Abstract
Aim
This study aimed to determine whether there were differences in attitude, awareness, and intention to perform female genital mutilation or cutting for their daughters in the future between female healthcare providers and mothers.
Methods
A comparative cross-sectional study design was used.
Results
A total of 508 women were included in the study. Of the participants, 68.7% (n = 349) were mothers (Group I) who visited the hospital and 31.3% (n = 159) were women healthcare professionals (Group II) [27% (n = 137) nurses and 4.3% (n = 22) doctors]. It was found that 8 (1.6%) of the participants did not have FGM/C and the FGM/C ratio was lower in group II (95%) than in group I (100%) (p < 0.001). In group I, 99.7% (n = 299) of the participants and 30.6% (n = 19) of those in group II reported intending to perform FGM for their daughters in the future (p < 0.001). The reasons for FGM/C most cited by participants were a traditional rite of passage into womanhood (78%), religious requirement (69.3%), and preservation of their virginity until marriage (59.3%). “Stop FGM” was given as a message on FGM/C by 60% of the participants (n = 79) who answered (n = 127, 100%) to open-ended questions.
Conclusion
The results of this study show that female health professionals with higher education and monthly income had less positive perception of their FGM/C and less intention to allow their daughters to undergo FGM/C.
Introduction
Female Genital Mutilation or cutting (FGM/C) is defined as “all procedures that involve the partial or total removal of the external genitalia or another injury to the female genital organs (such as stitching of the labia majora or pricking of the clitoris) for non-medical reasons” according to care of women and girls living with female genital mutilation: a clinical handbook based on the World Health Organization (WHO) Guidelines on the management of health complications from female genital mutilation.Citation1 The prevalence report estimated that over 200 million girls and women are living with FGM/C.Citation2,Citation3 Although FGM/C was prohibited by many countries in the Middle East and Africa, this procedure is still too common in several countries such as Somalia, Guinea, Mali, Djibouti, and Sudan in Africa.Citation1,Citation2,Citation4,Citation5 Somali Health and Demographic Survey (2020) reported that almost every Somali woman aged 15–49 has undergone female circumcision.Citation6
UNFPA and UNICEF have jointly led the largest global program to accelerate the elimination of female genital mutilation (FGM) since 2008 because FGM/C violates basic human rights.Citation7 Legal and policy frameworks banning female genital mutilation have been implicated in 14 of the 17 countries supported by the UNFPA-UNICEF Joint Programme. However, FGM/C is practiced for a variety of sociocultural reasons, including respect for tradition, rite of passage, social convention, enhancing fertility, marriageability, ensuring virginity, chastity and faithfulness, cleanliness and beauty, femininity, religion in regions and ethnic groups in which it is practiced common.Citation1,Citation8 The most common reason for FGM/C was reported in a study as a religion by Kaplan et alCitation9 and cultural reasons by Ali.Citation10
Besides genital mutilation has no health benefits and the practice can cause physical, mental, and sexual health problems in female children’s and women’s lives, such as severe pain, bleeding, infection, urinary problems, mental distress, and gynecological and childbirth complications.Citation2,Citation3,Citation6,Citation11 In a study, 41% of health professionals reported that they had seen female children with complications of FGM/C in Gambia.Citation9 Another study from Australia and New Zealand by Moeed et al indicated that 47% of obstetricians and gynecologists and trainees had seen at least one woman or girl with complications related to FGM/C “most commonly” urinary problems, problems in labour and dyspareunia.Citation12
According to the WHO, “healthcare providers should provide girls and women with the best clinical care while avoiding further harm to them. Health professionals have a key role to influence and change attitudes about FGM/C and women’s bodies and rights.Citation1 In addition, they could also consult in the decision-making process about whether a girl or a woman needs to seek further care. As a health-care provider, every contact with a girl or woman who has experienced FGM/C represents an opportunity to provide her with accurate information about her body and health. “In a community in which FGM/C is still common practice, it is important to be aware of the knowledge, attitude, and practice regarding FGM/C of health professionals. Although there are many studies on the determination of FGM/C knowledge, attitudes, and practice (KAP) of health professionalsCitation8,Citation9 and mothers,Citation13–15 there is a scarcity of research on KAP of comparison of the outcomes of both two groups.Citation16 This study aimed to determine whether there were differences in terms of attitude, awareness, and intention to perform female genital mutilation or cutting for their daughters in the future between women healthcare providers and mothers. The outcomes of the present study could provide insight into the views of women with or without health education.
