germany, which is an independent global market research vendor. Funding for this survey was provided by Bayer HealthCare Pharmaceuticals. The target was to survey approximately 2000 women in each of France, Germany, the UK, Italy, and Spain, approximately 500 in Greece, and approximately 1000 in the remaining countries. Different sample sizes for each country were chosen for two main reasons: first, to account for different population sizes across countries; and second, due to budget constraints. Larger sample sizes were included in some countries in order to allow more detailed analyses of subgroups on a national level. Women aged 15–49 years were recruited via purposive sampling from an existing GfK consumer online panel, setting quotas for age, education, income, and regional distribution in order to achieve nationally representative samples for each country. In order to qualify for the survey women had to complete a screening questionnaire. Women who had been sterilized or received a hysterectomy were automatically excluded from further questioning. The remainder of the questionnaire was designed to determine the women’s awareness and use of contraceptive methods in more detail, their behavior and attitude towards contraception, their use of physicians and other information resources when planning pregnancy, and their awareness of folic acid and its benefits. Women received an incentive of €3.60 for completing the survey. Data analysis was conducted using the software IBM SPSS Statistics (IBM Corporation, Armonk, NY, USA). Countries were analyzed individually; however, when calculating aggregated European results, country data were weighted according to the population size of women aged 15–49 years in each country. This report presents data from the survey relating to the awareness and use of folic acid, and the corresponding section of the questionnaire is included in the Supplementary materials.
Results
In total, 22,925 women completed the survey. The number of women included and excluded in each country is shown in . presents the unweighted and weighted sociodemographic characteristics of the survey respondents. Overall, 58% of the respondents had at least one biological child.
Table 1 Proportion of women included and excluded from the sample in each country
Table 2 Patient sociodemographic characteristics
Obstetric history and contraception
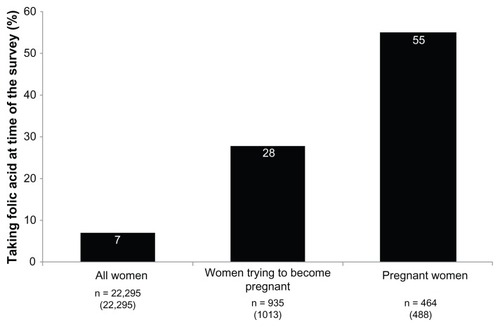
Of the combined European respondents who had at least one biological child, 38% reported that their first pregnancy was unplanned (). In general, the rates of unplanned pregnancy were fairly similar between the countries, ranging between 25% and 47% (with the exception of The Netherlands, which had the lowest rate of unplanned pregnancy at 16%).
Figure 1 The proportion of European women with at least one biological child who answered “yes” to the question, “Now please think of the pregnancy with your first child, was this a planned or unplanned pregnancy?”.
Abbreviations: EU, total Europe; AT, Austria; CZ, Czech Republic; DK, Denmark; FR, France; DE, Germany; GR, Greece; IT, Italy; NL, Netherlands; NO, Norway; PL, Poland; PT, Portugal; RU, Russia; ES, Spain; SE, Sweden; CH, Switzerland; TR, Turkey; UA, Ukraine; UK, United Kingdom; n, number.
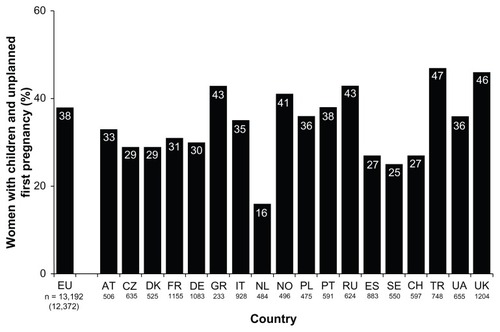
Of the women who did plan their first pregnancy, just under one-fifth (18%) reported that they had consulted their doctor or another health care professional prior to stopping their birth control. More than half (56%) of the women who planned their first pregnancy reported that they stopped using their method of contraception without first consulting their doctor or another health care professional (). The majority of the remaining women either had not used a contraceptive before (19%), or did not recall their behavior at that time point (4%). Frequencies varied considerably between the countries. The proportion of women who reported not consulting their doctor or another health care professional before stopping birth control in order to become pregnant was highest in Sweden (85%) and The Netherlands (81%). In contrast, only around one-third of women in Turkey (32%) and Poland (33%) did not consult their doctor under such circumstances.