Methods
Study Design
A comparative cross-sectional study design was used.
Study Setting
This comparative cross-sectional study was conducted in Mogadishu, Somalia Turkey Recep Tayyip Erdoğan Training and Research Hospital between October 2022 and January 2023. The hospital is one of the largest tertiary referral healthcare facilities in Mogadishu, East Africa. The hospital serves pediatric patients in the newborn intensive care unit with 18 beds and a pediatric intensive care unit with eight beds. The hospital also provides service with 54 beds and three pediatric outpatient clinics since 2015.
Participants
The participants in this study were women health professionals and mothers. A total of 508 women were included in the study, of which 68.7% (349) were women admitted to the hospital and 31.3% (159) were healthcare professionals. In post hoc power analysis using G-Power software, the power of the study was found to be 98.7% with 508 participants (Group I: 349 and Group II: 159), 0.05 alpha error, the 100% and 95% incidence rate of the event (having FGM/C) for Group I and Group II, respectively (Supplementary Figure 1).
Group I (Mothers)
The population of this group included 8236 mothers admitted for acute health conditions of their children to the pediatric outpatient clinics of the hospital between October 7, 2022, and January 15, 2023. Of those, 349 (%4.3) mothers agreed to take part in this study. Inclusion criteria for group I were (i) being mothers, (ii) aged over 18 years, (iii) being able to give informed consent, and (iv) applying to the pediatric outpatient clinics of the hospital. Exclusion criteria included fathers in the present study.
Group II (Female Health Professionals)
Between October 2022 and January 2023, 159 women health professionals in group II filled out the questionnaire, including 27% (n = 137) nurses and 4.3% (n = 22) doctors. Inclusion criteria for female health professionals were (i) being a women health professional and (ii) voluntary participation in the study. Inclusion criteria for mothers were (i) visiting the pediatric outpatient clinic of the hospital for acute health conditions of her child and (ii) voluntarily participating in the study. Exclusion Criteria for both women health professionals and mothers included (i) being male participants.
Data Collection Form
The form content was developed based on a handbook by the WHO (2018) entitled “Care of Girls & Women Living with Female Genital Mutilation: A Clinical Handbook”.Citation1 This form consisted of both open-ended and closed questions addressing sociodemographic characteristics, types of FGM/C, perceptions, and attitudes towards FGM/C, complications related to FGM/C, and intention to practice FGM/C for their daughters (Supplementary Data Collection Form).
Procedure
The data of female health professionals and mothers were collected by four data collectors. Data collectors who were third-year nursing students who volunteered to be data collectors in this study were trained by the same researcher (DS) for three days on the familiarization of the questionnaire, interview techniques, and data collection procedure, and they delivered the questionnaire to female health professionals and mothers. Data were collected through face-to-face interviews using a structured questionnaire. The principal investigator checked the filled questionnaires daily for completeness, accuracy, and consistency.
Ethical Permissions
The study was approved by the Non-Interventional Clinical Research Ethics Committee of XX (Approval number: MSTH −12,097, Date: October 17, 2022). All participants were informed about the purpose of the study and were assured of anonymity and confidentiality of the data. Written and verbal informed consent was obtained from all participants.
Statistical Analysis
Collected data were analyzed using the Epi info 7.2 software. Descriptive data were expressed with numbers (n), percentages (%), median, minimum (min), and maximum (max) values. The distribution property of the continuous data was evaluated with the Kolmogorov–Smirnov test. The x2 test or Fisher’s exact test was used to compare two categorical variables, and Mann–Whitney U-tests were used for two-group comparisons. Statistical significance was accepted as p < 0.05.
Results
The sociodemographic characteristics of the participants are shown in . A total of 508 women were included in the study. Of the participants, 68.7% (n = 349) were mothers (Group I) admitted to the hospital and 31.3% (n = 159) were female healthcare professionals (Group II) [27% (n = 137) nurses and 4.3% (n = 22) doctors]. It was found that 8 (1.6%) of the participants did not have FGM/C and the FGM/C ratio was lower in group II (95%) than in group I (100%) (p < 0.001). Type 2 FGM/C was most commonly performed in both groups (p < 0.001). Although the frequency of FGM/C is high in healthcare workers, it was observed that positive perception of their FGM/C was significantly lower in healthcare workers (3.8%) than in mothers (99.7%) (p < 0.001). While pain, bleeding, infection, swelling in the genital area, and painful or difficult urination were more common in the mother group (p < 0.001), psychological conditions were more common in the healthcare worker group according to self-reported (p = 0.003).
Table 1 Comparison Sociodemographic Characteristics, FGM/C-Related Characteristics and FGM/C Complications of Participants According to Groups (n = 508)
Ninety-nine percent (n = 299) of the participants in group I and 30.6% (n = 19) of participants in group II group reported that they intended to perform the FGM/C for their daughters in the future in (p < 0.001). Fifty-three percent of the participants in group I and 22.6% in group II had daughters with FGM/C (p < 0.001), with Type 2 being the most prevalent FGM/C type in both groups (p < 0.001). In terms of complications, physical problems, pain, hemorrhage, swelling in the genital area, acute urine retention, and acute urine retention were reported as more common physical health conditions in the daughters of participants in group I (p < 0.05) than in the daughters of participants in group II (p < 0.05) ().
Table 2 Comparison of the Distributions of Participants’ FGM/C Intention for Their Daughters, FGM-Related Complications, and Characteristics of FGM/C Practice
Female health professionals had less positive perception for their FGM/C and had less intention to allow their daughters to undergo FGM/C. The number of children with FGM/C of participants in Group I was more than those of Group II ().
Table 3 Comparison of Having FGM/C, Positive Perception for Their FGM/C and Intention to FGM/C for Her Child
In the comparison of FGM/C status and the participants’ sociodemographic characteristics, FGM/C was more common in those who were married (p = 0.016), had a low-income level (p < 0.001), and had more children (p = 0.003) (). Positive perception for their FGM/C was higher in married participants than single participants, primary school graduates compared to those with secondary school or higher education graduates (p < 0.001), those with lower income than those with higher income (p < 0.001), those with more children than those with fewer children (p < 0.001), and those with daughters than those without daughters (p < 0.001) ().
Table 4 Comparison of Participants’ Self-FGM/C Status and Perception with FGM/C According to Characteristics of Participants
It was found that those who had their daughters undergo FGM/C were older (p < 0.001), had a lower education level (p < 0.001), had lower monthly income (p < 0.001), and had more children (p < 0.001) (). In addition, participants with low education levels (p < 0.001), low income (p < 0.001), and those with more children (p < 0.001) had a higher intention to allow their children to undergo FGM/C ().
Table 5 Comparison of the FGM/C Status of the Participants’ Daughters and Their Intention to Allow Their Daughters to Undergo FGM/C, and Their Sociodemographic Characteristics
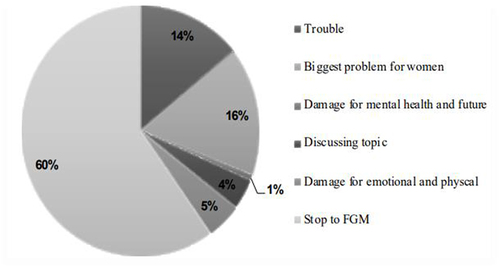
Seventy-eight percent of the participants perceived FGM/C as a rite of passage, 69.3% as a religious requirement, 59.3% as preservation of their virginity until marriage, 0.4% as being more feminine and beautiful, and 1.2% as being more hygienic and more beautiful, as well as provision of spiritual purity. The opinions of the participants about FGM/C are shown in .
Figure 1 Views of participants on FGM/C (n = 508).
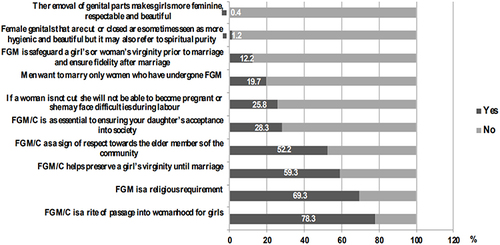
When participants were asked to describe FGM/C, 60% (n = 76) answered “Stop FGM”, 16% (n = 21) “Biggest problem for women”, 14% (n = 18), “Trouble”, and 13% (n = 17), “No to FGM”. The distribution of participants’ perceptions of FGM/C is shown in .
Discussion
The International Continence Society (ICS, 2018) has emphasized that FGM/C violates basic human rights. However, FGM/C is a common sociocultural practice in many countries (Payne CK). The prevalence of FGM/C varies from 0.3% to 99.2% in the African region.Citation17 In a study, the prevalence of FGM/C among women and girls ages 15 to 49 years old in Egypt was 87%,Citation18 FGM/C is still practiced in Somalia.Citation19 According to the Somalia Health and Demographic Survey,Citation6 99.2% of women have undergone FGM/C. A systematic review and meta-analysis study showed that the prevalence of FGM/C for both women and girls in 26 countries of Africa region has decreased while the prevalence for women in three countries including Somalia, Guinea-Bissau, Burkina Faso of Africa region has increased.Citation17 Almost all mothers and female health professionals in this study have undergone FGM/C. This result presents substantial evidence for health policymakers and professionals that there is a need for interventions and policies to prevent performing FGM/C for children and women in Mogadishu.