Figure 2 Among European women with biological children and who planned their first pregnancy, responses to the question, “When you were making plans to become pregnant with your first child, which of the following did you do?”.
Abbreviations: EU, total Europe; AT, Austria; CZ, Czech Republic; DK, Denmark; FR, France; DE, Germany; GR, Greece; IT, Italy; NL, Netherlands; NO, Norway; PL, Poland; PT, Portugal; RU, Russia; ES, Spain; SE, Sweden; CH, Switzerland; TR, Turkey; UA, Ukraine; UK, United Kingdom; n, number.
Awareness and use of folic acid
All women
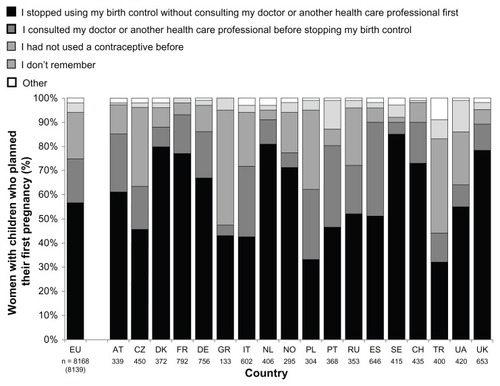
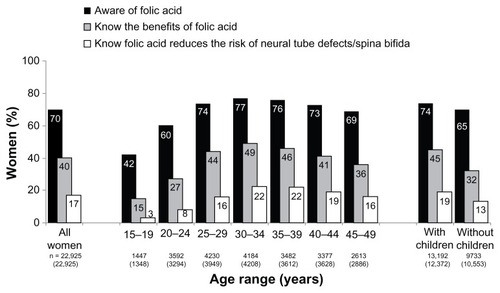
Overall, 70% of the women reported that they had heard of folic acid before, and 40% stated that they knew the benefits of folic acid. However, when the women were prompted to indicate which diseases and/or birth defects folic acid can protect against, only 17% of the overall sample knew that folic acid can reduce the risk of NTDs/spina bifida ().
Figure 3 The proportion of European women who answered “yes” to the questions, “Have you heard of folic acid?” and “Do you know what the benefits of folic acid are?” and the proportion of women who identified neural tube defects/spina bifida when asked, “Which of the following diseases/birth defects can folic acid protect against?”.
Abbreviations: EU, total Europe; AT, Austria; CZ, Czech Republic; DK, Denmark; FR, France; DE, Germany; GR, Greece; IT, Italy; NL, Netherlands; NO, Norway; PL, Poland; PT, Portugal; RU, Russia; ES, Spain; SE, Sweden; CH, Switzerland; TR, Turkey; UA, Ukraine; UK, United Kingdom; n, number.
The rate of awareness of folic acid and knowledge about its benefits differed across countries, with the highest rates of awareness in the UK and Poland (>90%) and the lowest rates in Turkey and Greece (,40%). A similar trend was observed for those who knew that folic acid can protect against NTDs/spina bifida, although the rates were particularly low in Greece, Russia, Turkey, the Ukraine (,3%), and France (7%). Considering the other potential options given in this question (where more than one option could be chosen), the following percentages of the overall sample indicated that folic acid can protect against anemia (16%), autism (3%), cystic fibrosis (4%), Down syndrome (7%), thrombosis (3%), and cardiovascular disease/health (8%).
Awareness and knowledge of the benefits of folic acid were particularly low among young women. For example, only 42% of the teenagers in the sample had heard of folic acid before, only 15% reported that they were aware of its benefits, and only 3% knew that folic acid could reduce the risk of NTDs/spina bifida (). However, women’s awareness of folic acid and knowledge of its benefits did increase after they had given birth to a child compared with those who had not had a child ().
Figure 4 The proportion of European women who answered “yes” to the questions, “Have you ever heard of folic acid?” and “Do you know what the benefits of folic acid are?” and the proportion of women who identified neural tube defects/spina bifida when asked, “Which of the following diseases/birth defects can folic acid protect against?”.
Abbreviation: n, number.