In this study, the female health professionals stated that they were positively perception for their FGM/C, and they had experienced more physical health problems related to their self-FGM/C than mothers. A study of Keles et al found that educated women were aware of the adverse health effects of FGM/C.Citation14 One of the associated factors of having FGM/C is socioeconomic status.Citation20 A study conducted by Elduma showed that women from poorer households were more prone to practice FGM/C than those from wealthier households.Citation20 This could show that female health professionals have easier access to knowledge and social media due to their educational and economical status than mothers with low education status.
This study has indicated that mothers and grandmothers were the primary decision makers for FGM/C. Regarding the key role of mothers and grandmothers in FGM/C, the results are similar to those reported by Abathun et al,Citation21 Pashaei et al,Citation22 Tag-Eldin et al,Citation23 Shell-Duncan et al,Citation24 Bjalkander et alCitation25 and Herieka and Dhar.Citation26 According to our findings, there is a need for educational programs for mothers and grandmothers who have a pivotal role as decision-makers on FGM/C of female children.
Beliefs about the reasons for performing FGM/C are cultural, religious requirements, social, medical, economic, and cosmetic.Citation8 Muhula showed that girls who did not undergo FGM were considered to be children since they did not have the traditional rite of passage into womanhood. In the same study, a participant stated that
Some of us we are big girls but are going to school. We seat with circumcised girls in class. They under look at us only that they consider themselves as women and we are a girl. They will not dare even seat with you.Citation27
Similar to the study of Muhula, three of the four participants cited as a rite of passage to womanhood for girls as the reason for FGM/C in our study. The second reason cited by 69.3% of participants was a religious requirement. According to the Somalia Health and Demographic Survey,Citation6 72% believed that female circumcision was a religious requirement. In a study by Gele et al, almost all of the participants believed that FGM/C is a religious requirement for their culture.Citation27
One of the reasons for FGM/C was virginity until marriage in this study. Similarly, in a study conducted in Somalia by Gele et al,Citation27 a participant mentioned that men preferred to marry circumcised women. These reasons show that social pressure, stigmatization toward uncircumcised in society and religious beliefs contribute significantly to the practice of FGM/C.Citation28,Citation29 The findings of our study are in line with other studies,Citation30 which point to daughters of participants in mothers have more undergone FGM/C than those in women health professionals and the intention to allow their daughters to undergo FGM/C has been higher in mothers than women health professionals in our study. In addition to higher education, women health professionals with higher monthly income were less likely to perform FGM/C on their daughters. This result was similar to the studies of Muhula et alCitation28 and Setegn et al.Citation29 These studies revealed that women who had higher education level and wealth were less supportive of the continuation of the practice of FGM. In another study conducted by Ameyaw et al,Citation31 women with higher education levels had less intentions to perform FGM/C on their daughters. Sabahelzain et alCitation32 indicated that education was critical in influencing mothers’ attitudes towards the practice of FGM/C.
Over half of the participants who answered the open-ended question related to the message for readers towards FGM/C practice stated “stop to FGM/C”, while only a few participants thought FGM/C was a distinguishing issue. In a study conducted by Adigüzel et al, almost all of the participants thought that FGM/C is a harmful traditional practice that should be stopped.Citation33 The most highly cited message from both mothers and women health professionals in our study is a clue to the need for help for female children and an increase in interventional educational programs for mothers and older women in Mogadishu.
There are two limitations of the study. First, the results showed the attitudes of only female health professionals towards FGM/C. There is need to studies including male health professionals with high educational status. Second, the outcomes of our study could show the prevalence of FGM/C. Also, the study was limited to a single health center, and a restricted group, which may have been a limitation as well. Hence, the findings of this study should be interpreted with these limitations in mind.
Conclusion
This study compared Somalian mothers and female health professionals in terms of attitude towards FGM/C and intention to allow their daughters to undergo FGM. The results of this study show that female health professionals who have high education and monthly income are aware of the psychological conditions related FGM/C, and they have less intention to allow their daughters to undergo FGM/C. Our study reveals crucial insight about a key role of female health professionals for policy implications. The female health professionals have greater responsibility for empowering women who visit hospitals through educational interventions regarding FGM/C-related complications including physical and psychological health problems of mother and their children. It is recommended that women health professionals who are aware of the complications of FGM/C and they have less intention to allow their daughters to undergo FGM/C should be engage with policymakers to accelerate the elimination of female genital mutilation (FGM) for healthy future of female children.
Data Sharing Statement
The dataset used and/or analyzed in the study is available from the corresponding author on reasonable request.
Ethical Statement
Ethical approval for this study was provided by the Somalia. Mogadishu–Turkey Recep Tayyip Erdogan Training and Research Hospital Ethics Committee (Approval number: MSTH −12097). The database management in accordance with privacy legislation and the presented study in accordance with the ethical principle of the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest.
Acknowledgments
The authors would like to thank the study participants for their contribution.
Additional information
Funding
References
- World Health Organization. Care of Women and Girls Living with Female Genital Mutilation: A Clinical Handbook. Geneva: World Health Organization; 2018.
- The Lancet Public Health. COVID-19 hindering progress against female genital mutilation. Lancet Public Health. 2021;6(3):e136. doi:10.1016/S2468-2667(21)00030-X
- UNICEF. Female genital mutilation/cutting: a global concern. New York: UNICEF; 2016. Available from: https://data.unicef.org/resources/female-genital-mutilationcutting-global-concern/. Accessed July 31, 2023.
- Khosla R, Banerjee J, Chou D, Say L, Fried ST. Gender equality and human rights approaches to female genital mutilation: a review of international human rights norms and standards. Reprod Health. 2017;14(1):59. doi:10.1186/s12978-017-0322-5
- Waigwa S, Doos L, Bradbury-Jones C, Taylor J. Effectiveness of health education as an intervention designed to prevent female genital mutilation/ cutting (FGM/C): a systematic review. Reprod Health. 2018;15(1):62. doi:10.1186/s12978-018-0503-x
- Somalia National Bureau of Statistics. Federal Government of Somalia. The Somali Health and Demographic Survey; 2020. Available from: https://somalia.unfpa.org/sites/default/files/pub-pdf/shds_report_2020_1.pdf. Accessed February 20, 2023.
- OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO. Eliminating female genital mutilation: an interagency statement; 2008. Available from: https://apps.who.int/iris/handle/10665/43839. Accessed July 31, 2023.
- Zurynski Y, Sureshkumar P, Phu A, Elliott E. Female genital mutilation and cutting: a systematic literature review of health professionals’ knowledge, attitudes and clinical practice. BMC Int Health Hum Rights. 2015;15:32. doi:10.1186/s12914-015-0070-y
- Kaplan A, Forbes M, Bonhoure I, et al. Female genital mutilation/cutting in The Gambia: long-term health consequences and complications during delivery and for the newborn. Int J Womens Health. 2013;5(1):323–331. doi:10.2147/IJWH.S42064
- Ali AA. Knowledge and attitudes of female genital mutilation among midwives in Eastern Sudan. Reprod Health. 2012;9:23. doi:10.1186/1742-4755-9-23
- World Health Organization. Female genital mutilation: integrating the prevention and the management of the health complications into the curricula of nursing and midwifery: a teacher’s guide. Geneva: World Health Organization; 2001 Available from: https://apps.who.int/iris/handle/10665/66857. Accessed November 11, 2022.
- Moeed SM, Grover SR. Female genital mutilation/cutting (FGM/C): survey of RANZCOG fellows, diplomates & trainees and FGM/C prevention and education program workers in Australia and New Zealand. Aust N Z J Obstet Gynaecol. 2012;52(6):523–527. doi:10.1111/j.1479-828X.2012.01476.x
- Van Eekert N, Van de Velde S, Anthierens S, et al. Mothers’ perceptions of the medicalisation of female genital cutting among the Kisii population in Kenya. Cult Health Sex. 2022;24(7):983–997. doi:10.1080/13691058.2021.1906952
- Keles E, Eker HH, Bektemur G, et al. Determinants of disagreement with female genital mutilation among mothers. Int J Womens Health. 2022;14:1863–1870. doi:10.2147/IJWH.S391043
- Melese G, Tesfa M, Sharew Y, Mehare T. Knowledge, attitude, practice, and predictors of female genital mutilation in Degadamot district, Amhara regional state, Northwest Ethiopia, 2018. BMC Women's Health. 2020;20(1):178. doi:10.1186/s12905-020-01041-2
- El-Gibaly O, Aziz M, Abou Hussein S. Health care providers’ and mothers’ perceptions about the medicalization of female genital mutilation or cutting in Egypt: a cross-sectional qualitative study. BMC Int Health Hum Rights. 2019;19(1):26. doi:10.1186/s12914-019-0202-x
- Farouki L, El-Dirani Z, Abdulrahim S, Akl C, Akik C, McCall SJ. The global prevalence of female genital mutilation/cutting: a systematic review and meta-analysis of national, regional, facility, and school-based studies. PLoS Med. 2022;19(9):e1004061. doi:10.1371/journal.pmed.1004061
- Ministry of Health and Population [Egypt]. El-Zanaty and Associates [Egypt], and ICF International. Egypt Health Issues Survey. Cairo and Rockville: Ministry of Health and Population and ICF International; 2015.