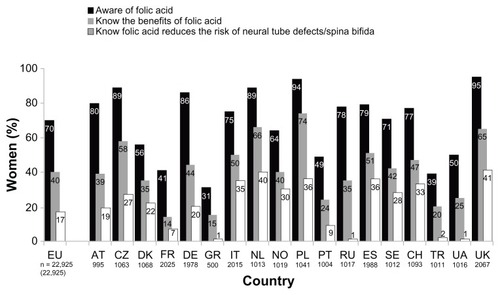
In total, only 37% of the respondents had taken folic acid at some point (7% at the time of the survey); the most common reason given was because of advice from a doctor or other health care professional (52%). This was followed by the woman being pregnant (33%) or planning to become pregnant (18%). Only 28% of those women currently trying to become pregnant (versus 55% of pregnant women) were taking a folic acid supplement even though guidelines recommend that all these women should take a folate supplement every day (). However, adherence to folic acid intake was reported to be low; only 56% of women using folic acid while trying to become pregnant reported that they took their supplement every day; 38% reported that, on average, they missed 1–2 out of 7 days, and 6% reported missing ≥ 3 days out of 7. This adherence level was comparable to women using folic acid, who were already pregnant; only 63% took their supplement every day, while 30% missed 1–2 days and 7% missed ≥ 3 out of 7 days.
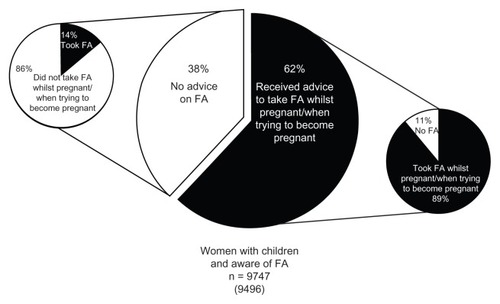
Women with biological children
Of the women with a biological child and who were aware of folic acid, 62% received advice to take folic acid either while they were pregnant or while planning a pregnancy, and of these women, 89% actually took folic acid (). In contrast, of the 38% of women who did not receive such advice only 14% took periconceptional folic acid of their own accord. The predominant source of information/advice on folic acid was reported to be from a gynecologist (79%), followed by a general practitioner (17%), or a midwife (16%). The main reasons reported by the women for not taking folic acid when pregnant or trying to become pregnant were: deficient advice (“No one advised me to take it,” 43%) and lack of awareness (“I didn’t know about folic acid,” 40%).
Figure 6 The proportion of European women with biological children and aware of FA who answered “yes” to the question, “Did you receive any advice/information to take folic acid either whilst you were pregnant or when you were thinking of becoming pregnant?” and “Again thinking of the pregnancy with your first child, did you take a folic acid supplement whilst you were pregnant or when you were trying to become pregnant for the first time?”
Abbreviations: FA, folic acid; n, number.
Discussion
This survey of more than 20,000 European women of child-bearing age showed that a large proportion of the sample is unaware of the need for folic acid supplementation, particularly during the periconceptional period. While 70% of the respondents indicated that they had heard of folic acid, less than one-half (40%) indicated that they knew what the benefits of folic acid are and even fewer (less than one-fifth) knew, when prompted, that folic acid can protect against NTDs/spina bifida. On average, less than 40% of the women had ever taken folic acid.
These findings are comparable to those of a number of other studies. In a survey of 4515 women of child-bearing age in Argentina, Brazil, Canada, France, Germany, Italy, Russia, the UK, and the USA, 83% of women surveyed had heard of folic acid and 55% knew that folic acid reduces the risk of NTDs.Citation18 In a survey of 148 women living in Vancouver, Canada, most of the women (95%) had heard of folic acid, while only 25% knew that it could prevent birth defects.Citation15 Similarly, a self-administered questionnaire of 578 women in Western Australia demonstrated that the majority (89%) of the women had heard, seen, or read about a link between folate and birth defects.Citation11 In the USA, the March of Dimes Foundation Survey of approximately 2000 women aged 18–45 years also found that a large proportion had heard of folic acid, but only a few knew that folic acid could prevent birth defects, and that it needs to be taken before pregnancy.Citation19 Similar to the present study, in the March of Dimes Foundation Survey those aged less than 24 years had the lowest rates of awareness, which indicates a particular need to educate younger women on the benefits of the periconceptional use of folic acid.Citation20
Health care providers can play an important role in counseling women on the benefits and timely use of folic acid and to motivate them to take folic acid when planning pregnancy or when pregnant. In this survey, the most common source of information on folic acid was reported to be from a gynecologist (79%), which is similar to other studies.Citation10 The importance of such advice can be observed by the fact that, when women received advice on folic acid intake when planning a pregnancy or when pregnant, the majority did go on to take folic acid. In contrast, periconceptional use of folic acid in women who did not receive advice was very low. In some cases the opportunity to provide timely counseling regarding folic acid supplementation prior to pregnancy can be missed because even women who plan their pregnancy may stop their method of contraception without first consulting their doctor or another health care professional about their plans to become pregnant; indeed, this was observed in nearly 60% of women in the current survey who planned their first child. Similar findings have been noted in recent surveys conducted among women of child-bearing potentialCitation18 and physicians.Citation21
There is accumulating evidence that even with the introduction of government policies, clinical recommendations, and health education campaigns, the decrease in the incidence of NTDs/spina bifida has been lower than anticipated.Citation8,Citation9 A contributing factor to low folate levels prior to conception is the high number of unplanned pregnancies. In this survey, 38% of the women reported that their first pregnancy was unplanned, which is consistent with a global survey among women of child-bearing age (36%),Citation18 and with other studies with rates ranging between 10% and 62%.Citation22,Citation23 In unplanned pregnancies, women are unable to commence periconceptional supplementation, as was noted in a study of Danish women.Citation24
An additional issue with taking daily folate supplements is compliance. The level of adherence with folic acid intake was similar between women who were trying to become pregnant and with those who were pregnant; in this survey, 44% and 37% of women, respectively, reported that they forgot to take their folic acid supplement at least once a week. Similarly, in a study of Swiss women, only 5% of the women were found to fully comply with folic acid recommendations, and in many cases the doctors did not know their patients’ true folic acid intake.Citation25 Elevating and maintaining optimal folate levels is essential because the occurrence of NTDs is known to be directly linked to maternal folate status in the periconceptional period.Citation26 Increasing red blood cell folate levels lessens the risk of an NTD-affected pregnancy. A maternal red blood cell folate concentration of ≥906 nmol/L (400 ng/mL) is associated with a very low risk of NTDs (0.8 per 1000 births).Citation26 Current European guidelines recommend that women receive a folic acid intake of 400 μg/day at least 1 month during preconception and up to the first 3 months postconception,Citation5,Citation6 but as indicated here and in other studies, folate intake is still inadequate.Citation20,Citation27,Citation28
It is therefore imperative that initiatives are implemented across Europe to increase awareness and knowledge of the benefits of folic acid among women of child-bearing age. Preconceptional counseling should be integrated into school curricula on health and sex education and into family planning consultations for contraception; while the latter may seem counterintuitive, family planning consultations represent an excellent opportunity to advise women about future pregnancies and preconceptional health care interventions. Implementing such strategies should be of particular value in younger age groups, in which knowledge and awareness of folic acid is particularly low, as shown in our survey. All women of child-bearing age, including those who are not planning pregnancy in the near future, should receive information and advice on the appropriate use of folic acid in order to make an informed decision. It has been suggested that in countries where food fortification is not permitted, creative, structural public health strategies are required to promote the use of folic acid to lessen the risk of NTDs.Citation29 In addition, it would be desirable to find alternative ways to increase folic acid consumption in women of child-bearing age other than through food fortification and folate supplements. Folate-fortified oral contraceptives have been identified as a reasonable delivery vehicle for improving folate status in women of childbearing age.Citation30 Two folate-fortified combined oral contraceptives were approved in the USA in 2010 for the improvement of folate status in women who desire contraception; one was comprised of ethinylestradiol (EE) 20 μg/drospirenone 3 mg/levomefolate calcium 451 μg, and the other was compromised of EE 30 μg/drospirenone 3 mg/levomefolate calcium 451 μg.Citation31 A double-blind randomized study showed that folate status improved during 26 weeks of treatment with EE 30 μg/drospirenone 3 mg/levomefolate calcium 451 μg, and folate concentrations declined slowly following the cessation of folate intake.Citation32
The findings in this report are subject to the inherent limitations of using a survey. First, many of the questions in this survey had predefined answers, and this means that the true answer might not have been provided as an option for some women. In addition, some of the questions required past recall, such as the intake of folic acid. The answers may not, therefore, reflect the actual extent of knowledge and consumption of folic acid of the entire population. Second, apart from the countries that used face-to-face interviews, the online nature of this survey may have been a limitation, as women without internet access or those who were not computer literate would not have been included. This may have meant that our sample was biased towards women of a higher education or income level. Hence, there may be a tendency to exclude and underestimate the number of women of child-bearing age from lower socioeconomic groups or with lower educational status. In addition, women were selected from an existing online panel, which will have limited the results to women who had already signed up to participate in studies, leading to a high response rate. Finally, because the majority of countries used online surveys, there was no means to obtain clarification of any ambiguous or missing answers; moreover, questions may have been subject to individual interpretation or recall bias. Despite these limitations, our results provide valuable insight into the awareness and utilization of folic acid in women across Europe.