- Payne CK, Abdulcadir J, Ouedraogo C, et al. International continence society white paper regarding female genital mutilation/cutting. Neurourol Urodyn. 2019;38(2):857–867. doi:10.1002/nau.23923
- Elduma AH. Female genital mutilation in Sudan. Open Access Maced J Med Sci. 2018;6:4304. doi:10.3889/oamjms.2018.099
- Abathun AD, Sundby J, Gele AA. Attitude toward female genital mutilation among Somali and Harari people, Eastern Ethiopia. Int J Womens Health. 2016;8:557–569. doi:10.2147/IJWH.S112226
- Pashaei T, Rahimi A, Ardalan A, et al. Related factors of female genital mutilation (FGM) in Ravansar (Iran). J Women’s Health Care. 2012;1(2):1000108. doi:10.4172/2167-0420.1000108
- Tag-Eldin MA, Gadallah MA, Al-Tayeb MN, Abdel-Aty M, Mansour E, Sallem M. Prevalence of female genital cutting among Egyptian girls. Bull. World Health Organ. 2008;86(4):269–274. doi:10.2471/blt.07.042093
- Shell-Duncan B, Moreau A, Wander K, Smith S. The role of older women in contesting norms associated with female genital mutilation/cutting in Senegambia: a factorial focus group analysis. PLoS One. 2018;13:e0199217. doi:10.1371/journal.pone.0199217
- Bjalkander O, Leigh B, Harman G, Bergstrom S, Almroth L. Female genital mutilation in Sierra Leone: who are the decision makers? Afr J Reprod Health. 2012;16:119–131.
- Herieka E, Dhar J. Female genital mutilation in the Sudan: survey of the attitude of Khartoum university students towards this practice. Sex Transm Infect. 2003;79(3):220–223. doi:10.1136/sti.79.3.220
- Gele AA, Bø BP, Sundby J. Have we made progress in Somalia after 30 years of interventions? Attitudes toward female circumcision among people in the Hargeisa district. BMC Res Notes. 2013;6:122. doi:10.1186/1756-0500-6-122
- Muhula S, Mveyange A, Oti SO, et al. The impact of community led alternative rite of passage on eradication of female genital mutilation/cutting in Kajiado County, Kenya: a quasi-experimental study. PLoS One. 2021;16(4):e0249662. doi:10.1371/journal.pone.0249662
- Setegn T, Lakew Y, Deribe K. Geographic variation and factors associated with female genital mutilation among reproductive age women in Ethiopia: a national population based survey. PLoS One. 2016;11(1):e0145329. doi:10.1371/journal.pone.0145329
- Gupta GR. Female genital mutilation/cutting: a statistical overview and exploration of the dynamics of change. Reprod Health Matters. 2013;21(42):184–191.
- Ameyaw EK, Tetteh JK, Armah-Ansah EK, Aduo-Adjei K, Sena-Iddrisu A. Female genital mutilation/cutting in Sierra Leone: are educated women intending to circumcise their daughters? BMC Int Health Hum Rights. 2020;20(1):19. doi:10.1186/s12914-020-00240-0
- Sabahelzain MM, Gamal Eldin A, Babiker S, Kabiru CW, Eltayeb M. Decision-making in the practice of female genital mutilation or cutting in Sudan: a cross-sectional study. Glob Health Res Policy. 2019;4:5. doi:10.1186/s41256-019-0096-0
- Adigüzel C, Baş Y, Erhan MD, Gelle MA. The Female Genital Mutilation/Cutting Experience in Somali Women: their Wishes, Knowledge and Attitude. Gynecol Obstet Invest. 2019;84(2):118–127. doi:10.1159/000493130