In conclusion, many women in this European survey were unaware of the importance of taking folic acid during the periconceptional period to reduce the risk of NTDs. The survey therefore highlights a real unmet need to provide women of child-bearing age with appropriate counseling and education regarding the benefits and timely use of folic acid supplementation. With this in mind, each consultation between a woman and her health care professional should be used as a means of education. Family planning consultations represent an excellent opportunity to advise women about future pregnancies and preconceptional health care interventions such as folic acid.
Acknowledgments
Funding for this study was provided by Bayer HealthCare Pharmaceuticals. The authors would like to thank Clare Wheatcroft and Claire Byrne of inScience Communications, Springer Healthcare, for medical writing assistance; funding for this was provided by Bayer HealthCare Pharmaceuticals.
Supplementary material
Table S1 Questionnaire
Disclosure
Johannes Bitzer has participated in advisory boards for Bayer HealthCare Pharmaceuticals, Merck Sharp and Dohme (MSD), Lilly, Solvay Pharma, and Boehringer Ingelheim, and has lectured at meetings supported by Bayer HealthCare Pharmaceuticals, MSD, Lilly, Solvay Pharma, and Boehringer Ingelheim. Dr von Stenglin and Dr Bannemerschult are employees of Bayer HealthCare Pharmaceuticals.
References
- BottoLDMooreCAKhouryMJEricksonJDNeural-tube defectsN Engl J Med1999341201509151910559453
- CheschierNfor ACOG Committee on Practice Bulletins-ObstetricsACOG practice bulletin. Neural tube defects Number 44. Jul 2003 (Replaces committee opinion number 252 Mar 2001)Int J Gynaecol Obstet200383112313314626221
- National Heart Lung, and Blood InstituteTypes of congenital heart defects [webpage on the Internet]Bethesda, MDUnited States Department of Health and Human Services2011 Available from: http://www.nhlbi.nih.gov/health/health-topics/topics/chd/types.htmlAccessed June 12, 2012
- De-RegilLMFernández-GaxiolaACDowswellTPena-RosasJPEffects and safety of periconceptional folate supplementation for preventing birth defectsCochrane Database Syst Rev201010CD00795020927767
- European Surveillance of Congenital Anomalies (EUROCAT)Special Report: Prevention of Neural Tube Defects by Periconceptional Folic Acid Supplementation in Europe. Part IIa–Country Specific Chapters (Austria to Ireland)Newtonabbey, IrelandEuropean Surveillance of Congenital Anomalies2009 Available from: http://www.eurocat-network.eu/content/Special-Report-NTD-3rdEd-Part-IIA.pdfAccessed October 6, 2010
- European Surveillance of Congenital Anomalies (EUROCAT)Special Report: Prevention of Neural Tube Defects by Periconceptional Folic Acid Supplementation in Europe. Part IIb–Country Specific Chapters (Italy to UK)Newtonabbey, IrelandEuropean Surveillance of Congenital Anomalies2009 Available from: http://www.eurocat-network.eu/content/Special-Report-NTD-3rdEd-Part-IIB.pdfAccessed October 6, 2010
- US Preventive Services Task ForceFolic acid for the prevention of neural tube defects: US Preventive Services Task Force recommendation statementAnn Intern Med2009150962663119414842
- Centers for Disease Control and Prevention (CDC)Spina bifida and anencephaly before and after folic acid mandate – United States, 1995–1996 and 1999–2000MMWR Morb Mortal Wkly Rep2004531736236515129193
- BusbyAAbramskyLDolkHArmstrongBfor Eurocat Folic Acid Working GroupPreventing neural tube defects in Europe: population based studyBMJ2005330749157457515760997
- BaykanZOztürkAPoyrazoğluSGünIAwareness, knowledge, and use of folic acid among women: a study from TurkeyArch Gynecol Obstet2011283612591253
- OddyWHMillerMPayneJMSernaPBowerCIAwareness and consumption of folate-fortified foods by women of childbearing age in Western AustraliaPublic Health Nutr2007101098999517683648
- PötzschSHoyer-SchuschkeJSeeligMSteinbickerVKnowledge among young people about folic acid and its importance during pregnancy: a survey in the Federal State of Saxony-Anhalt (Germany)J Appl Genet200647218719016682762
- SayedARNixonJBourneDEFolic acid awareness among women of reproductive age in Cape TownS Afr Med J20069611216440103
- KondoAKamihiraOShimosukaYOkaiIGotohMOzawaHAwareness of the role of folic acid, dietary folate intake and plasma folate concentration in JapanJ Obstet Gynaecol Res200531217217715771645
- FrenchMRBarrSILevy-MilneRFolate intakes and awareness of folate to prevent neural tube defects: a survey of women living in Vancouver, CanadaJ Am Diet Assoc2003103218118512589323
- RingelSLahatEElizovTAwareness of folic acid for neural tube defect prevention among Israeli womenTeratology1999601293210413336
- CastillaEEDutraMGFolate awareness among South American womenLancet199734990537359078232
- von StenglinABuchwaldSLynenRWomen’s awareness and use of folate supplements prior to and during pregnancy: a global perspectiveEur J Contracept Reprod Health Care201015s1111112
- Green-RaleighKCarterHMulinareJPrueCPetriniJTrends in folic acid awareness and behavior in the United States: the Gallup Organization for the March of Dimes Foundation surveys, 1995–2005Matern Child Health J200610Suppl 5S177S18216823638
- Centers for Disease Control and Prevention (CDC)Use of supplements containing folic acid among women of childbearing age – United States, 2007MMWR Morb Mortal Wkly Rep20085715818185493
- von StenglinABuchwaldSLynenRPhysicians’ knowledge and prescribing practices of folic acid supplementation: a global perspectiveEur J Contracept Reprod Health Care201015s1112113
- RayJGSinghGBurrowsRFEvidence for suboptimal use of periconceptional folic acid supplements globallyBJOG2004111539940815104602
- FinerLBHenshawSKDisparities in rates of unintended pregnancy in the United States, 1994 and 2001Perspect Sex Reprod Health2006382909616772190
- KnudsenVKOrozova-BekkevoldIRasmussenLBMikkelsenTBMichaelsenKFOlsenSFLow compliance with recommendations on folic acid use in relation to pregnancy: is there a need for fortification?Public Health Nutr20047784385015482608
- PorettiAAnheierTZimmermannRBoltshauserEfor Swiss Pediatric Surveillance Unit (SPSU)Neural tube defects in Switzerland from 2001 to 2007: are periconceptual folic acid recommendations being followed?Swiss Med Wkly200813841–4260861318941947
- DalyLEKirkePNMolloyAWeirDGScottJMFolate levels and neural tube defects. Implications for preventionJAMA199527421169817027474275
- European Surveillance of Congenital Anomalies (EUROCAT)Special Report: Prevention of Neural Tube Defects by Periconceptional Folic Acid Supplementation in EuropeNewtonabbey, IrelandEuropean Surveillance of Congenital Anomalies2009 Available from: http://www.eurocat-network.eu/content/Special-Report-NTD-3rdEd-Part-I.pdfAccessed October 6, 2010
- Centers for Disease Control and Prevention (CDC)Trends in wheat-flour fortification with folic acid and iron – worldwide, 2004 and 2007MMWR Morb Mortal Wkly Rep200857181018185494
- EichholzerMTönzOZimmermannRFolic acid: a public-health challengeLancet200636795191352136116631914
- United States Food and Drug AdministrationSummary minutes advisory committee for reproductive health drugs meeting December 15, 2003 [webpage on the Internet]Bethesda, MDUnited States Food and Drug Administration2003 Available from: http://www.fda.gov/ohrms/dockets/ac/03/minutes/4002M1_Final.htmAccessed December 20, 2012
- LassiZSBhuttaZAClinical utility of folate-containing oral contraceptivesInt J Womens Health2012418519022570577
- DiefenbachKTrummerDEbertFEthinylestradiol/drospirenone/levomefolate calcium versus ethinylestradiol/drospirenone + folic acid: folate status during 24 weeks of treatment and over 20 weeks following treatment cessationInt J Womens Health2013514916323610531